Abstract
OBJECTIVE: To assess the effect of armodafinil, 150 mg, on the physiologic propensity for sleep and cognitive performance during usual night shift hours in patients with excessive sleepiness associated with chronic (≥3 months) shift work disorder (SWD) of moderate or greater severity.
PATIENTS AND METHODS: This 12-week, randomized controlled study was conducted at 42 sleep research facilities in North America from April 2 through December 23, 2004, and enrolled 254 permanent or rotating night shift workers with SWD. Entry criteria included excessive sleepiness during usual night shifts for 3 months or longer (corroborated by mean sleep latency of ≤6 minutes on a Multiple Sleep Latency Test), insomnia (sleep efficiency ≤87.5% during daytime sleep), and SWD that was judged clinically to be of moderate or greater severity. Patients received armodafinil, 150 mg, or placebo 30 to 60 minutes before each night shift. Physiologic sleep propensity during night shift hours, clinical impression of severity, patient-reported sleepiness, and cognitive function were assessed during laboratory night shifts at weeks 4, 8, and 12.
RESULTS: Armodafinil significantly improved mean (SD) sleep latency from 2.3 (1.6) minutes at baseline to 5.3 (5.0) minutes at final visit, compared with a change from 2.4 (1.6) minutes to 2.8 (2.9) minutes in the placebo group (P<.001). Clinical condition ratings improved in more patients receiving armodafinil (79%) vs placebo (59%) (P=.001). As reported by patients' diaries, armodafinil significantly reduced sleepiness during laboratory nights (P<.001), night shifts at work (P<.001), and the commute home (P=.003). Armodafinil improved performance on standardized memory (P<.001) and attention (power, P=.001; continuity, P<.001) tests compared with placebo. Armodafinil was well tolerated and did not affect daytime sleep, as measured by polysomnography.
CONCLUSION: In patients with excessive sleepiness associated with chronic SWD of moderate or greater severity, armodafinil significantly improved wakefulness during scheduled night work, raising mean nighttime sleep latency above the level considered to indicate severe sleepiness during the daytime. Armodafinil also significantly improved measures of overall clinical condition, long-term memory, and attention.
Trial Registration: clinicaltrials.gov Identifier: NCT00080288
In patients with excessive sleepiness associated with chronic shift work disorder of moderate or greater severity, armodafinil significantly improved wakefulness during scheduled night work, raising mean nighttime sleep latency above the level considered to indicate severe sleepiness during the daytime. Armodafinil also significantly improved measures of overall clinical condition, long-term memory, and attention.
CDR = Cognitive Drug Research; CGI-C = Clinical Global Impressions of Change; CGI-S = Clinical Global Impressions of Severity of Illness; KSS = Karolinska Sleepiness Scale; MSLT = Multiple Sleep Latency Test; nCPAP = nasal continuous positive airway pressure; OSA = obstructive sleep apnea; SWD = shift work disorder
Approximately 15% of employed adults in the United States work during nighttime hours.1 Night work induces a misalignment between the sleep-wake schedule and sleep and wake propensity that is controlled by the hypothalamic circadian pacemaker.2,3 In most people who work and/or commute during the night and early morning, circadian misalignment results in impaired wakefulness while working or commuting and, despite prior sleep deprivation, insomnia during daytime sleep.2,4-6 These are the symptoms of shift work disorder (SWD).7,8 In the recently revised International Classification of Sleep Disorders: Diagnostic and Coding Manual,7 the American Academy of Sleep Medicine changed the name of the condition formerly known as shift work sleep disorder to “circadian rhythm sleep disorder, shift work type (shift work disorder).” The patients in the current study meet the criteria of what is now called shift work disorder.
For editorial comment, see page 955
The most severely affected individuals may report falling asleep while working or commuting. In fact, one-third of night workers admit to regularly nodding off or falling asleep at least once per week while working, and half admit to falling asleep while commuting.9 Mitler et al10 reported that 56% of professional truck drivers experienced episodes of drowsy driving, 80% of which occurred during night driving. Moreover, 54% of the drowsy driving episodes involved just 10% of the drivers.10 A recent study of 2570 working adults found that 44.8% of night shift workers and 35.8% of rotating shift workers reported excessive sleepiness (ie, an Epworth Sleepiness Scale score of ≥10), and 18.5% of night shift workers and 15.7% of rotating shift workers reported moderate to severe insomnia during daytime sleep.4
Shift work can impair individuals' health status, occupational performance, and social well-being.1,11-13 These impairments appear to be greatest among those meeting diagnostic criteria for SWD. Patients with SWD are also at greater risk of cardiovascular disease, ulcers, depression, sleepiness-related accidents, and absenteeism compared with shift workers without SWD.4 Excessive sleepiness associated with SWD has been shown to have other effects, including impairments in cognition and psychomotor performance, which in turn may contribute to increased accidents during work and motor vehicle crashes during the morning commute.4,14,15
A randomized controlled study showed that the wakefulness-promoting agent modafinil (200 mg) improves wakefulness and the ability to sustain attention in patients with SWD.16 Despite the drug's 15-hour half-life, these effects were not sustained vs placebo throughout the entire night.16 Modafinil is a racemic compound that contains equal amounts of 2 enantiomers with different terminal half-lives: R-modafinil (armodafinil) is eliminated more slowly than S-modafinil and has a half-life of approximately 15 hours compared with a half-life of approximately 3 to 4 hours for S-modafinil. Preliminary data in healthy volunteers revealed that armodafinil, 200 mg, enabled individuals to sustain wakefulness and neurobehavioral performance more effectively in the final third of a simulated night shift compared with modafinil, 200 mg.17 We anticipated that elevated plasma concentrations of armodafinil later in the overnight shift and on the commute home would benefit patients with SWD because they are substantially impaired at those times.16 The current study assessed the efficacy and safety of armodafinil in patients with excessive sleepiness associated with chronic SWD of moderate or greater severity.
PATIENTS AND METHODS
This 12-week, randomized, double-blind, placebo-controlled, parallel-group, multicenter study was conducted with a common protocol at 42 centers in the United States (37) and Canada (5) from April 2 through December 23, 2004 (a center in Australia planned to but did not enroll any patients), in compliance with the International Conference on Harmonization's Good Clinical Practice Consolidated Guidance. An independent ethics committee or institutional review board at each center approved the protocol.
Patients participated in a screening visit, during which the Clinical Global Impressions of Severity of Illness (CGI-S) scale18 was completed and electronic diaries were dispensed. After a sequence of 3 or more consecutive night shifts, patients returned for an overnight sleep laboratory night shift to undergo baseline assessments and daytime polysomnography. Patients who met inclusion and exclusion criteria received study medication or placebo at a subsequent randomization visit. After this, patients were evaluated at weeks 4, 8, and 12 during an overnight laboratory night shift scheduled immediately after a sequence of 3 or more consecutive work night shifts.
Men and women between the ages of 18 and 65 years who worked 5 or more night shifts per month (each shift ≤12 hours, with ≥6 hours worked between 10 pm and 8 am and with ≥3 shifts occurring on consecutive nights) and planned to maintain this schedule for the duration of the treatment were screened for inclusion. Only individuals who exhibited signs and symptoms of SWD of moderate or greater severity, as documented by a CGI-S rating of 4 or higher18 for sleepiness on work nights, including the commute to and from work, were enrolled in the study. During screening, patients were assessed for SWD according to the International Classification of Sleep Disorders criteria.7 Inclusion criteria included a diagnosis of SWD according to the International Classification of Sleep Disorders; a complaint of chronic (≥3 months) excessive sleepiness during night shifts, which was corroborated by a mean sleep latency of 6 minutes or less on a nighttime Multiple Sleep Latency Test (MSLT); and insomnia, as indicated by daytime sleep efficiency of 87.5% or less (determined by 8-hour polysomnography). Patients with a history of substance abuse or medical or psychiatric disorders8 that could account for excessive sleepiness during the night shift were excluded, as were patients with any disorder that might interfere with drug pharmacokinetics or a known sensitivity to stimulants or modafinil. Female patients of childbearing potential were required to have a negative serum pregnancy test result at screening and to use a medically accepted method of birth control. Steroidal contraceptives had to be used in combination with a barrier method. Patients who consumed on average more than 600 mg/d of caffeine during the 7 days preceding the baseline visit were excluded from the study. In addition, patients were excluded if they took prescription drugs disallowed by the protocol or consumed clinically important amounts of nonprescription drugs within 7 days of the screening visit. Before study enrollment, all patients gave written informed consent.
Study participants were randomly assigned (1:1) to receive armodafinil, 150 mg (Cephalon Inc, Frazer, PA), formulated as 50-mg tablets or matching placebo 30 to 60 minutes before each night shift and no later than 11 pm. The study sponsor generated and maintained the randomization code, and all clinical personnel from the sponsor, investigators, and patients remained blinded to the identity of the study drug for the duration of the study. A central interactive voice response system for the randomization process ensured an overall balance among treatment groups within each country.
Patients received a dose of 50 mg on the first night, 100 mg on the second and third nights, and 150 mg on all subsequent nights. Patients took study medication only on nights when they worked the night shift or attended the sleep laboratory. During laboratory night shifts, study medication was administered at 10 pm (±30 minutes). The investigator reviewed patient diaries, work schedules, and drug accountability records for compliance at all postbaseline visits.
Efficacy Measures
Sleep propensity during laboratory night shifts was evaluated electrophysiologically using 20-minute MSLT19 sessions at midnight and at 2, 4, 6, and 8 am. Sleep latency was measured as the time from lights out to the first 30-second epoch scored as sleep according to standard criteria.20 If a patient fell asleep during the session, he or she was awakened and kept awake while remaining in bed for the remainder of the 20 minutes. If a patient did not fall asleep during the session, the test was terminated and sleep latency recorded as 20 minutes. The MSLT scoring was conducted blind to study condition at a central scoring site by 1 of 4 trained registered polysomnographic technologists (supervised by J.K.W.) according to standard criteria for research studies.21 All recordings for which mean sleep latency was distinct (61%) were scored by 1 technologist; the remainder were evaluated by 2 scorers. If mean latency differed by 1 minute or more between those 2 scorers, the assessment of a third technologist resolved the difference.
Investigators used the Clinical Global Impressions of Change (CGI-C) scale18 to assess changes from baseline in symptom severity during the night shift and the commute (established using the investigator-rated CGI-S) according to 7 categories ranging from “very much improved” to “very much worse.” Patient-estimated sleepiness was evaluated using the Karolinska Sleepiness Scale (KSS).22 Patients completed the KSS before every MSLT session. Patients completed daily electronic diaries that contained questions related to sleepiness and sleep, mistakes or accidents, and caffeine use during the night shift and the commute home, as well as questions concerning sleep on the days after night shifts. The diaries were reviewed monthly.
The computerized Cognitive Drug Research (CDR) system23-25 was administered at 12:30, 2:30, 4:30, 6:30, and 8:30 am of each laboratory night shift. The CDR battery included tests of memory (eg, numeric working memory test, word recognition test, immediate word recall test, delayed word recall test, and picture recognition test) and attention (eg, simple reaction time test, choice reaction time test, and digit vigilance task). Composite factors derived from the CDR included quality of episodic secondary memory (ability to encode, store, and retrieve verbal and pictorial information of an episodic nature), speed of memory (time required to retrieve information from episodic and working memory), power of attention (ability to focus attention), and continuity of attention (ability to sustain attention). Cognitive Drug Research Ltd was contracted to provide the CDR computerized assessment system to conduct the psychomotor and cognitive tests for this study. The CDR computerized system was delivered to each site, and the site staff were trained by qualified personnel. All data were captured electronically, except word recall, for which the patients wrote the words on recall sheets. The electronic data and recall sheets were returned to CDR Ltd, where the data were processed using validated procedures by qualified personnel (supervised by K.A.W.). After processing the data, CDR Ltd completed a quality assurance procedure on the dataset and transferred it to the study sponsor.
Safety and Adverse Effect Assessments
Adverse events were monitored throughout the study. Clinical laboratory tests, vital sign measurements, and 12-lead electrocardiography were conducted at screening, baseline, and the 4-, 8-, and 12-week visits. Vital signs were measured at approximately 3 and 11 hours after dosing at each laboratory visit, as well as at 6:15 pm after the daytime polysomnography at baseline and the final visit (approximately 20 hours after the dose). Electrocardiography was conducted at approximately 3 hours after dosing. Physical examinations were conducted at screening, baseline, and the final visit.
Daytime polysomnography was conducted for 8 hours starting at 10:15 am during the baseline screening and final laboratory night shifts to assess the effect of armodafinil on daytime sleep. Patients were scheduled to sleep in a dark, sound-attenuated, temperature-controlled room and were instructed to remain in bed even if they awakened before the end of the scheduled sleep episode. Sleep was scored according to standard criteria20 at the Henry Ford Hospital Sleep Disorders and Research Center. The scorers were all trained on the Rechtschaffen and Kales scoring system (supervised by T.R.). All potential scorers were required to score a series of standardized polysomnograms. The standardized polysomnograms that were used for determining scorer qualification had been staged by a consensus scoring of 3 sleep specialists accredited by the American Board of Sleep Medicine. Scorers were not qualified to score polysomnograms for this study until they obtained a 90% epoch-by-epoch agreement between their scoring and the consensus scoring on 3 consecutive standardized polysomnograms. During the study, all recordings were scored blind as to the study, site, treatment condition, and study night. Ten percent of these polysomnograms were selected to be scored a second time as a reliability check. Scorers performing the reliability checks were not aware that this was a reliability check (ie, it was presented as another study polysomnogram). These records were selected on a quasi-random basis. That is, records were selected randomly with the constraints that the number of records from each site be proportional to their enrollment of individuals into the study and that an equal number of records be selected from each treatment condition. Sixty-seven records were scored as a quality check. On the basis of epoch-by-epoch scoring of wake; sleep stages 1, 2, 3, and 4; and rapid eye movement; a percent agreement of epoch-by-epoch scoring was obtained. The mean percent agreement was 89.6%, with a range of 81.6% to 95.6%. Diary data related to the effect of study medication on daytime sleep were reviewed monthly.
Statistical Analyses
Sample size estimates were based on the results of data from previous clinical studies with armodafinil and modafinil. This analysis showed that a sample size of 108 patients per treatment arm would provide 85% power to detect a 1.5-minute difference in mean sleep latency on the MSLT between the armodafinil, 150 mg, group and the placebo group, assuming a common SD of 3.65 minutes. This sample size would have at least 90% power to detect a difference of 25% in the proportion of patients reporting at least minimal improvement in the CGI-C ratings between the armodafinil group and the placebo group, assuming a 37% rate in the placebo group. The planned enrollment was approximately 250 patients to ensure that 216 had at least 1 postbaseline MSLT assessment.
Demographic and baseline characteristics were summarized using descriptive statistics. Between-group comparisons of continuous demographic variables were conducted using analysis of variance with treatment group as a factor. Categorical variables were compared using the Pearson χ2 test or Fisher exact test.
The prespecified primary hypothesis was that armodafinil would increase mean sleep latency and improve the overall clinical condition in patients with excessive sleepiness associated with SWD. Two primary efficacy analyses were prespecified to test this hypothesis. The first was the change from baseline to final visit (12-week or last postbaseline measurement) in overall mean sleep latency (averaged across the last 4 nighttime sessions at 2, 4, 6, and 8 am) compared with placebo as assessed by the MSLT. The second was the proportion of patients who showed at least minimal improvement in the CGI-C rating for overall clinical condition during the night shift and commute to and from work at the final visit (12-week or last postbaseline measurement) compared with placebo.
Safety analyses were conducted using data from randomized patients who received at least 1 dose of study medication or placebo. Efficacy analyses were performed on data from randomized patients who had received at least 1 dose of study medication or placebo and had a baseline and at least 1 postbaseline assessment on the MSLT and CGI-C. Analyses of all efficacy variables at weeks 4, 8, and 12 used observed cases, and the final visit analyses were performed using the last postbaseline observation carried forward.
To analyze the KSS scores, data from the 4 tests associated with the MSLT naps at 2, 4, 6, and 8 am were averaged; and to analyze factor scores on memory and attention from CDR data, tests at 2:30, 4:30, 6:30, and 8:30 am were averaged. Mean sleep latency, mean KSS score, and CDR factor and component scores were assessed using analysis of variance with treatment group and country as factors. The CGI-C data were analyzed using a Cochran-Mantel-Haenszel χ2 statistic, adjusted for country. All tests of significance were 2-tailed, and the .05 level of significance was used.
Diary data were summarized using descriptive statistics. The comparison of treatment groups for the data from electronic diaries and polysomnographic recordings was performed using the Wilcoxon rank sum test. Safety data, as well as diary data related to the effect of study medication on daytime sleep, were summarized using descriptive statistics.
RESULTS
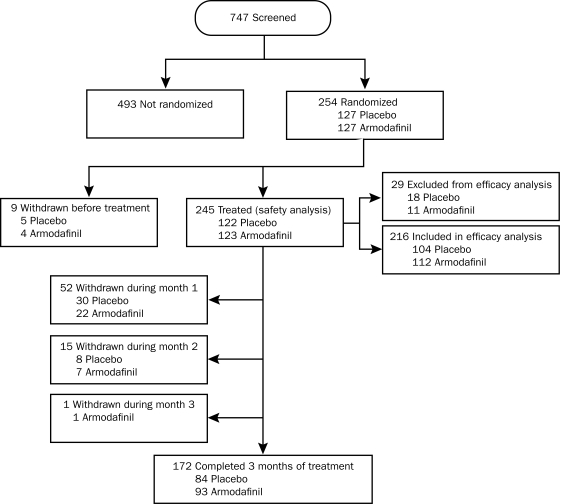
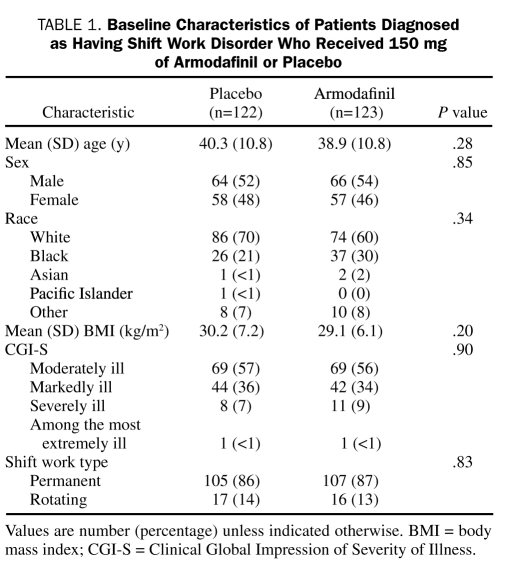
Of the 747 adults screened, 254 met entry criteria. Of these, 245 (96%) received at least 1 dose of study medication and were included in the safety analysis (Figure 1). At baseline, the armodafinil and placebo groups were similar in demographic variables and illness severity ratings (Table 1). Overall, 138 (56%) of 245 patients were rated by the investigator as moderately ill, and 107 (44%) of 245 patients were rated as markedly, severely, or extremely ill. Most patients (212/245; 87%) were permanent night shift workers. The largest area of industry represented was health care and social assistance, which accounted for 98 (40%) of 245 patients in the safety population.
FIGURE 1.
Patient disposition. Screened patients include patients referred from central advertising, investigators' advertising effort, and investigators' patients. Reasons patients were not randomized include the following: sleep efficiency of more than 87.5%, n=117; consent withdrawn, n=106; met exclusion criteria, n=67; clinically significant, uncontrolled medical or psychiatric condition, n=11; diagnosis of a sleep disorder other than shift work disorder (SWD), n=20; average daily caffeine consumption >600 mg/d, n=1; use of disallowed prescription or over-the-counter medications, n=10; history of substance abuse, n=2; positive urinary drug screen result at screening, n=27; disorder that may interfere with drug absorption, distribution, metabolism, or excretion, n=1; other (undetermined), n=1; mean sleep latency time greater than 6 minutes, n=45; lost to follow-up, n=36; patient in poor health, n=23; patient unable to comply with protocol, n=18; insufficient shift work exposure, n=16; patient does not meet clinical severity criteria, n=10; patient does not meet criteria for SWD diagnosis or excessive sleepiness, n=5; presence of another medical or psychiatric disorder that could account for the excessive sleepiness, n=4; adverse event, n=2; reason not provided, n=2; and other, n=55. Randomized patients who received at least 1 dose of drug and had a baseline and at least 1 postbaseline assessment for the Multiple Sleep Latency Test and Clinical Global Impressions of Improvement were included in efficacy analyses.
TABLE 1.
Baseline Characteristics of Patients Diagnosed as Having Shift Work Disorder Who Received 150 mg of Armodafinil or Placebo
The mean (SD) number of nights that patients received study medication was 42.4 (19.3) for the armodafinil group and 39.2 (18.2) for the placebo group. Sixty-eight (28%) of 245 patients withdrew from the study (30 in the armodafinil group and 38 in the placebo group). Reasons for discontinuing were adverse events (7 in the armodafinil group and 4 in the placebo group), consent withdrawn (3 in the armodafinil group and 16 in the placebo group), loss to follow-up (3 in the armodafinil group and 5 in the placebo group), nonadherence with study procedures (6 in the armodafinil group and 2 in the placebo group), and other (11 in the armodafinil group and 11 in the placebo group). No patients discontinued participation because of lack of efficacy.
The efficacy analysis included 216 (85%) of 254 patients. Patients were severely sleepy at baseline, with mean (SD) sleep latencies on the MSLT of 2.3 (1.6) minutes for the armodafinil group and 2.4 (1.6) minutes for the placebo group. For patients' own estimates of their sleepiness at baseline, the mean (SD) KSS score was 7.4 (1.4) in the armodafinil group and 7.3 (1.3) in the placebo group, and 97 (87%) of 112 patients in the armodafinil group and 87 (84%) of 104 in the placebo group had a KSS score of 6 or higher.
Primary Efficacy Measures
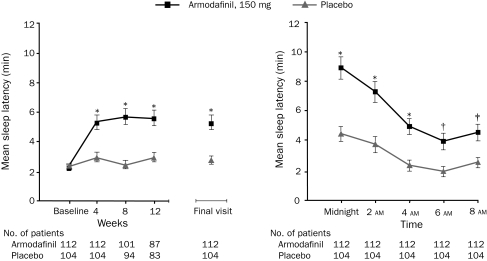
Armodafinil improved mean (SD) nighttime sleep latency (2-8 am) by 3.1 (4.5) minutes to 5.3 (5.0) minutes at the final visit, compared with an increase of 0.4 (2.9) minutes to 2.8 (2.9) minutes at the final visit in patients receiving placebo (difference between groups in change from baseline, P<.001; Figure 2, left). Of 112 patients who received armodafinil, 89 (79%) were rated as improved in the CGI-C ratings at the final visit compared with 61 (59%) of the 104 patients who received placebo (P=.001).
FIGURE 2.
Mean sleep latency on the Multiple Sleep Latency Test (MSLT). Sleep latency by visit for the last 4 tests (2-8 am) (left) and during the final visit night shift (midnight to 8 am) (right). Error bars indicate SEM. P values are based on the change from baseline compared with placebo. *P<.001, †P<.01, and ‡P<.05.
Secondary Efficacy Measures
Wakefulness Assessments. The significant increase from baseline in mean nighttime sleep latency in the armodafinil group relative to the placebo group was evident at the 4-, 8-, and 12-week assessments (Figure 2, left). The sleep latency for individual MSLT sessions at all 5 time points (midnight to 8 am) at the final visit was greater for patients who received armodafinil than for patients who received placebo (P<.001 at midnight, 2 am, 4 am; P=.007 at 6 am; P=.02 at 8 am (Figure 2, right). For the armodafinil group, 64 (57%) of 112 patients were “very much improved” or “much improved” at the final visit compared with 37 (36%) of 104 patients in the placebo group (P=.002). The proportion of patients with at least minimal improvement on the CGI-C rating of sleepiness was significantly greater for armodafinil than for placebo at the 4-week (armodafinil, 89/110 patients [81%]; placebo, 59/100 [59%]; P<.001), 8-week (armodafinil, 77/99 [78%]; placebo, 45/93 [48%]; P<.001), and 12-week (armodafinil, 75/96 [78%]; placebo, 50/89 [56%]; P=.001) assessments.
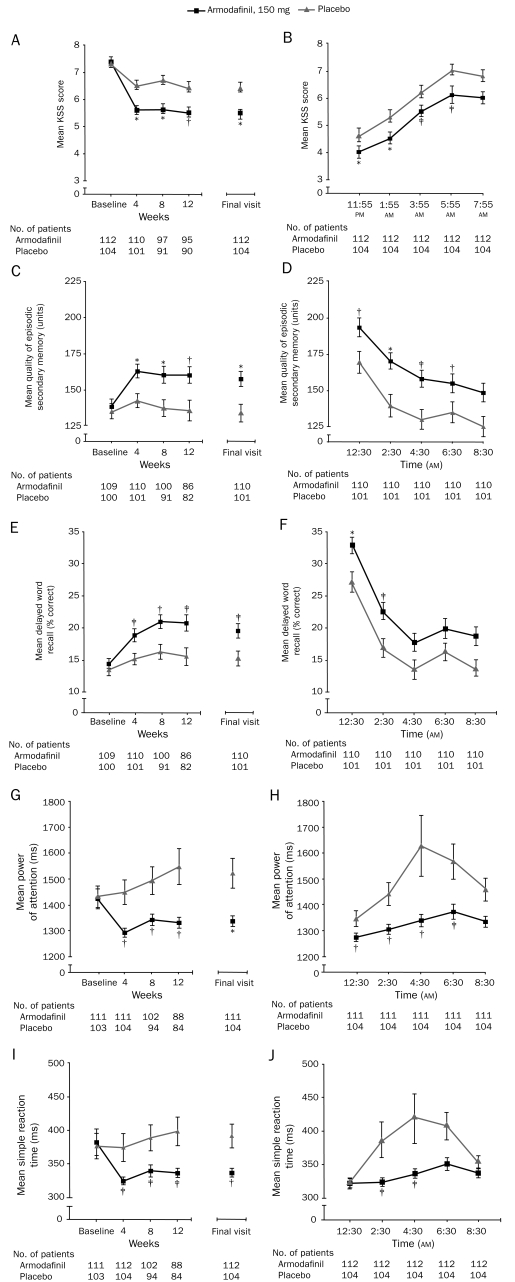
Patient-reported levels of sleepiness during the night shift on the KSS were significantly reduced for the armodafinil group compared with the placebo group at all visits (Figure 3, A). Patient-reported sleepiness at the first 4 time points at the final visit was significantly improved for patients who received armodafinil vs that for patients who received placebo (Figure 3, B).
FIGURE 3.
Mean Karolinska Sleepiness Scale (KSS) scores. Scores are by visit (A) and during the final visit night shift (midnight to 8 am) (B); for quality of episodic secondary memory by visit (C) and during the final visit night shift (midnight to 8 am) (D); for delayed word recall accuracy by visit (E) and during the final visit night shift (midnight to 8 am) (F); for power of attention by visit (G) and during the final visit night shift (midnight to 8 am) (H); and for simple reaction time by visit (I) and during the final visit night shift (midnight to 8 am) (J) compared with placebo. Data presented over time are during the final visit night shift. Error bars indicate SEM. P values are based on the change from baseline compared with placebo. *P≤.001, †P≤.01, ‡P<.05.
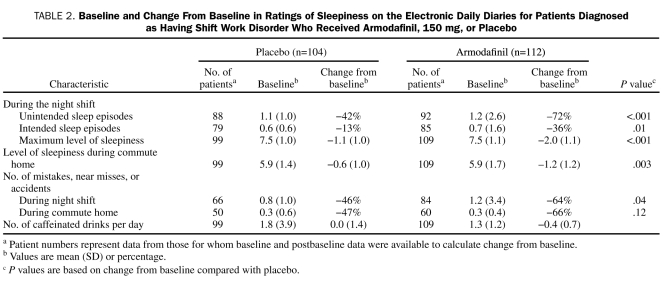
At the final visit, armodafinil was associated with significant improvement in most items assessed in the electronic diaries, including maximum level of sleepiness during the night shift and commute home and the mean number of mistakes, accidents, or near misses compared with placebo (Table 2).
TABLE 2.
Baseline and Change From Baseline in Ratings of Sleepiness on the Electronic Daily Diaries for Patients Diagnosed as Having Shift Work Disorder Who Received Armodafinil, 150 mg, or Placebo
Memory Assessments. Armodafinil significantly improved the mean score for the quality of episodic secondary memory factor compared with placebo at each visit (P<.001 at weeks 4 and 8; P=.002 at week 12; P<.001 at final visit; Figure 3, C) and during the first 4 tests on the final night shift (P=.002 at 12:30 am; P<.001 at 2:30 am; P=.02 at 4:30 am; P=.006 at 6:30 am; Figure 3, D). Within this factor score, armodafinil significantly improved the accuracy of delayed word recall compared with placebo at each visit (P=.02 at week 4; P=.006 at week 8; P=.02 at week 12 and at final visit; Figure 3, E) and during the first 2 tests on the final night shift (P<.001 at 12:30 am; P=.02 at 2:30 am; Figure 3, F).
The mean (SD) times for speed of memory were similar at baseline for armodafinil (2877.9 [666.5] milliseconds) and placebo (2914.0 [896.8] milliseconds). Armodafinil significantly improved speed of memory from baseline compared with placebo at week 8 (armodafinil, −240.9 milliseconds; placebo, −46.5 milliseconds; P=.02) and week 12 (armodafinil, −307.7 milliseconds; placebo, −115.2 milliseconds; P=.01), with a change at the final visit (armodafinil, −257.2 milliseconds; placebo, −140.4 milliseconds) that was not statistically significant (P=.09).
Attention Assessments. Armodafinil significantly improved mean power of attention from baseline at each study visit (P=.005 at week 4; P=.006 at week 8; P=.005 at week 12; P=.001 at final visit; Figure 3, G) and during the first 4 tests on the final night shift compared with placebo (P=.002 at 12:30 am; P=.006 at 2:30 am; P=.004 at 4:30 am; P=.03 at 6:30 am; Figure 3, H). Within this factor score, armodafinil significantly improved simple reaction time compared with placebo at all visits (P=.02 at week 4; P=.04 at week 8; P=.045 at week 12; P=.01 at final visit; Figure 3, I) and during the second and third tests on the final night shift (P=.02 at 2:30 am; P=.03 at 4:30 am) (Figure 3, J).
Continuity of attention improved at the final visit in patients who received armodafinil (increase in mean [SD] score, 2.9 [5.5] units) compared with those who received placebo (increase in mean [SD] score, 0.2 [5.7] units) (difference between groups in change from baseline, P<.001). The difference in change between the groups was significant at weeks 8 (P=.03) and 12 (P=.002).
Tolerability
The adverse events reported by 5% or more of patients who received armodafinil and reported more frequently than by patients who received placebo were headache (15/123 [12%] in the armodafinil group and 12/122 [10%] in the placebo group), nausea (9/123 [7%] in the armodafinil group and 4/122 [3%] in the placebo group), nasopharyngitis (7/123 [6%] in the armodafinil group and 4/122 [3%] in the placebo group), and anxiety (6/123 [5%] in the armodafinil group and 2/122 [2%] in the placebo group). Most adverse events were considered mild or moderate by the investigator. Severe adverse events, as determined by the site investigator, occurred more frequently in patients who took armodafinil (n=12) than in those who took placebo (n=3), with diarrhea (n=2) and low back pain (n=2) being the most common events in this category in the armodafinil group. Two serious adverse events were reported, 1 for the armodafinil group (suicidal ideation in a patient with a history of depression), which was considered by the investigator to be possibly related to the study medication, and 1 for the placebo group (viral meningitis), which was considered by the site investigator not to be related to study medication. No single adverse event led to withdrawal of more than 1 patient.
Changes from baseline to the final visit in mean laboratory parameters, mean vital signs, physical examination findings, and concomitant medication use were comparable for both groups, except for small increases in mean γ-glutamyltransferase values (mean [SD] change: armodafinil, 5.6 [30.8] U/L; placebo, 0.9 [7.5] U/L; P=.10) and a decrease in mean uric acid values (mean [SD] change: armodafinil, −4.38 [9.02] mg/L; placebo, −2.28 [10.33] mg/L; P=.10). The mean changes in laboratory parameters were not considered clinically meaningful, and the mean values remained within the reference ranges. Shifts in serum chemistry laboratory values from the reference range at baseline to values outside the reference range for at least 1 time point during the study occurred at comparable frequency in the armodafinil and placebo groups; none were considered clinically meaningful by the site investigators. For serum hematology laboratory values, slightly more shifts in lymphocyte and platelet values above the reference range were reported among patients who took armodafinil than among patients who received placebo, and there were slightly more shifts in neutrophil values below the reference range among patients who took armodafinil than among patients who received placebo. None of these changes were considered clinically meaningful by the site investigators.
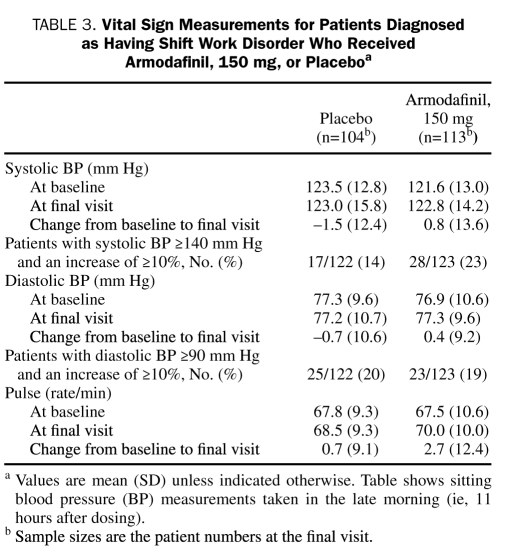
Differences in vital sign parameters were not statistically significant for measurements taken approximately 3 hours after dosing, approximately 11 hours after dosing (Table 3), or at 6:15 pm after the daytime polysomnogram at the final visit.
TABLE 3.
Vital Sign Measurements for Patients Diagnosed as Having Shift Work Disorder Who Received Armodafinil, 150 mg, or Placeboa
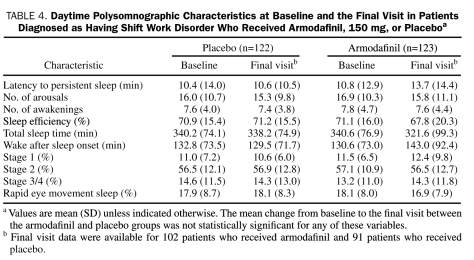
Armodafinil did not adversely affect daytime sleep variables (eg, sleep latency, sleep duration, and sleep-stage distribution) compared with placebo (Table 4). These findings were consistent with results from patient diaries.
TABLE 4.
Daytime Polysomnographic Characteristics at Baseline and the Final Visit in Patients Diagnosed as Having Shift Work Disorder Who Received Armodafinil, 150 mg, or Placeboa
DISCUSSION
Treatment with armodafinil, 150 mg, significantly reduced sleep propensity and subjective ratings of sleepiness and improved aspects of attention and memory in patients with SWD during usual night shift hours. These differences were associated with significantly greater improvement in the severity of patients' overall clinical condition compared with those who received placebo. Armodafinil increased nighttime mean sleep latency to greater than 5 minutes, although a proportion of individuals remained sleepy; patients who fall asleep in 5 minutes or less are often considered severely sleepy.26 This improvement was demonstrated at the first laboratory night shift and was sustained throughout the 12-week study. The findings confirm our hypothesis that armodafinil would significantly increase mean sleep latency and improve the overall clinical condition in patients with excessive sleepiness associated with SWD.
In a previous study in a similar population, modafinil, 200 mg, significantly improved overall mean nighttime sleep latency as measured by the MSLT by a mean of 1.7 minutes, with statistically significant increases in sleep latency vs placebo at the 2 and 4 am MSLT naps.16 In the current study, armodafinil, 150 mg, significantly improved the overall mean nighttime sleep latency as measured by the MSLT by a mean of 3.1 minutes at the final visit, with statistically significant increases in sleep latency at all 5 MSLT sessions from midnight to 8 am. A direct comparison study is necessary to compare the efficacy and safety of these agents.
The MSLT has also been used to assess sleepiness in other disorders for which excessive sleepiness is a cardinal symptom—narcolepsy and obstructive sleep apnea (OSA). The improvement in the mean sleep latency for patients with narcolepsy who received modafinil, 200 mg/d, for 9 weeks in a placebo-controlled clinical study was approximately 1.8 minutes vs baseline.27 A meta-analysis revealed that the summary estimate of improvement in mean sleep latency for patients with OSA who were successfully treated with nasal continuous positive airway pressure (nCPAP) was 0.74 minutes.28 Both modafinil and nCPAP are recognized as standard treatments for individuals with excessive sleepiness associated with narcolepsy29 or OSA,30 respectively, and the effects of these interventions on mean sleep latency have been shown to be associated with significantly improved health-related quality of life.31,32 Moreover, nCPAP treatment significantly reduces the elevated risk of motor vehicle crashes in patients with nontreated OSA.33,34 These findings suggest that an improvement in objective sleep latency comparable with that shown in the current study is sufficient to ameliorate the burden of illness and may be considered clinically relevant; our conclusion is similar to that reached in the meta-analysis mentioned herein, which showed a less than 1-minute mean improvement in objective sleep latency from nCPAP therapy in patients with OSA.28 Considering the nonlinear relationship between MSLT scores and sleepiness, a given numerical improvement in mean sleep latency at the low end of the scale is more clinically relevant than the same numerical improvement at the high end of the scale.35 The proportion of patients in the placebo group who were rated by the investigator as at least minimally improved on the CGI-C, the other coprimary outcome measure, was higher than what was anticipated and observed in a previous study16 of modafinil in patients with excessive sleepiness associated with SWD, for reasons that are not understood.
Excessive sleepiness impairs performance on various tasks, including those involving psychomotor performance or cognitive functions such as attention and memory.36-41 In the current study, attention was comprehensively enhanced as assessed by the CDR system with administration of armodafinil: the ability to both focus and sustain attention was improved compared with placebo, as shown by improvements in both speed and accuracy measures from an attention task (simple reaction time). Furthermore, armodafinil significantly improved long-term memory (quality of episodic secondary memory) and speed of memory compared with placebo, with significant improvements in the accuracy of delayed word recall. This improvement in accuracy was accompanied by an improvement in speed.
In the armodafinil group, reductions in patients' subjective ratings of sleepiness throughout the laboratory night shift were consistent with their ratings during actual work shifts and during the commute home. Furthermore, treatment with armodafinil was associated with significant reductions in reports of intended and unintended sleep episodes and mistakes, near misses, or accidents during the night shift. A similar magnitude of improvement was demonstrated for the commute home, although this effect was not statistically significant compared with placebo. Long-term, prospective studies of the impact of armodafinil on work performance and safety in patients with SWD are necessary to confirm the effects observed in the current 3-month trial.
Before treatment, our patients with SWD were severely sleepy, as shown by mean nocturnal sleep latencies of approximately 2 minutes, which are comparable to the latencies observed in patients with narcolepsy during the daytime.27 Patients with reports of excessive sleepiness associated with SWD are at substantially greater risk of impaired physical and mental well-being and performance.4 These risks constitute a public health concern. Untreated OSA and narcolepsy and working more than 24 consecutive hours42 can increase the risk of motor vehicle crashes.43,44 Patients diagnosed as having OSA are at a 2- to 7-fold greater risk of motor vehicle crashes,33 a risk that can be mitigated with appropriate treatment.33,34,45,46 Data from the health care field, which represented the largest segment of patients in the current study and is the largest and fastest growing industry in the United States, show that extended work shifts lasting more than 24 consecutive hours are also associated with increased risk of attentional failures, degraded performance, and increased risk of occupational accidents and serious fatigue-related medical errors and adverse events, resulting in patient injury and even death.42,47-50 Although the shift durations in these studies differ from those in the current study, SWD can increase the risk of attentional failures and degrade employee performance. To mitigate these risks, health care employers should implement fatigue management programs that include screening programs for the diagnosis and treatment of employees with SWD and other disorders of sleep and wakefulness.
Armodafinil was well tolerated and did not adversely affect scheduled daytime sleep. No clinically important effects on laboratory values, vital signs, polysomnograms, or electrocardiograms were seen. The current study did not find a statistically significant difference for armodafinil vs placebo in mean vital signs; increases in heart rate and blood pressure have been reported in other randomized, double-blind studies of the medication, although not consistently.51,52
Our study has several considerations that may limit the interpretation of data. Most patients enrolled were permanent night shift workers. This may limit the generalizability of these results to individuals working alternative shift schedules. This study was performed in SWD patients with both excessive sleepiness and insomnia, who may represent a more severely affected group; therefore, additional studies may be necessary to quantify the effects in a patient population with less severe SWD. The study did not include patients with SWD associated with starting work in the early morning. Although the prevalence of SWD is unknown in this population, approximately 3 times as many individuals work shifts that start in the early morning than night shifts. Further studies are necessary to determine whether these results are generalizable to those who start work in the early morning.
Although the effects of armodafinil were statistically significant and clinically relevant, a proportion of patients remained sleepy on objective assessment at the end of treatment. This finding suggests that armodafinil, 150 mg, is not equally effective in all patients and highlights the importance of ensuring that use of pharmacotherapy to enhance wakefulness is part of a comprehensive program that includes diagnostic screening for sleep disorders, education, and behavioral treatment interventions designed to optimize sleep and wakefulness. Recommended for industries such as the health care field, a comprehensive approach for SWD should address sleep and wake hygiene, strategic napping, appropriate time off between work periods, diet, exercise, appropriately timed light exposure to facilitate circadian adaptation, and work hour limits. Diagnosis and treatment of comorbid sleep disorders, such as OSA, narcolepsy, and restless legs syndrome, are important components of any comprehensive program for SWD.
CONCLUSION
Armodafinil, 150 mg, significantly improved measures of sleep propensity, subjective sleepiness, memory, and attention during scheduled night work hours in patients with excessive sleepiness associated with SWD without disturbing daytime sleep. The effects on wakefulness were apparent during the night shift and the commute home. Concurrent improvements in overall clinical condition were also found. Armodafinil was generally well tolerated. These findings support the inclusion of armodafinil as part of a comprehensive treatment program for excessive sleepiness associated with SWD.
Acknowledgments
We gratefully acknowledge Gwendolyn E. Niebler, DO, former Cephalon employee, for her contribution to the protocol design, role as medical monitor, and contribution to drafts of the manuscript; Rod J Hughes, PhD, former Cephalon employee, for contribution to the protocol design and drafts of the manuscript; Ronghua “Tiger” Yang, PhD, Cephalon employee, for statistical support during the submission and peer-review process; Mark Riotto, Cephalon employee, for editorial support; and Oxford PharmaGenesis Inc for editorial support on early drafts of the manuscript. The data analysis presented in this article was replicated independently by an academic clinical research group (Chalmers Research Group, CHEO RI, Ottawa, Ontario).
Footnotes
Cephalon Inc funded the study and developed the protocol in collaboration with the authors. For more information on the role of the funding source, see page 971, and for the financial disclosures of the authors, see page 969.
Participating Investigators
Investigators who participated in this study are as follows: Richard Bogan, MD, Columbia, SC; Gerald Burns, MD, Metairie, LA; Martin Cohn, MD, Naples, FL; James Cook, MD, Danville, IN; Bruce Corser, MD, Cincinnati, OH; Richard Marcus, MD, Hickory, NC; Karl Doghramji, MD, Philadelphia, PA; Cynthia Dorsey, PhD, Belmont, MA; Helene Emsellem, MD, Chevy Chase, MD; Milton Erman, MD, San Diego, CA; James Ferguson, MD, Salt Lake City, UT; Jonathan Flescher, MD, Raleigh, NC; Yury Furman, MD, Los Angeles, CA; Paul Haberman, MD, Santa Monica, CA; Barbara Harris, PhD, Scottsdale, AZ; Dennis Hill, MD, Salisbury, NC; Max Hirshkowitz, PhD, Houston, TX; John Hudson, MD, Austin, TX; Steven Hull, MD, Overland Park, KS; David Laman, MD, Pittsburgh, PA; D. Alan Lankford, PhD, Atlanta, GA; Jed Black, MD, Stanford, CA; Michael Neeb, PhD, Toledo, OH; Vernon Pegram, PhD, Birmingham, AL; Richard Pellegrino, MD, Hot Springs, AK; John Pinto, MD, Las Vegas, NV; Russell Rosenberg, PhD, Atlanta, GA; Murray Rosenthal, DO, San Diego, CA; Markus Schmidt, MD, Dublin, OH; J. Baldwin Smith III, MD, Winston-Salem, NC; James Ware, PhD, Norfolk, VA; Kenneth Wright, PhD, Boulder, CO; James Wyatt, PhD, Chicago, IL; Gary Zammit, PhD, New York, NY; Henry Lahmeyer, MD, Northfield, IL; Siriwan Kriengkairut, MD, Bismarck, ND; William Leeds, DO, Topeka, KS; Francisco Candal, MD, Slidell, LA; Derek Loewy, MD, Tucson, AZ; Michael Alexander, MD, Niagara Falls, Ontario, Canada; Leonid Kayumov, PhD, Scarborough, Ontario, Canada; Mortimer Mamelak, MD, Toronto, Ontario, Canada; Adam Moscovitch, MD, Calgary, Alberta, Canada; Colin Shapiro, MD, Toronto, Ontario, Canada; Nick Antic, MD, Daw Park, Adelaide, South Australia, Australia.
Financial Disclosures
Dr Czeisler has received consulting fees from or served as a paid member of scientific advisory boards for Actelion Ltd, Avera Pharmaceuticals Inc, Cephalon Inc, Delta Airlines, Eli Lilly and Co, Fedex Kinko's, Federal Motor Carrier Safety Administration, US Department of Transportation, Fusion Medical Education LLC, Garda Siochana Inspectorate (Dublin, Ireland), Global Ground Support, Hypnion Inc (acquired by Eli Lilly and Co in April 2007), Johnson & Johnson, Koninklijke Philips Electronics NV, Morgan Stanley, Sanofi-Aventis Groupe, Portland Trailblazers, Respironics Inc, Sepracor Inc, Sleep Multimedia Inc, Sleep Research Society, Somnus Therapeutics Inc, Takeda Pharmaceuticals, Vanda Pharmaceuticals Inc, Vital Issues in Medicine, Warburg-Pincus and Zeo; owns an equity interest in Lifetrac Inc, Somnus Therapeutics Inc, Vanda Pharmaceuticals Inc, and Zeo Inc and receives royalties from McGraw Hill and Penguin Press; has received lecture fees from the Accreditation Council of Graduate Medical Education; Alfresa; American Academy of Allergy, Asthma and Immunology Program Directors; American Physiological Society; Association of University Anesthesiologists; Baylor College of Medicine; Beth-Israel Deaconess Medical Center; Brown Medical School/Rhode Island Hospital; Cephalon Inc; Clinical Excellence Commission (Australia); Dalhousie University; Duke University Medical Center; Harvard University; Institute of Sleep Health Promotion (NPO); London Deanery; Morehouse School of Medicine; Mount Sinai School of Medicine; National Emergency Training Center; National Institutes of Health; North East Sleep Society; Osaka University School of Medicine; Partners HealthCare Inc; Sanofi-Aventis Inc; St. Lukes Roosevelt Hospital; Takeda; Tanabe Seiyaku Co Ltd; Tokyo Electric Power Company; University of Michigan; University of Pennsylvania; University of Pittsburgh; University of Tsukuba; University of Virginia Medical School; University of Wisconsin Medical School; World Federation of Sleep Research and Sleep Medicine Societies; and has received research prizes with monetary awards from the American Academy of Sleep Medicine; American Clinical and Climatological Association; Association for Patient-Oriented Research; Sleep Research Society; National Institute for Occupational Safety and Health and National Sleep Foundation; clinical trial research contracts from Cephalon Inc, Merck & Co Inc, and Pfizer Inc; and an investigator-initiated research grant from Cephalon Inc. Dr Czeisler is the incumbent of an endowed professorship provided to Harvard University by Cephalon Inc and holds a number of process patents in the field of sleep/circadian rhythms (eg, photic resetting of the human circadian pacemaker). Since 1985, Dr Czeisler has served as an expert witness on various legal cases related to sleep and/or circadian rhythms.
Dr Czeisler's research laboratory at the Brigham and Women's Hospital has received unrestricted research and education funds and/or support for research expenses from Cephalon Inc, Koninklijke Philips Electronics NV, ResMed, and the Brigham and Women's Hospital. The Harvard Medical School Division of Sleep Medicine (HMS/DSM), which he directs, has received unrestricted research and educational gifts and endowment funds from Boehringer Ingelheim Pharmaceuticals Inc, Cephalon Inc, George H. Kidder, Esq, Gerald McGinnis, GlaxoSmithKline, Herbert Lee, Hypnion, Jazz Pharmaceuticals, Jordan's Furniture, Merck & Co Inc, Peter C. Farrell, PhD, Pfizer, ResMed, Respironics Inc, Sanofi-Aventis Inc, Sealy Inc, Sepracor Inc, Simmons, Sleep Health Centers LLC, Spring Aire, Takeda Pharmaceuticals, and Tempur-Pedic; the HMS/DSM has received gifts from many organizations and individuals, including Aetna US Healthcare, Alertness Solutions Inc, American Academy of Sleep Medicine, Axon Sleep Research Laboratories Inc, Boehringer Ingelheim Pharmaceuticals Inc, Department of Medicine at Brigham & Women's Hospital, Bristol-Myers Squibb, Catalyst Group, Cephalon Inc, Clarus Ventures, Comfortaire Corporation, Committee for Interns and Residents, Eli Lilly and Co, Farrell Family Foundation, Fisher & Paykel Healthcare Corporation, George H. Kidder, Esq, GlaxoSmithKline, Gosule, Butkus & Jesson, LLP, Hypnion Inc, Innovative Brands Group (Nature's Rest), Jordan's Furniture, King Koil Sleep Products, Land and Sky, Merck Research Laboratories, MPM Capital, Neurocrine Biosciences Inc, Orphan Medical/Jazz Pharmaceuticals, Park Place Corporation, Pfizer Global Pharmaceuticals, Pfizer Healthcare Division, Purdue Pharma LP, PR21, ResMed Inc, Respironics Inc, Sanofi-Aventis Inc, Sanofi-Synthelabo, Sealy Mattress Company, Sealy Inc, Select Comfort Corporation, Sepracor Inc, Simmons Co, Sleep Ave LLC, SleepCare LLC, Sleep HealthCenters LLC, Spring Air Mattress Co, Takeda Pharmaceuticals, Tempur-Pedic Medical Division, Total Sleep Holdings, Vanda Pharmaceuticals Inc, and the Zeno Group; and the HMS/DSM Sleep and Health Education Program has received educational grant funding from Cephalon Inc, Takeda Pharmaceuticals, Sanofi-Aventis Inc, and Sepracor Inc.
Dr Walsh reports that research support has been provided to his institution by the following companies: Ancile Pharmaceuticals, Bristol-Myers Squibb, Cephalon Inc, Evotec Neurosciences, Jazz Pharmaceuticals, Lorex Pharmaceuticals, Lundbeck A/S, Merck & Co, Neurocrine Biosciences, Orphan Medical, Pfizer Inc, Sanofi-Synthelabo, Searle Pharmaceuticals, Sepracor, Somaxon, Takeda America, Ventus, and Wyeth-Ayerst Research. Dr Walsh has provided consulting services to the following companies: Abbott Laboratories, Actelion, Alza Corp, Ancile Pharmaceuticals, Aventis, Bristol-Myers Squibb, Cephalon Inc, CoCensys Pharmaceuticals, Elan Pharmaceuticals, Eli Lilly, Evotec Neurosciences, GlaxoSmithKline, Guilford, Jazz Pharmaceuticals, King Pharmaceuticals, Lorex Pharmaceuticals, Lundbeck A/S, Merck & Co, Merck KgaA-Darmstadt, Neurocrine Biosciences, Neurogen, Organon, Pfizer Inc, Respironics, Restiva Pharmaceuticals, Sanofi-Aventis, Sanofi-Synthelabo, Searle Pharmaceuticals, Sepracor, Serentis, SleepTech, Somaxon, Takeda America, TransOral, and Ventus; has received honoraria for medical education activities from Searle Pharmaceuticals, Cephalon Inc, Sanofi-Synthelabo, Elan Pharmaceuticals, and Pfizer Inc.
Dr Roth has received grants from Aventis, Cephalon, GlaxoSmithKline, Merck, Neurocrine, Pfizer, Sanofi, Schering-Plough, Sepracor, Somaxon, Syrex, Takeda, TransOral, Wyeth, and Xenoport; and has been a consultant to Abbott, ACADIA, Acoglix, Acorda, Addrenex, Actelion, Alchemers, Alza, Ancel, Arena, AstraZeneca, Aventis, AVER, Bayer, Bristol-Myers Squibb, BTG, Cephalon, Cypress, Dove, Eisai, Elan, Eli Lilly, Evotec, Forest, GlaxoSmithKline, Hypnion, IMPAX, Intec, Intra-Cellular Therapies, Jazz, Johnson & Johnson, King, Lundbeck, McNeil, MediciNova, Merck, Neurim, Neurocrine, Neurogen, Novartis, Orexo, Organon, Otsuka, Pfizer, Prestwick, Procter & Gamble, Purdue, Resteva, Roche, Sanofi, Schering-Plough, Sepracor, Servier, Shire, Somaxon, Syrex, Takeda, TransOral, Vanda, Vivometrics, Wyeth, Yamanuchi, Xenoport. Dr Roth has served on the speakers' bureau for Cephalon and Sanofi.
Dr Wesnes is the sole shareholder of Cognitive Drug Research Ltd, which was contracted by Cephalon to provide the cognitive testing system used in this study. Cognitive Drug Research Ltd conducts research for the worldwide pharmaceutical industry and in the last 7 years has worked for the world's largest 17 pharmaceutical companies and numerous other companies. Since 2001 (3 years before the start of this study), Dr Wesnes had been a paid consultant to Eisai, Pharmaton SA, Cephalon, Merck & Co Inc, Novartis, and Roche. He owns no shares or stocks in any pharmaceutical company or other company that may result in any conflict of interest.
Role of the Funding Source
All involved parties were responsible for conducting the study in compliance with the Good Clinical Practice Consolidated Guidance. Cephalon Inc funded the study and developed the protocol in collaboration with the authors. The sponsor was responsible for conduct of the study, including but not limited to selection of qualified investigators, quality control, independent review board approval, protection of human subjects and informed consent, data collection and management, adverse event reporting, and regulatory reporting. A qualified statistician (S.A.) employed by the study sponsor conducted the statistical analysis of the data. The data analysis presented in this article was also replicated independently by an academic clinical research group (Chalmers Research Group, CHEO RI, Ottawa, Ontario, Canada). Operational management of the study was performed by Covance Inc (Princeton, NJ) and Clinical Trial Services (Audubon, PA) under the direction of the sponsor, and all responsibility for the quality and integrity of the trial data resided with the sponsor. All authors had a lead role in designing the study, developing the protocol, interpreting the data, and writing the manuscript. Authors attended investigator meetings and trained individual site investigators. Lead investigators at each study site were responsible for obtaining informed consent, adherence to the protocol, patient safety, and data collection. All authors had full access to the data and contributed to data interpretation and preparation of this report. The corresponding author had final responsibility for the decision to submit for publication.
REFERENCES
- 1.Bureau of Labor Statistics Workers on Flexible and Shift Schedules in 2004 Summary. http://www.bls.gov/news.release/flex.nr0.htm. http://www.bls.gov/news.release/flex.nr0.htm Accessed August 25, 2009.
- 2.Åkerstedt T. Shift work and disturbed sleep/wakefulness. Occup Med (Lond) 2003;53(2):89-94 [DOI] [PubMed] [Google Scholar]
- 3.Richardson GS, Malin HV. Circadian rhythm sleep disorders: pathophysiology and treatment. J Clin Neurophysiol. 1996;13(1):17-31 [DOI] [PubMed] [Google Scholar]
- 4.Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep 2004;27(8):1453-1462 [DOI] [PubMed] [Google Scholar]
- 5.Torsvall L, Åkerstedt T, Gillander K, Knutsson A. Sleep on the night shift: 24-hour EEG monitoring of spontaneous sleep/wake behavior. Psychophysiology 1989;26(3):352-358 [DOI] [PubMed] [Google Scholar]
- 6.Åkerstedt T. Shift work and sleep disorders [editorial]. Sleep 2005;28(1):9-11 [PubMed] [Google Scholar]
- 7.American Academy of Sleep Medicine The International Classification of Sleep Disorders: Diagnostic and Coding Manual 2nd ed.Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 8.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR 4th ed.Text revision Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 9.Gold DR, Rogacz S, Bock N, et al. Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. Am J Public Health 1992;82(7):1011-1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitler MM, Miller JC, Lipsitz JJ, Walsh JK, Wylie CD. The sleep of long-haul truck drivers. N Engl J Med. 1997;337(11):755-761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knutsson A. Health disorders of shift workers. Occup Med (Lond) 2003;53(2):103-108 [DOI] [PubMed] [Google Scholar]
- 12.Ohayon MM, Lemoine P, Arnaud-Briant V, Dreyfus M. Prevalence and consequences of sleep disorders in a shift worker population. J Psychosom Res. 2002;53(1):577-583 [DOI] [PubMed] [Google Scholar]
- 13.Segawa K, Nakazawa S, Tsukamoto Y, et al. Peptic ulcer is prevalent among shift workers. Dig Dis Sci. 1987;32(5):449-453 [DOI] [PubMed] [Google Scholar]
- 14.Akerstedt T. Work hours, sleepiness and accidents: introduction and summary. J Sleep Res. 1995;4(suppl 2):1-3 [DOI] [PubMed] [Google Scholar]
- 15.Smith L, Folkard S, Poole CJ. Increased injuries on night shift. Lancet 1994;344(8930):1137-1139 [DOI] [PubMed] [Google Scholar]
- 16.Czeisler CA, Walsh JK, Roth T, et al. U.S. Modafinil in Shift Work Sleep Disorder Study Group Modafinil for excessive sleepiness associated with shift-work sleep disorder [published correction appears in N Engl J Med. 2005;353(10):1078] N Engl J Med. 2005;353(5):476-486 [DOI] [PubMed] [Google Scholar]
- 17.Dinges DF, Arora S, Darwish M, Niebler GE. Pharmacodynamic effects on alertness of single doses of armodafinil in healthy subjects during a nocturnal period of acute sleep loss. Curr Med Res Opin. 2006;22(1):159-167 [DOI] [PubMed] [Google Scholar]
- 18.Guy W. ECDEU Assessment Manual for Psychopharmacology Revised, 1976 Rockville, MD: US Dept of Health and Human Services; 1976. [Google Scholar]
- 19.Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S. Guidelines for the multiple sleep latency test (MSLT): a standard measure of sleepiness. Sleep 1986;9(4):519-524 [DOI] [PubMed] [Google Scholar]
- 20.Rechtschaffen A, Kales A, eds. A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects Vol Publication 204 Washington, DC: National Institutes of Health; 1968. [Google Scholar]
- 21.Mitler MM, Carskadon MA, Hirshkowitz M. Evaluating sleepiness. In: Kryger MH, Roth T, Dement WC, eds. Principles and Practice of Sleep Medicine 4th ed.Philadelphia, PA: Elsevier Saunders; 2005:1417-1423 [Google Scholar]
- 22.Gillberg M, Kecklund G, Akerstedt T. Relations between performance and subjective ratings of sleepiness during a night awake. Sleep 1994;17(3):236-241 [DOI] [PubMed] [Google Scholar]
- 23.Keith MS, Stanislav SW, Wesnes KA. Validity of a cognitive computerized assessment system in brain-injured patients. Brain Inj 1998;12(12):1037-1043 [DOI] [PubMed] [Google Scholar]
- 24.Wesnes KA, McKeith IG, Ferrara R, et al. Effects of rivastigmine on cognitive function in dementia with Lewy bodies: a randomised placebo-controlled international study using the Cognitive Drug Research computerised assessment system. Dement Geriatr Cogn Disord. 2002;13(3):183-192 [DOI] [PubMed] [Google Scholar]
- 25.Wesnes KA, Ward T, McGinty A, Petrini O. The memory enhancing effects of a Ginkgo biloba/Panax ginseng combination in healthy middle-aged volunteers. Psychopharmacology (Berl) 2000;152(4):353-361 [DOI] [PubMed] [Google Scholar]
- 26.Arand D, Bonnet M, Hurwitz T, Mitler M, Rosa R, Sangal RB. The clinical use of the MSLT and MWT. Sleep 2005;28(1):123-144 [DOI] [PubMed] [Google Scholar]
- 27.Modafinil US in Narcolepsy Multicenter Study Group Randomized trial of modafinil for the treatment of pathological somnolence in narcolepsy. Ann Neurol. 1998;43(1):88-97 [DOI] [PubMed] [Google Scholar]
- 28.Patel SR, White DP, Malhotra A, Stanchina ML, Ayas NT. Continuous positive airway pressure therapy for treating sleepiness in a diverse population with obstructive sleep apnea: results of a meta-analysis. Arch Intern Med. 2003;163(5):565-571 [DOI] [PubMed] [Google Scholar]
- 29.Littner M, Johnson SF, McCall WV, et al. Standards of Practice Committee Practice parameters for the treatment of narcolepsy: an update for 2000. Sleep 2001;24(4):451-466 [PubMed] [Google Scholar]
- 30.Kushida CA, Littner MR, Hirshkowitz M, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 2006;29(3):375-380 [DOI] [PubMed] [Google Scholar]
- 31.Beusterien KM, Rogers AE, Walsleben JA, et al. Health-related quality of life effects of modafinil for treatment of narcolepsy. Sleep 1999;22(6):757-765 [DOI] [PubMed] [Google Scholar]
- 32.Siccoli MM, Pepperell JC, Kohler M, Craig SE, Davies RJ, Stradling JR. Effects of continuous positive airway pressure on quality of life in patients with moderate to severe obstructive sleep apnea: data from a randomized controlled trial. Sleep 2008;31(11):1551-1558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sassani A, Findley LJ, Kryger M, Goldlust E, George C, Davidson TM. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep 2004;27(3):453-458 [DOI] [PubMed] [Google Scholar]
- 34.Douglas NJ, Engleman HM. Effects of CPAP on vigilance and related functions in patients with the sleep apnea/hypopnea syndrome. Sleep 2000;23(suppl 4):S147-S149 [PubMed] [Google Scholar]
- 35.Punjabi NM, Bandeen-Roche K, Young T. Predictors of objective sleep tendency in the general population. Sleep 2003;26(6):678-683 [DOI] [PubMed] [Google Scholar]
- 36.Durmer J, Dinges D. Neurocognitive consequences of sleep deprivation. Semin Neurol. 2005;25(1):117-129 [DOI] [PubMed] [Google Scholar]
- 37.Dawson D, Reid K. Fatigue, alcohol and performance impairment [letter]. Nature 1997;388(6639):235 [DOI] [PubMed] [Google Scholar]
- 38.Pilcher JJ, Huffcutt AI. Effects of sleep deprivation on performance: a meta-analysis. Sleep 1996;19(4):318-326 [DOI] [PubMed] [Google Scholar]
- 39.Roehrs T, Greenwald M, Roth T. Risk-taking behavior: effects of ethanol, caffeine, and basal sleepiness. Sleep 2004;27(5):887-893 [DOI] [PubMed] [Google Scholar]
- 40.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation [published correction appears in Sleep. 2004;27(4):600] Sleep 2003;26(2):117-126 [DOI] [PubMed] [Google Scholar]
- 41.Dinges DF, Pack F, Williams K, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night. Sleep 1997;20(4):267-277 [PubMed] [Google Scholar]
- 42.Barger LK, Cade BE, Ayas NT, et al. Harvard Work Hours, Health, and Safety Group Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352(2):125-134 [DOI] [PubMed] [Google Scholar]
- 43.Findley L, Unverzagt M, Guchu R, Fabrizio M, Buckner J, Suratt P. Vigilance and automobile accidents in patients with sleep apnea or narcolepsy. Chest 1995;108(3):619-624 [DOI] [PubMed] [Google Scholar]
- 44.Aldrich MS. Automobile accidents in patients with sleep disorders. Sleep 1989;12(6):487-494 [DOI] [PubMed] [Google Scholar]
- 45.Engleman HM, Asgari-Jirhandeh N, McLeod AL, Ramsay CF, Deary IJ, Douglas NJ. Self-reported use of CPAP and benefits of CPAP therapy: a patient survey. Chest 1996;109(6):1470-1476 [DOI] [PubMed] [Google Scholar]
- 46.Krieger J, Meslier N, Lebrun T, et al. Accidents in obstructive sleep apnea patients treated with nasal continuous positive airway pressure: a prospective study. Chest 1997;112(6):1561-1566 [DOI] [PubMed] [Google Scholar]
- 47.Ayas NT, Barger LK, Cade BE, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA 2006;296(9):1055-1062 [DOI] [PubMed] [Google Scholar]
- 48.Barger LK, Ayas NT, Cade BE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006;3(12):e487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351(18):1838-1848 [DOI] [PubMed] [Google Scholar]
- 50.Lockley SW, Cronin JW, Evans EE, et al. Harvard Work Hours, Health, and Safety Group Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351(18):1829-1837 [DOI] [PubMed] [Google Scholar]
- 51.Harsh JR, Hayduk R, Rosenberg R, et al. The efficacy and safety of armodafinil as treatment for adults with excessive sleepiness associated with narcolepsy. Curr Med Res Opin. 2006;22(4):761-774 [DOI] [PubMed] [Google Scholar]
- 52.Roth T, White D, Schmidt-Nowara W, et al. Effects of armodafinil in the treatment of residual excessive sleepiness associated with obstructive sleep apnea/hypopnea syndrome: a 12-week, multicenter, double-blind, randomized, placebo-controlled study in nCPAP-adherent adults. Clin Ther. 2006;28(5):689-706 [DOI] [PubMed] [Google Scholar]