Abstract
Objectives
To identify the number and current location of children, aged 0 to 16 years, requiring long term ventilation in the United Kingdom, and to establish their underlying diagnoses and ventilatory needs.
Design
Postal questionnaires sent to consultant respiratory paediatricians and all lead clinicians of intensive care and special care baby units in the United Kingdom.
Subjects
All children in the United Kingdom who, when medically stable, continue to need a mechanical aid for breathing.
Results
141 children requiring long term ventilation were identified from the initial questionnaire. Detailed information was then obtained on 136 children from 30 units. Thirty three children (24%) required continuous positive pressure ventilation by tracheostomy over 24 hours, and 103 received ventilation when asleep by a non-invasive mask (n=62; 46%), tracheostomy (n=32; 24%), or negative pressure ventilation (n=9; 7%). Underlying conditions included neuromuscular disease (n=62; 46%), congenital central hypoventilation syndrome (n=18; 13%), spinal injury (n=16; 12%), craniofacial syndromes (n=9; 7%), bronchopulmonary dysplasia (n=6; 4%), and others (n=25; 18%). 93 children were cared for at home. 43 children remained in hospital because of home circumstances, inadequate funding, or lack of provision of home carers. 96 children were of school age and 43 were attending mainstream school.
Conclusions
A significant increase in the number of children requiring long term ventilation in the United Kingdom has occurred over the past decade. Contributing factors include improved technology, developments in paediatric non-invasive ventilatory support, and a change in attitude towards home care. Successful discharge home and return to school is occurring even for severely disabled patients. Funding and home carers are common obstacles to discharge.
Key messages
The number of children requiring long term ventilatory support has increased substantially in the past 8 years
Ventilatory support at home is the best option for meeting the child’s psychological needs and enhancing quality of life
The majority of children dependent on long term ventilation live at home and attend mainstream schools
A shift of care has occurred from intensive care units to less acute areas
Introduction
Society has the new responsibility of considering those children who are dependent on technology for their survival. A growing population of children exist who have chronic respiratory failure due to conditions such as muscle disease, disorders of ventilatory control, or abnormalities of the airway, and who require long term ventilation.1,2 At present these children often experience prolonged hospitalisations, which separate them from their families and place them in environments inappropriate for their health and development. A recent survey of intensive care units showed that there were significant numbers of children requiring long term ventilation who were resident in hospital, often in an intensive care setting.3 It is recognised that hospital is both an unsuitable environment for a growing child and an inappropriate use of resources.4 Concerns have also been raised that the continuing availability of paediatric intensive care beds would be severely curtailed unless successful home transfer of these children was achieved.1
The benefits of home care of children requiring long term ventilation are well documented.5–7 Advances in ventilator technology, and a growing experience and acceptance of home care, have increased the possibilities for discharging children requiring long term ventilation from hospital to home. Ten years ago a survey identified 24 children in the United Kingdom on long term ventilation, nine of whom were cared for at home.8 In 1993, a postal survey of the Paediatric Intensive Care Society identified 31 children receiving ventilatory support at home.9 Unfortunately, the response rate to the questionnaire was poor. Subsequently there have been no data on the status of home care of children requiring long term ventilation in the United Kingdom, despite considerable advances in the field and ongoing concerns regarding funding and care in the community.
To obtain up to date information on the current use of long term ventilation in children, we surveyed all consultant respiratory paediatricians and the lead clinicians of intensive care units and special care baby units about children ventilated long term for respiratory failure. Such information is central to the planning of resource allocation, and for evaluating the discharge process and enabling further study into the impact of home ventilation on the children, their families, and the health service.
Subjects and methods
Initially we sent a brief questionnaire to all UK consultant respiratory paediatricians and lead clinicians of intensive care and special care baby units asking them to identify the number of children aged 0 to 16 years who were dependent on long term ventilatory support.
We defined long term ventilatory support as: “any child who, when medically stable, continued to need a mechanical aid for breathing which may be acknowledged after a failure to wean, three months after the institution of ventilation.” Medically stable was not defined but was left to the judgment of the child’s consultant. We excluded data on premature infants who were likely to wean successfully, but included data on children with chronic lung disease of prematurity where weaning was proving impossible beyond three months from term.
We obtained contact addresses for all 112 consultant members of the British Paediatric Respiratory Society from the society’s secretary. Of the 112 initial questionnaires posted, 89 (80%) consultants responded. In addition, we obtained the addresses of the 49 lead clinicians of paediatric intensive care units from the Paediatric Intensive Care Society, of whom 30 (61%) responded to our initial questionnaire. All non-responders or their secretaries were contacted by telephone, and the number of children on long term ventilation was noted. We also became aware of a few children through the parents of other children requiring long term ventilatory support. We then contacted the relevant hospital in the area.
We established a working party of 20 healthcare workers from centres throughout the United Kingdom who had a specific interest in the care of children on long term ventilation. This network provided us with a back up to ensure maximal ascertainment of cases.
The children were registered by their surname, first name, date of birth, and home postcode. Only six children were reported twice by different consultants. These children were registered once on the database under the lead consultant.
All positive responders were sent a more detailed questionnaire. The specific information requested on each child included:
Date of birth and home postcode
The diagnostic category most responsible for ventilator dependence (for example neuromuscular disease)
Date of onset of ventilation (month and year)
The present location of the child—that is, hospital unit or home
Time in present location (in months)
Reasons for hospital stay, if applicable
Method of ventilatory support
Time dependent on the ventilator
Type of ventilator device and maintenance
Professionals coordinating the discharge
Educational provision
Concurrent use of other technology (for example oxygen treatment and monitoring, transcutaneous carbon dioxide monitoring, humidification, wheelchair use)
Funding sources
Support at home.
We reviewed the birth dates and home postcodes to ensure that no child was included twice. Replies were then entered on to a database.
Results
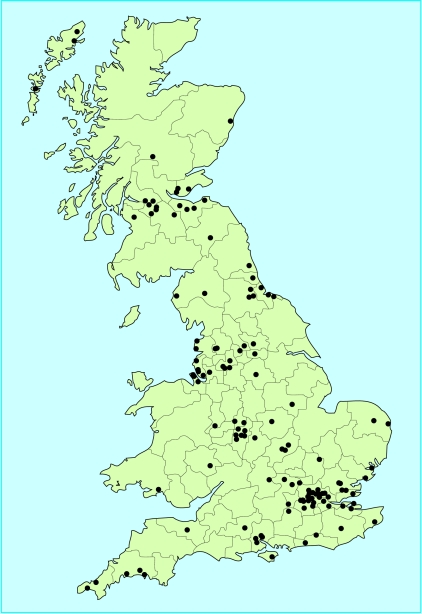
From the initial questionnaire, 141 children requiring long term ventilatory support were identified. More detailed questionnaires were then sent out in May 1997. We received replies from 30 centres, with 49 primary consultants identified from a wide range of specialities (table 1). The survey documented 136 children in the United Kingdom who were chronically dependent on a mechanical aid to breathe (figure). We failed to gain full details on five children despite repeated requests.
Table 1.
Range of specialties caring for 136 children on long term ventilation in the United Kingdom
| Consultant specialty | No of children |
|---|---|
| Respiratory paediatrician | 65 |
| Chest physician | 19 |
| General paediatrician | 15 |
| Spinal injury | 10 |
| Anaesthetist | 7 |
| Paediatric intensivist | 7 |
| Paediatric neurologist | 5 |
| Paediatric neurosurgeon | 2 |
| Neurodevelopmental paediatrician | 2 |
| Paediatric anaesthetist | 1 |
| ENT (paediatric) | 1 |
| Anaesthetics/spinal injury (adult) | 1 |
| Plastic surgeon (paediatric) | 1 |
Age range and aetiology
Table 2 lists the number of children requiring long term ventilation in the United Kingdom according to age range. The main aetiologies of children requiring long term ventilatory support were neuromuscular disease, congenital central hypoventilation syndrome (Ondine’s Curse), spinal injury, craniofacial syndromes, and bronchopulmonary dysplasia (table 3).
Table 2.
Number of children on long term ventilation in the United Kingdom according to age
| Age interval | No |
|---|---|
| <12 months | 5 |
| 1 to 5 years | 44 |
| 6 to 10 years | 43 |
| 11 to 16 years | 44 |
Table 3.
Main diagnostic categories of children requiring long term ventilation in the United Kingdom
| Disorder | No at home | No in hospital |
|---|---|---|
| Neuromuscular disease | 52 | 10 |
| Congenital central hypoventilation syndrome | 13 | 5 |
| Spinal injury | 10 | 6 |
| Craniofacial syndrome | 9 | 0 |
| Bronchopulmonary dysplasia | 1 | 5 |
| Other | 8 | 17 |
| Total | 93 | 43 |
Ninety three children (68%) were cared for at home. Table 4 details the locations of the children in hospital. In each category more children were cared for at home than in hospital. The only exception was bronchopulmonary dysplasia, when five out of six children received hospital care.
Table 4.
Hospital location of 43 children requiring long term ventilation in the United Kingdom
| Hospital location | No of children |
|---|---|
| General ward | 17 |
| Step down unit* | 10 |
| Intensive care unit | 7 |
| Spinal injury unit | 3 |
| Special care baby unit | 3 |
| Community home | 3 |
Any unit that is not classified as either a paediatric intensive care unit or ward setting—for example, high dependency unit, transitional care unit, long term ventilation unit.
Mode of ventilatory support
Sixty five children (48%) received positive pressure support by a tracheostomy. Sixty two children (46%) needed ventilation by a face or nasal mask, and nine children (7%) were managed with negative pressure ventilation.
Fifty two of the 93 children (56%) at home used non-invasive ventilation by a face or nasal mask. This reflects the high proportion of children with neuromuscular disease who are commonly ventilated using non-invasive techniques (table 5).
Table 5.
Types of ventilatory support used at home and in hospital to treat 136 children requiring long term ventilation in the United Kingdom
| Ventilatory support | Home | Hospital |
|---|---|---|
| Delivery mode | ||
| Tracheostomy | 33 | 32 |
| Non-invasive mask | 52 | 10 |
| Negative pressure device | 8 | 1 |
Time on ventilatory support
Children who were dependent on ventilatory support fell into three broad categories: those on support 24 hours per day; those receiving support only when asleep; and those receiving support intermittently when awake and when asleep.
Thirty three of the 136 children (24%) required ventilatory support 24 hours per day. Of these, 13 had been successfully discharged home. Ninety six children (71%) required ventilation when asleep only; 20 were still in hospital, and three were in a paediatric intensive care unit. Seven children required additional ventilatory support intermittently during the day as well as when asleep.
Reasons for prolonged hospitalisation
Several factors were identified as delaying discharge from hospital to home (table 6). Twenty two children (51%) remained in hospital due to failure to recruit qualified nursing staff or trained carers to care for the child in the home environment. Incomplete funding arrangements were a factor in 16 (37%) cases. A further 15 children (35%) were still cared for in hospital because their home was assessed as unsuitable to meet either the child’s needs or that of the equipment.
Table 6.
Obstacles to discharge in 43 hospitalised children requiring long term ventilation
| Obstacle | No of children |
|---|---|
| Staff unavailable for support at home | 22 |
| Funding negotiations not complete | 16 |
| Housing unsuitable | 15 |
| Not established on ventilator for home use | 12 |
| Social reasons | 9 |
| Awaiting transfer to local hospital | 7 |
Funding of home care
Ventilator equipment for the home care of eight children (9%) was provided either by the parents or from charitable sources. Only one child received the full cost of home care from the Department of Social Services. The remaining 84 children (90%) received funding for their respiratory equipment and support from the local health authority.
Patient support at home
The skill of healthcare professionals assisting families in the care of the children at home varied widely. Forty six families (49%) met all their child’s medical needs themselves. Despite this burden on the families, only 16 (17%) had formal respite arrangements in place.
Education
The most surprising finding was the number of children attending mainstream schools. Of 81 children of school age requiring long term ventilation and living at home with their families, 43 (53%) attended mainstream schools. Only two of the 81 children required a home tutor. This was because their local mainstream school was unable to cope with their disability, and because attendance at the local special needs school would have involved a 100 mile round trip. Thirty six children attended special needs schools.
Of the 15 children of school age still in hospital, only three attended the hospital school. The other 12 children attended schools in the community, with three going to their previous mainstream school on a daily basis.
Discussion
Our survey of long term ventilation of children in the United Kingdom, completed during 1997, documents a significant increase in the prevalence of children requiring long term ventilatory support since Robinson first reported on this subject in 1990,8 and a rising incidence (table 7).
Table 7.
Incidence of children in the United Kingdom dependent on ventilatory support by calendar year
| 1988 | 1989 | 1990 | 1991 | 1992 | 1993 | 1994 | 1995 | 1996 | 1997* | |
|---|---|---|---|---|---|---|---|---|---|---|
| Incidence | 1 | 2 | 4 | 4 | 11 | 19 | 11 | 27 | 28 | 18 |
Until end of September.
From the outset, we aimed for complete ascertainment by identifying and contacting all centres and consultants in the United Kingdom who were likely to care for children requiring long term ventilatory support. The initial questionnaire identified 141 such children. Of this group, detailed information was reported in 136 cases. While our findings may not include all cases, they do provide the best available figures for this important group of children. Factors contributing to these increased numbers include improved technology, developments in non-invasive ventilatory support of children and its use in neuromuscular disease, a change in attitude towards home care of these children, and an increase in the number of survivors of paediatric and neonatal intensive care units.10
A recent survey of children requiring long term ventilatory support in Canada identified 82 such children.11 This number is comparable per head of population to our study. In France, the number of children dependent on long term ventilation, and the underlying aetiologies, are also comparable to our study.12 Although the United States has not fully studied this area, it does show a similar pattern, except for a uniquely large number of infants with bronchopulmonary dysplasia. In the United States, considerable cost savings have been shown in ventilated children who have returned home safely on a comprehensively planned programme of care.13
Our study has established that children dependent on long term ventilatory support are successfully being reintegrated into their homes and returning to school, even in the case of severe disability. The number of children successfully discharged from hospital to home, despite the need for ongoing technological care, was greater than anticipated. A previous report highlighted the inappropriateness of caring for long term ventilated children in intensive care.3 Our current findings, however, show that a shift of care seems to have occurred from intensive care units to units where stabilisation of the medical condition, rehabilitation, and reintegration are achieved. This is an appropriate but difficult move requiring effort, time, and resources. For those children still in hospital, the main problems were neither medical nor technical; discharge was frequently stalled by the emotional and practical support required and limited resources.
A surprising and encouraging finding in our study was that most of the children attended mainstream schools. However, there was great disparity in the type of education available to the cohort. Four children requiring ventilatory support 24 hours per day were educated in mainstream schools, yet 26 children with less physical disability and dependent only on ventilatory support during the night were educated in special needs schools.
We identified only nine children for whom family problems were listed as a cause of delayed discharge from hospital. On further investigation, four of the children were expected to return home eventually and the other five were thought to be unable to return home. All these children required ventilation 24 hours per day. Four of the five children had learning disabilities in addition to their physical disabilities. In two cases, the family withdrew from any involvement, and the children remain hospitalised awaiting fostering.
The discharge process can be long and complicated. To help with this issue, discharge guidelines have been formulated by a working party on long term ventilation of children in the United Kingdom.14 The key principles of the discharge process are that the child is a member of the family, that the family must be supported and involved in decision making, and that the responsibility for care of the child transfers from the hospital to the community health team and the family at discharge. The guidelines emphasise the importance of communication and teamwork.
Currently, the financial burden of home care falls on the health authority in which the child resides, as there is no centralised funding for individuals dependent on ventilatory support. Not surprisingly, funding for home ventilation is a common obstacle to discharge and can take many months of negotiation to arrange. Our study established that considerable variability exists between health authorities with respect to the funding requirements of children dependent on ventilatory support. Costs do differ widely depending on the level of dependency of the child and associated disabilities.14
Home care for most children requiring long term ventilatory support is the best option for meeting the child’s medical and psychological needs. It also enhances their quality of life. It is likely that this population of children will continue to increase as medical technology advances and a better understanding of the role of ventilatory support at home develops. Having established minimum prevalence figures there is a need for continuing data on appropriate outcome measures, clinical progress, and incidence figures to assist the rational planning of services.
Figure.
Geographical distribution of 136 children requiring long term ventilation in the United Kingdom
Acknowledgments
We thank the staff who responded to our survey and I Barker, B Boosfeld, R Bullock, C Doyle, S Kerr, R Lane, K Lucking, J Noyes, H Porter, M Samuels, J Shneerson, A Simonds, A Walker, T Ward, J W H Watt, and R Yates as members for the UK working party on the long term ventilation of children.
Footnotes
Funding: NHS Executive, Research and Development Directorate, and Mother and Child Health Programme.
Conflict of interest: None.
References
- 1.Fraser J, Henrichsen T, Mok Q, Tasker R. Prolonged mechanical ventilation as a consequence of acute illness. Arch Dis Child. 1998;78:253–256. doi: 10.1136/adc.78.3.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simonds AK. From intensive care unit to home discharge in the 24 hour ventilator-dependent patient. Eur Respir Mon. 1998;8:364–379. [Google Scholar]
- 3.Fraser J, Mok Q, Tasker R. Survey of occupancy of paediatric intensive care units by children who are dependent on ventilators. BMJ. 1997;315:347–348. doi: 10.1136/bmj.315.7104.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davies RH, Harvey I, Newton-John H, Ward TA. Home ventilation of a child with motor and sensory neuropathy. BMJ. 1996;313:153–155. doi: 10.1136/bmj.313.7050.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frates RC, Splaingard ML, Smith EO, Harrison GM. Outcome of home mechanical ventilation. J Pediatr. 1985;106:850–856. doi: 10.1016/s0022-3476(85)80372-3. [DOI] [PubMed] [Google Scholar]
- 6.Eigen H, Zander J. Home mechanical ventilation of pediatric patients. Am Rev Respir Dis. 1990;141:258–259. doi: 10.1164/ajrccm/141.1.258. [DOI] [PubMed] [Google Scholar]
- 7.Fields AI, Rosenblatt A, Pollack MM, Kaufman J. Home care cost-effectiveness for respiratory technology-dependent children. Am J Dis Child. 1991;145:729–733. [PubMed] [Google Scholar]
- 8.Robinson RO. Ventilator dependency in the United Kingdom. Arch Dis Child. 1990;65:1235–1236. doi: 10.1136/adc.65.11.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barker I. Central funding and a central resource providing information are needed. BMJ. 1996;313:940. doi: 10.1136/bmj.313.7062.940a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newton-John HF. Long-term mechanical ventilation of patients in Australia. Med J Aust. 1989;150:3–6. doi: 10.5694/j.1326-5377.1989.tb136309.x. [DOI] [PubMed] [Google Scholar]
- 11.Dhillon JS, Frewen TC, Singh NC, Speechley KN. Chronic mechanical ventilation-dependent children in Canada. Paediatr Child Health. 1996;1:111–116. [Google Scholar]
- 12.Fauroux B, Howard P, Muir JF. Home treatment for chronic respiratory insufficiency: the situation in Europe in 1992. The European working group on home treatment for chronic respiratory insufficiency. Eur Respir J. 1994;7:1721–1726. doi: 10.1183/09031936.94.07091721. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg AI, Faure AM, Vaughan CJ, Snarski R, Seleny FL. Home care for life-supported persons: an approach to program development. J Pediatr. 1984;104:785–795. doi: 10.1016/s0022-3476(84)80969-5. [DOI] [PubMed] [Google Scholar]
- 14.Jardine E, Wallis C. Core guidelines for the discharge home of the child on long-term assisted ventilation in the United Kingdom. Thorax. 1998;53:762–767. doi: 10.1136/thx.53.9.762. [DOI] [PMC free article] [PubMed] [Google Scholar]