Abstract
Social support is believed to mediate psychosocial recovery in vulnerable populations following trauma. In this study, we examine the relationships between perceived social support and posttraumatic stress disorder symptoms in a cohort of 287 socio-economically disadvantaged adults with orofacial injury by using three waves of data collected over one year following the injury. Using structural equation modeling process, we evaluate the cross-lagged effects between perceived social support (PSS) and PTSD symptoms. We found that PSS had a direct influence on PTSD only when examined concurrently. After controlling the covariates, the model supports the cross-lagged effect for PTSD symptoms on PSS at T2 and T3, which suggests a reciprocal contribution between symptoms and support as time progressed. Our data suggest that, over time, high rates of PTSD symptoms are related to a diminished perception of available social support.
Keywords: PTSD, social support, orofacial injuries
Introduction
Patients with intentional orofacial injuries account for a significant subset of the trauma admissions to our urban medical centers (Hall & Ofodile, 1991; Leathers et al., 1997; Mathog, Toma, Clayman, & Wolf, 2000). Common reactions to the traumatic experience include symptoms of repeated and unwanted experiencing of the event, increased arousal, anxiety, and a persistent sense of current threat. In many of these patients, the constellation of symptoms may be significant enough to meet the diagnostic criteria for Post-Traumatic Stress Disorder (PTSD) and capable of impairing social and occupational functioning for extended periods of time. In our earlier study (Glynn et al., 2003), we found that 25% of patients with mandibular fracture evidenced an acute stress reaction consistent with acute PTSD; (23%) continued to experience significant PTSD symptomatology at 12 months following injury (Glynn et al., 2007). These findings mirror many cross-sectional studies (Dougall, Ursano, Posluszny, Fullerton, & Baum, 2001; Harvey & Bryant, 1999; Zatzick et al., 2006) indicating that PTSD and depression are significant psychological disabilities following severe injuries.
The issue of psychological sequelae of trauma is especially relevant to the care of socioeconomically disadvantaged individuals. Studies of the antecedents, patterns and consequences of orofacial injuries indicate a differential exposure and impact among such vulnerable populations (Brasileiro & Passeri, 2006; R. E. King, Scianna, & Petruzzelli, 2004; Ogundare, Bonnick, & Bayley, 2003). The pervasiveness of mental health problems and the high rates of unmet mental health and social needs among these patients may render them more susceptible to psychological difficulties following any sort of trauma, including facial injury (Asarnow et al., 1999; Glynn et al., 1999; Lento et al., 2004). Accordingly, medical professionals have begun advocating for the incorporation of psychological assessments and care into the management of patients with traumatic injuries (Zatzick & Roy-Byrne, 2006). The successful implementation of such integrated care models depends on the ability to identify risk and protective factors for PTSD and an understanding of how they influence symptoms over time. Of the various personal and environmental factors, available social support has received particular attention as a moderator of the relationship between the traumatic experience and the ensuing psychological distress (Brewin, Andrews, & Valentine, 2000). Most researchers (Lin & Ensel, 1984; Sarason, Pierce, & Sarason, 1990; Wethington & Kessler, 1986) have assumed that social support is uniformly positive in its effects on well-being, postulating that positive social relationships buffer or cushion the individual from the harmful consequences of the stress experience (Cohen & Wills, 1985).
Implicit to the buffering hypothesis is the assumption that social support is a constant resource independent of stress. However, this theory has been criticized for fostering a static view of social support and neglecting the temporal changes in its relation to stressors (Yap and Devilly, 2004). Some investigators (Rook (1984; 1987) have conjectured that negative social interactions may have a stronger influence on the patients’ well-being than positive ones and that life stressors and psychological problems can actually worsen the quality of social support and diminish its benefit. Viewing social support as an endogenous resource that can be depleted by chronic stressors and illness (Lepore, Evans, & Schneider, 1991; Norris & Kaniasty, 1996; Yap & Devilly, 2004), several investigators (Holahan, Moos, Holahan, & Cronkite, 1999; Quittner, Glueckauf, & Jackson, 1990) have examined the mediating aspect of social support in the stress-distress paradigm and found that the perception of available social support could deteriorate under the ongoing strain of chronic illness or environmental stressors. Mediated by chronic stress, perceived social support (PSS) ends up actually contributing to psychological distress. This viewpoint is particularly relevant to post injury symptomatology where contextual factors including social support and life stressors may combine with individual vulnerability factors to influence the development of PTSD (Brewin et al., 2000). Although social support may initially buffer against symptoms, its protective function may break down at increasing levels of trauma or increased exposure to stressful life events (Riggs, Byrne, Weathers, & Litz, 1998; Ruscio, Weathers, King, & King, 2002; Samper, Taft, King, & King, 2004). Furthermore, the very nature of some PTSD symptoms (e.g. irritability, feelings of detachment or estrangement from others) may erode social relationships over time.
Recognizing the paucity of studies on the dynamic interaction between perceived social support and PTSD in vulnerable populations, we sought to examine the temporal dimensions of the relationship using a cohort of socioeconomically marginalized, minority individuals with assault-related orofacial injuries. Utilizing longitudinal psychosocial assessments of a cohort of vulnerable patients treated for traumatic orofacial injury, we used a cross-lagged structural equation model (SEM) to clarify the reciprocal association between PTSD related symptoms and PSS. We tested the direct and the cross-lagged social support-symptom relationship at three different intervals over a one-year period. We hypothesized that PSS would have a significant influence on ensuing psychological symptoms with positive PSS positively influencing the symptoms in the early months following trauma exposure. However, symptomatology continuing for longer periods of time could end up negatively impacting the individual’s PSS. Correspondingly, we further hypothesized that symptoms persisting over time may have an indirect negative effect on PSS.
Methods
Our prospective study recruited from patients presenting with orofacial injury to the King-Drew Medical Center (KDMC) in South Los Angeles between July 1996 and May 2001. The KDMC is a prototypic, inner-city hospital serving a predominately indigent and minority population. Although the spectrum of injury included the mouth, mandible, midfacial, and frontal regions, patients must have at least one fracture involving the mandible to be eligible for the study. All patients had a similar spectrum of injury severity and received treatment as usual for orofacial injuries. Exclusion criteria include gunshot injuries, altered mental status attributable to head injuries, and an inability to provide informed consent. In addition to the baseline data collected at the time of hospital admission and discharge, 4 follow-up assessments were conducted at 10-days, 1 month, 6 months, and 12 months post hospital discharge.
Measures
General socio-demographic data including information on age, gender, ethnicity, employment, marital status, substance and alcohol use, and educational level of each patient were collected at the time of admission. However, we did not collect data on the history of mental health difficulties among the participants prior to their injuries.
Prior Traumatic Exposure
At the 10 day follow-up visit, we administered the Posttraumatic Disorder Scale (PDS, Foa, 1995; Foa, Cashman, Jaycox, & Perry, 1997) to assess lifetime traumatic exposure prior to the facial injury and current PTSD from prior traumatic exposure. The PDS was developed specifically as a brief self-report instrument that would help provide a reliable diagnosis of PTSD. The structure and content of the PDS mirror the DSM-IV diagnostic criteria for PTSD and it has good psychometric properties, construct validity, a test-retest reliability of .83 (Foa et al., 1997) and concordance with diagnoses established through clinical interviews. To accommodate time constraints of a trauma care setting, the 12 categories of lifetime traumatic exposure were combined into 7 conceptual categories (e.g. serious accident, natural disaster, assault (including sexual assault), imprisonment, life-threatening illness, witnessing sudden or violent death, other life threat).
PTSD symptoms from the orofacial injury
At the one month, six month, and 12 month follow-up visits, we assessed the patients for PTSD symptomatology associated with the orofacial injury using the Posttraumatic Disorder Scale (PDS). Endorsement of the component 17 symptoms corresponding to the three symptom clusters (i.e. re-experiencing, avoidance, and hyper-arousal) outlined in Criteria B, C, D of the DSM-IV (American Psychiatric Association, 2000), reflected the objective and subjective responses to the orofacial injury.
Perceived Social Support
For the measurement of perceived social support, a social support index measure was constructed for this study (Brown, Shetty, Delrahim, Belin, & Leathers, 1999). We designed this simple measure to accommodate the physical limitations attendant to orofacial injury and to minimize lengthy interviews about social support. The social support measure includes three items: 1) I have enough friends and social life; 2) I have close contact with members of my family; and 3) When things get really bad, I know I can count on my friends and family for help. A positive response for each item scored 1 and a negative response got a 0 score. The three items were summed to determine the individual’s PSS. Using Stata’s Cronbach’s Alpha via Kuder-Richardson 20, the reliability coefficient of this measure based on our sample is .71.
Sample
Subjects
A sample of 336 patients was recruited at baseline. The majority of orofacial injuries among the participants were attributable to assault (82%) with the remaining comprising of fall/accident (14%) or motor vehicle accidents (4%). The patients were predominantly male (89%) with a mean age of 34.25 (SD=10.04) years. In terms of ethnicity, 73% self-identified as African American; 22% as Hispanic/Latino; 10% as Caucasian; 5% as Native American; and 3% Asian American or others. For marital status, 66.7% reported never being married; 15.5% were married; and the remaining 17.8% were widowed, separated, or divorced. Many (38.7%) of the sample had not completed high school, while 61.3% reported to have completed high school or higher education. A high percentage (68%) of the participants reported being unemployed.
Missing Data
Despite rigorous follow-up efforts, the itinerant lifestyles of our cohort of vulnerable patients were reflected by the diminishing recall rates over time. We obtained complete baseline data for all 336 participants; 292 patients returned for the 10-day follow-up visit (attrition = 13%); by 1 month, the attrition rate had only increased slightly to 14.6% (n=287). At the 6-month and 12-month recall, the rate of attrition was 42% compared to baseline (n=194 at 6 months and n=193 at 12 months). Using pairwise ML method, we are able to use a total of 287 cases with complete and incomplete data between the 1 to 12 month recalls. No demographic variables predicted loss of follow-up at 1-month. However, subjects returning for 6- and 12-month interviews were more likely to have graduated from high school and were more likely African American. Statistics on missing data was previously reported in Glynn et al (2007).
Predictors of PDS scores related to the orofacial injury
According to Glynn et al. (2007), PTSD symptoms, as documented by the PDS scores, decreased significantly throughout the year (F(1182) = 19.936, p < 0.001); nonetheless many individuals continued to report high psychological distress. Based on univariate tests of the variables associated with symptoms of PTSD, none of the socio-demographic variables predicted 6- and 12- month PDS scores. However, patient gender, and self-report of prior exposure to trauma at baseline were significant predictors of PDS scores at 1-month. In a two-sample t-test, females showed a higher PDS score than males (X = 35.89, SD = 12.84 for females and X = 29.68, SD = 11.09 for males; p < .00). Subjects with prior exposure to trauma also had higher PDS scores at 1 month and at 12 months (at 1 month: X = 32.84, SD =12.72 for prior trauma and X = 29.31, SD =10.72 with no prior trauma; p< .00; at 12 months: X = 28.15, SD =11.74 for prior trauma and X = 23.48, SD =7.75 with no prior trauma; p< .01). Self-report substance and alcohol use are not significant predictors for symptomatology or PSS. The demographic and exposure variables that significantly predicted severe PTSD symptoms at 1 month were incorporated into the SEM model as covariates.
Data Analytic Strategy
We used the general approach cross-lagged structural equation modeling process to examine the relationship of PSS and symptomatology over the period of 1-year. A cross-lagged model (Kessler & Greenberg, 1981) allowed us to capture the directional effects and the correlated changes in the social support-symptom relationship over the course of one-year post injury at three equal intervals. To utilize available data, the Pairwise Based ML with Robust Corrections method in the EQS (Version 6.1) program was used to examine the structural models. The Pairwise ML Robust method uses the ML approach to correct the misspecification (Savalei & Bentler, 2005).
We examined the relationships between PDS score and the PSS, as represented by the social support index score, at the 1, 6 and 12 months intervals. Three indices and their cutoff points, as suggested by Hu and Bentler (1999), were used to assess goodness of fit for the models. The Multivariate Wald test was used with the robust information matrix to test whether free parameters could be simultaneously constrained at zero to improve the empirical identification of model parameter with only minimal loss in the overall fit. The PDS severity score and the social support index are included in this cross-lagged model to determine their cross-lagged effect. The Sobel test (1982) provides an approximate significance test for the indirect effect for a simple mediation.
Results
Cross-lagged path analysis
Figure 1 represents the hypothesized cross-lagged model examining the relationship between PSS and PDS scores and using gender and prior trauma as control variables. The structural model was tested using a Pairwise ML method. Table 1 shows the means, standard deviations, and zero-order correlations for the six observed variables. On the basis of the Mardia’s multivariate normality test through EQS, these observed variables were not multivariate normal. Therefore, the Satorra-Bentler (1994) robust chi-square was used to adjust for the impact of non-normality.
Figure 1. Initial Cross-Lagged Model.
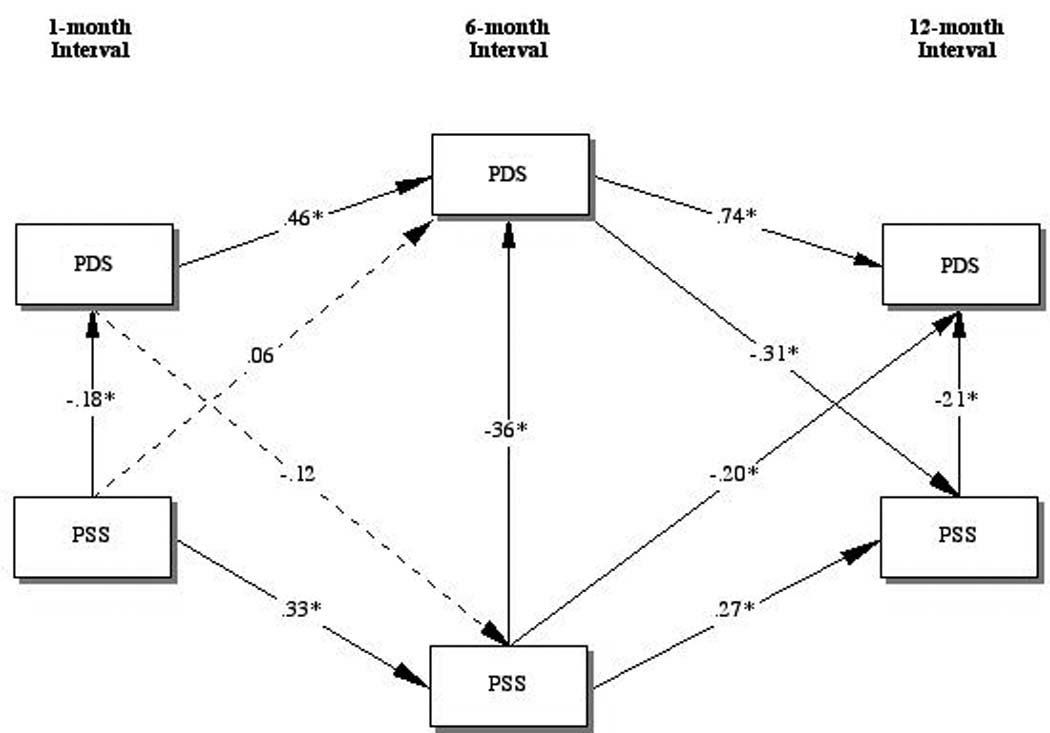
* p< .05
Dashed lines represent non-significant path.
Covariates are omitted from this figure.
Table 1.
Correlation Matrix with means and standard deviations
| PDS1 | PDS2 | PDS3 | PSS1 | PSS2 | PSS3 | |
|---|---|---|---|---|---|---|
| PDS1 | 1.00 | |||||
| PDS2 | 0.50 | 1.00 | ||||
| PDS3 | 0.46 | 0.66 | 1.00 | |||
| PSS1 | −0.20 | −0.18 | −0.11 | 1.00 | ||
| PSS2 | −0.17 | −0.45 | −0.24 | 0.29 | 1.00 | |
| PSS3 | −0.24 | −0.39 | −0.40 | 0.13 | 0.48 | 1.00 |
| Mean | 30.37 | 28.38 | 27.43 | 2.66 | 2.53 | 2.69 |
| SD | 11.44 | 11.94 | 11.44 | .786 | .893 | .751 |
| N | 287 | 194 | 193 | 287 | 191 | 197 |
Note. PDS is the total PTSD severity score, 1=1-month assessment; 2=6-month assessment; and 3=12-month assessment. PSS is the perceived social support score. The pairwise correlations are all significant at p<0.05.
The independence model to test our hypothesis that the PSS and PDS variables are uncorrelated with one another was easily rejected (χ2(28, N=287) = 683.2, p<.01). The initial hypothesized model (Figure 1), using the scaled chi-square, shows a marginal good fit of the model to the data (χ2(11, N=287) = 17.75, p =.09; CFI = .99; RMSEA= .043; (90% confidence interval = .000 - .078); and SRMR = .038). We used the Wald test in the post hoc model modifications to develop a better model fit. This analysis shows that two paths could be constrained to produce a more parsimonious model with only minimal loss to the goodness of fit. Figure 1 shows that most paths are significant at .05, except for the cross-lagged path from time interval 1 to 2, which suggests no significant direct effect between PTSD symptoms and PSS from 1 month to 6 months post injury. These paths were trimmed for the final model. Using the scaled chi-square, the final model (Figure 2) has a χ2(13, N=287) = 10.06, p =.69; CFI = 1; RMSEA= .000; (90% confidence interval = .000 - .043); and SRMR = .052.
Figure 2. Final Cross-Lagged Model.
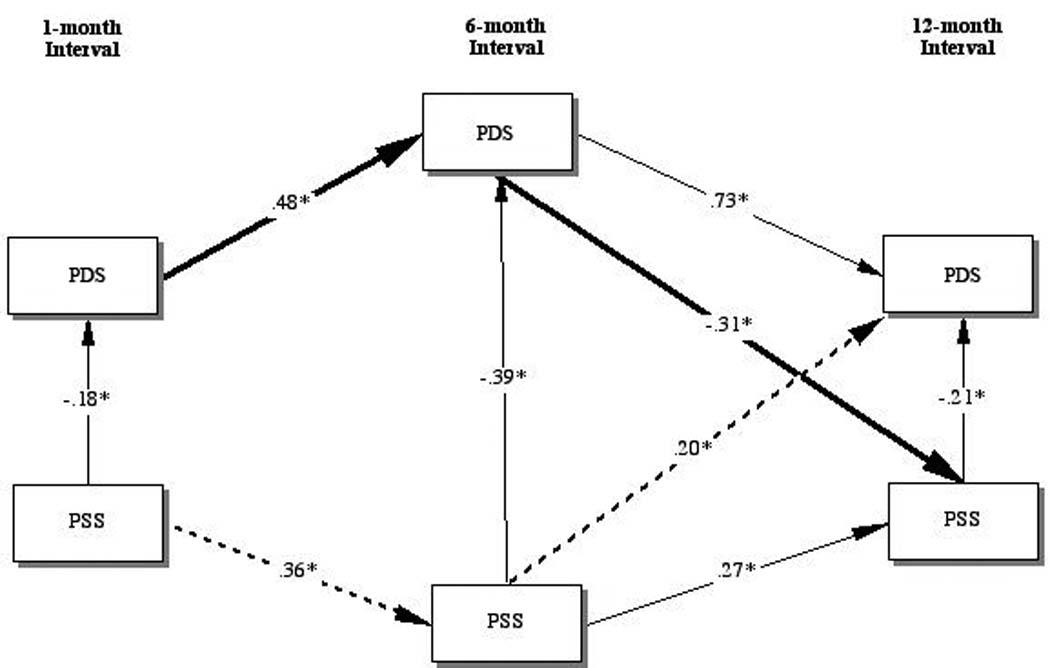
Bolded lines represent significant direct effect.
Dashed lines represent not significant (p > .05) indirect effect.
* p< .05
Covariates are omitted from this figure.
Direct Effects
The model in figure 2 shows a significant direct effect between PSS and PDS at 1-month with a β of -.18 (z = -2.73; p<.01); at 6 months the β = -.39 (z = -4.93; p<.01); and at 12 months β = -.21 (z = -2.15; p<.01). A cross-lagged direct effect between PSS at 6-month to PTSD at 12-month is also significant β = -.2 (z = 2.15; p<.01). As PSS increased, PTSD symptoms decreased. However, the model also indicates that PTSD symptoms at 6 months significantly predict PSS at 12 months with a β of -.31 (z = -2.81; p<.01).
Cross-lagged Effects
We first examined the cross-lagged effects for PSS on PDS. The specific cross-lagged effect for PSS is indicated by the dashed line in Figure 2. Using the Sobel test, PSS at 1 month is a not a significant predictor for symptoms at 12 months when mediated by PSS at 6 months (β = (.36) × (.2) = .07; p>.07). However, the mean indirect effect from PDS at 1 month to PDS at 6 months to PSS at 12 months is significant, (β = (.48) × (-.31) = -.15; p<.01). This specific cross-lagged effect is indicated by the bolded line in Figure 2. Table 2 shows the effects decomposition of all the variables on PSS at 12 months.
Table 2.
Decomposition of Effects with Standardized Values on Perceived Social Support at 12 Months
| Direct Effect | Indirect Effect | Total Effect | |
|---|---|---|---|
| PDS T1a | -- | −.147* | −.147* |
| PDS T2b | −.306* | -- | −.306* |
| PSS T1 a | -- | .165* | .165* |
| PSS T2 b | .268* | .119* | .387* |
Note. T1 = Assessment at 1 month
T2 = Assessment at 6 month
p < .05.
Cross-Lagged Effects Between PTSD Symptom Clusters
To explore the impact of specific PTSD symptoms on PSS over time, we decomposed the PDS variables by their respected symptom clusters (B = re-experiencing, cluster C = effortful avoidance/emotional numbing, and cluster D = hyper-arousal) and tested the cross-lagged effect separately for each symptom cluster. In comparison, symptom clusters C and D shared similar relationship to the full model, except for the re-experiencing symptoms (Cluster B). The time-lagged effect of re-experiencing cluster is not significant (β = (.35) × (-.21) = -.07; p>.05). In contrast to the other clusters, PSS at 6 months has significant direct influence on re-experiencing symptoms at 12 months (β = .27; p<.05). Upon examining the standard coefficients (β) and the Sobel tests in these analyses, with the exception of re-experiencing, all other symptoms clusters over time have a significant influence on PSS; however social support appears to have a much higher influence on the re-experiencing symptoms after a six-month time lag. Table 3 shows the effects decomposition of the PTSD Symptom Clusters on PSS at 12 months.
Table 3.
Decomposition of Effects with Standardized Values of PTSD Symptom Clusters on PSS at 12 Months1
| Direct Effect | Indirect Effect | |
|---|---|---|
| Re-experiencing T1 | -- | -.077 |
| Re-experiencing T2 | −.208* | -- |
| Avoidance T1 | -- | −.135* |
| Avoidance T2 | −.305* | -- |
| Hyperarousal T1 | -- | −.149* |
| Hyperarousal T2 | −.309* | -- |
Note. Control variables and PSS at time 1 and 2 are omitted from this table.
T1 = Assessment at 1 month
T2 = Assessment at 6 month
p < .05.
Discussion
Using a cross-lagged model, we examined the (potentially) changing relationships of perceived social support and trauma symptoms after an orofacial injury in a socioeconomically marginalized, predominantly male sample. The cross-lagged model does not attempt to establish causation, but it is a method to examine the relative contribution of the variables in the model. By comparing the cross-lagged effects for each variable, both as endogenous and exogenous, we are able to observe the influence of symptoms on social support. Through our model, we found a strong relationship between perceived support and symptoms related to PTSD, although not quite consistent with our initial assumptions. Contrary to our hypothesis, perceived support only has a positive direct influence on psychological symptoms when examined concurrently at each time interval. Perceived social support does not appear to mediate subsequent symptoms, even during the early stages following injury. Rather, persisting PTSD symptoms tended to have a significant negative influence on PSS later in time.
Neither symptoms nor PSS have any significant direct influence on each other from time-1 to time-2, but PDS has a direct and indirect influence on PSS at 12 months. This finding supports the cross-lagged effect from symptoms to PSS. The finding of delayed effect echoes other longitudinal studies on stress and PSS (Holahan et al., 1999; Lepore et al., 1991; Norris & Kaniasty, 1996) which could not substantiate the role of PSS as a buffer over time. In the case of PTSD, the psychological distress resulting from trauma significantly influenced a person’s perception of their available support after an extended period of time. It may be that the symptoms of PTSD (e.g. irritability, numbing, avoidance) may lead to an atrophy of social relationships. Early studies on the predictors of PTSD have shown a strong correlation between life events, coping, and social resources; however, social support is the variable that contributes the most to symptoms (Solomon, Mikulincer, & Habershaim, 1990). The generally accepted theoretical model suggests that social resources are mediated by environmental factors, life events, and individual’s resiliency. However, aside from these factors, our model also shows that the course of PTSD symptoms could also have a negative influence on PSS.
Though the lack of significant association between PSS and PDS from 1 month to 6 months was unexpected, a number of factors may help explain this finding. First of all, during the early recovery phase, the survivor’s social network may be primed to accommodate and/or compensate for any trauma symptoms or other adjustment issues evidenced, yielding little relation between symptoms and perceived support. Over time, members of the network may anticipate a return to baseline and be less likely to make these accommodations. Second, as indicated by previous reports on this sample (Glynn et al., 2003; Lento et al., 2004), patients in this study experienced high rates of other stressful life events during the subsequent year. Although patients undergoing orofacial surgery for mandible bone fracture do recover without permanent visible deformity, the social circumstances leading up to the injuries and the recovery process may have lingering negative effects. Perhaps the magnitude of stressful life events may lessen the beneficial impact of social support. After traumatic events, the demands for support will likely increase; however, stressful life events may limit PSS or produce the withdrawal of support from others (Solomon & Mikulincer, 1990; Solomon et al., 1990). Undesirable life events can have a significant impact on internal resilience factors and external resources (L. A. King, King, Fairbank, Keane, & Adams, 1998). Furthermore, the facial injuries, particularly those of assaultive origin, may alter the perception of self-efficacy, which in turn may influence individuals’ help-seeking behaviors and their perception of social support.
Many PTSD researchers have identified avoidance and emotional numbing symptoms to be the primary factors that interfere with the familial relationships, but most of these studies concern veterans and combat related trauma (Galovski & Lyons, 2004; Riggs et al., 1998; Wilson & Kurtz, 1997). Consistent with previous research, we found in our civilian sample that symptoms of avoidance/numbing and hyperarousal make the same contribution to PSS at 12 months in our exploratory analyses. However, the symptoms of re-experiencing do not have a significant indirect effect on PSS over time; the very private nature of these experiences (e.g. dreams, memories) may render them less likely to impact on relationships except in their most extreme forms (e.g acting in a flashback). Emotional expression plays a vital role in maintaining relationships, therefore detachment, isolation, and withdrawal can add conflicts and strains to these relationships. Hyperarousal, especially if reflected in irritability and argumentativeness, might also be expected to have a long-term deleterious effect on relationships. But, our findings regarding these differences are explorative and should be interpreted with caution.
Overall, the results highlight the fact that PTSD symptoms may erode the availability of social support for trauma survivors not immediately, but over time. The findings suggest that interventions designed to assist traumatized persons and their loved ones be informed by typical responses to trauma and how individuals cope with its deleterious effects. Educational and family interventions may be an essential protection against long-term negative outcomes.
Limitations
One of the drawbacks in this study is the rate of attrition over the 12-month follow-up. Even with the expectation of some attrition due to the itinerant life-styles of the patient population and is not unique in health services research (Desmond, Maddux, Johnson, & Confer, 1995; Flick, 1988), the high attrition does raise a serious question of whether our analysis generated correct estimates. We cannot minimize this serious drawback when attempting to predict the reciprocal contribution of PDS and PSS over time, though we attempted to address this limitation by using the SEM approach to build a parsimonious model with strong theoretical groundwork. Therefore, we must interpret our results cautiously. Nonetheless, the lack of research on the stress-distress relations for this understudied population makes our investigation useful. Our findings provide indication where further research might be necessary to address the unmet needs for this population.
Another limitation is the use of brief self-report measures of the constructs of interest. Conducting research in natural settings always presents the challenge of balancing clinical rigor with feasibility. Since the assessments involved injured patients and were conducted in an acute trauma care setting of a busy public hospital, the battery of assessments was kept to a reasonable length. However, we are reassured by the fact that, with regard to PDS and the Structured Clinical Interview for Diagnosis, the sensitivity (.82) and specificity (.79) have been reported to be high (Foa, Cashman, Jaycox, & Perry, 1997). Although a more elaborate social support measure would have strengthened our conclusion, such measures are also more involved and may be too burdensome for individuals who are recovering from orofacial injuries. The questions eliciting social support was constructed with consideration to the speech and pain limitations and based on our earlier experiences with a similar patient pool (Brown et al., 1998).
In interpreting these data, it is important to keep in mind that our study participants were mostly male survivors of interpersonal violence. Not all, but a significant portion of our sample (25%) met clinical screening criteria for PTSD at 1-month follow-up, and their psychological distress based on the PDS continued to be high during the 12-month observation. The mean PDS score from our sample at 12 months was 27.15 (SD, 11.31), which are higher than that of the PDS normative sample (mean, 23.41; SD, 14.68), collected from 248 mental health consumers throughout the U.S. who had experienced a traumatic event a minimum of 1 month earlier.
Despite the limitations, the study does possess unique strengths. First, few studies have examined the long-term effects of PTSD on PSS and their temporal relationships. Although some studies have devised complicated theoretical models to help explain the various factors that may predict the outcome of PTSD, our study examined how specific symptoms of PTSD are related to social support over time. Few trauma studies have applied a cross-lagged SEM design to evaluate the effect of one variable on change in another as suggested by D.W. King et al (2006).
Second, our subjects represented a rarely studied group; specifically, primarily male victims of assault and accidents, and living in inner-city communities with high rates of community violence and enduring stressors. It is interesting our results are similar to other studies focused on combat trauma or sexual assaults (D. W. King, Vogt, & King, 2004; Scarpa, Haden, & Hurley, 2006). Kawachi and Subramanian (2006) suggest that ecological impact, such as social capital or collective efficacy, is contextually relevant to the exposure to trauma and its psychological outcome. Though our study lacked such ecological measures and assessment, our sample clearly represents a racially concentrated, inner-city community. Community-based research provides a way to compare the ecological influence on health services research, and therefore it is crucial in advancing our knowledge about trauma and PTSD.
Third, psychosocial problems specifically related to facial injuries and PTSD are understudied. The impact of injury to a very visible region of the body and its impact on symptoms relating to trauma could have a different manifestation compared to other injuries to other regions. Indeed, an important next step is to examine the mediating effects for interpersonal resources, social support and stressful life events on the course of PTSD for this population.
To our knowledge, our investigation is the first prospective study to elaborate on the temporal relationship between perceived social support and posttraumatic stress for vulnerable individuals seeking treatment of facial injury. Our findings are especially relevant to effective treatment modalities, particularly in the psychosocial functioning. It also reinforces the need for trauma care professional and social service providers to be sensitized and trained in providing ongoing brief psychological assessment and social support resources during post-treatment assessment.
Figure 3.
Figure 4.
Acknowledgments
The project described was conducted by the UCLA Facial Injury Research Center and supported by Grant Number P50/DE-10598 from the National Institute of Dental and Craniofacial Research.
We gratefully acknowledge the assistance of Thomas R. Belin, Ph.D. for advice on the statistical analyses.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Asarnow JR, Glynn SM, Asarnow R, Shetty V, Leathers R, Belin TR, et al. Mental health needs of inner-city, orofacial injury patients. International journal of oral biology. 1999;24:31–35. [Google Scholar]
- Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: A 5-year prospective study. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontics. 2006;102(1):28–34. doi: 10.1016/j.tripleo.2005.07.023. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68(5):748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Brown KA, Shetty V, Atchison K, Leathers R, Black E, Delrahim S. Social support, well-being and risk behaviors among minority males treated at an urban orofacial injury center. International Journal of Oral Biology. 1998;23(1):37–45. [Google Scholar]
- Brown KA, Shetty V, Delrahim S, Belin T, Leathers R. Correlates of missed appointments in orofacial injury patients. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontics. 1999;87(4):405–410. doi: 10.1016/s1079-2104(99)70238-6. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310–357. [PubMed] [Google Scholar]
- Desmond DP, Maddux JF, Johnson TH, Confer BA. Obtaining follow-up interviews for treatment evaluation. J Subst Abuse Treat. 1995;12(2):95–102. doi: 10.1016/0740-5472(94)00076-4. [DOI] [PubMed] [Google Scholar]
- Dougall AL, Ursano RJ, Posluszny DM, Fullerton CS, Baum A. Predictors of posttraumatic stress among victims of motor vehicle accidents. Psychosomatic Medicine. 2001;63(3):402–411. doi: 10.1097/00006842-200105000-00009. [DOI] [PubMed] [Google Scholar]
- Flick SN. Managing attrition in clinical research. Clinical Psychology Review. 1988;8(5):499–515. [Google Scholar]
- Foa EB. The Posttraumatic Stress Disorder Scale. Minneapolis: National Computer System; 1995. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9(4):445–451. [Google Scholar]
- Galovski T, Lyons JA. Psychological sequelae of combat violence: A review of the impact of PTSD on the veteran's family and possible interventions. Aggression and Violent Behavior. 2004;9(5):477–501. [Google Scholar]
- Glynn SM, Asarnow JR, Asarnow R, Shetty V, Black E, Forney D. Orofacial injury and development of acute PTSD. International Journal of Oral Biology. 1999;24:26–30. [Google Scholar]
- Glynn SM, Asarnow JR, Asarnow R, Shetty V, Elliot-Brown K, Black E, et al. The development of acute post-traumatic stress disorder after orofacial injury: a prospective study in a large urban hospital. Journal of Maxillofacial Surgery. 2003;61(7):785–792. doi: 10.1016/s0278-2391(03)00239-8. [DOI] [PubMed] [Google Scholar]
- Glynn SM, Shetty V, Elliot-Brown K, Leathers R, Belin TR, Wang J. Chronic posttraumatic stress disorder after facial injury: a 1-year prospective cohort study. J Trauma. 2007;62(2):410–418. doi: 10.1097/01.ta.0000231556.05899.b0. discussion 418. [DOI] [PubMed] [Google Scholar]
- Hall SC, Ofodile FA. Mandibular fractures in an American inner-city - The Harlem Hospital Center experience. Journal of the National Medical Association. 1991;83(5):421–424. [PMC free article] [PubMed] [Google Scholar]
- Harvey AG, Bryant RA. Predictors of acute stress following motor vehicle accidents. Journal of Traumatic Stress. 1999;12(3):519–525. doi: 10.1023/A:1024723205259. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC. Resource loss, resource gain, and depressive symptoms: A 10-year model. Journal of Personality and Social Psychology. 1999;77(3):620–629. doi: 10.1037//0022-3514.77.3.620. [DOI] [PubMed] [Google Scholar]
- Hu L-t, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Kawachi I, Subramanian SV. Measuring and Modeling the Social and Geographic Context of Trauma: A Multilevel Modeling Approach. Journal of Traumatic Stress. 2006;19(2):195–203. doi: 10.1002/jts.20108. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Greenberg DF. Linear panel analysis : models of quantitative change. New York: Academic Press; 1981. [Google Scholar]
- King DW, King LA, McArdle JJ, Grimm K, Jones RT, Ollendick TH. Characterizing Time in Longitudinal Trauma Research. Journal of Traumatic Stress. 2006;19(2):205–215. doi: 10.1002/jts.20112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DW, Vogt DS, King LA. Risk and resilience factors in the etiology of chronic posttraumatic stress disorder. In: Litz BT, editor. Early intervention for trauma and traumatic loss. New York, NY, US: Guilford Press; 2004. pp. 34–64. [Google Scholar]
- King LA, King DW, Fairbank JA, Keane TM, Adams GA. Resilience-recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: Hardiness, postwar social support, and additional stressful life events. Journal of Personality and Social Psychology. 1998;74(2):420–434. doi: 10.1037//0022-3514.74.2.420. [DOI] [PubMed] [Google Scholar]
- King RE, Scianna JM, Petruzzelli GJ. Mandible fracture patterns: A suburban trauma center experience. American Journal of Otolaryngology. 2004;25(5):301–307. doi: 10.1016/j.amjoto.2004.03.001. [DOI] [PubMed] [Google Scholar]
- Leathers R, Shetty V, Black E, Atchison K, Tomori Y, Cordero R, et al. Orofacial injury profiles and patterns of care in an inner-city hospital. Journal of Dental Research. 1997;76:952–952. [Google Scholar]
- Lento J, Glynn S, Shetty V, Asarnow J, Wang J, Belin TR. Psychological functioning and needs of indigent patients with facial injury: a prospective controlled study. Journal of Oral and Maxillofacial Surgery. 2004;62(8):925–932. doi: 10.1016/j.joms.2004.02.009. [DOI] [PubMed] [Google Scholar]
- Lepore SJ, Evans GW, Schneider ML. Dynamic role of social support in the link between chronic stress and psychological distress. Journal of Personality and Social Psychology. 1991;61(6):899–909. doi: 10.1037//0022-3514.61.6.899. [DOI] [PubMed] [Google Scholar]
- Lin N, Ensel WM. Depression-mobility and its social etiology: The role of life events and social support. Journal of Health and Social Behavior. 1984;25(2):176–188. [PubMed] [Google Scholar]
- Mathog RH, Toma T, Clayman L, Wolf S. Nonunion of the mandible: An analysis of contributing factors. Journal of Oral and Maxillofacial Surgery. 2000;58(7):746–752. doi: 10.1053/joms.2000.7258. [DOI] [PubMed] [Google Scholar]
- Norris FH, Kaniasty K. Received and perceived social support in times of stress: A test of the social support deterioration deterrence model. Journal of Personality and Social Psychology. 1996;71(3):498–511. doi: 10.1037//0022-3514.71.3.498. [DOI] [PubMed] [Google Scholar]
- Ogundare BO, Bonnick A, Bayley N. Pattern of mandibular fractures in an urban major trauma center. Journal of Oral and Maxillofacial Surgery. 2003;61(6):713–718. doi: 10.1053/joms.2003.50118. [DOI] [PubMed] [Google Scholar]
- Quittner AL, Glueckauf RL, Jackson DN. Chronic parenting stress: Moderating versus mediating effects of social support. Journal of Personality and Social Psychology. 1990;59(6):1266–1278. doi: 10.1037//0022-3514.59.6.1266. [DOI] [PubMed] [Google Scholar]
- Riggs DS, Byrne CA, Weathers FW, Litz BT. The quality of the intimate relationships of male Vietnam veterans: Problems associated with posttraumatic stress disorder. Journal of Traumatic Stress. 1998;11(1):87–101. doi: 10.1023/A:1024409200155. [DOI] [PubMed] [Google Scholar]
- Rook KS. The negative side of social interaction: impact on psychological well-being. Journal of Personality and Social Psychology. 1984;46(5):1097–1108. doi: 10.1037//0022-3514.46.5.1097. [DOI] [PubMed] [Google Scholar]
- Rook KS. Social support versus companionship: effects on life stress, loneliness, and evaluations by others. Journal of Personality and Social Psychology. 1987;52(6):1132–1147. doi: 10.1037//0022-3514.52.6.1132. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Weathers FW, King LA, King DW. Male war-zone veterans' perceived relationships with their children: The importance of emotional numbing. Journal of Traumatic Stress. 2002;15(5):351–357. doi: 10.1023/A:1020125006371. [DOI] [PubMed] [Google Scholar]
- Samper RE, Taft CT, King DW, King LA. Posttraumatic stress disorder symptoms and parenting satisfaction among a national sample of male Vietnam veterans. Journal of Traumatic Stress. 17;4:311–315. doi: 10.1023/B:JOTS.0000038479.30903.ed. [DOI] [PubMed] [Google Scholar]
- Sarason IG, Pierce GR, Sarason BR. Social support and interactional processes: A triadic hypothesis. Journal of Social and Personal Relationships. Special Issue: Predicting, activating and facilitating social support. 1990;7(4):495–506. [Google Scholar]
- Satorra A, Bentler PM. Corrections to test statistics and standard errors in covariance structure analysis. In: von Eye A, Clogg CC, editors. Latent variables analysis: Applications for developmental research. Thousand Oaks, CA, US: Sage Publications, Inc.; 1994. pp. 399–419. [Google Scholar]
- Savalei V, Bentler PM. A Statistically Justified Pairwise ML Method for Incomplete Nonnormal Data: A Comparison With Direct ML and Pairwise ADF. Structural Equation Modeling. 2005;12(2):183–214. [Google Scholar]
- Scarpa A, Haden SC, Hurley J. Community Violence Victimization and Symptoms of Posttraumatic Stress Disorder: The Moderating Effects of Coping and Social Support. Journal of Interpersonal Violence. 2006;21(4):446–469. doi: 10.1177/0886260505285726. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structual equations models. In: Leinhart S, editor. Sociological Methodology. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- Solomon Z, Mikulincer M. Life events and combat-related posttraumatic stress disorder: The intervening role of locus of control and social support. Military Psychology. 1990;2(4):241–256. [Google Scholar]
- Solomon Z, Mikulincer M, Habershaim N. Life-events, coping strategies, social resources, and somatic complaints among combat stress reaction casualties. British Journal of Medical Psychology. 1990;63(2):137–148. doi: 10.1111/j.2044-8341.1990.tb01607.x. [DOI] [PubMed] [Google Scholar]
- Wethington E, Kessler RC. Perceived support, received support, and adjustment to stressful life events. Journal of Health and Social Behavior. 1986;27(1):78–89. [PubMed] [Google Scholar]
- Wilson JP, Kurtz RR. Assessing posttraumatic stress disorder in couples and families. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York, NY, US.: Guilford Press; 1997. pp. 349–372. [Google Scholar]
- Yap MBH, Devilly GJ. The role of perceived social support in crime victimization. Clinical Psychology Review. 2004;24(1):1–14. doi: 10.1016/j.cpr.2003.09.007. [DOI] [PubMed] [Google Scholar]
- Zatzick DF, Grossman DC, Russo J, Pynoos R, Berliner L, Jurkovich G, et al. Predicting Posttraumatic Stress Symptoms Longitudinally in a Representative Sample of Hospitalized Injured Adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(10):1188–1195. doi: 10.1097/01.chi.0000231975.21096.45. [DOI] [PubMed] [Google Scholar]
- Zatzick DF, Roy-Byrne PP. From bedside to bench: how the epidemiology of clinical practice can inform the secondary prevention of PTSD. Psychiatric Services. 2006;57(12):1726–1730. doi: 10.1176/ps.2006.57.12.1726. [DOI] [PubMed] [Google Scholar]


