Abstract
Background
Lower extremity peripheral arterial disease (PAD) is a coronary heart disease (CHD) risk equivalent. Selected studies have demonstrated less intense risk factor management and diminished mobility in individuals with PAD as compared to individuals with clinical recognized CHD. However, comparable data have not been reported from a nationally representative population.
Objectives
To assess the prevalence, treatment, and control of cardiovascular risk factors among individuals with PAD as defined by an ankle-brachial index (ABI) <0.90 (but without recognized CHD) as compared with individuals with recognized CHD (but without PAD). A second objective was to evaluate the diagnostic accuracy of measures of walking dysfunction to identify individuals with PAD.
Design, Setting, and Participants
We analyzed data from 7,571 participants aged 40 or older who participated in the National Health and Nutrition Examination Survey (NHANES) 1999-2004, a nationally representative cross-sectional survey of the U.S. population.
Results
The prevalence of PAD without CHD was 4.1% (95%CI 3.6, 4.5) compared to 7.9% (7.1, 8.9) for CHD (without PAD). Hypertension prevalence was similar, but treatment and control rates were lower among individuals with PAD compared to CHD (treatment: 69% vs 84%, p<0.001; control: 50% vs 63%, p=0.01). Treatment of hypercholesterolemia was lower among individuals with PAD (54% vs 79%, p<0.001) but control was similar (83% vs 85%, p=0.78). Diabetes awareness, treatment, and control did not differ between the two groups. Walking mobility limitations were specific, but insensitive, for the identification of individuals with PAD.
Conclusion
PAD in the absence of clinically recognized CHD is under-treated and poorly controlled in the general U.S. population. Leg symptoms are not adequate to identify individuals with PAD, who are at high risk of ischemic events.
Atherosclerosis is the most common cause of lower extremity peripheral arterial disease (PAD) and previous studies have documented the high risk of coronary heart disease (CHD) and cerebrovascular events among individuals with PAD (1-6). The ankle-brachial index (ABI) is a simple, noninvasive procedure used to provide an accurate diagnosis of lower extremity PAD in epidemiologic surveys (7). Inasmuch as coronary heart disease event rates for individuals with PAD are similar to those for individuals with established heart disease (3;8), PAD is considered a CHD “risk equivalent” by both the National Cholesterol Education Program-Adult Treatment Panel III and Joint National Commission for the Treatment of Hypertension. The ABI is also used in clinical practice to identify populations with, or at high risk for, cardiovascular disease. Thus, use of the ABI should permit appropriate intensification of risk reduction interventions (7). Although current clinical practice standards define PAD as worthy of treatment as a CHD risk equivalent, data from case series and non-population based surveys suggest that individuals with PAD are under-treated (9-11). In addition to use of the ABI measurement, clinicians have traditionally utilized the presence of limb ischemic symptoms to identify individuals at risk for PAD. Recent investigations have also documented a high prevalence of mobility limitations among persons with lower extremity diseases, including PAD (12-14). However, these studies have not assessed the diagnostic utility of physical function questions to identify persons with PAD nor examined predictors of walking dysfunction, including a low ABI, in a nationally representative cohort.
The objectives of this study were 1) to assess the prevalence, treatment, and control of cardiovascular risk factors among individuals with PAD, as compared to CHD; and 2) to evaluate the diagnostic ability of measures of walking mobility to identify individuals with a low ABI in a nationally representative sample of U.S. adults. We hypothesized (a) that individuals with PAD would have a similar (or more adverse) cardiovascular risk factor profile and receive less aggressive treatment compared to individuals with a history of CHD and that (b) general measures of walking mobility would have high specificity but low sensitivity for the identification of individuals with PAD, as defined by a low ABI. In this population-based study, we directly compare risk factor treatment and control in individuals with PAD (but without CHD) to those with a history of CHD (but without PAD).
DESIGN AND METHODS
Study Population
This study was based on data from the 1999-2004 National Health and Nutrition Examination Survey (NHANES), a cross-sectional survey of the civilian, non-institutionalized population of the United States. Detailed in-person interviews, physical examinations, and blood samples were obtained from over 15,332 participants of all ages and valid ABI information was available for 7,571 individuals aged 40 and older (74% of eligible persons). For the main analyses, we excluded 53 participants who were missing information on CHD status and 20 participants with ABI values > 1.5, values usually related to non-compressible pedal arteries (1;15). Our study sample consisted of 7,498 persons aged 40 and older.
Assessment of Lower Extremity Peripheral Arterial Disease
PAD can be determined with high sensitivity and specificity using the ratio of the systolic blood pressure in the ankle to that in the arm (ABI) (16-18). We defined PAD on the basis of ABI measurements obtained from NHANES 1999-2004 in participants aged 40 and over during the examination component of the survey. In NHANES, the established ABI technique employs measurement of systolic blood pressure at the right brachial artery and at both posterior tibial arteries using Doppler ultrasound. If the participant had a medical condition that did not permit use of the right arm measurement, the left arm was used for brachial pressure measurement. Systolic blood pressure was measured twice at each limb site for participants aged 40-59 and once at each site for participants aged 60 and over. The left and right ABI measurements were obtained by dividing the mean systolic blood pressure in the right and left ankle by the mean blood pressure in the arm. Peripheral arterial disease was defined in a subject when the ABI was less than 0.90 in either leg.
Assessment of Walking Mobility Limitation
Current national consensus-derived care standards define lower extremity symptoms as “any exertional limitation of the lower extremity muscles or any history of walking impairment” (7). Intermittent claudication (lower extremity muscle discomfort that occurs reproducibly with exertion and that is consistently relieved by rest) is often the first clinical manifestation of PAD. Standardized assessment of this primary leg ischemic symptom in population-based studies is typically conducted using a traditional or updated version of the Rose Questionnaire (19;20). These Rose-derived questionnaires were not administered in NHANES. However, as is often done in clinical practice, NHANES participants were asked a set of questions to elicit information regarding physical functioning by asking about their difficulties “doing certain activities because of a health problem.” “Health problem” was defined as “any long-term physical, mental, or emotional problem or illness.” As part of the physical functioning assessment, walking mobility limitation was determined by self-reported level of difficulty (“no difficulty,” “some difficulty,” “much difficulty,” or “unable to do”) when “walking for a quarter mile [that is about 2 or 3 blocks],” “walking up 10 steps without resting,” and “walking from one room to another on the same level.” In individuals aged <60, the mobility limitation questions were only asked to participants who reported a physical, mental or emotional problem. To avoid selection issues, we limited our analysis to the sample of persons 60+ who were eligible for the complete physical functioning assessment, did not report needing special equipment for walking, and who were not missing information on PAD or CHD status. This yielded a large walking impairment cohort with a sample size of N=3,533 after exclusions (<10% with missing data).
Other Study Variables
The NHANES examination included measurement of height, weight, blood pressure, and collection of blood samples by trained personnel. Hypertension was defined as a mean systolic blood pressure of 140 mm Hg or greater, a mean diastolic blood pressure of 90 mm Hg or greater, or hypertension medication use. Mean blood pressure was comprised of up to 4 readings on two separate occasions. Total cholesterol was measured enzymatically (20). Hypercholesterolemia was defined as a total cholesterol level 240 mg/dL or higher, or medication use. Individuals were considered “aware” of their hypertension or hypercholesterolemia if they reported having been told by doctor or other health care professional that they had high blood pressure or high cholesterol. Hypertension was considered controlled in individuals receiving treatment if the mean blood pressure was < 140/90 mm Hg. Hypercholesterolemia was considered controlled in individuals receiving treatment if total cholesterol was <240 mg/dL. Diabetes was defined by a self-reported physician diagnosis. Persons reporting “borderline diabetes” or solely reporting a diabetes diagnosis during pregnancy were considered non-diabetic. Hemoglobin A1c (HbA1c) levels were used to evaluate glucose control among individuals with diagnosed diabetes. Daily aspirin use (“currently taking aspirin every day”) was assessed as part of the prescription medication questionnaire and at the time of submission was only available for the NHANES 1999-2002 survey period. Aspirin included buffered aspirin products such as Anacin, Bayer, Bufferin, Midol, Ascripton, Ecotrin, Pabrin, and Alka Seltzer.
Information on age, sex, race/ethnicity, and smoking was based on self-report during the questionnaire portion of the survey. Smoking status was determined using answers to the questions, “Have you smoked at least 100 cigarettes in your life?” and “Do you now smoke cigarettes?” For the purposes of this study, prevalent coronary heart disease was defined as self-reported coronary heart disease, angina, or previous heart attack. Stroke history was also defined on the basis of self-report.
We calculated the Framingham Risk Score based on age, total cholesterol, smoking status, total cholesterol, and average systolic blood pressure in men and women in this study. Nonetheless, because this is a study population that includes individuals with pre-existing disease, the predictive capacity of the Framingham Risk Score is uncertain. However, it remains a useful summary measure to compare cardiovascular risk factors across groups.
Detailed information regarding data collection in NHANES 1999-2004 is available elsewhere (21).
Statistical Analyses
The NHANES surveys are ongoing complex, multi-stage probability samples of the civilian, non-institutionalized population of the United States. The NHANES 1999-2004 survey over-sampled the elderly, low-income persons, adolescents, Mexican-Americans, and Non-Hispanic blacks to provide more reliable estimates for these population subgroups. Analyses were performed using Stata Version 9.2 (StataCorp College Station, Texas) svy commands to obtain unbiased estimates from the NHANES sampling design. Standard errors for all estimates were obtained using the Taylor series (linearization) method (22). To assess the diagnostic utility of the walking mobility limitation questions to identify individuals with an ABI <0.9, we calculated the sensitivity, specificity, positive and negative predictive values of these “tests.” Multivariable logistic regression models were used to investigate the association between PAD and walking dysfunction before and after adjustment for potential confounding factors. In these analyses, Model 1 was adjusted for demographic factors (age, sex, and race/ethnicity). Model 2 was adjusted for all variables in Model 1 plus history of coronary heart disease (yes/no), diabetes status (yes/no), smoking history (current/former/never), hypertension (yes/no), and hypercholesterolemia (yes/no). Model 3 was adjusted for all variables in Model 2 but also included self-rated general health status (fair/poor vs. excellent/very good/good).
RESULTS
The mean age in the study population was 68 years, 58% of the population was female, 79% of the population was Non-Hispanic White, 14% Non-Hispanic Black, and 3% Mexican American. All estimates reported here are designed to be nationally representative of the non-institutionalized population aged 40 and older in the U.S. in 1999-2004. The prevalence estimates of PAD (ABI<0.9), CHD, PAD in the absence of CHD, and CHD in the absence of PAD by selected characteristics are presented in Table 1. The overall prevalence of PAD defined solely on the basis of an ABI <0.9 in U.S. adults aged 40 or older in the 1999-2004 period was 5.8% (95%CI 5.2, 6.5). The prevalence estimates of PAD in the 1999-2000, 2001-2002, and 2003-2004 surveys were 5.0%, 6.0%, and 6.3%, respectively (p-trend = 0.14). The prevalence of CHD was 9.8% (95%CI 8.8, 10.8) in 1999-2004 and was 10.1%, 9.0%, and 10.3% for each two-year period. The prevalence of PAD in the absence of a history of CHD was 4.4% (95%CI 3.9, 4.8) in the 1999-2004 survey period. Individuals with PAD were older and were more likely to be Non-Hispanic Black compared to individuals with a history of CHD. In contrast to the well-established higher prevalence of coronary heart disease in men, women were more likely to have PAD, particularly PAD in the absence of CHD (p-value <0.001).
Table 1.
Selected characteristics*of the study population by prevalence of peripheral arterial disease (PAD) and coronary heart disease (CHD), adults 40+, NHANES 1999-2004, N=7,498
| Total PAD (ABI<0.9) N= 636 |
Total History of CHD N = 878 |
PAD (ABI <0.90) without a history of CHD N = 482 |
CHD without PAD (ABI <0.90) N = 724 |
|
|---|---|---|---|---|
| Total (Overall Prevalence), % (SE) | 5.8 (0.3) | 9.8 (0.5) | 4.4 (0.2) | 8.3 (0.4) |
| Sex | ||||
| Female | 58.1 (2.5) | 40.3 (2.4) | 64.7 (2.6) | 40.7 (2.6) |
| Male | 41.9 (2.5) | 59.7 (2.4) | 35.3 (2.6) | 59.3 (2.6) |
| Age, Mean (SE) | 67.7 (0.7) | 65.3 (0.6) | 66.9 (0.9) | 64.4 (0.6) |
| Age Group , % (SE) | ||||
| 40-49 | 9.7 (1.9) | 10.6 (1.6) | 12.6 (2.4) | 12.2 (1.8) |
| 50-59 | 16.1 (2.2) | 22.5 (2.3) | 15.3 (2.5) | 23.2 (2.5) |
| 60-69 | 24.5 (2.3) | 27.9 (1.9) | 24.6 (2.6) | 28.5 (1.8) |
| 70 or over | 49.7 (2.6) | 39.0 (2.2) | 47.5 (3.3) | 36.0 (2.2) |
| Race/ethnicity† | ||||
| Non - Hispanic White | 78.8 (2.1) | 84.6 (1.6) | 76.8 (2.4) | 84.6 (1.6) |
| Non - Hispanic Black | 14.0 (2.0) | 6.9 (0.9) | 15.9 (2.4) | 6.7 (0.9) |
| Mexican American | 3.3 (0.9) | 2.7 (0.7) | 3.5 (0.9) | 2.6 (0.6) |
| Body Mass Index (kg/m2), Mean (SE) | 28.5 (0.3) | 28.9 (0.2) | 28.6 (0.4) | 29.1 (0.3) |
Estimates are proportions or means and their standard errors.
“Other” race/ethnicitycategory not reported.
The overall prevalence of any reported walking difficulty in the NHANES population among individuals 60 and older was 33.2% (95% CI 30.8, 35.6). In contrast, the reported rate of walking difficulty was 51.3% (95%CI 46.3, 56.3) among persons of this same age range with an ABI<0.90. The diagnostic utility of measures of walking difficulty for the identification of PAD defined by an ABI<0.9 are presented in Table 2. Measures of walking difficulty were highly specific for the identification of persons with PAD (i.e., defined by a low ABI) but were not particularly sensitive. When information from all three walking difficulty questions was combined, having “some” or “much” difficulty walking or being “unable” to walk a quarter mile, 10 steps, or from room to room had a sensitivity (probability of any walking difficulty in persons with ABI <0.9) of 49.4% (95%CI, 44.3 to 54.5) and a specificity (probability of no walking difficulty in persons with a normal ABI) of 73.0% (95%CI, 70.4 to 75.6). The corresponding positive predictive value (probability of ABI <0.9 in persons with any walking difficulty) was 18.8% (95%CI 15.6, 22.5) and negative predictive value (probability of normal ABI in persons with no walking difficulty) was 91.9% (95%CI, 91.0 to 93.0).
Table 2.
Diagnostic accuracy of measures walking difficulty to identify peripheral arterial disease as defined by low ankle-brachial index (ABI <0.90), Adults 60+, NHANES 1999-2004 ,N=3,533
| Sensitivity (95% CI) |
Specificity (95% CI) |
Positive predictive value (95% CI) |
Negative predictive value (95% CI) |
|
|---|---|---|---|---|
| Difficulty walking a quarter mile | ||||
| Some (or more) | 44.34 (39.81,48.97) | 78.18 (75.84,80.34) | 20.46 (17.22,24.12) | 91.73 (90.44,92.86) |
| Much (or more) | 23.37 (18.43, 29.16) | 91.89 (90.37, 93.18) | 26.72 (20.82, 33.58) | 90.45 (88.99,91.74) |
| Unable | 11.14 (7.56,16.12) | 96.27 (95.14, 97.14) | 27.41 (17.53, 40.15) | 89.54 (88.09, 90.83) |
| Difficulty walking up 10 steps without resting | ||||
| Some (or more) | 31.87 (25.98, 38.41) | 81.87 (79.51, 84.02) | 18.20 (14.33, 22.85) | 90.47 (88.84, 91.88) |
| Much (or more) | 12.19 (8.6,17.01) | 95.09 (94.03, 95.97) | 23.92 (16.96, 32.60) | 89.53 (88.04, 90.86) |
| Unable | 4.45 (2.45, 7.95) | 98.36 (97.69, 98.83) | 25.52 (13.93, 42.04) | 89.05 (87.51, 90.42) |
| Difficulty walking from room to room | ||||
| Some (or more) | 5.62 (3.73, 8.38) | 97.56 (96.83, 98.13) | 22.59 (15.05, 32.46) | 89.09 (87.48, 90.51) |
| Much (or more) | 1.03 (0.42, 2.52) | 99.82 (99.62, 99.91) | 41.94 (18.06, 70.31) | 88.85 (87.28, 90.24) |
| Unable* | -* | -* | -* | -* |
|
Any difficulty walking (quarter mile, 10 steps, or room to room) |
||||
| Some (or more) | 49.38 (44.29, 54.49) | 73.04 (70.36, 75.57) | 18.82 (15.64, 22.48) | 91.94 (90.69, 93.03) |
| Much (or more) | 25.67 (20.68, 31.38) | 90.48 (89.00,91.77) | 25.43 (20.30,31.36) | 90.58 (89.14, 91.84) |
| Unable | 11.90 (8.11,17.14) | 95.64 (94.45, 96.59) | 25.70 (16.96, 36.93) | 89.56 (88.08, 90.87) |
Cell size too small to make reliable estimates.
In multivariable logistic regression models, an ABI <0.90 was a robust predictor of walking difficulty, even after adjustment for demographics, co-morbidities, cardiovascular risk factors and general health status (OR = 1.98, 95% CI 1.49, 2.62, see Table 3, Model 3). Age, hypertension, male gender, a history of coronary heart disease, smoking, and self-rated health status were also consistent predictors of walking difficulty in older adults. Nonetheless, the association between walking mobility and low ABI was not highly confounded by the classic atherosclerosis risk factors. In other words, the coefficient for ABI <0.90 changed only modestly comparing Model 2 (adjusted for age, demographics, co-morbidities, and cardiovascular risk factors) and Model 3 (adjusted for all variables in Model 2 plus general health status) to Model 1 (adjusted for demographics only). Body mass index was not associated with PAD in this study population and this measure was not included in our multivariable models. In sensitivity analyses, the ORs for the covariates presented in Table 3 remained similar when ABI was modeled as a continuous variable and (data not shown).
Table 3.
Adjusted odds ratios (95% CI) of any walking dysfunction in adults 60+, NHANES 1999-2004
| Model 1 OR (95% CI) |
Model 2 OR (95% CI) |
Model 3 OR (95% CI) |
|
|---|---|---|---|
| Ankle brachial index <0.90 (peripheral arterial disease) | 2.31 (1.82, 2.93) | 2.06 (1.56, 2.71) | 1.98 (1.49, 262) |
| Age (per 10 years) | 1.44 (1.30, 1.59) | 1.41 (1.25, 1.58) | 1.42 (1.25, 1.61) |
| Male (vs. Female) | 1.90 (1.65, 2.19) | 2.19 (1.80, 2.67) | 2.20 (1.80, 2.69) |
| Race/ethnicity (vs. Non-Hispanic White) | |||
| Non-Hispanic Black | 1.46 (1.11,1.92) | 1.34 (1.01, 1.80) | 1.11 (0.84, 1.48) |
| Mexican American | 1.04 (0.80, 137) | 1.04 (0.78, 1.40) | 0.75 (0.56, 1.00) |
| Other | 0.90 (0.62, 1.2) | 0.99 (0.66, 1.46) | 0.80 (0.53, 1.19) |
| History of coronary heart disease (yes vs. no) | - | 1.72 (1.35, 2.20) | 1.33 (1.02, 1.72) |
| Diabetes (yes vs. no) | - | 1.46 (1.12, 1.89) | 1.20 (0.87, 1.65) |
| Smoking (vs. never) | - | ||
| Current | - | 1.66 (1.14, 2.40) | 1.50 (1.04, 2.17) |
| Former | - | 1.38 (1.11, 1.72) | 1.35 (1.09, 1.66) |
| Hypertension (yes vs. no) | - | 1.39 (1.09, 1.76) | 1.37 (1.07, 1.76) |
| Hypercholesterolemia (yes vs. no) | - | 0.98 (0.80, 1.19) | 0.98 (0.80, 1.19) |
| Self-rated general health status (fair/poor vs excellent/very good/good) |
- | - | 3.60 (2.72, 4.76) |
Legend: Walking dysfunction was defined as having “some difficulty,” “much difficulty,” or “unable to do” when “walking for a quarter mile (that isabout 2 or 3 blocks],” “walking up 10 steps without resting,” or “walking from one room to another on the same level.” The sample size here was limited to all persons age 60 and older.
Model 1 is adjusted for age, sex, and race/ethnicity. Model 2 isadjusted for all variables in Model 1 plus history of coronary heart disease, diabetes status, smoking status, hypertension, and hypercholesterolemia. Model 3 isadjusted for all variables in Model 2plus self-rated general health status.
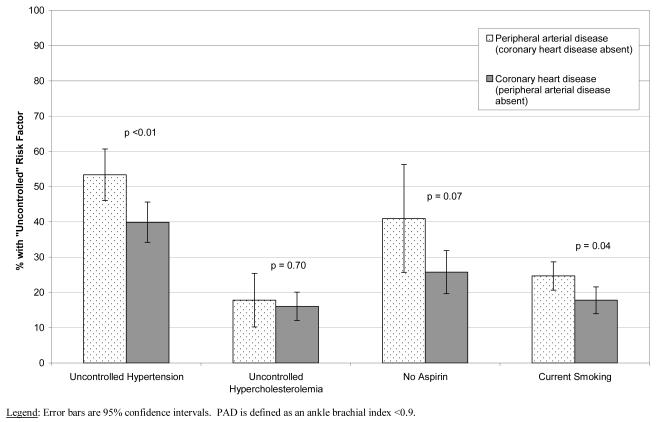
The prevalence of PAD overlapped strongly with existing classic atherosclerosis risk factors with 89.5% (95% CI 86.6 to 92.5) of persons with PAD having at least one other major risk factor (i.e., hypertension, hypercholesterolemia, diabetes, or smoking). Table 4 shows the prevalence of major cardiovascular risk factors and awareness, treatment, and control of hypertension and hypercholesterolemia in adults 40 years or older in 1999-2004 in the following four groups: All individuals with PAD (“total PAD” group); all individuals with CHD (“total CHD” group); individuals with PAD but no history of CHD; or individuals with CHD but no history of PAD. The prevalence of hypertension was high at >65% in all groups, with no difference comparing individuals with PAD without a history of CHD to persons with CHD without PAD (p-value = 0.75). However, awareness, treatment and control of hypertension were all significantly lower among individuals with PAD without a history of CHD compared to individuals with CHD without PAD. The prevalence of hypercholesterolemia was higher among persons with a history of CHD without PAD (56.3% vs 42.2%, p-value <0.001) as was awareness (91.8% vs 84.1%, p-value = 0.07) and treatment (78.9% vs 54.2%, p-value <0.001), but no differences were observed between the groups in control of high cholesterol (83.8 vs 85.8%, p-value = 0.78). Neither treatment nor control of diabetes differed between the two groups by any of the measures examined (all p-values >0.05). There was, however, a much higher prevalence of current smoking among individuals with PAD (25.8% vs 18.3%, p-value <0.01. The Framingham Risk Score—a summary measure of cardiovascular risk factors here— was similar in the two groups. Daily aspirin use was higher among individuals with CHD without PAD compared to individuals with PAD but no clinically recognized CHD (74.3 vs 59.5%,), but this result was of borderline statistical significance, (p-value=0.07). A direct comparison of the prevalence of “uncontrolled” risk factors comparing persons with PAD (but without CHD) to individuals with CHD (but without PAD) is presented in Figure 1. Similar results for the prevalence of major cardiovascular risk factors were observed when analyses were stratified by age (data not shown).
Table 4.
Prevalence and control of risk factors in adults 40 or older with peripheral arterial disease (PAD) or coronary heart disease (CHD) *, NHANES 1999 - 2004
| Total PAD N =595 |
Total CHD N = 845 |
PAD (ABI <0.90) without a history of CHD N = 448 |
CHD without PAD (ABI <0.90) N = 698 |
P-value‡ | |
|---|---|---|---|---|---|
| Hypertension, % (SE) | 70.9 (2.2) | 67.7 (2.1) | 67.7 (2.4) | 65.5 (2.3) | 0.56 |
| Aware, % (SE) | 82.4 (1.8) | 89.5 (1.4) | 80.1 (22) | 89.8 (1.6) | 0.002 |
| Treated, % (SE) | 70.2 (2.8) | 83.6 (1.4) | 66.2 (3.2) | 84.3 (1.7) | <0.001 |
| Controlled, % (SE) | 48.0 (3.5) | 58.5 (3.0) | 46.6 (3.7) | 60.1 (2.9) | 0.004 |
| High total cholesterol (≥240 mg/dl) , % (SE) | 48.1 (2.6) | 57.7 (1.8) | 42.2 (2.7) | 56.4 (1.8) | <0.001 |
| Aware, % (SE) | 84.2 (2.5) | 91.7 (1.8) | 81.3 (3.2) | 92.1 (1.8) | 0.006 |
| Treated, % (SE) | 62.3 (3.7) | 79.6 (2.6) | 53.0 (4.5) | 79.5 (3.1) | <0.001 |
| Controlled, % (SE) | 82.0 (3.5) | 83.6 (2.2) | 82.2 (3.9) | 83.9 (2.0) | 0.70 |
| Diagnosed diabetes, % | 20.0 (2.5) | 20.6 (1.6) | 17.1 (2.5) | 19.2 (2.0) | 0.54 |
| No medication use, % (SE) | 11.1 (4.2)‡ | 15.6 (3.8) | 15.2 (6.0)‡ | 18.7 (4.5) | 0.64 |
| Insulin only, % (SE) | 22.3 (5.5) | 16.2(3.6) | 10.6 (3.7) | 9.3 (2.2) | 0.74 |
| Oral medications only, % (SE) | 54.8 (6.4) | 53.9 (4.5) | 57.3 (6.8) | 54.8 (5.2) | 0.76 |
| Both insulin and oral medications, % (SE) | 11.9 (2.5) | 14.3 (3.6) | 16.9 (4.1) | 17.2 (4.4) | 0.94 |
| Mean hemoglobin A1c , %-point (SE) | 7.4 (0.2) | 7.1 (0.1) | 7.5 (0.3) | 7.0 (0.1) | 0.19 |
| Smoking, % (SE) | |||||
| Current | 24.8 1.7) | 18.9 (1.7) | 24.7 (2.0) | 17.8 (1.9) | 0.006 |
| Former | 40.9 (2.7) | 46.0 (1.9) | 36.6 (3.2) | 44.6 (2.0) | 0.04 |
| Peripheral arterial disease (ABI <0.9), % (SE) | - | 14.8 (1.7) | - | - | - |
| History of coronary heart disease, % (SE) | 25.5 (2.5) | - | - | - | - |
| History of stroke, % (SE) | 10.4 (1.4) | 12.1 (1.5) | 7.2 (1.3) | 10.7 (1.5) | 0.12 |
| Daily aspirin Use, % (SE)§ | 63.8 (5.9) | 74.3 (2.7) | 59.0 (7.8) | 74.3 (3.1) | 0.07 |
| Mean Framingham Risk Score, points (SE) | 14.8 (0.7) | 14.0 (0.6) | 13.7 (0.8) | 13.3 (0.6) | 0.63 |
| Framingham Risk Score | |||||
| < 10% | 31.6 (3.4) | 32.3 (3.2) | 35.8 (3.6) | 34.5 (3.2) | 0.79 |
| 10-20% | 42.3 (3.8) | 45.5 (2.6) | 42.3 (3.8) | 46.0 (2.6) | 0.48 |
| >20% | 26.1 (3.3) | 22.2 (2.5) | 21.8 (3.3) | 19.5 (2.4) | 0.51 |
Analyses limited to those persons non-missing information on cardiovascular risk factor and treatment information (N=7,100).
P-values for comparison of the PAD without a history of CHD group to the CHD without a history of PAD group.
Relative standard error is >30%. Estimate may be unreliable.
At the time of submission, data on aspirin use was not available for NHANES 2003-2004 The analysis of aspirin use is based on data from NHANES 1999-2002 only (N= 1,410)
Figure 1.
Prevalence of uncontrolled cardiovascular risk factors and lack of aspirin treatment comparing persons with peripheral arterial disease (without coronary heart disease) to persons with coronary heart disease (without peripheral arterial disease), adults 40 or older, NHANES 1999-2004
DISCUSSION
This study provides a nationally representative assessment of contemporary risk factor treatment and control among persons with PAD in the general U.S. population. These data confirm that control of ischemic risk for those with PAD has not achieved the gains achieved for individuals with known CHD. The overall PAD prevalence of 5.8% represents 6.9 million individuals (95% CI 6.2 to 7.7 million) and indicates the “yield” of individuals with PAD if the ABI was used in clinical practice as in the NHANES survey as a diagnostic method to identify individuals with PAD in the general U.S. population aged 40 and older. After excluding individuals with a known history of CHD, the use of the ABI would still identify a slightly smaller population of 4.4% (5.3 million individuals, 95% CI 4.7 to 5.7). In other words, approximately 75% of the population at high risk for a cardiovascular ischemic event due to the presence of PAD cannot be identified from a clinical history of CHD alone. The prevalence of PAD estimated here is consistent with estimates using the ABI from large, community based studies including the Cardiovascular Health Study (4), the Atherosclerosis Risk in Communities Study (23), the Framingham Study (24), and previous NHANES publications (25;26).
Numerous studies have established a low ABI, and thus PAD, as an atherosclerotic disease associated with high risk for fatal and non-fatal myocardial infarction, stroke, and death (1-6;27;28). Thus, there is consensus amongst individual investigators, international atherosclerosis care guidelines, and more specific PAD care guidelines which recommend the use of the ABI to detect PAD in target populations in which PAD prevalence is known to be high (3;7;29;30). Several PAD public health advocacy consortiums and non-profit foundations have also issued statements calling for increased awareness, improved detection, and implementation of targeted diagnostic protocols for PAD (31;32). Targeted evaluation by use of the ABI is also recommended by the American Diabetes Association among all individuals aged 50 or older with diabetes (33;34). For individuals with diabetes, the documentation of a low ABI may permit both insight into leg symptoms (that may not be merely neuropathic) and could serve to highlight amputation prevention treatments in this high risk population. The ABI may also serve as a motivational tool to achieve cardiovascular risk reduction target goals in individuals with diabetes. Further studies are needed to assess whether ABI testing may reduce the risk of leg amputation and diabetes-related lower-limb complications.
Our data demonstrate that risk factor control among individuals with PAD has not yet achieved parity with individuals with CHD. We found that PAD in the absence of clinically recognized CHD was under-treated and poorly controlled. In particular, less than 50% of persons with PAD without a history of CHD who had hypertension were adequately controlled. Control of hypertension among individuals with a history of CHD was only somewhat better (with 60% controlled). Given that individuals with diabetes who also have a history of CHD are at extremely high risk for a future cardiovascular disease event, one might have expected higher rates of risk factor treatment and control in this group compared to individuals with a low ABI but without a history of CHD; however, this was not the case. Prevalence and control of diabetes was similar in the two groups, suggesting that diabetes alone – and the physician and patient education programs that lead to improved control – have been adequate to effect treatment.
The high prevalence of current smoking in individuals with PAD is concerning; the 25% prevalence of current smoking in this high risk population highlights the need for aggressive smoking cessation efforts, as called for in national PAD guidelines. Also concerning was the low prevalence of daily aspirin use (59%).
Detection of PAD, while most efficiently performed by use of the ABI, could theoretically also be accomplished if clinicians utilized a review of walking impairment in high risk PAD populations, although many PAD cases might be missed with this strategy. As shown in previous studies, a low ABI is clearly associated with decreased walking mobility (12-14); approximately half of all persons aged 60+ with a ABI <0.9 also had some level of walking mobility limitation. Even after adjusting for health status and known risk factors for PAD, ABI was strongly associated with walking dysfunction. Our results suggest that walking limitations are quite specific for the identification of persons with an ABI <0.9, but will be inadequate to detect a high fraction of individuals with PAD.
This study benefited from the large sample size and the rigorous methodology in NHANES which provides nationally representative estimates, and is thus generalizable to the U.S. adult population aged 40 and older. Importantly, the NHANES data allowed for identification of individuals with PAD regardless of the participant or their physician’s awareness of the condition. Nonetheless, several important limitations of this study should be considered. The cross-sectional nature of the study limits our ability to draw conclusions regarding the temporality of the observed relationships. The use of self-reported information for coronary heart disease is likely to have underestimated the true burden of this disease in the population. However, use of self-reported history is highly specific and reflects a common clinical decision-making tool used in all practice settings. The ABI is also an imperfect gold standard for the presence of large vessel lower extremity arterial disease. However, the ABI nonetheless has high sensitivity and specificity for identifying subclinical disease and remains the most common clinical tool for the assessment of asymptomatic PAD. There are also important limitations to the physical functioning assessment in NHANES. To avoid selection issues related to the skip-patterns in the activity limitation portion of the questionnaire, we limited our analysis to participants aged 60+. Nonetheless, the mobility limitation questions asked about difficulties related to an unspecified “health problem” and this may have characterized individuals differently than if physical functioning abilities had been assessed in all individuals regardless of their perceived health status. A “survival effect” is also an inherent limitation of cross-sectional data; that is, individuals who survived a heart attack and/or are living with CHD may have a more favorable risk factor profile compared to individuals who died and were not classified as CHD cases in this study.
These data verify that the vast majority of individuals with PAD have co-existing risk factors for cardiovascular disease, indicating these patients should already have been identified for cardiovascular risk management. However, the presence of PAD is known to independently increase the short term risk of ischemic events (2;35;36) and the suboptimal control of treatment and control of cardiovascular risk factors is concerning.
Conclusions
The NHANES data demonstrate that PAD is common, and that over three fourths of individuals with PAD do not have a clinical history of CHD. Although ischemic event rates in individuals with PAD are known to be comparable to those that occur in individuals with CHD, treatment and control of major atherosclerosis risk factors are not comparable. Walking impairment is significant in those with PAD, and is associated with the severity of PAD as defined by the ABI. Nevertheless, a history of walking impairment is not a sensitive tool to diagnose PAD. Prospective data are required to verify that routine use of the ABI would prompt clinicians to initiate treatments that are known to be effective or would increase long-term compliance with treatment recommendations. Aggressive risk factor management, linked to prompt establishment of the PAD diagnosis, may be an effective public health strategy for the prevention of cardiovascular ischemic events in individuals with this common atherosclerotic syndrome.
Acknowledgements
Dr. Selvin was supported by NIH/NIDDK Grant K01 DK076595.
Reference List
- (1).Newman AB, Sutton-Tyrrell K, Vogt MT, Kuller LH. Morbidity and mortality in hypertensive adults with a low ankle/arm blood pressure index. JAMA. 1993;270(4):487–489. [PubMed] [Google Scholar]
- (2).Murabito JM, Evans JC, Larson MG, Nieto K, Levy D, Wilson PWF. The Ankle-Brachial Index in the Elderly and Risk of Stroke, Coronary Disease, and Death: The Framingham Study. Archives of Internal Medicine. 2003;163(16):1939–1942. doi: 10.1001/archinte.163.16.1939. [DOI] [PubMed] [Google Scholar]
- (3).Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation. 2002;106(25):3143. [PubMed] [Google Scholar]
- (4).Newman AB, Shemanski L, Manolio TA, Cushman M, Mittelmark M, Polak JF, et al. Ankle-Arm Index as a Predictor of Cardiovascular Disease and Mortality in the Cardiovascular Health Study. Arterioscler Thromb Vasc Biol. 1999;19(3):538–545. doi: 10.1161/01.atv.19.3.538. [DOI] [PubMed] [Google Scholar]
- (5).Criqui MH, Langer RD, Fronek A, Feigelson HS, Klauber MR, McCann TJ, et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992;326(6):381–386. doi: 10.1056/NEJM199202063260605. [DOI] [PubMed] [Google Scholar]
- (6).Criqui MH, Coughlin SS, Fronek A. Noninvasively diagnosed peripheral arterial disease as a predictor of mortality: results from a prospective study. Circulation. 1985;72(4):768–773. doi: 10.1161/01.cir.72.4.768. [DOI] [PubMed] [Google Scholar]
- (7).Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 Practice Guidelines for the Management of Patients With Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic): A Collaborative Report from the American Association for Vascular Surgery/Society for Vascular Surgery,* Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 2006;113(11):e463–e465. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]
- (8).Vogt MT, McKenna M, Anderson SJ, Wolfson SK, Kuller LH. The relationship between ankle-arm index and mortality in older men and women. J Am Geriatr Soc. 1993;41(5):523–530. doi: 10.1111/j.1532-5415.1993.tb01889.x. [DOI] [PubMed] [Google Scholar]
- (9).Hirsch AT, Gotto AM., Jr Undertreatment of dyslipidemia in peripheral arterial disease and other high-risk populations: an opportunity for cardiovascular disease reduction. Vascular Medicine. 2002;7(4):323–331. doi: 10.1191/1358863x02vm453ra. [DOI] [PubMed] [Google Scholar]
- (10).Nass CM, Allen JK, Jermyn RM, Fleisher LA. Secondary prevention of coronary artery disease in patients undergoing elective surgery for peripheral arterial disease. Vascular Medicine. 2001;6(1):35–41. doi: 10.1177/1358836X0100600107. [DOI] [PubMed] [Google Scholar]
- (11).Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW, et al. Peripheral Arterial Disease Detection, Awareness, and Treatment in Primary Care. JAMA: The Journal of the American Medical Association. 2001;286(11):1317–1324. doi: 10.1001/jama.286.11.1317. [DOI] [PubMed] [Google Scholar]
- (12).Eberhardt MS, Saydah S, Paulose-Ram R, Tao M. Mobility Limitation Among Persons Aged ΓëÑ40 Years With and Without Diagnosed Diabetes and Lower Extremity Disease -- United States, 1999-2002. MMWR: Morbidity & Mortality Weekly Report. 2005;54(46):1183–1186. [PubMed] [Google Scholar]
- (13).McDermott MM, Mehta S, Liu K, Guralnik JM, Martin GJ, Criqui MH, et al. Leg Symptoms, the Ankle-Brachial Index, and Walking Ability in Patients With Peripheral Arterial Disease. Journal of General Internal Medicine. 1999;14(3):173–181. doi: 10.1046/j.1525-1497.1999.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (14).McDermott MM, Greenland P, Liu K, Guralnik JM, Celic L, Criqui MH, et al. The Ankle Brachial Index Is Associated with Leg Function and Physical Activity: The Walking and Leg Circulation Study. Ann Intern Med. 2002;136(12):873–883. doi: 10.7326/0003-4819-136-12-200206180-00008. [DOI] [PubMed] [Google Scholar]
- (15).Wattanakit K, Folsom AR, Duprez DA, Weatherley BD, Hirsch AT. Clinical significance of a high ankle-brachial index: Insights from the Atherosclerosis Risk in Communities (ARIC) Study. Atherosclerosis. 2007;190(2):459–464. doi: 10.1016/j.atherosclerosis.2006.02.039. [DOI] [PubMed] [Google Scholar]
- (16).Feigelson HS, Criqui MH, Fronek A, Langer RD, Molgaard CA. Screening for peripheral arterial disease: the sensitivity, specificity, and predictive value of noninvasive tests in a defined population. Am J Epidemiol. 1994;140(6):526–534. doi: 10.1093/oxfordjournals.aje.a117279. [DOI] [PubMed] [Google Scholar]
- (17).Lijmer JG, Hunink MGM, van den Dungen JJAM, Loonstra J, Smit AJ. ROC analysis of noninvasive tests for peripheral arterial disease. Ultrasound in Medicine & Biology. 1996;22(4):391–398. doi: 10.1016/0301-5629(96)00036-1. [DOI] [PubMed] [Google Scholar]
- (18).Ouriel K, McDonnell AE, Metz CE, Zarins CK. Critical evaluation of stress testing in the diagnosis of peripheral vascular disease. Surgery. 1982;91(6):686–693. [PubMed] [Google Scholar]
- (19).Rose G, McCartney P, Reid DD. Self-administration of a questionnaire on chest pain and intermittent claudication. Br J Prev Soc Med. 1977;31(1):42–48. doi: 10.1136/jech.31.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Leng GC, Fowkes FG. The Edinburgh Claudication Questionnaire: an improved version of the WHO/Rose Questionnaire for use in epidemiological surveys. J Clin Epidemiol. 1992;45(10):1101–1109. doi: 10.1016/0895-4356(92)90150-l. [DOI] [PubMed] [Google Scholar]
- (21).Survey Operations Manuals, Brochures, and Consent Documents: 1999-current NHANES. National Center for Health Statistics, Centers for Disease Control; 2007. http://www.cdc.gov/nchs/about/major/nhanes/currentnhanes.htm: [Google Scholar]
- (22).National Center for Health Statistics [Last Accessed May 9,2007];National Health and Nutrition Examination Survey (NHANES) Analytic Guidelines. 2007 http://www cdc gov/nchs/about/major/nhanes/nhanes2003-2004/analytical_guidelines htm.
- (23).Zheng ZJ, Sharrett AR, Chambless LE, Rosamond WD, Nieto FJ, Sheps DS, et al. Associations of ankle-brachial index with clinical coronary heart disease, stroke and preclinical carotid and popliteal atherosclerosis:: the Atherosclerosis Risk in Communities (ARIC) Study. Atherosclerosis. 1997;131(1):115–125. doi: 10.1016/s0021-9150(97)06089-9. [DOI] [PubMed] [Google Scholar]
- (24).Murabito JM, Evans JC, Nieto K, Larson MG, Levy D, Wilson PWF. Prevalence and clinical correlates of peripheral arterial disease in the Framingham Offspring Study. American Heart Journal. 2002;143(6):961–965. doi: 10.1067/mhj.2002.122871. [DOI] [PubMed] [Google Scholar]
- (25).Gregg EW, Sorlie P, Paulose-Ram R, Gu Q, Eberhardt MS, Wolz M, et al. Prevalence of Lower-Extremity Disease in the U.S. Adult Population >=40 Years of Age With and Without Diabetes: 1999-2000 National Health and Nutrition Examination Survey. Diabetes Care. 2004;27(7):1591–1597. doi: 10.2337/diacare.27.7.1591. [DOI] [PubMed] [Google Scholar]
- (26).Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004;110(6):738–743. doi: 10.1161/01.CIR.0000137913.26087.F0. [DOI] [PubMed] [Google Scholar]
- (27).Weatherley B, Nelson J, Heiss G, Chambless L, Sharrett AR, Nieto FJ, et al. The association of the ankle-brachial index with incident coronary heart disease: the Atherosclerosis Risk In Communities (ARIC) study, 1987-2001. BMC Cardiovascular Disorders. 2007;7(1):3. doi: 10.1186/1471-2261-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (28).Doobay AV, Anand SS. Sensitivity and Specificity of the Ankle-Brachial Index to Predict Future Cardiovascular Outcomes: A Systematic Review. Arterioscler Thromb Vasc Biol. 2005;25(7):1463–1469. doi: 10.1161/01.ATV.0000168911.78624.b7. [DOI] [PubMed] [Google Scholar]
- (29).Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA: The Journal of the American Medical Association. 2003;289(19):2560–2571. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- (30).Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FGR. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) Journal of Vascular Surgery. 2007;45(1 Supplement 1):S5–S67. doi: 10.1016/j.jvs.2006.12.037. [DOI] [PubMed] [Google Scholar]
- (31).Belch JJF, Topol EJ, Agnelli G, Bertrand M, Califf RM, Clement DL, et al. Critical Issues in Peripheral Arterial Disease Detection and Management: A Call to Action. Archives of Internal Medicine. 2003;163(8):884–892. doi: 10.1001/archinte.163.8.884. [DOI] [PubMed] [Google Scholar]
- (32).Hirsch AT, Gloviczki P, Drooz A, Lovell M, Creager MA. Mandate for Creation of a National Peripheral Arterial Disease Public Awareness Program: An Opportunity to Improve Cardiovascular Health. Vascular and Endovascular Surgery. 2004;38(2):121–130. doi: 10.1177/153857440403800203. [DOI] [PubMed] [Google Scholar]
- (33).Peripheral Arterial Disease in People With Diabetes. Diabetes Care. 2003;26(12):3333–3341. doi: 10.2337/diacare.26.12.3333. [DOI] [PubMed] [Google Scholar]
- (34).American Diabetes Association Standards of Medical Care in Diabetes--2007. Diabetes Care. 2007;30(suppl1):S4–41. [PubMed] [Google Scholar]
- (35).Wild SH, Byrne CD, Smith FB, Lee AJ, Fowkes FG. Low Ankle-Brachial Pressure Index Predicts Increased Risk of Cardiovascular Disease Independent of the Metabolic Syndrome and Conventional Cardiovascular Risk Factors in the Edinburgh Artery Study. Diabetes Care. 2006;29(3):637–642. doi: 10.2337/diacare.29.03.06.dc05-1637. [DOI] [PubMed] [Google Scholar]
- (36).Heald CL, Fowkes FGR, Murray GD, Price JF. Risk of mortality and cardiovascular disease associated with the ankle-brachial index: Systematic review. Atherosclerosis. 2006;189(1):61–69. doi: 10.1016/j.atherosclerosis.2006.03.011. [DOI] [PubMed] [Google Scholar]