Abstract
The literature supports a variety of predictor variables to account for the psychological and stress burden experienced by cancer family caregivers. Missing among the predictor variables are the differences by or influence of race/ethnicity. The purpose of this study was to describe the sample, explore differences in outcomes by patient and family caregiver characteristics, and determine if any of the patient and family characteristics, including race/ethnicity, predicted outcomes. Cross-sectional surveys were used to determine sociodemographics, psychological and physical health, and burdens of caregiving among 54 caregivers. The analysis consisted of descriptive methods, including frequencies and t tests, and regression modeling. The sample was 35% African American or Hispanic. African American and Hispanic caregivers were younger than white caregivers and more often women, were rarely the spouse of the patient, and frequently had other dependents, including children and older parents. African American and Hispanic caregivers reported lower incomes and more burden related to finances and employment than did white caregivers. When controlling for sociodemographic factors, there was no difference by race/ethnicity on the outcome measures. The experience of caregiving may supersede race/ethnicity and may be its own cultural entity. Areas of concern include the interrelationship between socioeconomic status and race/ethnicity, the absence of cultural frameworks to direct caregiver research, and the question of cultural relevance of measurement tools.
Keywords: African American, Cancer, Ethnic diversity, Family caregiver, Hispanic, Minority, Quality of life
The psychological toll of caring for a family member with cancer has been well documented over the years.1–5 Anxiety and depression are the most often cited cancer family caregiver impairments, with prevalence estimates for depression ranging from 12%2 to 30%6 and estimates for anxiety at 35%.2 In several studies, the cancer family caregiver’s mental health burden exceeded that of the person with cancer.7–10
The literature supports a variety of predictor variables to account for the psychological and stress burden experienced by family caregivers of individuals with cancer. The predictor variables include sleep deprivation11–13; perceived burden of caregiving14,15; caregiver shift in role, responsibility level, and leisure activity16; and lifestyle interference and social isolation.17,18 Notably missing among the predictor variables is the influence of race and ethnicity, most likely secondary to the paucity of data on minority cancer family caregivers.
The noncancer caregiver literature, dominated by studies of family caregivers of those with dementia, has matured such that ethnic and racial differences in caregiver stressors, resources, and outcomes are apparent.19–23 However, interpretation of these racial and ethnic differences and their implications continue to challenge researchers and practitioners. Major areas for cogitation include the spurious nature of racial and ethnic categorization19; the interrelationship between socioeconomic status and race/ethnicity19,21,24; the use of race and ethnicity as proxies for culture, values, and beliefs; the absence of cultural frameworks to direct caregiver research; and the question of cultural relevance and sensitivity of measurement tools.21
Although it is highly probable that the concerns cited in the noncancer caregiver research apply to cancer family caregivers, it is necessary to discern fundamental characteristics of minority cancer family caregivers prior to more sophisticated investigations. It is possible that the physical and time demands and existential concerns imposed by a cancer diagnosis usurp any racial and ethnic differences. The purpose of our study was to describe the sample, explore differences in outcomes by patient and family caregiver characteristics among a racially and ethnically diverse sample, and determine if any of the patient and family caregiver characteristics, including race/ethnicity, predicted outcomes. Specifically, the following research questions were explored:
Are there any predictors or variance by patient and caregiver characteristics, including race/ethnicity, related to outcomes of burden, reactions, and responses to caregiving?
Do caregiver characteristics, burden, reactions and responses to caregiving, predict outcomes by race/ethnicity, independent of demographic and socioeconomic characteristics?
The conceptual framework Labor of Caregiving25 guided the selection of study variables (see “Measurement” section). Labor of Caregiving was developed from in-depth interviews with family caregivers of individuals with advanced cancer or AIDS. Four phases of the caregiving experience over the illness trajectory emerged: “Becoming a Caregiver,” “Taking Care,” “Midwifing the Death,” and “Taking the Next Steps.” Each phase includes distinct themes, specifically, “Becoming a Caregiver” includes facing the present, choosing to care, looking to the future, and developing competency; “Taking Care” includes managing the illness, facing and preparing for dying, managing the environment, coming to know one’s own strength, personal suffering, responding to family issues, and struggling with the healthcare system; “Midwifing the Death” includes waiting and doing and hoping for a good death; and “Taking the Next Step” includes experiencing relief, tying up loose ends, dealing with regrets, and moving ahead. The study presented here focuses on the first 2 phases, “Becoming a Caregiver” and “Taking Care.”
Methods
Research Design
A cross-sectional design was used to achieve the study goals. Self-report surveys were used to determine demographic, psychological, and physical health characteristics and burdens related to the caregiving experience among cancer family caregivers. The Yale School of Nursing Institutional Review Board approved the protocol. Participants provided written informed consent before completing the surveys.
Participant Eligibility
Caregivers of adults with a diagnosis of cancer who were receiving treatment in the form of radiation, chemotherapy, and/or surgery for the cancer were eligible if the caregivers were 18 years or older and able to read and speak English.
Recruitment and Sample
Recruitment occurred via 2 pathways. First, researchers relied on clinicians in a large academic urban cancer treatment center to identify minority (African American or Hispanic) patients who were receiving treatment (chemotherapy, surgery, and/or radiation therapy) of cancer. Over a 9-month period in 2006, the clinicians identified 71 patients. Second, 120 patients in a larger home care intervention study of women with gynecologic cancer were identified between June 2004 and September 2006. A total of 191 patients receiving treatment of cancer were identified from the 2 sources of recruitment. The 191 patients were approached by the researchers and asked to identify a caregiver. Caregiver was defined as someone who is involved with and helps the patient with his or her care and/or household activities; the caregiver was not necessarily a relative nor did he or she need to be living with the patient.
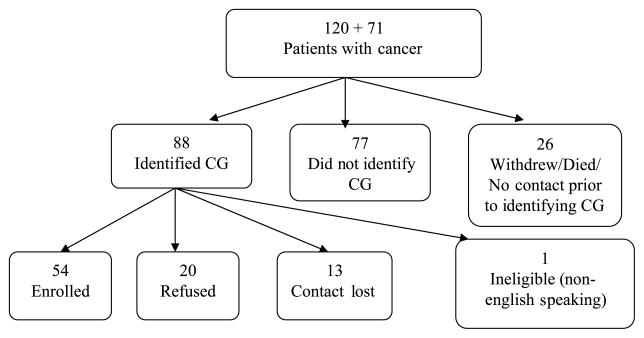
Thirty-two African American and Hispanic caregivers were identified from both sources, and 19 (59%) agreed to participate. Fifty-six white caregivers were identified, and 35 (63%) agreed to participate. The final sample (n = 54) consisted of 19 (35%) African American or Hispanic caregivers and 35 (65%) white caregivers. Details of recruitment are in Figure 1.
Figure 1.
Caregiver (CG) recruitment flow chart.
Measurement
Two self-report demographic questionnaires were developed specifically for the study. One of the questionnaires was used to collect information on a variety of caregiver characteristics, including sex, age, race/ethnicity, relationship to patient, education status, religious affiliation, attendance at religious services, employment status, number of people in household, presence of dependent children in the home, and presence of elderly parents in the home. A second, shorter demographic questionnaire was used to gather patient demographics, diagnosis, and treatment information.
Depressive symptoms were defined as the presence of symptoms indicative of a depressive disorder as measured by the Center for Epidemiological Studies-Depression scale (CES-D). The CES-D was developed at the National Institutes of Health specifically to meet the need for a brief, inexpensive measure of depressive symptoms, suitable for use in community surveys. The CES-D consists of 20 items and 6 major symptom areas. Each item is rated on a scale from 0 to 3 in terms of frequency of occurrence during the past week, and the total score may range from 0 to 60, with a score of 16 or more indicating impairment. The scale has high internal consistency, reliability, test-retest stability, and construct validity in community and clinical samples.26 With family caregiver populations, internal consistency has been consistently around .90.3,27–30 Cronbach α for our sample was .92.
Caregiver overall health status was measured by the Medical Outcomes Study Short-Form (SF-12).31 The SF-12 consists of 12 items derived from the Medical Outcomes Study Short Form 36-item health survey to measure quality of life. The scale has been extensively tested and validated and found to be internally consistent, reliable, and valid. It consists of 2 summary measures: physical and mental health components, which assess one’s physical, emotional, and social health. There are 4 scales consisting of 2 questions each—physical functioning, role physical, role emotional, and mental health—and 4 items each representing 1 subscale—bodily pain, general health, vitality, and social functioning. A high degree of correspondence was achieved in reproducing the physical and mental health component measures of the Short-Form 36-item survey using the SF-12 items; correlations were greater than 0.95.31
The Caregiver Reactions Assessment (CRA) is a 24-item scale that has been used extensively with cancer family populations.32 It consists of 5 subscales, caregiver’s health, self-esteem, schedule, finances, and family support.32 The CRA corresponds to the theoretical constructs of the Labor of Caregiving by measuring the impact of “Taking Care” related to managing the environment, preparing for death, and knowing one’s strengths.25 Responses are measured on a 5-point Likert-type scale (strongly disagree to strongly agree). The individual items are summed and averaged for a total score or a total subscale score. Higher scores indicate higher levels of burden for the caregiver or a negative impact related to caregiving.32 Internal consistency reliability is reported at .70 to .90 for each subscale in samples of caregivers of patients with various types of cancer.3,33–35 Our results had similar internal consistency for each subscale ranging from .70 to .85.
The Caregiver Demands Scale36 (Demands) is a 32-item scale with 7 subscales measuring the demands imposed by managing the illness25 related to meals and feeding, intimate care, walk and transfers, treatments, the healthcare system, supervision, rest, and new skills. The Demands scale directly relates to the Labor of Caregiving constructs “Becoming a Caregiver” (developing competency) and “Taking Care” (illness management). It is scored on a 5-point Likert-type scale, with higher scores indicating greater demand on the caregiver. Total score internal consistency in a study of caregivers of individuals with multiple cancers or AIDS was .78. In our sample, total score internal consistency was similar at .73.
Recently, the concept of mutuality has entered the cancer caregiver literature and holds intuitive promise as an important factor in caregiver research. Mutuality encompasses the caregiver/patient dyad’s shared meaning, attitude, and orientation toward the disease37 and includes themes related to the Labor of Caregiving construct “Becoming a Caregiver.”25 The Mutuality and Interpersonal Sensitivity Scale (MISS) is a 5-point Likert-type scale consisting of 2 subscales—sensitivity and mutuality, with answers ranging from “always true” to “never true.” The scale is scored by summing the items and reporting means. Higher scores are reported by the caregiver when he or she feels that there is agreement between himself or herself and the patient regarding their shared illness experience. With only limited use and psychometrics to date, the MISS has demonstrated reasonable internal consistency (.90–.93) in a sample of caregivers of breast and prostate cancer patients (F. Lewis and L. L. Northouse, written communication, October 28 and 30, 2006). Cronbach α for our sample was only slightly lower at .85 for the sensitivity subscale and .88 for the mutuality subscale.
Data Collection
Data collection took place from June 2004 through October 2006, with one data collection point at the time of enrollment per participant. Caregivers were contacted by telephone to schedule meeting times for data collection, which took place in the caregiver’s home, during one of the patient’s chemotherapy or radiation therapy appointments, or during a clinic visit, as the caregiver preferred. Three caregivers were unable to meet with the researchers for data collection. These 3 caregivers were mailed the instruments with detailed instructions; they completed the instruments and returned them by mail.
Statistical Analysis
Data were analyzed using statistical SAS software for windows version 9.1.38 Descriptive statistics of all demographic and testing measures were conducted. Internal consistency reliability coefficients were calculated for this sample on each measure. A comparison of means (using Student t test for continuous variables and χ2 test and Mann-Whitney U test for categorical variables) was conducted for African American and Hispanic and white participants.
Frequency tables were constructed using the Fisher exact test to ensure test validity even with small cells. The Fisher exact test was used to detect difference in frequencies between the 2 subgroups (African Americans and Hispanics and whites). For continuous variables, the 2-sample Student t test with pooled estimates of variance was used to compare means, except in cases where the F test indicated unequal variance. When unequal variances were indicated, the Satterwaite approximation was used.
Regression models were constructed using stepwise model building. Criterion for entry to the model (and staying in the model) was significance at the .15 level. All available demographic and socioeconomic characteristics of the caregivers and the clinical characteristics of the patients (Table 1) were considered as candidates for entry to the model. The significant findings are reported and discussed in the following sections.
Table 1.
Caregiver Demographic and Socioeconomic Data by Race/Ethnicity
| Characteristic | Total Group (n = 54) | African Americans/Hispanics (n = 19, 35%) | Whites (n = 35, 65%) | P Value |
|---|---|---|---|---|
| Age of CG, y, mean (SD) | 54.67 (14.56) | 40.97 (10.66) | 61.94 (10.52) | <.0001 |
| Age of PT, y, mean (SD) | 56.31 (14.76) | 52.61 (20.06) | 58.01 (11.09) | .30 |
| Length of time as CG, mo, mean (SD) | 9.69 (14.70) | 13.36 (16.97) | 8.04 (13.44) | .25 |
| CG sex | <.0001 | |||
| Female | 20 (37.0) | 16 (84.2) | 4 (11.4) | |
| Male | 34 (63.0) | 3 (15.8) | 31 (88.6) | |
| PT sex | .002 | |||
| Female | 45 (84.9) | 11 (61.1) | 34 (97.1) | |
| Male | 8 (15.1) | 7 (38.9) | 1 (2.9) | |
| Income, $ | .07 | |||
| 0–24,999 | 6 (12.8) | 4 (26.7) | 2 (5.7) | |
| 25,000–49,999 | 11 (23.4) | 5 (33.3) | 6 (17.1) | |
| 50,000–89,999 | 15 (31.9) | 2 (13.3) | 13 (37.1) | |
| >90,000 | 15 (31.9) | 4 (26.7) | 11 (31.4) | |
| Relationship to PT | <.0001 | |||
| Spouse | 29 (53.7) | 1 (5.3) | 28 (80.0) | |
| Not spouse | 25 (46.3) | 18 (94.7) | 7 (20.0) | |
| Diagnosis | <.0001 | |||
| Gynecologic | 40 (73.6) | 6 (31.6) | 34 (97.0) | |
| Not gyn | 14 (26.4) | 13 (68.4) | 1 (3.0) | |
| Cancer treatment | <.0001 | |||
| S, R, C | 10 (18.5) | 3 (15.8) | 7 (20.0) | |
| S and R only | 1 (1.9 | 0 (0.0) | 1 (2.9) | |
| R and C only | 4 (7.4) | 4 (21.1) | 0 (0.0) | |
| S and C only | 23 (42.6) | 2 (10.5) | 21 (60.0) | |
| R only | 3 (5.6) | 3 (15.8) | 0 (0.0) | |
| S only | 6 (11.1) | 1 (5.3) | 5 (14.3) | |
| C only | 6 (11.1) | 5 (26.3) | 1 (2.9) | |
| No. of comorbidities | .77 | |||
| 0 | 18 (33.3) | 6 (31.6) | 12 (34.3) | |
| 1 | 22 (40.7) | 9 (47.4) | 13 (37.1) | |
| 2 | 8 (14.8) | 3 (15.8) | 5 (14.3) | |
| >2 | 6 (11.1) | 1 (5.3) | 5 (14.3) | |
| HH composition | ||||
| Total no. in HH, mean (SD) | 2.83 (1.18) | 3.42 (1.54) | 2.53 (0.79) | .01 |
| No. of CGs living with | ||||
| Spouse | 41 (75.9) | 9 (47.4) | 32 (91.4) | .00 |
| Children <18 y | 14 (25.9) | 9 (47.4) | 5 (14.3) | .02 |
| Children >18 y | 10 (18.5) | 4 (21.1) | 6 (17.1) | 1.00 |
| Parents | 6 (11.1) | 5 (26.3) | 1 (2.9) | .02 |
| Siblings | 2 (3.7) | 2 (10.5) | 0 (0.0) | .12 |
| Other relatives | 7 (13.0) | 4 (21.1) | 3 (8.6) | .23 |
| Nonrelatives | 5 (9.3) | 4 (21.1) | 1 (2.9) | .05 |
| Education | .0045 | |||
| <HS graduate | 16 (29.6) | 7 (36.8) | 9 (25.7) | |
| ≥HS, < college graduate | 21 (38.9) | 11 (57.9) | 10 (28.6) | |
| ≥College graduate | 17 (31.5) | 1 (5.3) | 16 (45.7) | |
| Religious affiliation | 1.00 | |||
| None | 14 (25.9) | 5 (26.3) | 9 (25.7) | |
| Protestant | 14 (25.9) | 5 (26.3) | 9 (25.7) | |
| Catholic | 20 (37.0) | 7 (36.8) | 13 (37.1) | |
| Other | 6 (11.1) | 2 (10.5) | 4 (11.4) | |
| Attendance at place of worship | 1.00 | |||
| Never | 10 (18.9) | 3 (15.8) | 7 (20.0) | |
| Occasional | 20 (37.7) | 7 (36.8) | 13 (37.1) | |
| Regular | 23 (43.4) | 9 (47.4) | 14 (40.0) | |
| Employment status | .11 | |||
| Employed | 37 (68.5) | 16 (84.2) | 21 (60.0) | |
| Not working | 5 (9.3) | 2 (10.5) | 3 (8.6) | |
| Retired | 12 (22.2) | 1 (5.3) | 11 (31.4) | |
Abbreviations: C, chemotherapy; CG, caregiver; Gyn, gynecologic; HH, household; HS, high school; PT, patient; R, radiation therapy; S, surgery.
Values are presented as n (%), unless otherwise indicated.
Results
Sample
Fifty-four family caregivers participated in the study. The ethnically/racially diverse sample was 63% (n = 34) male and 35% (n = 19) African American or Hispanic (African American, n = 11; Hispanic, n = 8). See Table 1 for a complete description of the demographic and socioeconomic characteristics of the caregivers and the clinical characteristics of the patients for whom they were caring. There was a significant difference in caregiver sex by race/ethnicity, with women largely represented among the African American and Hispanic caregivers (84.2%) and men largely represented among the white caregivers (88.6%). The mean (SD) age of the total sample was 54.7 (15.5) years, with a significant difference (P < .0001) between whites (61.9 ± 10.5 years) and African Americans and Hispanics (41.0 ± 10.7 years). Although 70.4% of the total caregiver sample had at least a high school education, significantly more white caregivers than African American and Hispanic caregivers had attained a college degree or higher (n = 16, 45.7%, vs n = 1, 5.3%, respectively). Among all caregivers, 68.5% (n = 37) were employed, 63.8% (n = 30) reported a household income of $50,000 or more, 74.1% (n = 40) identified a religious affiliation, and 81.1% (n = 43) attended a place of worship occasionally or regularly.
There were no statistically significant differences by race for employment status, income level, religious affiliation, or attendance at a place of worship. There was a significant difference (P ≤ .00001) by race for the caregiver’s relationship to the patient. Most African American and Hispanic caregivers (n = 18, 94.7%) were not spouses of the patients, and conversely, most white caregivers (n = 28, 80.0%) were spouses of the patients.
Household composition was significantly different between the 2 groups in several ways (Table 1). African American and Hispanic caregivers reported a significantly larger number of household members than did their white counterparts (3.4 vs 2.5 members, respectively; P = .01). African American and Hispanic caregivers were also significantly more likely than white caregivers to have younger children (P = .02), parents (P = .02), and nonrelatives (P = .05) living in the same household.
Patients of the caregivers had a variety of cancer diagnoses, with a majority (n = 40, 73.6%) having gynecological cancer. There was a significant difference by race for types of diagnoses (P ≤ .00001). Ninety-seven percent (n = 34) of all white patients had gynecological cancer, whereas only 31.6% (n = 6) of African American and Hispanic patients had gynecological cancer. The remaining 14 patients had the following cancer diagnoses: breast, colorectal, lung, gastrointestinal, leukemia, or lymphoma (Table 1).
Treatment was described as surgery, radiation therapy, and/or chemotherapy. Twenty-three (42.6%) patients received a combination of surgery and chemotherapy, and 10 (18.5%) patients received all 3 modalities of treatment (Table 1). Six (11.1%) patients received either surgery or chemotherapy alone, and 3 (5.6%) received only radiation therapy. There was a significant difference (P ≤ .00001) by race for types of treatment. Most (n = 21, 60.0%) white patients received a combination of surgery and chemotherapy versus only 2 (10.5%) African American or Hispanic patients. The single most common form of treatment for the African American or Hispanic patients was chemotherapy alone (n = 5, 26.3%).
Psychological and Physical Health Measures
There were no significant differences in total scores among white and African American and Hispanic caregivers on psychological and physical health as measured by the SF-12 and CES-D scales. The total sample of caregivers, on average, fell below the CES-D cutoff score of 16, thus failing to meet criteria for expression of depressive symptoms (Table 2).
Table 2.
Psychological and Physical Health, and the Experience of Caregiving
| Scale | Total Group (n = 54) | African Americans and Hispanics (n = 19, 35%) | Whites (n = 35, 65%) | P value |
|---|---|---|---|---|
| CES-Da | 14.43 (10.19) | 13.00 (0.95) | 14.77 (9.52) | .55 |
| Hopeful | 2.15 (0.94) | 1.68 (0.82) | 2.38 (0.87) | .01 |
| Happy | 2.33 (0.94) | 1.95 (0.91) | 2.50 (0.88) | .04 |
| Sad | 3.08 (0.88) | 3.42 (0.84) | 2.91 (0.86) | .04 |
| SF-12 Physicalb | 54.55 (8.25) | 52.84 (8.64) | 55.53 (8.08) | .28 |
| SF-12 Mentalb | 44.27 (1.90) | 45.67 (14.27) | 43.81 (10.30) | .60 |
| Downhearted and blue | 4.28 (1.23) | 4.79 (1.27) | 4.06 (1.09) | .03 |
| Caregiver reactionsa | 2.54 (0.46) | 2.64 (0.55) | 2.45 (0.37) | .17 |
| Lack of family support | 1.79 (0.77) | 2.06 (0.95) | 1.61 (0.60) | .04 |
| Impact on finances | 2.22 (0.93) | 2.56 (0.90) | 2.02 (0.91) | .04 |
| Caregiver demandsa | 1.59 (0.78) | 1.47 (0.83) | 1.61 (0.74) | .62 |
| Work | 1.89 (1.64) | 3.33 (1.63) | 1.17 (1.11) | .004 |
| Mutualityb | 4.05 (0.62) | 4.34 (0.48) | 4.03 (0.53) | .12 |
| Try to see lighter side | 3.92 (1.06) | 4.58 (0.61) | 3.59 (1.07) | .0006 |
| Interpersonal sensitivityb | 3.35 (0.74) | 3.52 (0.75) | 3.31 (0.65) | .18 |
Abbreviation: CES-D, Center for Epidemiological Studies-Depression scale.
Values are presented as mean (SD).
Higher scores reflect more distress.
Higher scores reflect better performance.
Although there was little variability by race on the total scores, several items were sensitive to differences between the 2 groups. For example, on the CES-D, whites were more likely to agree with the statement “I feel hopeful about the future” (P = .01) and “I am happy” (P = .04), whereas, inversely, African American and Hispanic caregivers were more likely to agree with the statement “I am sad” (P = .04). On the SF-12, African American and Hispanic caregivers were more likely to report feeling “downhearted and blue” (P = .03).
Experience of Caregiving
No significant differences were found in the scores between white and African American and Hispanic caregivers on measures of the caregiving experience (CRA, Demands, and MISS) (Table 2).
Subscale scores on the CRA indicated that African American and Hispanic caregivers reported an increased burden related to a lack of family support (P = .04) in 2 areas—feeling abandoned and feeling that caregiving was dumped on them. African American and Hispanic caregivers also reported more burden related to the impact that caregiving had on their finances (P = .04); it was more difficult for them to pay for the patients’ health needs.
The scores on 1 subscale of the Demands scale indicated that African American and Hispanic caregivers reported significantly more difficulty with taking time off from work (P = .004), although there was no significant difference in how many white versus African American and Hispanic caregivers reported taking time off from work (35% vs 33% of each group, respectively).
Research Questions
Significant findings are reported here for both research questions. Caregiver characteristics, burden, and responses to the experience of caregiving varied only by 1 caregiver characteristic, length of time (LoT) as a caregiver. The LoT that one was a caregiver ranged from approximately 2 to 3 weeks to almost 5 years (0.33 to 56 months), with a mean (SD) LoT as a caregiver of 9.7 (15) months (Table 1). In the regression stepwise modeling as described above, the effect of LoT as a caregiver was significant only with the SF-12 scores. Significantly lower scores (P = .048, n = 42) indicating worse functionality were reported by those with longer times of caregiving (r2 = 0.09). Because of the low number of participants (n = 42) in the model when including LoT as a variable, the model was also analyzed without LoT. When not considering LoT as a caregiver, the relationship of the caregiver to the patient had a significant effect on burden. Spouses of patients, regardless of sex, reported significantly less burden related to family support (P = .028, r2 = 0.10, n = 51), and their sensitivity (MISS) scores were significantly lower (P = .05, r2 = 0.08, n = 49) when not accounting for LoT as a caregiver.
Caregiver characteristics, burden, and responses to the experience of caregiving did not vary by race/ethnicity when controlling for demographic and socioeconomic characteristics except that white caregivers reported less burden related to family support when not considering income (P = .035, r2 = 0.09, n = 51), and when considering or correcting for income in the stepwise modeling, it was the only variable that was significant for effect with the burden related to family support. Caregivers with higher income reported significantly less burden related to the experience of caregiving (P = .021, r2 = 0.12, n = 45). Correcting for income, female caregivers reported lower SF-12 scores or worse functioning (P = .004, r2 = 0.09, n = 44), and those who were working full-or part-time had higher SF-12 scores (P = .025, r2 = 0.10, n = 44). When controlling for sex and work status, there was a significant effect of income on functioning; higher income was associated with better functioning (P = .040, r2 = 0.10). Without considering income, there was still no effect of race/ethnicity on any outcome variable; however, better functioning was reported by caregivers who were working (P = .006, n = 49) and older caregivers (P = .015, n = 49).
Discussion
The small sample size in this study and the cross-sectional design warrant cautious viewing of the results. However, it is important to recognize that there were no differences reported overall in outcomes by race/ethnicity. The differences reported in a small number of items and subscales lend themselves to further investigation, specifically in a longitudinal study of a larger sample that could better isolate the influence of factors related to demographic, socioeconomic, and race/ethnicity effects. Despite these limitations, we found that African American and Hispanic caregivers were clearly younger and more often women. They were also rarely the spouse of the patient and, interestingly, were frequently responsible for other members of their households, such as children and older parents. This is consistent with the non-cancer caregiver literature.22,23 African American and Hispanic caregivers reported lower household incomes than did the white caregivers, and they reported more burden and demands related to finances, work, and lack of family support, which may contribute to the difficulties with “Taking Care.”25 This is also consistent with the noncancer caregiver literature and speaks to the overriding influence of socioeconomic status on performance.19,21,24 Despite differences in responsibilities or stresses related to household responsibilities and composition and financial constraints, African American and Hispanic caregivers did not report more depressive symptoms. Patient diagnosis may have influenced responses on the depression and health measures. Patients of African American and Hispanic caregivers were diagnosed less frequently with ovarian cancer, which has a particularly poor prognosis, than do patients of white caregivers. The difference in diagnosis may have muted a difference in the measures of mental health because of caregiving burden. The difference in household composition by group with a larger number of people in the household and the presence more frequently of younger children and older parents in households of African American and Hispanic caregivers may explain their reports of higher burden related to “Taking Care”25 in the areas related to lack of family support and financial- or work-related issues. It seems reasonable that income- and work-related burden would be related. The lower incomes reported by African American and Hispanic caregivers as compared with white caregivers would also limit their ability to pay for services and support that may have assisted with dependent child or elderly parent care, healthcare for the patient, and transportation-type expenses. Taking time off from work was also more difficult for African American and Hispanic caregivers. The lower incomes reported by African American and Hispanic caregivers may be proxy markers for hourly wage, temporary, or full-time jobs without benefits such as paid time off for family- or health-related issues, thus contributing to their difficulty in taking time off from work.
When controlling for demographic and socioeconomic characteristics, there was no difference by race/ethnicity between the 2 groups overall. Therefore, the experience of caregiving may be independent of race or ethnicity and be its own cultural experience. Demographic and socioeconomic factors may have more influence on the experience than race or ethnicity alone. Despite lower income and what would seem to be more responsibility related to household composition and, thus, burden, the African American and Hispanic caregivers did not report worse depressive symptoms or mental or physical health, and they also did not report more demands or burden related to caregiving overall. Thus, the areas where higher burden and demand were reported (family support, financial, and work-related areas) seem to be related specifically to socioeconomic factors.
Implications
A future study with a limit on the number of diagnoses and types of treatment would have the advantage of being homogenous with respect to clinical characteristics, thereby allowing one to better isolate the influence of race/ethnicity on the experience of caregiving. However, this would limit the generalizability but may help to isolate the influences on caregiving. Age, sex, and race/ethnicity are immutable characteristics; however, the mutable factors that may contribute to caregiver burden and have a negative impact on the caregiving experience seem to be related to demographic and socioeconomic factors and can be supported with various interventions. Interventions that can support those with limited family, financial, and work resources, that is, social support, transportation services, legislation and policies for job support with paid leave, and community support, including child and elder care services, combined with clinical interventions such as more targeted information, need to be explored. It seems that the burdens of caregiving and the relationship with socioeconomic and cultural factors are worldwide issues for patients and caregivers; therefore, when first encountering and assessing patients, nurses need to be sensitive to the needs of the caregivers.24,39 Although differences in burden or the experiences of caregiving may be more closely related to socioeconomic factors rather than to cultural or ethnic factors, clinicians should be aware that individuals may make decisions regarding support and services based on socioeconomic and cultural or ethnic factors.24 Clinicians should identify those at risk early in the caregiving and patient care trajectory and assess for factors related to family, finances, and work that may put the caregiver at increased risk and intervene and make referrals early for support services.
The interpretation of racial and ethnic differences challenges researchers and practitioners. Areas of concern and the need for further understanding include the interrelationship among socioeconomic status and race/ethnicity,19,21,24 the absence of cultural frameworks to direct caregiver research, and the question of cultural relevance and sensitivity of measurement tools.21
Acknowledgments
NIH-1P20NR08349. Principal Investigator M. Funk, PhD at Yale University School of Nursing.
References
- 1.Grov E, Dahl A, Moum T, Fossa S. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase [published online ahead of print April 22, 2005] Ann Oncol. 2005;16(7):1185–1191. doi: 10.1093/annonc/mdi210. [DOI] [PubMed] [Google Scholar]
- 2.Grunfeld E, Coyle D, Whelan T, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. Can Med Assoc J. 2004;170:1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kurtz M, Kurtz J, Given C, Given B. Depression and physical health among family caregivers of geriatric patients with cancer—a longitudinal view. Med Sci Monit. 2004;10:CR447–CR456. [PubMed] [Google Scholar]
- 4.Laizner A, Yost L, Barg F, McCorkle R. Needs of family caregivers of persons with cancer: a review. Semin Oncol Nurs. 1993;9:114–120. doi: 10.1016/s0749-2081(05)80107-x. [DOI] [PubMed] [Google Scholar]
- 5.Taylor EJ. Spiritual needs of patients with cancer and family caregivers. Cancer Nurs. 2003;26:260–266. doi: 10.1097/00002820-200308000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Blanchard C, Albrecht T, Buckdeschel J. The crisis of cancer: psychological impact on family caregivers. Oncology. 1997;11:189–194. [PubMed] [Google Scholar]
- 7.McCorkle R, Siefert ML, Dowd MF, Robinson JP, Pickett M. Effects of advanced practice nursing on patient and spouse depressive symptoms, sexual function, and marital interaction after radical prostatectomy. Urol Nurs. 2007;27:65–77. [PubMed] [Google Scholar]
- 8.Harding R, Higginson IJ, Donaldson N. The relationship between patient characteristics and carer psychological status in home palliative cancer care. Support Care Cancer. 2003;11:638–643. doi: 10.1007/s00520-003-0500-6. [DOI] [PubMed] [Google Scholar]
- 9.Northouse LL, Mood D, Kershaw T, et al. Quality of life of women with recurrent breast cancer and their family members. J Clin Oncol. 2002;20:4050–4064. doi: 10.1200/JCO.2002.02.054. [DOI] [PubMed] [Google Scholar]
- 10.Matthews BA. Role and gender differences in cancer-related distress: a comparison of survivor and caregiver self-reports. Oncol Nurs Forum. 2003;30:493–499. doi: 10.1188/03.ONF.493-499. [DOI] [PubMed] [Google Scholar]
- 11.Carter PA, Acton GJ. Personality and coping: predictors of depression and sleep problems among caregivers of individuals who have cancer [see comment] J Gerontol Nurs. 2006;32:45–53. doi: 10.3928/0098-9134-20060201-11. [DOI] [PubMed] [Google Scholar]
- 12.Carter PA. Family caregivers’ sleep loss and depression over time. Cancer Nurs. 2003;26:253–259. doi: 10.1097/00002820-200308000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Carter P, Chang B. Sleep and depression in cancer caregivers. Cancer Nurs. 2000;23:410–415. doi: 10.1097/00002820-200012000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Lee S, Colditz G, Berkman L, Kawachi I. Caregiving and risk of coronary heart disease in US women: a prospective study. Am J Prev Med. 2003;24:113–119. doi: 10.1016/s0749-3797(02)00582-2. [DOI] [PubMed] [Google Scholar]
- 15.Schulz R, Beach S. Caregiving as risk factor for mortality. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 16.Williamson G, Shaffer D, Schulz R. Activity restriction and prior relationship history as contributors to mental health outcomes among middle-aged and older spousal caregivers. Health Psychol. 1998;17:152–162. doi: 10.1037//0278-6133.17.2.152. [DOI] [PubMed] [Google Scholar]
- 17.Goldstein M, Concato J, Fried T, et al. Factors associated with caregiver burden among caregivers of terminally ill patients with cancer. J Palliat Care. 2004;20:38–43. [PubMed] [Google Scholar]
- 18.Cameron J, Franche R, Cheung A, Stewart D. Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer. 2002;94:521–527. doi: 10.1002/cncr.10212. [DOI] [PubMed] [Google Scholar]
- 19.Pinquart M, Sorensen S. Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: a meta-analysis. Gerontologist. 2005;45:90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]
- 20.Dilworth-Anderson P, Gibson BE. The cultural influence of values, norms, meanings, and perceptions in understanding dementia in ethnic minorities. Alzheimer Dis Assoc Disord. 2002;16:S56–S63. doi: 10.1097/00002093-200200002-00005. [DOI] [PubMed] [Google Scholar]
- 21.Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: a 20-year review (1980–2000) Gerontologist. 2002;42:237–272. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- 22.Aranda MP. Racial and ethnic factors in dementia care-giving research in the US [comment] Aging Mental Health. 2001;5:S116–S123. doi: 10.1080/13607860120044891. [DOI] [PubMed] [Google Scholar]
- 23.Aranda MP, Knight BG. The influence of ethnicity and culture on the caregiver stress and coping process: a sociocultural review and analysis. Gerontologist. 1997;37:342–354. doi: 10.1093/geront/37.3.342. [DOI] [PubMed] [Google Scholar]
- 24.Guberman N, Maheu P. Beyond cultural sensitivity: universal issues in caregiving. Generations. 2004;27:39–43. [Google Scholar]
- 25.Brown Stetz K. The labor of caregiving: a theoretical model of caregiving during potentially fatal illness. Qual Health Res. 1999;9:182–197. doi: 10.1177/104973299129121776. [DOI] [PubMed] [Google Scholar]
- 26.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 27.Kurtz ME, Kurtz JC, Given CW, Given B. A randomized, controlled trial of a patient/caregiver symptom control intervention: effects on depressive symptomatology of caregivers of cancer patients. J Pain Symptom Manage. 2005;30:112–122. doi: 10.1016/j.jpainsymman.2005.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stetz KM, Brown M. Physical and psychosocial health in family caregiving: a comparison of AIDS and cancer caregivers. Public Health Nurs. 2004;21:533–540. doi: 10.1111/j.0737-1209.2004.21605.x. [DOI] [PubMed] [Google Scholar]
- 29.Kozachik SL, Given CW, Given BA, et al. Improving depressive symptoms among caregivers of patients with cancer: results of a randomized clinical trial. Oncol Nurs Forum. 2001;28:1149–1157. [PubMed] [Google Scholar]
- 30.Nijboer C, Triemstra M, Tempelaar R, Mulder M, Sanderman R, van den Bos GA. Patterns of caregiver experiences among partners of cancer patients. Gerontologist. 2000;40:738–746. doi: 10.1093/geront/40.6.738. [DOI] [PubMed] [Google Scholar]
- 31.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The Caregiver Reaction Assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health. 1992;15:271–283. doi: 10.1002/nur.4770150406. [DOI] [PubMed] [Google Scholar]
- 33.Sherwood PR, Given BA, Given CW, et al. Predictors of distress in caregivers of persons with a primary malignant brain tumor. Res Nurs Health. 2006;29:105–120. doi: 10.1002/nur.20116. [DOI] [PubMed] [Google Scholar]
- 34.Given B, Wyatt G, Given C, et al. Burden and depression among caregivers of patients with cancer at the end of life. Oncol Nurs Forum. 2004;31:1105–1117. doi: 10.1188/04.ONF.1105-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Given BA, Given CW, Helms E, Stommel M, DeVoss DN. Determinants of family care giver reaction. New and recurrent cancer. Cancer Pract. 1997;5:17–24. [PubMed] [Google Scholar]
- 36.Stetz KM. The relationship among background characteristics, purpose in life, and caregiving demands on perceived health of spouse caregivers. Sch Inq Nurs Pract. 1989;3(2):133–153. [PubMed] [Google Scholar]
- 37.Lewis F, Fletcher K. Mutuality and sensitivity about breast cancer: the development of a valid and reliable self-report measure for couples. In development. [Google Scholar]
- 38.SAS software for windows version 9.1. Cary, NC: SAS Institute Inc; 2003. [Google Scholar]
- 39.Aoun S, Kristjanson L, Oldham L. The challenges and unmet needs of people with neurodegenerative conditions and their carers. ACCNS J Community Nurses. 2006;11:17–20. [Google Scholar]