Abstract
During their passage through the circulatory system, tumor cells undergo extensive interactions with various host cells including endothelial cells and platelets. Mechanisms mediating tumor cell adhesion, migration, and metastasis to vessel wall under flow condition are largely unknown. The aim of this study was to investigate the potential roles of GPIIb/IIIa and αvβ3 integrins underlying the HeLa-endothelium interaction in static and dynamic flow conditions. HeLa cell migration and invasion were studied by using Millicell cell culture insert system. The numbers of transmigrated or invaded HeLa cells significantly increased by thrombin-activated platelets and reduced by eptifibatide, a platelet inhibitor. Meanwhile, RGDWE peptides, a specific inhibitor of αvβ3 integrin, also inhibited HeLa cell transmigration. Interestingly, the presence of endothelial cells had significant effect on HeLa cell migration regardless of static or cocultured flow condition. The adhesion capability of HeLa cells to endothelial monolayer was also significantly affected by GPIIb/IIIa and αvβ3 integrins. The arrested HeLa cells increased nearly 5-fold in the presence of thrombin-activated platelets at shear stress condition (1.84 dyn/cm2 exposure for 1 hour) than the control (static). Our findings showed that GPIIb/IIIa and αvβ3 integrins are important mediators in the pathology of cervical cancer and provide a molecular basis for the future therapy, and the efficient antitumor benefit should target multiple receptors on tumor cells and platelets.
1. Introduction
Metastasis is one of the leading causes of cancer patients' death. Tumor cells disseminate to distant organs via the lymph or the blood stream during metastasis. The metastasis includes several critical pathogenic steps which are angiogenesis, invasion into the capillary venules, circulation in the blood stream, adherence to a new local extravasation and colonization [1]. The arrest of metastasizing tumor cells within the blood stream is prerequisite for their extravasation. In the blood stream, tumor cells are exposed to flow-dependent shear forces, plasma proteins, blood cells, and platelets, all of which may affect tumor cell survival, arrest, and extravasation. Mechanisms which mediate tumor cell arrest involve adhesive interactions of tumor cells with endothelial cells. Recently, intense researches have unveiled an elaborate integrin network controlling the adhesion and migration of tumor cells [2, 3]. The integrin families overexpressed on the tumor cells have now been recognized as key regulators of various neoplastic processes by virtue of their ability to facilitating cancer cell adhesion and migration [4]. The integrins are heterodimeric adhesion receptors formed by the noncovalent association of α and β subunits. αvβ3 integrin mediates cell adhesion and migration on a variety of extracellular matrix proteins, including fibronectin, fibrinogen, laminin, collagen, osteopontin, and others [5]. However, αvβ3 integrin prefers to highly express on developing tissues rather than the normal or mature one [6]. As a class of apparent malignantly developing tissue, the aberrant expression of αvβ3 integrin has been demonstrated on various kinds of cancer including metastasis human melanoma, breast, prostate, and glioblastoma tumor cells. All these evidences lead to the confirmation that overexpression of αvβ3 integrin may be cited as a reliable index to determine the malignancy of a specific tumor [7–9]. It has been demonstrated that prostate cancer cell adhesion and migration to vitronectin and osteopontin were αvβ3-dependent. The similar pattern was also found in the model of ovarian cancer [10].
In the normal physiological condition, platelets do not attach to intact endothelium unless the platelet-endothelium interaction has been disturbed due to the vascular damage. The mechanism of coagulation directed by the aggregation of activated platelets is now known to involve two specific glycoproteins, that is, GPIb and GPIIb/IIIa (also called αIIbβ3), which is composed of two subunits which are GPIIb and GPIIIa [11, 12]. Some disorders of GPIIb/IIIa such as Glanzmann thrombasthenia show the importance of GPIIb/IIIa in mediating the natural physiological hemostasis and thrombosis. There exists a clear medical link between thrombosis and tumor metastasis. Clinical statistics showed that half of cancer patients have accompanying platelet activation and thrombosis [13–15]. Investigators have long speculated that tumor cells can induce the aggregation of platelets which will coat the former and then reduce the possible immunological attack during the hematogenous metastasis. However, how GPIIb/IIIa mediates this process under dynamic fluid stress has not been confirmed.
To investigate what are the roles of GPIIb/IIIa and αvβ3 integrins for cancer cell adhesion, migration, and metastasis, our present study was designed to explore the behaviors of HeLa cell-endothelial cell interaction under the static and dynamic flow conditions. Their contributions towards the metastasis of cervical cancer were also evaluated and to elucidate whether there exists synergistic relationship between GPIIb/IIIa and αvβ3 during mediating the interaction process of HeLa cell-endothelial cell.
2. Materials and Methods
2.1. Reagents
Cell culture medium RPMI1640 and newborn calf serum (NCS) were purchased from Gibco (Grand Island, NY, USA). Trypsin, HAT (hypoxanthine, aminopterin, and thymidine) supplement, thrombin, gelatin, penicillin, and streptomycin were obtained from Sigma-Aldrich (St. Louis, MO, USA). 2-[4-(2-Hydroxyethyl)-1-piperazine]ethanesulfonic acid (HEPES) was supplied by Amresco (Cleveland, USA). Human eptifibatide and arg-gly-asp-trp-glu peptides (RGDWE peptides) were purchased from Cali-bio (CA, USA) and SBS Genetech (Beijing, China), respectively. All other chemicals used were of analytic grade without further purification.
2.2. Cell Culture
The HUVEC line EA.Hy926 was obtained from the Institute of Biomedical Engineering of Western China Medical College (Sichuan, China). This cell line, a hybridoma of HUVEC and the human epithelial cell line A549, has been shown to retain a number of properties of endothelial cell, including the production of human factor VIII-related antigen. The cells were cultured in RPMI 1640 containing 20 mM HEPES, 10% NCS, 2% NaHCO3, 100 U/mL penicillin and 100 mg/mL streptomycin, and 2% HAT supplement at the temperature of 37°C in humidified 5% CO2 atmosphere.
HeLa cells, generous gift from Dr. Anying Zhang in our department, were also cultured in RPMI1640 medium supplemented with 10% NCS and 100 units/mL penicillin and 100 μg/mL streptomycin at 37°C in a humidified atmosphere containing 5% CO2. Prior to adhesion assay, cells were detached from 25 cm2 culture flasks (Corning, NY, USA) with 0.25% trypsin in phosphate buffered saline (PBS) (pH 7.4).
2.3. Platelet Isolation
Platelet isolation was adopted from the method established by Chiang and coworkers with some modifications [16]. Briefly, human blood was drawn by venipuncture from healthy volunteers into heparin sodium (1 U/mL) anticoagulant. Platelet-rich plasma (PRP) was prepared by centrifugation of whole blood at 120 × g for 10 minutes. Platelet-poor plasma (PPP) was obtained by further centrifugation of the blood at 500 × g for 10 minutes. The final platelet count of the PRP was adjusted to the desired levels (2 × 108/mL) with PPP. Specimens were stored at 37°C in capped polypropylene tubes and used for the following experiments.
2.4. Cell Treatment with Thrombin, Eptifibatide, and RGDWE Peptides
To potentiate platelet activation, platelets were treated for 30 minutes with thrombin (0.55 U/mL) at room temperature before incubation with HeLa cells. For inhibition studies, platelets and HeLa cells were also treated for 30 minutes with eptifibatide (0.65 μg/mL) and RGDWE peptides (425 μg/mL) to block the GPIIb/IIIa and αvβ3 integrins, respectively. Control experiments were performed in which platelets, and HeLa cells were treated exactly as stated above but in the absence of thrombin, eptifibatide, or RGDWE peptides.
2.5. Cell Migration Assay in Static Condition
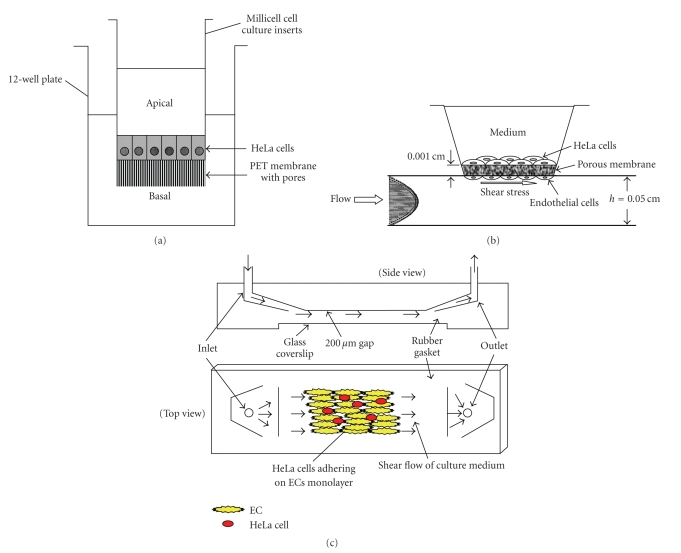
Millicell cell culture insert (Millipore, Billerica, MA, USA) containing PET membrane with pore size of 8 μm was used for HUVECs migration experimental system as described previously (Figure 1(a)) [17]. Briefly, 1.5 mL of RPMI1640 culture medium was firstly added into each well of 12-well plates, then the Millicell cell culture inserts were put in the plate wells, and 500 μL cell suspension of HeLa (5 × 104 cells) was added into the each insert. The cells were allowed to migrate for 8 hours at 37°C and 5% CO2 in the presence of thrombin-activated platelets, eptifibatide, or RGDWE peptides. The culture media were removed and the nonmigrated HeLa cells inside the PET membranes were scraped by a cotton stick. The HeLa cells that migrated through the pores and adhered onto the outer side of PET membrane were fixed and dipped in a mixed solution (5 mL) of acetic acid and methyl alcohol (1 : 3 in volume ratio) for 30 minutes after the inserts were washed twice with PBS. The PET membranes were taken out using a scalpel and dyed for 10–15 minutes with Giemsa solution (0.9%) in a glass slide. The redundant Giemsa were washed by Milli-Q water, and then the migrated HeLa cells (dyed into dark blue) were observed and recorded under an inverted microscope (TE-2000U, Nikon, Japan). The migrated cell number was quantified by cell counting from more than six microscopic fields for each sample (magnification 20×), and three PET membranes were used for each experimental group.
Figure 1.
Schematic illustrations of Millicell cell culture insert system with 8 μm-pore size for migration and invasion assay in static condition (a), coculture flow system for migration assay (b), and parallel flow chamber system for adhesion assay (c).
2.6. Cell Invasion Assay
HeLa cell invasion was also examined by modified Millicell cell culture insert. The inner side of PET membrane (Figure 1(a)) was modified to be precoated with 100 μL gelatin (1 mg/mL) overnight. Before cell invasion experiment, HeLa cells were firstly labelled with 10 μM DiO fluorescent dyes (Beyotime, Beijing, China) for 20 minutes, and washed three times by centrifugation at 1700 rpm, 6 minutes for each time, to remove the abundant DiO fluorescent molecules. The labelled HeLa cell suspension of 500 μL (5 × 104 cells) in RPMI 1640 with 10% NCS was seeded onto the inner side of PET membrane of the Millicell cell culture insert. One and half milliliters of RPMI 1640 with 10% NCS culture medium were added into the wells of the 12-well plates. Invasion was detected after 24-hour incubation at 37°C and 5% CO2. The culture media in the cell culture inserts were removed and washed three times with PBS. Cells in the inner side of PET membrane were gently wiped away by cotton stick. HeLa cells that invaded to the outer side of the PET membrane were quantified by cell counting under an inverted fluorescent microscope TE-2000U from more than five random microscopic fields (magnification 10×).
2.7. Blood Flow Simulation
Cell coculture parallel flow system [18], designed and presented by Professor Jeng-Jiann Chiu Lab in the National Health Research Institutes of Taiwan, was used for transmembrane migration assay combining cell coculture and dynamic flow conditions (Figure 1(b)). Two sets of glass slides and silicone gaskets were fastened by vacuum suction through ports with a polycarbonate insert holder, which was machined precisely to allow the incorporation of the coculture module into a channel cut in the lower gasket. The chamber allows direct observation of the cells during flow experiment via the observation window opened in the upper gasket. The chamber was connected to a perfusion loop system. The fluid medium entered at a port through slit into the channel, and exited through another slit. The HUVECs side of the co-culture was subjected to shear flow, while the opposite side with HeLa cells was maintained in a static condition.
A rectangular parallel plate perfusion chamber [19], also designed and presented by Professor Jeng-Jiann Chiu Lab in the National Health Research Institutes of Taiwan, was used to examine adhesion of HeLa cells to cultured HUVECs monolayer under shear flow condition (Figure 1(c)). This system comprises a transparent polymethylmethacrylate plate, two silastic rubber gaskets, and a standard glass coverslip. The coverslip with near 90% confluent monolayer of HUVECs was mounted over the groove with the cells facing the inside, and an approximate 500 μm high gap was formed over the HUVECs.
The wall shear stress (τw) is related to the volumetric flow rate (Q) by τw = 6μQ/w(h)2, where μ is the fluid viscosity, w is the width of the flow field, and h is the height. The shear stress can be regulated through flow rate of Q. The chamber was placed on the stage of an inverted microscope.
2.8. Cell Migration Assay under Hela Cells/HUVECs Coculture and Shear Flow
HUVECs were seeded onto the outer side of the PET membrane at a density of 2 × 105 cells/mL. We kept the insert in an incubator at 37°C for 6 hours to allow HUVECs to adhere to the outer side of the PET membrane and then turned up the insert to seed DiO labelled HeLa cells (500 μL cell suspension containing 5 × 104 cells) onto the inner side of PET membrane. The cocultured insert was set into co-culture flow system to expose shear stress (8 dyn/cm2) for 8 hours. The procedures for HeLa cell labeling and the counting of migrated HeLa cell numbers were mentioned above (see Cell Invasion Assay). The migrated HeLa cells were quantified by cell counting from more than six random microscopic fields for each sample (magnification 10×).
2.9. Cell Adhesion Assay under Shear Flow
The adhesion assay under flow was adopted from the method established by Chiu and coworkers [19]. HUVECs were preseeded on a coverslip at a cell concentration of 2 × 106/mL and incubated for 48 hours. To facilitate their visualization against the background of monolayer endothelial cells, HeLa cells were labelled by the method as mentioned above (see Cell Invasion Assay). DiO-labelled HeLa cell suspension (1 mL) at the concentration of 1 × 105 cells/mL was also seeded to the same coverslip (with HUVECs monolayer) and incubated for 6 hours. The co-cultured coverslip was fixed in the flow chamber for continuous shear stress exposure (1.84 dyn/cm2, 1 hour). The adhesion capability was evaluated by calculating the ratio of the number of static adhesive cells (0 dyn/cm2, control) to that of shear flow condition (1.84 dyn/cm2, I hour) under fluorescent microscope. The adhered HeLa cell number on the HUVECs monolayer was quantified by cell counting from more than ten random microscopic fields for each sample (magnification 10×).
2.10. Presentation of Data and Statistical Analysis
Data are presented as mean ± standard deviation (SD). The statistical significance of differences was tested using two-tailed Student's t-test, and P < .05 was considered to be significant.
3. Results
3.1. Role of GPIIb/IIIa, αvβ3 Integrins, and Endothelial Cells on HeLa Cell Migration
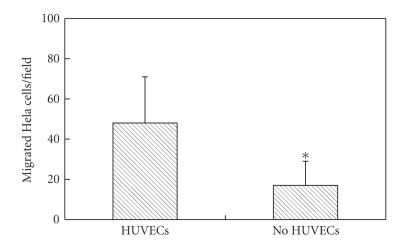
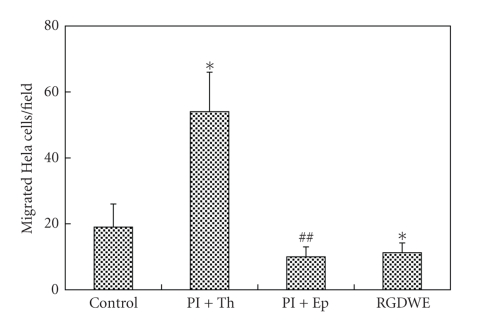
Migrated HeLa cell number significantly increases in the presence of HUVECs than the control (no HUVECs culture on the bottom of wells) as shown in Figure 2. We next examined how GPIIb/IIIa and αvβ3 integrins affect HeLa cell migration in static condition. Activation of platelets by thrombin leads to remarkably increasing migration ability of HeLa cell. However, migrated cell number decreases after inhibition of GPIIb/IIIa and αvβ3 integrins by eptifibatide and RGDWE peptides, respectively (Figure 3).
Figure 2.
HUVECs induced HeLa cell migration. HUVECs (1 × 106 cells/mL) were seeded onto the bottom of 12-well plate before the inserts were set into the plate wells. The cells were allowed to migrate for 8 hours at 37°C and 5% CO2. The numbers of migrated HeLa cells were quantified by cell counting from more than six micrographic fields using magnification of 20×. *P < .05 no HUVECs versus HUVECs.
Figure 3.
Migration of HeLa cells in the presence of platelets (Pl), thrombin (Th), eptifibatide (Ep), or RGDWE peptides (RGDWE). Cells were allowed to migrate for 8 hours at 37°C and 5% CO2. Each data point is the mean of more than six micrographic fields using magnification of 20×. Pl+Th: in the presence of thrombin-activated platelets; Pl+Ep: thrombin-activated platelets treated with eptifibatide (Ep); RGDWE: HeLa cells were treated with RGDWE peptides to block αvβ3 integrin. Control is considered as the sample of equal volume of cell culture medium added. *P < .05 (Pl+Th), RGDWE versus control; ##P < .01 (Pl+Ep) versus (Pl+Th).
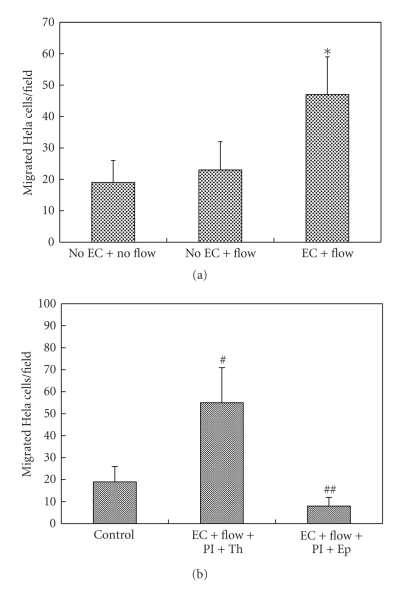
3.2. GPIIb/IIIa and αvβ3 Integrins Mediate HeLa Cell Transmigration under Coculture Flow Condition
Furthermore, we questioned whether the above-mentioned HeLa cell migrating phenomenon exists in dynamic flow condition, and whether shear flow also contributes to cell migration. Therefore, HUVECs were seeded onto the outer side of PET membrane and exposed to shear stress (8 dyn/cm2, 8 hours) as shown in Figure 1(b). The migrated HeLa cell number enhances under shear flow in the presence of HUVECs monolayer (Figure 4(a)), and migration also greatly augments when the platelets were activated by thrombin (Figure 4(b)). It is very similar to the static culture condition.
Figure 4.
HeLa cell migration under shear flow in HeLa cells/HUVECs coculture parallel flow system. HeLa cells labelled by DiO were cultured onto the inner side of insert PET membrane, and the outer side seeded with HUVECs was exposed to 8 dyn/cm2 shear flow for 8 hours. The numbers of migrated HeLa cells were quantified by cell counting from more than six micrographic fields using magnification of 20×. (a) Flow and monolayer endothelium induced HeLa cells migration. *P < .05 (EC+flow) versus (No EC+flow). (b) Migration of HeLa cells in the presence of thrombin-activated platelets (Pl+Th) or activated platelets with eptifibatide (Pl+Ep) under the above-mentioned flow condition. #P < .05 versus control: ##P < .01 (Pl+Ep) versus (Pl+Th). Control is considered as the sample of equal volume of cell culture medium added.
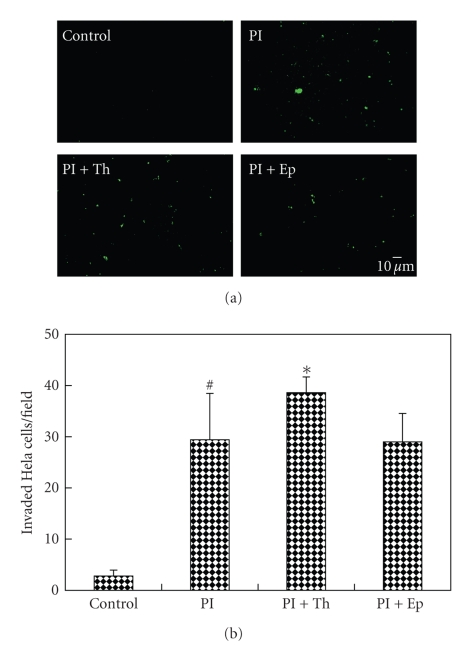
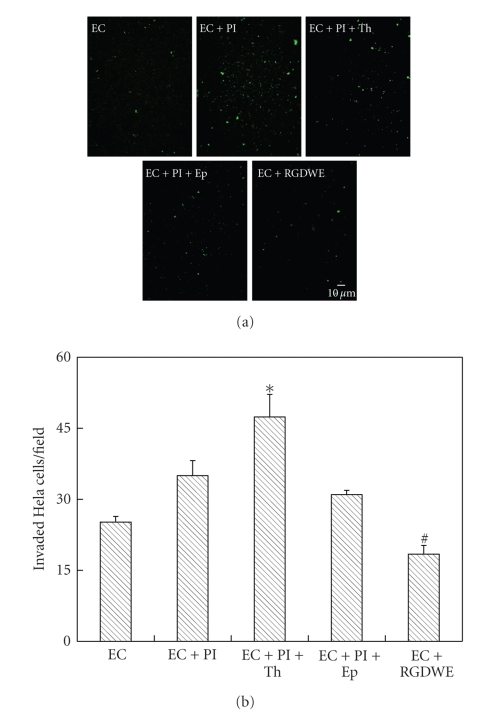
3.3. GPIIb/IIIa and αvβ3 Integrins Induce Invasion of HeLa Cells In Vitro
The invaded HeLa cell number obviously increased comparing with the control (the sample of equal volume of cell culture medium added), and invasion ability of HeLa cells also enhanced in the presence of thrombin-activated platelets (Figure 5). To further confirm the potential roles of platelet during HeLa cell invasion, eptifibatide, a specific inhibitor of platelet GPIIb/IIIa integrin, was added after platelet activation. It was found that the invaded number of HeLa cell decreased and recovered near to the level in the presence of platelet alone (Figure 5). In the prior experiments (Figures 2 and 4(a)), it was demonstrated that endothelial cells could significantly enhance and induce HeLa cell migration regardless of HUVECs seeded onto the well bottom of plate or the outer side of PET membrane. Here, the transmembrane invasion ability of HeLa cells was also evaluated in the presence of HUVECs seeded onto the outer side of PET membrane. It was shown that the invaded cell numbers of HeLa were relative higher than that of without HUVECs, and the cell invasion tendency in the presence of HUVECs was also very similar by comparing with Figures 5 and 6. Moreover, specific blocking of αvβ3 integrin by RGDWE peptides led to a decrease of the invaded cell number (Figure 6).
Figure 5.
Transmembrane invasion of HeLa cells through PET membrane precoated with gelatin. (a) representative images of HeLa cells invasion (labelled into green) and (b) the statistical data of invaded HeLa cell numbers in various conditions. The numbers of invaded HeLa cells were quantified by cell counting from more than five micrographic fields using magnification of 10×. Pl: in the presence of platelets; Pl+Th: in the presence of thrombin-activated platelets; Pl+Ep: thrombin-activated platelets treated with eptifibatide; RGDWE: HeLa cells were treated with RGDWE peptides to block αvβ3 integrin. *P < .05 (Pl+Th) versus Pl or (Pl+Ep); #P < .05 Pl versus control. Control is considered as the sample of equal volume of cell culture medium added.
Figure 6.
Transmembrane invasion of HeLa cells through PET membrane precoated with gelatin and a monolayer of HUVECs cultured in the outer side of PET membrane. The numbers of invaded HeLa cells (labelled into green) were quantified by cell counting from more than five micrographic fields using magnification of 10×. EC: HUVECs cultured on the outer side of PET membrane. EC+Pl: in the presence of HUVECs monolayer and platelet; EC+Pl+Th: in the presence of HUVECs monolayer and thrombin-activated platelets; EC+Pl+Ep: in the presence of HUVECs monolayer and thrombin-activated platelets treated with eptifibatide; EC+RGDWE: in the presence of HUVECs monolayer and HeLa cells with RGDWE peptides blocked αvβ3 integrin. *P < .05 (EC+Pl+Th) versus (EC+Pl) or (EC+Pl+Ep); #P < .05 (EC+RGDWE) versus EC.
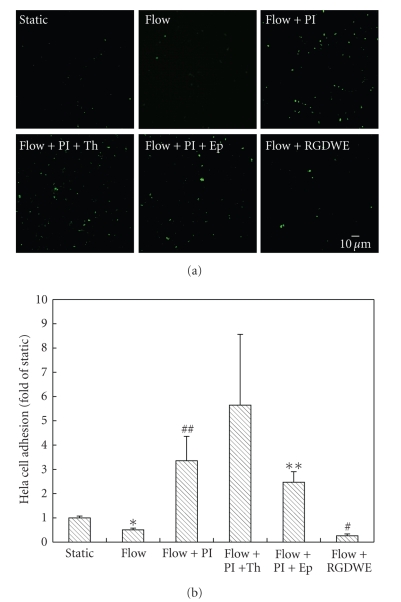
3.4. GPIIb/IIIa and αvβ3 Integrins Participate HeLa Cell Adhesion on Monolayer Endothelial Cells under Shear Flow
To examine the possibility that GPIIb/IIIa and αvβ3 integrins could also regulate HeLa cell adhesion on monolayer endothelial cells under shear flow, parallel flow chamber system was used to simulate the blood flow for the study of HeLa cell adhesion behavior. The number of adhered HeLa cells increased when platelets were present in the perfusion medium, and it enhanced remarkably (nearly 5-fold of the static case) after the platelets activation by thrombin under a low shear stress condition of 1.84 dyn/cm2 for 1 hour. By blocking the GPIIb/IIIa integrin on platelets and αvβ3 integrin on HeLa cells using eptifibatide and RGDWE peptides, respectively, the adhered HeLa cells on monolayer HUVECs significantly decreased (Figure 7), which indicated that GPIIb/IIIa and αvβ3 integrins participated in the adhesion interaction of cancer cells and endothelial cells.
Figure 7.
Effect of platelets, thrombin, eptifibatide, and RGDWE peptides on adhesion of HeLa cells to HUVECs monolayer under static (0 dyn/cm2) and low shear stress conditions (1.84 dyn/cm2, 1 hour). (b) and (c) are the representative images of HeLa cells adhesion (labelled into green) and the statistical data of adhered HeLa cell numbers in various conditions, respectively. The numbers of adhered HeLa cells were quantified by cell counting from more than ten micrographic fields using magnification of 10×. *P < .05 flow versus static; **P < .01 (Flow+Pl+Ep) versus (Flow+Pl+Th); #P < .05 (Flow+RGDWE); ##P < .01 (Flow+Pl) versus Flow.
4. Discussion
Although the formation of metastasis requires the successful completion of several sequential interrelated steps by the cancer cells, interaction of cancer cells and host cells in blood vessel plays an important role in the final metastasis formation. So a thorough understanding of the mechanisms how the platelet-cancer cell interaction regulates cancer metastasis could help researchers develop new therapeutic interventions [20–22]. In this study, our focus centers on the aggregation or not of cancer cells with platelets through GPIIb/IIIa and αvβ3 integrins whether it contributes to HeLa cell migration, invasion, and adhesion both in static and dynamic flow conditions.
In our present work, we used the Millicell cell culture insert system to investigate HeLa cell transmigration and invasion in vitro. In static condition, HeLa cell transmembrane migration and invasion increased significantly in the presence of thrombin-activated platelets and recovered to normal after the platelet GPIIb/IIIa integrin was blocked by eptifibatide both in static and co-culture flow system conditions (Figures 3, 4, and 5). These data provided strong evidences that platelet GPIIb/IIIa integrin participated and mediated HeLa cells migration. The number of HeLa cells that invade through gelatin matrix in the presence of platelets is approximately 10-fold higher than control condition while in the presence of thrombin-activated platelets is only near 12-fold of control (Figure 5). These results suggest that HeLa cells may induce platelet activation through GPIIb/IIIa activation and therefore induce HeLa cell-platelet interaction or that other integrins might be involved [23, 24]. This interaction of cancer cells-platelets could promote not only platelet aggregation but also the expression of matrix metalloproteinases that are involved in the matrix degradation and invasion process. It was reported that αvβ3 integrin overexpressed on the HeLa cell surfaces, and which could bind to GPIIb/IIIa integrin [25]. Further study showed that the number of migrated HeLa cells decreased after the αvβ3 integrin was specifically blocked by RGDWE peptides (Figures 3 and 6). It suggested that GPIIb/IIIa and αvβ3 integrins will cooperate to mediate HeLa cell migration, or that there was a synergic effect when GPIIb/IIIa and αvβ3 integrins were activated. Because cancer cell does not only interact with platelets, leucocytes and endothelial cells were also involved. Published data have provided evidence that leucocytes facilitated melanoma cell adhesion [26]. Here, we found that HeLa cell migration was remarkably affected whether the endothelial cells were cultured on plate wells or the outer side PET membrane (Figures 2, 4, and 6). Endothelial cells enhanced HeLa cell migration both in static and shear flow conditions, suggesting that endothelial cells could secrete some cytokines or chemoattractants to induce HeLa cell transmigration, for instance, basic fibroblast growth factor and vascular endothelial growth factor.
We also used a laminar flow chamber to further assay HeLa cell adhesion under shear stress conditions to mimic the in vivo situation. Under physiological conditions, tumor cells which are under the hematogenous metastasis are exposed to a wide range of mechanical shear stresses from blood flow. This dynamic fluid system definitely impinges on the motion of individual tumor cells, especially their behaviors of adhesion to the endothelium. The relevant reports which focus on the behavior of the cell adhesion under dynamic condition are rare [27].
Interestingly, results shown in Figure 7 indicated that the capability of HeLa cell adhesion to endothelium is significantly affected by GPIIb/IIIa and αvβ3 integrins. Previous studies have shown that the activated platelets can also bind to the cancer cells via GPIIb/IIIa and αvβ3 interaction through the bridges of fibronectin, fibrinogen, or von Willebrand factor. So it could be speculated that more HeLa cells would be arrested on the endothelial cells via the P-selectin and its ligand PSGL-1 is present on endothelium [28, 29]. The aggregation of platelets will strengthen cancer cell adhesion and migration. Our data support the hypothesis, and a new model that activated platelets will adhere to cancer cells via GPIIb/IIIa and αvβ3 interaction to form a loosed platelet coating on cancer surface, which will lead to cancer cells to reduce or avoid shear stress exposure and also assist more cancer cell adhesion [30, 31]. On the other hand, the activated platelets aggregated to form tiny local thrombus, and resulting in local blood viscosity enhanced to provide more chance for cancer cell adhesion [32–35]. Moreover, cancer cell-induced platelet activation possibly amplifies cancer cell adhesion to endothelium to some extent [36]. Our investigation further demonstrated that cell migration, invasion, and adhesion were also highly regulated by αvβ3 integrin on the HeLa cells. These results might add a new aspect why the majority of actively metastatic tumors were found to highly express αvβ3 integrin.
Taken together, the present work demonstrates a novel role for GPIIb/IIIa and αvβ3 integrins in supporting the HeLa cell migration, invasion, and adhesion. The presence of platelets and their activated state resulted in enhancement of HeLa cell transmigration and cell recruitment to HUVECs monolayer under shear flow. These findings promote our understanding of the roles of GPIIb/IIIa and αvβ3 integrins in cancer metastasis, which could be a new strategy to cancer treatment.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (30700151), by Starting Funds (Y02002010901008), and Innovative Talent Incubation Program for Youth (Y02018023601062) from UETSC. The authors would also thank Professor Jeng-Jiann Chiu in National Health Research Institutes of Taiwan, for kind gifts of parallel flow chamber and coculture flow system, and Professor Zili You in this department for cell culture help and facilities.
References
- 1.Felding-Habermann B, Habermann R, Saldívar E, Ruggeri ZM. Role of β3 integrins in melanoma cell adhesion to activated platelets under flow. The Journal of Biological Chemistry. 1996;271(10):5892–5900. doi: 10.1074/jbc.271.10.5892. [DOI] [PubMed] [Google Scholar]
- 2.Hughes PE, Diaz-Gonzalez F, Leong L, et al. Breaking the integrin hinge: a defined structural constraint regulates integrin signaling. The Journal of Biological Chemistry. 1996;271(12):6571–6574. doi: 10.1074/jbc.271.12.6571. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz MA, DeSimone DW. Cell adhesion receptors in mechanotransduction. Current Opinion in Cell Biology. 2008;20(5):551–556. doi: 10.1016/j.ceb.2008.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bombeli T, Schwartz BR, Harlan JM. Adhesion of activated platelets to endothelial cells: evidence for a GPIIbIIIa-dependent bridging mechanism and novel roles for endothelial intercellular adhesion molecule 1 (ICAM-1), αvβ3 integrin, and GPIbα. Journal of Experimental Medicine. 1998;187(3):329–339. doi: 10.1084/jem.187.3.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pécheur I, Peyruchaud O, Serre CM, et al. Integrin αvβ3 expression confers on tumor cells a greater propensity to metastasize to bone. The FASEB Journal. 2002;16(10):1266–1268. doi: 10.1096/fj.01-0911fje. [DOI] [PubMed] [Google Scholar]
- 6.Pilch J, Habermann R, Felding-Habermann B. Unique ability of integrin αvβ3 to support tumor cell arrest under dynamic flow conditions. The Journal of Biological Chemistry. 2002;277(24):21930–21938. doi: 10.1074/jbc.M201630200. [DOI] [PubMed] [Google Scholar]
- 7.Chen Y-P, O'Toole TE, Ylanne J, Rosa J-P, Ginsberg MH. A point mutation in the integrin β3 cytoplasmic domain (S752—>P) impairs bidirectional signaling through α(IIb)β3 (platelet glycoprotein IIb-IIIa) Blood. 1994;84(6):1857–1865. [PubMed] [Google Scholar]
- 8.Rolli M, Fransvea E, Pilch J, Saven A, Felding-Habermann B. Activated integrin αvβ3 cooperates with metalloproteinase MMP-9 in regulating migration of metastatic breast cancer cells. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(16):9482–9487. doi: 10.1073/pnas.1633689100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao Y, Bachelier R, Treilleux I, et al. Tumor αvβ3 integrin is a therapeutic target for breast cancer bone metastases. Cancer Research. 2007;67(12):5821–5830. doi: 10.1158/0008-5472.CAN-06-4499. [DOI] [PubMed] [Google Scholar]
- 10.Tremblay P-L, Huot J, Auger FA. Mechanisms by which E-selectin regulates diapedesis of colon cancer cells under flow conditions. Cancer Research. 2008;68(13):5167–5176. doi: 10.1158/0008-5472.CAN-08-1229. [DOI] [PubMed] [Google Scholar]
- 11.Han J, Lim CJ, Watanabe N, et al. Reconstructing and deconstructing agonist-induced activation of integrin αIIbβ3. Current Biology. 2006;16(18):1796–1806. doi: 10.1016/j.cub.2006.08.035. [DOI] [PubMed] [Google Scholar]
- 12.Jy W, Horstman LL, Park H, Mao W-W, Valant P, Ahn YS. Platelet aggregates as markers of platelet activation: characterization of flow cytometric method suitable for clinical applications. American Journal of Hematology. 1998;57(1):33–42. doi: 10.1002/(sici)1096-8652(199801)57:1<33::aid-ajh6>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 13.Abulencia JP, Tien N, McCarty OJT, Plymire D, Mousa SA, Konstantopoulos K. Comparative antiplatelet efficacy of a novel, nonpeptide GPIIb/IIIa antagonist (XV454) and abciximab (c7E3) in flow models of thrombosis. Arteriosclerosis, Thrombosis, and Vascular Biology. 2001;21(1):149–156. doi: 10.1161/01.atv.21.1.149. [DOI] [PubMed] [Google Scholar]
- 14.Im JH, Fu W, Wang H, et al. Coagulation facilitates tumor cell spreading in the pulmonary vasculature during early metastatic colony formation. Cancer Research. 2004;64(23):8613–8619. doi: 10.1158/0008-5472.CAN-04-2078. [DOI] [PubMed] [Google Scholar]
- 15.Nieswandt B, Moser M, Pleines I, et al. Loss of talin1 in platelets abrogates integrin activation, platelet aggregation, and thrombus formation in vitro and in vivo. Journal of Experimental Medicine. 2007;204(13):3113–3118. doi: 10.1084/jem.20071827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiang H-S, Yang R-S, Huang T-F. The Arg-Gly-Asp-containing peptide, rhodostomin, inhibits in vitro cell adhesion to extracellular matrices and platelet aggregation caused by Saos-2 human osteosarcoma cells. British Journal of Cancer. 1995;71(2):265–270. doi: 10.1038/bjc.1995.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu Y, Yang H, Otaka K, Takatsuki H, Sakanishi A. Effects of vascular endothelial growth factor (VEGF) and chondroitin sulfate a on human monocytic THP-1 cell migration. Colloids and Surfaces B. 2005;43(3-4):216–220. doi: 10.1016/j.colsurfb.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 18.Chiu J-J, Chen L-J, Chen C-N, Lee P-L, Lee C-I. A model for studying the effect of shear stress on interactions between vascular endothelial cells and smooth muscle cells. Journal of Biomechanics. 2004;37(4):531–539. doi: 10.1016/j.jbiomech.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 19.Chiu J-J, Chen C-N, Lee P-L, et al. Analysis of the effect of disturbed flow on monocytic adhesion to endothelial cells. Journal of Biomechanics. 2003;36(12):1883–1895. doi: 10.1016/s0021-9290(03)00210-0. [DOI] [PubMed] [Google Scholar]
- 20.Alon R, Ley K. Cells on the run: shear-regulated integrin activation in leukocyte rolling and arrest on endothelial cells. Current Opinion in Cell Biology. 2008;20(5):525–532. doi: 10.1016/j.ceb.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cosemans JMEM, Iserbyt BF, Deckmyn H, Heemskerk JWM. Multiple ways to switch platelet integrins on and off. Journal of Thrombosis and Haemostasis. 2008;6(8):1253–1261. doi: 10.1111/j.1538-7836.2008.03041.x. [DOI] [PubMed] [Google Scholar]
- 22.Craig DH, Gayer CP, Schaubert KL, et al. Increased extracellular pressure enhances cancer cell integrin-binding affinity through phosphorylation of β1-integrin at threonine 788/789. American Journal of Physiology. 2009;296(1):C193–C204. doi: 10.1152/ajpcell.00355.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Basson MD. An intracellular signal pathway that regulates cancer cell adhesion in response to extracellular forces. Cancer Research. 2008;68(1):2–4. doi: 10.1158/0008-5472.CAN-07-2992. [DOI] [PubMed] [Google Scholar]
- 24.Lawler K, Meade G, O'Sullivan G, Kenny D. Shear stress modulates the interaction of platelet-secreted matrix proteins with tumor cells through the integrin αvβ3. American Journal of Physiology. 2004;287(5):C1320–C1327. doi: 10.1152/ajpcell.00159.2004. [DOI] [PubMed] [Google Scholar]
- 25.McCarty OJT, Jadhav S, Burdick MM, Bell WR, Konstantopoulos K. Fluid shear regulates the kinetics and molecular mechanisms of activation-dependent platelet binding to colon carcinoma cells. Biophysical Journal. 2002;83(2):836–848. doi: 10.1016/S0006-3495(02)75212-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liang S, Slattery MJ, Dong C. Shear stress and shear rate differentially affect the multi-step process of leukocyte-facilitated melanoma adhesion. Experimental Cell Research. 2005;310(2):282–292. doi: 10.1016/j.yexcr.2005.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burdick MM, McCaffery JM, Kim YS, Bochner BS, Konstantopoulos K. Colon carcinoma cell glycolipids, integrins, and other glycoproteins mediate adhesion to HUVECs under flow. American Journal of Physiology. 2003;284(4):C977–C987. doi: 10.1152/ajpcell.00423.2002. [DOI] [PubMed] [Google Scholar]
- 28.Theilmeier G, Lenaerts T, Remacle C, Collen D, Vermylen J, Hoylaerts MF. Circulating activated platelets assist THP-1 monocytoid/endothelial cell interaction under shear stress. Blood. 1999;94(8):2725–2734. [PubMed] [Google Scholar]
- 29.Watanabe N, Bodin L, Pandey M, et al. Mechanisms and consequences of agonist-induced talin recruitment to platelet integrin αIIbβ3. Journal of Cell Biology. 2008;181(7):1211–1222. doi: 10.1083/jcb.200803094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nieswandt B, Hafner M, Echtenacher B, Männel DN. Lysis of tumor cells by natural killer cells in mice is impeded by platelets. Cancer Research. 1999;59(6):1295–1300. [PubMed] [Google Scholar]
- 31.Palumbo JS, Talmage KE, Massari JV, et al. Platelets and fibrin(ogen) increase metastatic potential by impeding natural killer cell-mediated elimination of tumor cells. Blood. 2005;105(1):178–185. doi: 10.1182/blood-2004-06-2272. [DOI] [PubMed] [Google Scholar]
- 32.Kunita A, Kashima TG, Morishita Y, et al. The platelet aggregation-inducing factor aggrus/podoplanin promotes pulmonary metastasis. American Journal of Pathology. 2007;170(4):1337–1347. doi: 10.2353/ajpath.2007.060790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sierko E, Wojtukiewicz MZ. Platelets and angiogenesis in malignancy. Seminars in Thrombosis and Hemostasis. 2004;30(1):95–108. doi: 10.1055/s-2004-822974. [DOI] [PubMed] [Google Scholar]
- 34.Sierko E, Wojtukiewicz MZ. Inhibition of platelet function: does it offer a chance of better cancer progression control? Seminars in Thrombosis and Hemostasis. 2007;33(7):712–721. doi: 10.1055/s-2007-991540. [DOI] [PubMed] [Google Scholar]
- 35.Tomita M, Shimizu T, Hara M, Ayabe T, Onitsuka T. Prognostic impact of thrombocytosis in resectable non-small cell lung cancer. Interactive Cardiovascular and Thoracic Surgery. 2008;7(4):613–615. doi: 10.1510/icvts.2007.174391. [DOI] [PubMed] [Google Scholar]
- 36.Bastida E, Ordinas A. Platelet contribution to the formation of metastatic foci: the role of cancer cell-induced platelet activation. Haemostasis. 1988;18(1):29–36. doi: 10.1159/000215780. [DOI] [PubMed] [Google Scholar]