The authors surveyed lymphomas to determine the range of expression of the mantle cell lymphoma- associated SOX11 transcription factor and its relation to cyclin D1. In addition to mantle cell lymphoma, SOX11 was strongly expressed only in lymphoblastic malignancies and Burkitt’s lymphomas, and its expression was independent of cyclin D1. See related perspective article on page 1488.
Keywords: lymphoid, SOX11 transcription factors, lymphoblastic neoplasms, mantle cell lymphoma, Burkitt’s lymphoma
Abstract
Background
We surveyed lymphomas to determine the range of expression of the mantle cell lymphoma-associated SOX11 transcription factor and its relation to cyclin D1.
Design and Methods
On hundred and seventy-two specimens were immunostained for the SOX11 N and C termini. Cyclin D1 was detected by immunohistochemistry and quantitative reverse transcriptase polymerase chain reaction; in situ hybridization for t(11;14) was applied when needed.
Results
Nuclear SOX11 was strongly expressed in most B and T-lymphoblastic leukemia/lymphomas and half of childhood Burkitt’s lymphomas, but only weakly expressed in some hairy cell leukemias. Chronic lymphocytic leukemia/lymphoma, marginal zone, follicular and diffuse large B-cell lymphomas were negative for SOX11, as were all cases of intermediate Burkitt’s lymphomas/diffuse large B-cell lymphoma, myeloma, Hodgkin’s lymphomas and mature T-cell and NK/T-cell lymphomas.
Conclusions
In addition to mantle cell lymphoma, SOX11 is strongly expressed only in lymphoblastic malignancies and Burkitt’s lymphomas. Its expression is independent of cyclin D1 (except for weak expression in hairy cell leukemias) and unlikely to be due to translocations in lymphoid neoplasia.
Introduction
The SOX11 transcription factor, normally expressed in the developing central nervous system, is aberrantly transcribed and expressed in mantle cell lymphoma (MCL)1 and has been suggested to correlate with overall survival.2 Common MCL simulators do not express nuclear SOX11 but questions remain as to its relation to cyclin D1 (CCND1) and whether SOX11 is restricted to MCL. We surveyed most categories of B- and T-cell lymphomas for SOX11, including plasmacytoma/myeloma3 and hairy cell leukemia, which are characterized by elevated levels of CCND1.4–6
Design and Methods
Current World Health Organization (WHO) clinical, histological and immunophenotypic criteria7 were used to diagnose 172 previously unreported cases of lymphoma on formalin-fixed paraffin sections, with or without ancillary flow cytometric and molecular studies. All biological material was used according to the research ethics principles established for our institution. The samples came from patients aged less than 1 year old to 89 years old. The male: female ratio was 1.7:1.
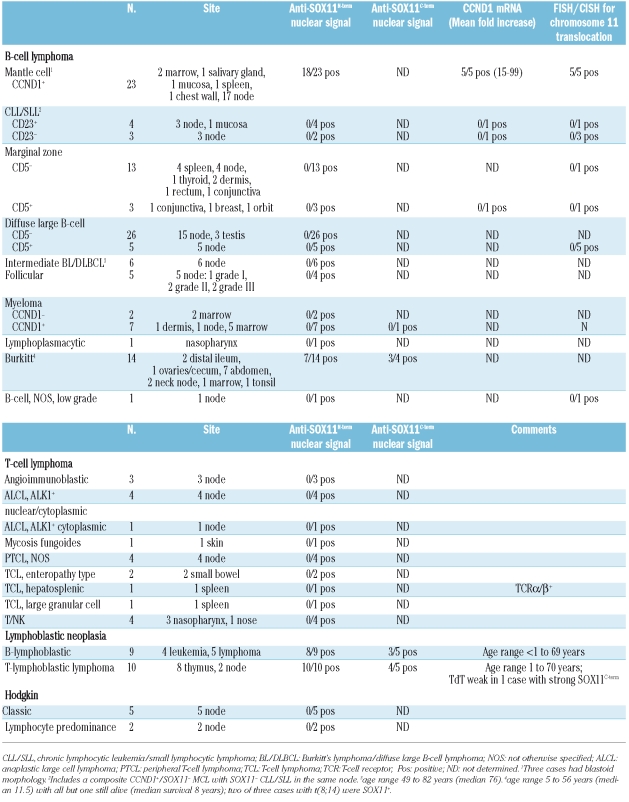
B-cell lymphoma, T-cell lymphoma, NK/T-cell lymphoma and Hodgkin’s lymphoma comprised mature (peripheral) lymphomas and B/T lymphoblastic leukemia/lymphoma comprised the immature category (Table 1). CD5+ B-cell lymphomas comprise subgroups within recognized lymphoma entities. Burkitt’s lymphoma was distinguished by typical starry-sky and nuclear morphology, predominantly intra-abominal origin, a Ki-67 index greater than 95% and consistent CD10+ and BCL2− staining.7 Intermediate Burkitt’s lymphoma/diffuse large B-cell lymphoma had a similar proliferation index and starry-sky pattern but were largely nodal and showed nuclear, cellular and immunophenotypic features (strong BCL2+ or CD10− in all cases) inconsistent with Burkitt’s lymphoma.
Table 1.
Lymphoid neoplasias studied for nuclear SOX11 expression.
Immunohistochemistry
Sections were microwaved for antigen retrieval in Tris/EDTA, pH 9, for 8+7 min and then stained on an automatic immunostainer using SOX11 antibodies, as detailed below and, as needed, a rabbit monoclonal anti-CCND1 antibody (1:70, NeoMarkers, USA). Signals were detected using Envision (Dako) and 3, 3′-diaminobenzidine.
Characterization of SOX11 antibodies
Two primary rabbit anti-human SOX11 antibodies were raised by the HPR-project.8,9 The first, SOX11N-term, targets the N-terminus of SOX11 and was used successfully in MCL.1 The immunogen shows some homology with SOX4 but SOX11N-term shows no nuclear reactivity in tonsil sections, known to express SOX4.
SOX11C-term was raised against the immunogen EDDDDDDDDDELQLQIKQEPDEEDEEPPHQQLLQPPGQQPSQLLRRYNVAKVPASPTLSSSAESPEGASLYDEVRAGATSGAGGGSRLYYSFKNITKQHPPPLAQPALSPASSRSVSTSSS, a 121 amino acid carboxy terminal peptide, specific for SOX11. The specificity of both antibodies was verified in the MCL cell lines, SP53 and Granta-519, using a western blot of extracted proteins, which were separated by reducing sodium dodecyl sulphate polyacrylamide gel electrophoresis (SDS-PAGE) (NuPAGE 10% Bis-Tris gels, Invitrogen, CA, USA). Each well was loaded with lysate from approximately 6×105 cells and the gel was blotted onto a PVDF membrane (Amersham Hybond-P, GE Healthcare, Sweden) for 30 min (15 V) and blocked overnight in 5% milk/phosphate-buffered saline (PBS). SOX11N-term or SOX11C-term was applied diluted 1:500 for 30 min. After washing with PBS a horseradish peroxidase (HRP)-labeled goat anti-rabbit antibody, diluted 1:10,000 was applied. Bands were detected with SuperSignal West Femto Max Sensitivity Substrate (Pierce) according to the manufacturer’s protocol.
Short interfering RNA knockdown study
Washed Granta-519 cells were suspended in 100 μL nucleofector solution (Reactionlab, Sweden) at 5×106 cells/sample. Each cuvette was then loaded with 50 pmol of small interfering RNA (siRNA) (Ambion, Austin, USA) consisting of antisense SOX11.1 [pool] UAACGUACCAACAUACUUGuu, UGCGUCACG ACAUCUUAUCuu, UCUUCGAGGAGCCUAGAGGuu and AGACCGACAAGCUUCAAACuu (or controls using complementary sense oligoRNA), transfected (Amaxa Biosystems, Germany), then incubated in R-10 medium at 37°C for 3 h, plated at a density of 0.50–0.75×106 cells/mL and grown for 2–3 days.
Quantitative real-time polymerase chain reaction
Briefly, reverse transcribed RNA template was used in a fluorogenic 5′ nuclease assay to determine CT values on a Rotorgene cycler (Corbett Research). Primers and probes for CCND1 and the reference gene TBP and cycling conditions have been published previously.10 Each sample was run in triplicate with Granta-519 cDNA as a positive control, one negative water control and two no template controls using DNase I-treated RNA.
Gene expressions were calculated to determine the fold increase in normalized CCND1 CT values relative to a benign node calibrator using the appropriate formulae.11
Interphase fluorescent in situ hybridization and chromogenic in situ hybridization
We isolated whole nuclei from thick sections digested in 0.5% pepsin. Filtered nuclei were spread on a glass slide, after-fixed in Carnoy’s fixative, pre-hybridized in 0.1% Triton-100, digested in 0.3 mg/mL pronase, rinsed in glycine/PBS, dehydrated in ethanol and air-dried. A dual-color, dual-fusion translocation probe (Vysis, USA) was hybridized as previously reported.1 Yellow fusion signals are evidence of t(11;14). For each specimen 50 nuclei were scored for the number of fusion signals using the cut-off value of six, which was based on fusion counts in 350 total nuclei from benign nodes and follicular lymphoma.
Chromogenic in situ hybridization (CISH), was performed according to the manufacturer’s protocol using a mixture of Texas Red- and fluorescein isothiocyanate (FITC)-labeled probes (Dako DuoCISH™) which target sequences flanking the CCND1 locus. Overlapping blue and red signals indicate co-localization and a split signal indicates a break at the CCND1 locus. Several MCL were used as positive controls.
Results
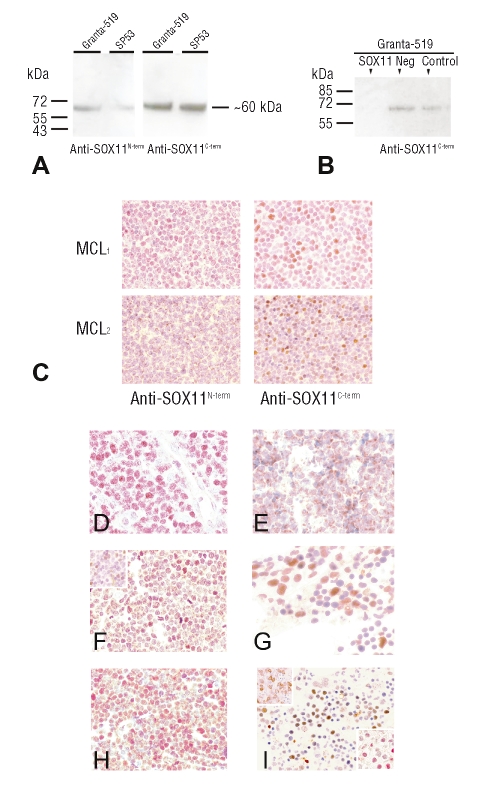
Both antibodies yielded an approximately 60 kDa band on western blots, corresponding to SOX11 (Figure 1A); after SOX11 knock-down the band was not detectable using SOX11C-term (Figure 1B). Nineteen MCL in the original report1 were reanalyzed with SOX11C-term and results between the two antibodies were concordant to a high degree apart from occasional differences in staining intensity: one case remained negative with both antibodies, one converted to being positive (Figure 1C) and two became immunonegative. Cytoplasmic staining1 appeared to be reciprocally related to nuclear intensity for both antibodies and was not scored. Of 23 new MCL specimens, 19 (83%) expressed nuclear SOX11. Five of the 23 specimens were studied with molecular techniques and showed 15 to 99-fold increases in CCND1 expression and between 14 and 72% of nuclei with fluorescent in situ hybridization (FISH) fusion signals, confirming the presence of t(11;14). No consistent relation between CCND1 staining intensity, CCND1 transcription level and the intensity of SOX11 staining was apparent. For example, two MCL showing 22 and 34-fold increases of CCND1 mRNA lacked nuclear SOX11 protein.
Figure 1.
(A) A Western blot of proteins extracted from two MCL cell lines showing bands of approximately 60 kDa for SOX11 using either anti-SOX11 antibody. (B) The lane labeled SOX11 denotes Granta-519 cell extract after knock-down with specific siRNA and staining with anti-SOX11C-term, which yielded no band, in contrast to the SOX11 bands noted in negative and control lanes; these lanes contain extracts after nucleofection with scrambled sequence siRNA and untransfected cells, respectively. (C) A case of MCL (MCL1) with weak nuclear signals after applying SOX11N-term showed stronger signals using SOX11C-term. Another case of MCL (MCL2) showed only cytoplasmic signals until immunoreacted with SOX11C-term, after which nuclear signals appeared (DAB with hematoxylin counterstain, Olympus BX45, magnification x125, colors corrected after acquisition with Adobe Photoshop). (D) Strong nuclear SOX11 signals after staining with anti-SOX11C-term is seen in a true Burkitt’s lymphoma. (E) Intermediate Burkitt’s lymphoma/diffuse large B-cell lymphoma shows no nuclear stain (signal is limited to cytoplasm). (F) Positive nuclear staining in lymphoblastic neoplasia is exemplified by a case of adult nodal T-cell lymphoblastic lymphoma (inset, TdT stain). (G) Signals are present in the bone marrow from a patient with B-cell acute lymphoblastic leukemia. (H) A case of childhood orbital B-cell lymphoblastic lymphoma also expresses SOX11. (I) Bone marrow in hairy cell leukemia, case 9, expressing DBA.44 (inset, upper left), CCND1 (inset, lower right) and SOX11 detected with anti-SOX11C-term (DAB with hematoxylin counterstain, magnification x125, except D, x230,).
Both SOX11 and molecular analysis could differentiate CD5+ simulators from MCL (Table 1). Despite a lack of CCND1, there were challenges in distinguishing 29 cases of CD5+ non-MCL, including cases of marginal zone lymphoma, CD23− chronic lymphocytic leukemia/small lymphocytic lymphoma, CD5+ diffuse large B-cell lymphoma and B-cell lymphoma not otherwise specified, from MCL. Twelve of these were analyzed further and all were negative for t(11;14) by FISH and/or had normal levels of CCND1 transcription. All 12 cases were also immunonegative for nuclear SOX11, whereas all six CCND1+ MCL tested with molecular techniques expressed SOX11. As expected, other typical cases of chronic lymphocytic leukemia/small lymphocytic lymphoma and follicular, mantle zone and diffuse large B-cell lymphomas also lacked SOX11 in the nuclei. Hodgkin’s lymphoma and T-cell lymphoma subtypes, including NK/T-cell lymphoma, were similarly negative. Most tumors in all categories which lacked nuclear SOX11 showed variably intense cytoplasmic signals, as previously reported.1
Unexpectedly, we found strong nuclear SOX11 staining in both childhood Burkitt’s lymphoma and acute lymphoblastic leukemia/lymphoma, regardless of phenotype (B- or T-cell). Seven of fourteen cases of Burkitt’s lymphoma were positive and this was reconfirmed with SOX11C-term staining (Figure 1D). Importantly, none of six high-grade adult B-cell lymphomas intermediate between Burkitt’s lymphoma and diffuse large B-cell lymphoma (see footnote in Table 1) was positive with the SOX11N-term antibody (Figure 1E). Even more strikingly, all ten cases of T-cell lymphoblastic lymphoma (Figure 1F) and eight of nine stained B-cell acute lymphoblastic leukemia/lymphoblastic lymphomas (Figure 1G) were positive for SOX11N-term. SOX11C-term also confirmed the presence of the protein in three cases of B-cell lymphoblastic lymphoma but was negative in both stained B-cell acute lymphocytic leukemias; four of five tested T-cell lymphoblastic lymphomas were also positive with SOX11C-term. It was notable that two T-cell lymphoblastic lymphomas produced no or weak immunohistochemical signals for terminal deoxynucleotidyl transferase (TdT), despite their otherwise typical morphological and immunophenotypic features. The apparent slight decrease in sensitivity of SOX11C-term compared with SOX11N-term could not be further evaluated due to limited availability of SOX11C-term.
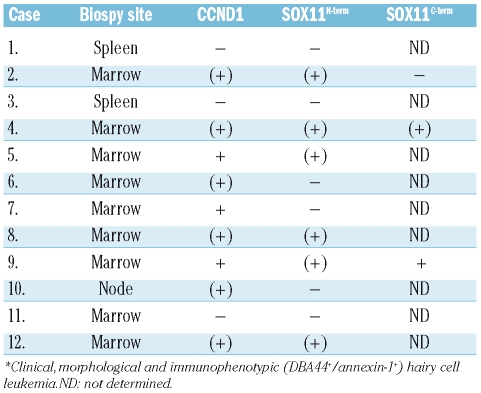
Hairy cell leukemia typically shows modestly elevated CCND1 transcription with weak immunostaining for the protein. Our previous study showed no upregulation of SOX11 transcription but we nevertheless found very weak SOX11N-term immunostaining in six of 12 (DBA44+/annexin-1+) cases (Table 2), which generally paralleled the strength of the CCND1 signal, in contrast to the lack of staining covariation noted in MCL. Moreover, in two of three cases of hairy cell leukemia tested the presence of SOX11 protein was confirmed with the SOX11C-term antibody but only a single specimen (case 9 in Table 2) produced a moderately strong signal (Figure 1H–I). The third subtype with frequent modestly upregulated CCND1 transcription was represented by seven cases of CCND1+ myeloma (n=5)/plasmacytoma (n=2) and two cases of CCND1− myeloma (Table 1). Regardless of CCND1 status, the nuclear SOX11 signal was consistently absent.
Table 2.
Expression of CCND1 and SOX11 in cases of hairy cell leukemia.*
Discussion
The Sox family of transcription factors is widely distributed in animals and SOX proteins are implicated in fundamental developmental processes such as differentiation of murine embryonic stem cells,12 neurogenesis and chondrogenesis.13 SOX11 is expressed in the developing human nervous system,14 medulloblastoma15 and glioma16 but has no defined role in B-lymphocyte ontogeny. We have previously shown that SOX11 is aberrantly expressed in both MCL1 and epithelial ovarian cancer17 in which SOX11 predicts recurrence-free survival. Although the functional effect and downstream genes activated by SOX11 are yet to be described, it is intriguing that the strong nuclear expression of SOX11 in lymphoid neoplasia appears limited to three disparate categories, which include the two mature B-cell tumors, MCL and true Burkitt’s lymphoma, and immature lymphoblastic neoplasms. Further study of the biology of this cohort may reveal common pathways to neoplasia related to SOX11 expression.
Interestingly, frequent nuclear SOX11 expression in clinically, morphologically and genetically typical Burkitt’s lymphoma was not matched by expression in adult intermediate Burkitt’s lymphoma/diffuse large B-cell lymphoma. The number of cases was too small to draw firm conclusions but the potential difference merits more extensive investigation.
We reconfirmed nuclear SOX11 expression in the vast majority of prospectively studied MCL. Rare clinically and morphologically typical cases of MCL with or without t(11;14)(q13;q32) may fail to stain for CCND1, using a sensitive rabbit monoclonal antibody.1,18 This study confirms the consistent SOX11 immunonegativity in the nuclei of common MCL simulators, including the problematic CD5+ variants of common peripheral B-cell lymphoma subtypes, for which ancillary molecular techniques may not be available to rule out CCND1–MCL. It remains to be determined whether SOX11 is expressed in MCL variants lacking the t(11;14) translocation and expressing cyclin D2 or cyclin D3, which are said to maintain the MCL gene expression signature.19
The mechanism of SOX11 dysregulation is unclear but our negative immunostaining for nuclear SOX11 in CCND1+ myeloma cells indicates that the protein is not dependent on CCND1. In myeloma, upregulated CCND1 is due to a polysomic chromosome 11 in half of cases, while in about one in six cases it is due to the same translocation as in MCL: t(11;14)(q13;q32).3 Moreover, strong SOX11-specific signals occurred at high frequency in Burkitt’s lymphoma and T and B-lymphoblastic neoplasms, tumors devoid of t(11;14) but which may contain a variety of other translocations, including those involving transcription factors. These facts make it unlikely that any recognized structural or numerical chromosomal changes are a direct cause of elevated SOX11. Hairy cell leukemia differed markedly from all the above neoplasms in that nuclear SOX11 staining, present in about half of the specimens, was generally very weak and paralleled that of weak or negative cyclin D1, the regulation of which is not due to altered gene dosage or t(11;14).4 It should be noted that the presence of SOX11 in lymphoblastic leukemia/lymphoma introduces an important cause for caution in the use of this marker for MCL given that adult lymphoblastic lymphoma is a rare morphological mimic of MCL.
In conclusion, strong nuclear SOX11 expression in lymphoma is extended to include even lymphoblastic and Burkitt’s lymphomas, indicating a wider role for the protein in lymphomagenesis than previously reported.
Acknowledgments
the authors would like to thank Kristina Lövgren, Christina Andersson, Alicja Flasch, Helen Svensson and Ihab Dahi for their technical assistance.
Footnotes
Authorship and Disclosures
MD wrote the paper and takes primary responsibility for it. SE and CB were the principal investigators and responsible for developing the antibodies with SE, SS, EG performing the special laboratory work involved with testing the antibodies. MD and JW developed protocols and performed in situ hybridization experiments. MS, CG, WA-A and TW ran the RT-PCR assay.
The authors reported no potential conflicts of interest.
Funding: this work was supported by a grant from the Swedish Research Council (16x-04723, to TW), ALF grants from Lund University Hospital to MD and TW, and by grants from the Lund Institute of Technology (LTH), Bioinvent International AB, the Leukemia and Lymphoma Society (Grant n. 6085-06 and R6189-09), Smärtafonden and CREATE Health, a strategic Center for Translational Cancer Research (www.createhealth.se) to CB and SE
References
- 1.Ek S, Dictor M, Jerkeman M, Jirstrom K, Borrebaeck CA. Nuclear expression of the non B-cell lineage Sox11 transcription factor identifies mantle cell lymphoma. Blood. 2008;111:800–5. doi: 10.1182/blood-2007-06-093401. [DOI] [PubMed] [Google Scholar]
- 2.Wang X, Asplund AC, Porwit A, Flygare J, Smith CI, Christensson B, et al. The subcellular Sox11 distribution pattern identifies subsets of mantle cell lymphoma: correlation to overall survival. Br J Haematol. 2008;143:248–52. doi: 10.1111/j.1365-2141.2008.07329.x. [DOI] [PubMed] [Google Scholar]
- 3.Troussard X, Avet-Loiseau H, Macro M, Mellerin MP, Malet M, Roussel M, et al. Cyclin D1 expression in patients with multiple myeloma. Hematol J. 2000;1:181–5. doi: 10.1038/sj.thj.6200025. [DOI] [PubMed] [Google Scholar]
- 4.Bosch F, Campo E, Jares P, Pittaluga S, Munoz J, Nayach I, et al. Increased expression of the PRAD-1/CCND1 gene in hairy cell leukaemia. Br J Haematol. 1995;91:1025–30. doi: 10.1111/j.1365-2141.1995.tb05429.x. [DOI] [PubMed] [Google Scholar]
- 5.de Boer CJ, Kluin-Nelemans JC, Dreef E, Kester MG, Kluin PM, Schuuring E, et al. Involvement of the CCND1 gene in hairy cell leukemia. Ann Oncol. 1996;7:251–6. doi: 10.1093/oxfordjournals.annonc.a010568. [DOI] [PubMed] [Google Scholar]
- 6.Miranda RN, Briggs RC, Kinney MC, Veno PA, Hammer RD, Cousar JB. Immunohistochemical detection of cyclin D1 using optimized conditions is highly specific for mantle cell lymphoma and hairy cell leukemia. Mod Pathol. 2000;13:1308–14. doi: 10.1038/modpathol.3880239. [DOI] [PubMed] [Google Scholar]
- 7.Swerdlow SH, Campo E, Harris NL, Jaffe E, Pileri SA, Stein H, et al. WHO Classification of Haematopoietic and Lymphoid Tumours. 4th edition. Lyon: IARC; 2008. [Google Scholar]
- 8.Agaton C, Galli J, Hoiden Guthenberg I, Janzon L, Hansson M, Asplund A, et al. Affinity proteomics for systematic protein profiling of chromosome 21 gene products in human tissues. Mol Cell Proteomics. 2003;2:405–14. doi: 10.1074/mcp.M300022-MCP200. [DOI] [PubMed] [Google Scholar]
- 9.Ek S, Andréasson U, Hober S, Kampf C, Ponten F, Uhlen M, et al. From gene expression analysis to tissue microarrays: a rational approach to identify therapeutic and diagnostic targets in lymphoid malignancies. Mol Cell Proteomics. 2006;5:1072–81. doi: 10.1074/mcp.M600077-MCP200. [DOI] [PubMed] [Google Scholar]
- 10.Specht K, Kremer M, Muller U, Dirnhofer S, Rosemann M, Hofler H, et al. Identification of cyclin D1 mRNA overexpression in B-cell neoplasias by real-time reverse transcription-PCR of microdissected paraffin sections. Clin Cancer Res. 2002;8:2902–11. [PubMed] [Google Scholar]
- 11.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(−ΔΔC(T)) method. Methods. 2001;25:402–8. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 12.Kuroda T, Tada M, Kubota H, Kimura H, Hatano SY, Suemori H, et al. Octamer and Sox elements are required for transcriptional cis regulation of Nanog gene expression. Mol Cell Biol. 2005;25:2475–85. doi: 10.1128/MCB.25.6.2475-2485.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ng LJ, Wheatley S, Muscat GE, Conway-Campbell J, Bowles J, Wright E, et al. SOX9 binds DNA, activates transcription, and coexpresses with type II collagen during chondrogenesis in the mouse. Dev Biol. 1997;183:108–21. doi: 10.1006/dbio.1996.8487. [DOI] [PubMed] [Google Scholar]
- 14.Hargrave M, Wright E, Kun J, Emery J, Cooper L, Koopman P. Expression of the SOX11 gene in mouse embryos suggests roles in neuronal maturation and epithelio-mesenchymal induction. Dev Dyn. 1997;210:79–86. doi: 10.1002/(SICI)1097-0177(199710)210:2<79::AID-AJA1>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 15.Lee CJ, Appleby VJ, Orme AT, Chan WI, Scotting PJ. Differential expression of SOX4 and SOX11 in medulloblastoma. J Neurooncol. 2002;57:201–14. doi: 10.1023/a:1015773818302. [DOI] [PubMed] [Google Scholar]
- 16.Weigle B, Ebner R, Temme A, Schwind S, Schmitz M, Kiessling A, et al. Highly specific overexpression of the transcription factor SOX11 in human malignant gliomas. Oncol Rep. 2005;13:139–44. [PubMed] [Google Scholar]
- 17.Brennan DJ, Ek S, Doyle E, Drew T, Foley M, Flannelly G, et al. The transcription factor SOX11 is a prognostic factor for improved recurrence-free survival in epithelial ovarian cancer. Eur J Cancer. 2009;45:1510–7. doi: 10.1016/j.ejca.2009.01.028. [DOI] [PubMed] [Google Scholar]
- 18.Cheuk W, Wong KO, Wong CS, Chan JK. Consistent immunostaining for cyclin D1 can be achieved on a routine basis using a newly available rabbit monoclonal antibody. Am J Surg Pathol. 2004;28:801–7. doi: 10.1097/01.pas.0000126054.95798.94. [DOI] [PubMed] [Google Scholar]
- 19.Fu K, Weisenburger DD, Greiner TC, Dave S, Wright G, Rosenwald A, et al. Cyclin D1-negative mantle cell lymphoma: a clinicopathologic study based on gene expression profiling. Blood. 2005;106:4315–21. doi: 10.1182/blood-2005-04-1753. [DOI] [PMC free article] [PubMed] [Google Scholar]