Abstract
Background
Phonation threshold flow (PTF) may provide a tool to assess laryngeal function and could differentiate between normal and pathological voices. Both polyps and nodules contribute to an increased PTF by creating an incomplete glottal closure and increased vocal fold mass and thickness.
Study Design
Prospective study.
Methods
The Kay Elemetrics Phonatory Aerodynamic System (PAS) was used to collect mean flow rate (MFR) and PTF measurements from 40 normal subjects, 21 patients with vocal fold nodules, and 23 patients with vocal fold polyps. Gender based differences were assessed using a t-test. The effect of vocal pathology on PTF and MFR was determined with an ANOVA. Diagnostic potential was evaluated using a receiver operation characteristics (ROC) analysis.
Results
Both PTF (p=0.047) and MFR (p=0.008) were significantly affected by gender. Using a two-way ANOVA and correcting for gender differences, the influence of pathology on PTF was determined to be significant (p<0.001). Post-hoc tests found a significant difference between normal and polyp subjects (p<0.001), but not normal and nodule subjects (p=0.177) or nodule and polyp subjects (p=0.246). ROC analysis found that PTF (AUC=0.691) and MFR (AUC=0.684) had a similar diagnostic utility.
Conclusions
PTF can be used to differentiate between normal and pathological voices. As a parameter which is experimentally sensitive to the biomechanical parameters providing its theoretical basis, it could be used clinically to analyze laryngeal functionality. Future research could focus on measuring PTF in other pathologies, such as paralysis or scarring, which would also affect the effort required to produce voice.
Keywords: Phonation threshold flow, mean flow rate, vocal nodules, vocal polyps
INTRODUCTION
Nodules and polyps are two of the most common vocal pathologies seen in the clinical setting. A nodule is a callous-like formation on the vocal folds generally displaying bilateral symmetry and associated with less severe symptoms than polyps.1,2 Vocal therapy is the treatment of choice for nodules with surgery reserved for those cases that do not respond to initial voice therapy.1 Polyps are unilateral masses of the vocal folds associated with more severe symptoms.1,3,4 While patients with less severe or translucent polyps have been reported to benefit from voice therapy,5 most patients undergo concurrent surgery to address the mass.1,2 Both nodules and polyps cause breathiness, vocal fatigue, a decrease in mucosal vibrations and incomplete glottal closure.3 Diagnosis is most commonly made according to videostroboscopy because acoustic and aerodynamic parameters have struggled to achieve high reliability and diagnostic power.4 Imaging provides a picture of the system, but does not give insight into its functionality. An aerodynamic parameter could assess the way changes observed with videostroboscopy have affected the energy transducing capabilities of the larynx. Additionally, diagnosis based on multiple parameters provides an improved capability to differentiate between polyps and nodules.1 Multiple parameter diagnosis in a clinical setting requires the establishment of a reliable, easily measured aerodynamic parameter.
Many researchers have used aerodynamic parameters to investigate vocal health.6,7 In addition to providing information about normal phonation, aerodynamic analysis shows promise in differentiating pathologic from normal voices.7,8 Of particular interest are phonation threshold pressure (PTP) and phonation threshold flow (PTF) which hold diagnostic promise. Studied in 1975 by Baer, PTP reflects the ease of phonation by measuring the subglottal pressure required for voicing.9-11 Early PTP measurements were highly invasive, requiring direct measurements of subglottal pressure using a tracheal puncture.12 Building on the theory that intraoral pressure equals subglottal pressure during unvoiced stop consonants, researchers developed a noninvasive means of measuring PTP by having subjects pronounce /papapa/ while measuring intraoral pressure. Although promising, this method required extensive training to generate meaningful meansurements.13 Mechanical airflow interruption techniques now provide an alternative method to measure PTP not dependent on subject-controlled interruption.10,14
Jiang and Tao proposed PTF as a measure of the airflow necessary to produce phonation.15 PTF is defined by the equation:
UPTF is phonation threshold flow, B is the damping coefficient, c is mucosal wave velocity, L is vocal fold length, x0 is neutral glottal width, T is vocal fold thickness, and ρ is glottal airflow density. As the airflow alternative to PTP, PTF also provides a measure of the ease of phonation. Jiang and Tao predicted that PTF could be sensitive to subtle changes in laryngeal tissue properties, glottal configuration and vocal tract loading.15 Studies focusing on vocal fold masses found that both polyps and nodules increase airflow by preventing complete glottal closure, thereby increasing air leakage.4 Additionally, a greater driving force is required to set the more massive vocal folds into vibration, further increasing the airflow.4 Hottinger et al. used an excised larynx setup to test the responsiveness of PTP and PTF to changes in glottal width by using shims to alter vocal fold abduction. They found that while PTP showed little change in response to variations in vocal fold abduction, PTF was highly responsive.16 Jiang and Tao proposed pressure recovery at the glottis as the mechanism for this difference and suggested that PTF was the better parameter for the study of pathologies involving an incomplete glottal closure.17 Further studies of PTP and PTF revealed that both parameters were affected by the hysteresis phenomenon, where the onset value for a parameter differs from its offset. Regner et al. demonstrated that onset PTF, the airflow required to initiate phonation, is higher than offset PTF, the airflow at the point phonation ceases. As phonation is commonly associated with a prephonatory airflow peak, taking PTF measurements at the offset of phonation provides a more accurate measure of airflow threshold.18 PTF measurements may be accomplished using an extraoral flow transducer based on the assumption that the vocal tract is continuous, with oral airflow being approximately equal to glottal airflow. An anesthesia type airflow mask can be used for this, making it especially promising for use in the clinical setting.15 The Kay Elemetrics Phonatory Aerodynamic System (PAS) has been used to measure airflow with success.7
This study evaluated PTF among subjects with normal vocal folds, subjects with vocal nodules, and subjects with vocal polyps to determine if it differed according to subject diagnosis. PTF measurements were recorded from 40 normal subjects, 21 subjects with vocal nodules and 23 subjects with vocal polyps using the PAS.
MATERIALS AND METHODS
Subjects
The study compared 40 normal speakers with no history of vocal pathologies, 21 patients with stroboscopically confirmed vocal fold nodules, and 23 patients with stroboscopically confirmed vocal fold polyps. Vocal pathology subjects were recruited from the Shanghai EENT Hospital of Fudan University where they were diagnosed and reviewed by the same board certified physician. Vocal polyp patients had a mean age of 34.6±11.7 (Range: 28 to 60), while patients with vocal nodules had a mean age of 39.3±8.89 (Range: 25 to 54). As PTF may be influenced by race and age, control subjects were recruited from the faculty at Fudan University and were of similar race and age as subjects in both experimental groups (42.7±8.20, Range: 19 to 59). A t-test confirmed that the remaining age differences between the groups did not significantly influence PTF (p=0.507) or mean flow rate (MFR) (p=0.870). The polyp group was comprised of 12 female subjects and 11 male subjects. Of the 40 normal subjects, 21 were female and 19 were male. Nodules are much more common in females19; therefore, the nodule group contained only female subjects. Gender based aerodynamic measures were corrected for by using a two-way ANOVA for parameter evaluation. All subjects recruited were free of respiratory, neurological, psychiatric, and auditory problems. None of the subjects were professional vocalists nor had any received vocal training. The nodule patients selected for this study all displayed bilaterally symmetrical masses located on the medial surface, near the junction of the anterior and middle third of the vocal fold. Polyp subjects all displayed a unilateral broad-based mass that was less than approximately 4 mm in diameter, located on the free edge of the vocal fold.
Data Collection
Prior to collecting data, the protocol was approved by the Institutional Review Board of the University of Wisconsin-Madison and the Ethics Committee of the Shanghai Eye, Ear, Nose, and Throat Hospital of Fudan University. Airflow and sound pressure level (SPL) recordings were made with the Kay Elemetrics Phonatory Aerodynamic System (PAS), model 6800, as directed by the manufacturer. Subjects were allowed to practice until they felt comfortable with the procedure. Subjects phonated a sustained /a/ into a cardboard tube placed so that it rested above the tongue approximately one inch into the mouth. For MFR recordings subjects maintained an intensity of 72 dB, using visual feedback, for two to three seconds. Measurements of SPL in dB and airflow in liters/second were made during the course of phonation. The MFR trial was repeated five times with subjects resting for three to five seconds between recordings. For PTF measurement, subjects were instructed to initiate phonation at a soft intensity and decrease intensity over three to five seconds until no phonation was detected. The short recording time prevented the potentially confounding effect of vocal fatigue from having an impact. Recordings of the SPL in dB and airflow in liters/second were made during the course of the phonation. PTF was estimated as the airflow at the point where phonation ceased. The cessation in phonation was defined as the point where SPL decreased to the level of ambient noise in the room, which was determined to be approximately 50 dB (Figure 1). Each subject repeated the PTF trial ten times, resting for five to six seconds between recordings.
Figure 1.
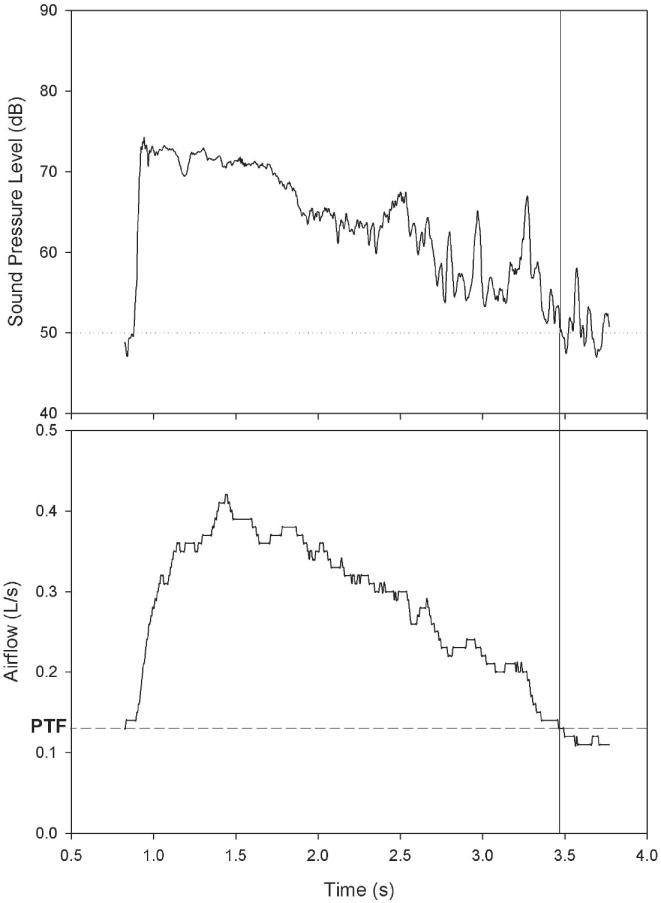
Estimation of phonation threshold flow (PTF). Phonation offset was defined as the point where subject phonation decreased to 50 dB, the level of ambient noise. The glottal airflow at this time was estimated as the PTF.
Data Analysis
Mean and standard deviation values were calculated for both PTF and MFR. The influence of gender on the measurements was assessed using a t-test without assuming equal variance. Nodule, polyp, and normal subject PTF readings were compared with a two-way ANOVA considering both gender and pathology. Bonferroni post-hoc tests were used to investigate differences between individual groups. A significance level of α=0.05 was employed for all measurements. A receiver operating characteristics (ROC) analysis was used to evaluate the diagnostic potential of the two parameters.
RESULTS
A total of 98 samples were collected. Of these 98 samples, 14 were removed due to incomplete collection (2 subjects) or abnormal measurement values that indicated potential deviations from the protocol (12 subjects whose mean MFR<PTF). Forty normal speakers, 21 subjects with vocal nodules, and 23 with vocal polyps comprised the remaining 84 samples. Summary statistics are presented in Table I.
Table I.
Summary statistics for subjects in the normal, polyp, and nodule groups.
| Group | Gender | n | Age | MFR | PTF |
|---|---|---|---|---|---|
| Normal | Female | 21 | 33.8±11.5 | 0.11±0.04 | 0.05±0.02 |
| Male | 19 | 35.5±12.2 | 0.15±0.09 | 0.06±0.04 | |
| Total | 40 | 34.6±11.7 | 0.13±0.07 | 0.06±0.03 | |
| Nodule | Female | 21 | 39.3±8.89 | 0.16±0.07 | 0.08±0.05 |
| Polyps | Female | 12 | 42.3±10.2 | 0.13±0.07 | 0.06±0.03 |
| Male | 11 | 43.2±5.76 | 0.34±0.18 | 0.16±0.09 | |
| Total | 23 | 42.7±8.20 | 0.23±0.17 | 0.11±0.08 | |
| Overall | 84 | 38.0±10.7 | 0.16±0.11 | 0.08±0.06 |
All numbers presented as mean ± standard deviation. n = sample size; MFR = mean flow rate; PTF = phonation threshold flow.
Gender Differences
The mean PTF measurement for men was 0.10±0.08 L/sec, while the mean PTF value for women was 0.07±0.04 L/sec. The difference in PTF between males and females was statistically significant (p=0.047). Mean MFR for males and females were 0.22±0.16 L/sec and 0.13±0.63 L/sec, respectively (p=0.008).
Pathological Differences
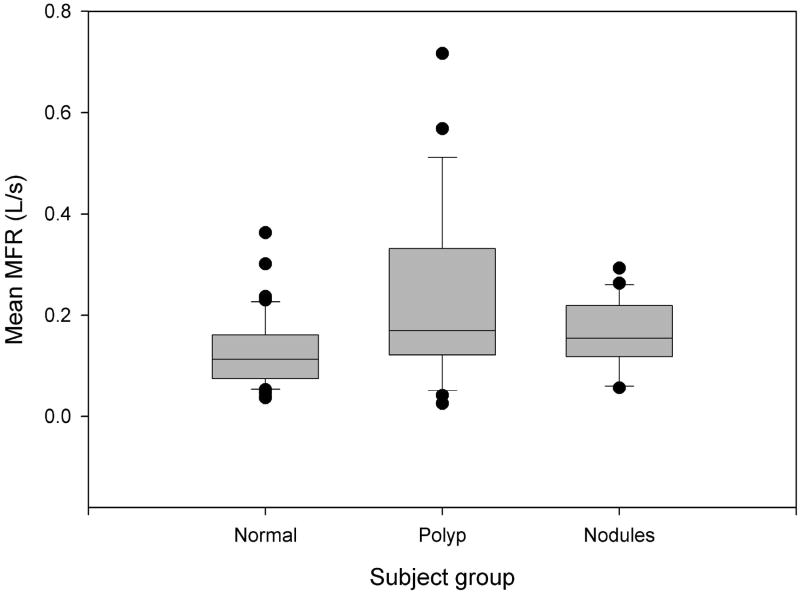
The gender analysis results indicated gender had a considerable effect on both PTF and MFR; therefore, gender was included in the ANOVA. The resulting two-way ANOVA using PTF data showed that, after adjusting for gender differences, the influence of pathology was significant (p<0.001) (Figure 2). Bonferroni post-hoc tests revealed a significant difference between normal subjects and subjects with vocal fold polyps (p<0.001). There was not a significant difference between subjects with vocal fold nodules and those with normal voices (p=0.177) or between those with vocal fold polyps and vocal fold nodules (p=0.246). A two-way ANOVA on MFR data revealed that MFR was significantly influenced by vocal pathology (p<0.001). Post-hoc analysis identified significant differences between normal and vocal fold polyp groups (p<0.001) as well as between vocal fold polyp and vocal fold nodule groups (p=0.039). Normal and vocal fold nodule MFR values were not significantly different (p=0.568) (figure 3).
Figure 2.
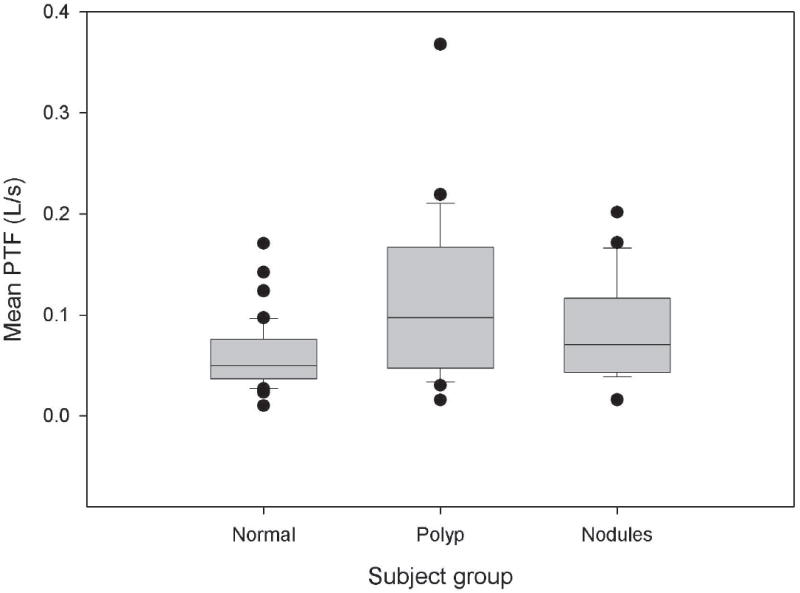
Box plots of phonation threshold flow (PTF) for the normal, polyp, and nodule subject groups. There is a significant difference between normal subjects and subjects with polyps (p < 0.001).
Figure 3.
Box plots of mean flow rate (MFR) for the normal, polyp, and nodule subject groups. There is a significant difference between normal subjects and subjects with polyps (p < 0.001) and between subjects with polyps and subjects with nodules (p = 0.039).
ROC Analysis
Receiver operating characteristics (ROC) analysis was used to evaluate the potential of PTF to distinguish normal from pathological subjects. The area under the curve (AUC) for PTF was 0.691 (p=0.003) which was very similar to the AUC found using MFR (0.684, p=0.004) (Figure 4). MFR obtained a sensitivity of 0.705 and a specificity of 0.600 while PTF identified pathology with a sensitivity of 0.636 and a specificity of 0.650.
Figure 4.
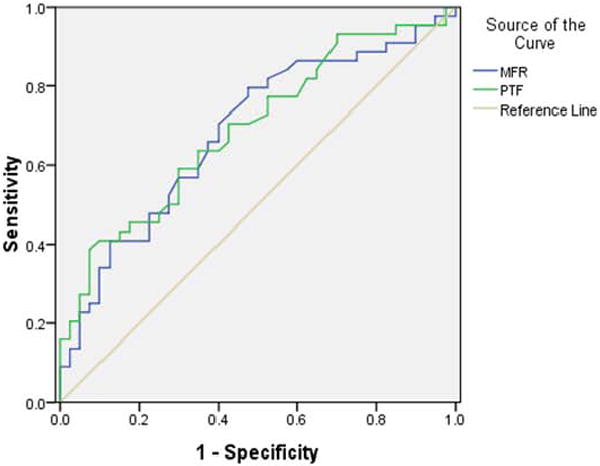
ROC analysis of PTF and MFR. MFR and PTF are similar in performance with AUC values of 0.684 and 0.691, respectively.
DISCUSSION
Data collected from both normal and pathological subjects provide support for the potential of phonation threshold flow (PTF) as a parameter capable of assessing normal and pathological voices. A significant difference was found between the PTF of normal subjects and subjects with vocal polyps. Additionally, males displayed a significantly higher PTF than females. This can be attributed to males having a longer vocal fold length, a parameter with which PTF has a direct relationship.
Of the 98 subjects tested, 14 did not appear to adhere to the study protocol. Attempts to minimize potential confounding effects were made. An airflow tube was used instead of a mask to standardize the vocal tract by holding the tongue in place and to minimize variability associated with mask placement and trial length. Trials were kept below five seconds to avoid vocal fatigue. In 12 subjects, the measured PTF was greater than the MFR. This can most likely be attributed to a post-phonatory expiratory airflow peak. While trial length was not long and subjects rested between trials, it is possible that the experiment disrupted the normal respiratory cycle, thus resulting in an urge to exhale upon completion of the trial. As researchers become increasingly familiar with the PTF measurement procedure, they can be more mindful of post-phonatory expiratory airflow peaks and provide minimal subject training to generate more accurate values.
Two limitations of the study will be the subject of future research seeking to improve current PTF measurement methodology. The experimental system measures airflow at a precision of .01 L/s. While this is sufficient for measuring MFR, greater precision is desired when measuring the low airflow values at the phonation threshold. Secondly, alternative means by which the phonation offset is determined could be explored. This study determined phonation offset as the point at which the sound pressure level of subject phonation decreased to the level of ambient noise in the room. It is possible that subject phonation could continue below 50 dB, but detection would require a sound proof room. Because PTF is presented as a parameter which could be used in the clinic to assess laryngeal health, the procedures outlined represent methods deemed clinically feasible.
Though PTF measurement is in its infancy and can be improved, it shows potential for clinical value. It has been demonstrated to be theoretically15 and now experimentally dependent upon biomechanical properties of the larynx. A significant difference between normal subjects and subjects with polyps was found. The elevated PTF was presumably the result of an increased pre-phonatory glottal width and vocal fold mass due to the polyp. While a significant difference was not found between subjects with polyps and subjects with nodules, there was a discernible difference in the means. Future research with improved collection procedures and increased sample size may demonstrate statistical significance. A significant difference was not observed between normal subjects and subjects with nodules, likely because the presence of nodules did not significantly increase the pre-phonatory glottal width, an observation made during stroboscopic examination. Future studies examining the relationship between polyp size and PTF could be helpful in analyzing disease severity from a functional perspective. Investigating other vocal pathologies such as scarring or paralysis, which would affect vocal fold stiffness, may provide further information on how pathologies affect voice production. Pre- and post-treatment measurements could also be recorded and used to evaluate treatment efficacy.
While measurements of subglottal pressure and MFR during sustained phonation provide insight into the aerodynamics underlying voice production, measuring these parameters at the phonation threshold is more valuable in determining the amount of effort required to produce voice. This is the first study measuring PTF for normal and pathological subjects; however, ROC analysis demonstrated that PTF has a comparable and even slightly better diagnostic potential than MFR, a parameter which has been researched extensively. Difficulties associated with PTP measurement, such as the variability of subject-controlled labial interruption or the reflexive response that can be elicited by mechanical interruption, are not encountered during PTF measurement. Airflow can be easily and noninvasively measured using a tube or circumferentially-vented face mask. PTF is also more sensitive than PTP to parameters such as glottal abduction. As PTF measurement is further developed and refined, it could become a routine test in both the clinical and experimental settings, reflective of laryngeal health and tissue characteristics.
CONCLUSION
Phonation threshold flow (PTF) and mean flow rate (MFR) were measured in normal subjects, subjects with vocal fold polyps, and subjects with vocal fold nodules. Differences in PTF between genders and among normal, polyp, and nodule groups were examined. Significant differences were found between males and females as well as between normal subjects and subjects with polyps. With further research, PTF could become a clinical parameter used to evaluate laryngeal functionality, as it is dependent upon biomechanical properties of the larynx and has been demonstrated to be sensitive to pathology.
Acknowledgments
The authors thank Yi Chai for his valuable contributions to the statistical analysis used in this paper.
This research was supported by an NIH grant number R01 DC008153 from the National Institute on Deafness and Other Communication Disorders.
Funding: This research was supported by an NIH grant number R01 DC008153 from the National Institute on Deafness and Other Communication Disorders.
References
- 1.Rosen CA, Lombard LE, Murry T. Acoustic, aerodynamic and videostroboscopic features of bilateral vocal fold lesions. Ann Otol Rhino Laryngol. 2000;109:823–828. doi: 10.1177/000348940010900907. [DOI] [PubMed] [Google Scholar]
- 2.Altman KW. Vocal fold masses. Otolaryngol Clin North Am. 2007;40:1091–1108. doi: 10.1016/j.otc.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Johns MM. Update on the etiology, diagnosis, and treatment of vocal fold nodules polyps and cysts. Curr Opin Otolaryngol Head Neck Surg. 2003;11:456–461. doi: 10.1097/00020840-200312000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Jiang J, Stern J, Chen HJ, Solomon NP. Vocal efficiency measurements in subjects with vocal cord polyps and nodules: A preliminary report. Ann Otol Rhinol Laryngol. 2004;113:277–282. doi: 10.1177/000348940411300404. [DOI] [PubMed] [Google Scholar]
- 5.Cohen SM, Garrett CG. Utility of voice therapy in the management of vocal fold polyps and cysts. Otolaryngol Head Neck Surg. 2007 May;136(5):742–6. doi: 10.1016/j.otohns.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Holmberg EB, Doyle P, Perkell JS, Hammarberg B, Hillman RE. Aerodynamic and acoustic voice measurements of patients with vocal nodules: Variation in baseline and changes across voice therapy. J Voice. 2003;17:269–82. doi: 10.1067/s0892-1997(03)00076-6. [DOI] [PubMed] [Google Scholar]
- 7.Yiu EM, Yuen YM, Whitehill T, Winkworth A. Reliability and applicability of aerodynamic measures in dysphonia assessment. Clin Linguist Phon. 2004 Sep-Dec;18(6-8):463–78. doi: 10.1080/02699200410001703592. [DOI] [PubMed] [Google Scholar]
- 8.Titze IR. Vocal efficiency. J Voice. 1992;6:135–138. [Google Scholar]
- 9.Titze IR. Phonation threshold pressure: A missing link in glottal aerodynamics. J Acoust Soc Am. 1992;91:2926–35. doi: 10.1121/1.402928. [DOI] [PubMed] [Google Scholar]
- 10.Jiang J, O’Mara T, Conley D, Hanson D. Phonation threshold pressure measurement during phonation by airflow interruption. Laryngosocpe. 1999;109:425–32. doi: 10.1097/00005537-199903000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Baer T. Ph.D. dissertation. MIT; Cambridge, MA: 1975. Investigation of phonation using excised larynges. [Google Scholar]
- 12.Isshiki N. Regulatory mechanism of voice intensity variation. J Speech Hear Res. 1964;7:17–29. doi: 10.1044/jshr.0701.17. [DOI] [PubMed] [Google Scholar]
- 13.Hertegård S, Gauffin J, Lindestad PA. A Comparison of subglottal and intraoral pressure measurements during phonation. J Voice. 1995;9(2):149–155. doi: 10.1016/s0892-1997(05)80248-6. [DOI] [PubMed] [Google Scholar]
- 14.Fisher KV, Swank PR. Estimating phonation threshold pressure. J Speech Lang Hear Res. 1997 Oct;40(5):112–9. doi: 10.1044/jslhr.4005.1122. [DOI] [PubMed] [Google Scholar]
- 15.Jiang J, Tao C. The minimum glottal airflow necessary to initiate vocal fold oscillation. J Acoust Soc Am. 2007 May;121(5 Pt1):2873–81. doi: 10.1121/1.2710961. [DOI] [PubMed] [Google Scholar]
- 16.Hottinger DG, Chao T, Jiang JJ. Comparing phonation threshold flow and pressure by abducting excised larynges. Laryngoscope. 2007;117:1695–1699. doi: 10.1097/MLG.0b013e3180959e38. [DOI] [PubMed] [Google Scholar]
- 17.Tao C, Jiang JJ. The phonation critical condition in rectangular glottis with wide prephonatory gaps. J Acoust Soc Am. 2008;123:1637–1641. doi: 10.1121/1.2832328. [DOI] [PubMed] [Google Scholar]
- 18.Regner MF, Tao C, Jinag J, Zhuang P. Onset and offset phonation threshold flow in excised canine larynges. Laryngoscope. 2008 Apr 7; doi: 10.1097/MLG.0b013e31816e2ec7. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pontes P, Kyrillos L, Behlau M, De Biase N, Pontes A. Vocal nodules and laryngeal morphology. J Voice. 2002;16(3):408–414. doi: 10.1016/s0892-1997(02)00112-1. [DOI] [PubMed] [Google Scholar]