Abstract
Background
Real-time sharing of blood glucose results with providers could improve communication and lead to more timely medication titration. New technology platforms are available to support the delivery of innovative models of care delivery.
Methods
In the Diabetes Connected Health (DCH) pilot study, patients with diabetes received access to an online application that stored and graphed glucose readings uploaded from a standard glucometer. Both patients and providers had access to this Web site, where data could be viewed, analyzed, and discussed. To examine the impact of the DCH program, we assessed adoption of the program, patient and provider satisfaction, frequency of use, and changes in glucose levels over a period of 3 months.
Results
The mean age of the 7 pilot participants was 51 (range 35–65). Participants sent in an average of 50 readings in Month 1 and 38 readings in Month 3 and made, on average, 6 comments in Months 1 and 12 comments in Month 3. The mean blood glucose range decreased in Month 3 versus Month 1 (141.1 and 146.5, respectively). Self-reported HbA1c fell from 6.8% at the start of the study to 5.8% at the end. Five/seven participants described the site as excellent or good. Qualitative data analysis highlighted key benefits of the program as well as areas for improvement.
Conclusions
This pilot study of a shared glucose monitoring Web application was well received by patients. Programs like this may lead to improvements in the quality of clinical care delivered to people with type 2 diabetes.
Keywords: connected health, diabetes, internet, pilot
Background
Self-monitoring of blood glucose may improve self-care among patients with diabetes when coupled with relevant lifestyle information that can be used by providers to enhance patient education and motivation. Traditionally patients with diabetes receive their care in face-to-face clinical encounters and monitor their blood glucose between visits using portable glucometers. These blood sugar readings and the associated information they carry are recorded in a portable notebook or in the glucometers themselves. Provider-directed changes in diet and medication are made during clinical visits (typically 3–6 visits/year) or sometimes by phone or even e-mail exchanges based in part on the information found in this glucose log.
Considerable evidence exists that “current standard of care” frequently fails to deliver on evidence-based recommendations for practice.1,2 Requirements for more transparent reporting of outcomes and new payment systems that reimburse based on outcomes rather than visits are driving healthcare systems to explore new methods of care delivery.
Several information and communication solutions have emerged as feasible strategies to enhance the flow of information and collaboration between patients and providers.3–5 We designed a remote blood glucose monitoring application [“Diabetes Connected Health” (DCH)] based on an easy-to-use Web site for both patients and their care providers. Linking technology allows patients to upload glucometer readings from commercially available glucometers (One-Touch® Ultra® 2) to a secure Web site using a modem connected through a home telephone line. We designed separate Web site interfaces for patients and providers. We hypothesized that the ongoing shared access to blood glucose readings provided by this program would improve communication between patients and providers and enhance diabetes care. In this paper we report clinical and technical results of our initial pilot study of this novel application.
Research Design and Methods
In the DCH pilot study, patients with diabetes received access to an online application that stored and graphed glucose readings uploaded from a standard glucometer. Both patients and providers had access to this Web site, where the data could be viewed, analyzed, and discussed. To examine the impact of the DCH program, we assessed barriers to implementation and adoption of the program, patient and provider satisfaction, frequency of use, and changes in glucose levels over a period of 3 months. The study was conducted from November 2007 to March 2008 and was approved by the Institutional Review Board at Massachusetts General Hospital.
Setting
Subjects for the pilot study were recruited from the Bulfinch Medical Group (BMG), a primary care practice within the Massachusetts General Hospital practice-based research network. The BMG practice included one nurse practitioner, two registered nurses, and a nutritionist who all shared responsibility for diabetes care with the patient's primary care providers. Nurses were certified in diabetes self-management education.
Participants
A pool of 20 patients was identified by the BMG care team as potential candidates for the pilot study. Inclusion criteria required that patients be diagnosed with type 2 diabetes and that they self-monitored their blood glucose as directed by the treating provider. In addition, participants were required to have access to the Internet and to an analog land-based phone line. Subjects were excluded if they were outside the age range of 18 to 65 years old, had incompatible telephone service, or did not speak English. After an initial telephone screening, eight subjects declined to participate (four were not interested, two lived too far away to participate, and two were not comfortable with the way their data would be used in the study) and five were found to be ineligible (two had no internet access, two had incompatible telephone service, and one was a Mac user incompatible with PCs), leaving seven eligible subjects who enrolled in the pilot program.
Subjects who declined participation in the study were asked a brief set of questions for research purposes. These questions were directed toward obtaining feedback on the study concept and to gather data regarding reasons for declined participation.
Design Features of the Diabetes Connected Health Web Application
The Web site homepage prominently featured a graphic representation of blood glucose readings, clearly depicting trends in readings over time, peaks and troughs, and the user's normal/ideal blood glucose range. The optimal blood glucose range was set by the provider for each individual. Uploading data directly from the glucometer prevented mistakes in entering important statistics in the logbook by circumventing the manual record-keeping process. Additionally the Web site included a “journal” page, which was formatted in a similar fashion to the traditional paper-based logbooks. Due to the convenient upload feature, the online journal eliminated the need for users to handwrite their daily glucose readings. It also provided patients with an area where they were able to make notes and comments about each reading (e.g., foods eaten and moods) without trying to “squeeze” notes into the tiny margins of a paper logbook. Figures 1 and 2 display the patient homepage and journal page.
Figure 1.
Patient home page.
Figure 2.
Patient journal page.
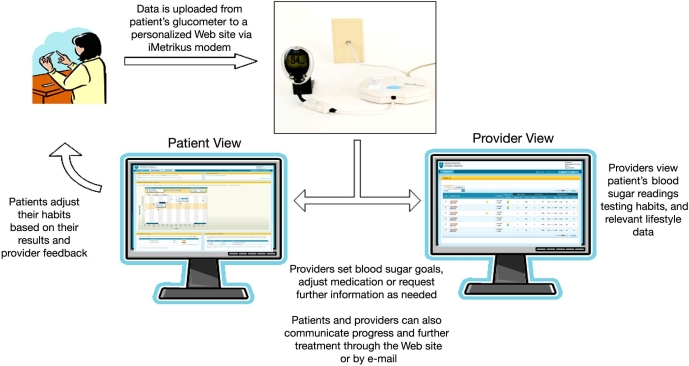
The providers and care management team at BMG also received access to a “provider version” of the Web site and were able to view each subject's blood glucose readings in the same format as the patient. Access to patient blood glucose readings and notes enabled providers to better acquaint themselves with their patient's blood glucose trends and overall management habits, thereby potentially allowing the provider to be more proactive in recommending treatments while avoiding clinical visits. A one-way messaging feature on the provider's Web site allowed them to send comments to each patient based on their assessment of the patient's glucose trends. This was designed to improve communication between provider and patient and to encourage active participation in managing the disease for both parties, without overburdening the clinic practices with unsolicited patient e-mails. During the study, subjects continued to receive usual clinic-based care from their provider. The feedback loop between patient and provider is depicted in Figure 3.
Figure 3.
Diabetes management program feedback loop.
Study Procedures
At the initial study visit, each consented participant was given study equipment, completed an initial survey, and received training materials and a demonstration for the use of the materials and the Web site. Each participant was asked to upload their readings using the modem once per day. Subjects were also asked to log in to the Web site once a day and to use the various features to examine their data.
Subjects were contacted by study staff 1 month after enrollment for a brief follow-up telephone interview and to address any issues or questions that may have arisen. This telephone conversation was recorded and transcribed for later analysis.
At the final study visit, each subject was asked to complete a final questionnaire about the study and was asked for their overall impression of the DCH application. They were given the option to attend a focus group after the close of the study to provide further feedback on their experiences. This information was used to improve the study design and Web site tool for a larger upcoming randomized controlled trial.
The focus group session lasted approximately 3 hours and was facilitated by a member of the study staff who helped to guide the conversation using a series of preestablished, open-ended questions. The session was recorded and transcribed by study staff members who were present at the time of the focus group. The discussion questions were divided into two parts: (1) initial impressions and (2) Web site feedback for the new prototype. For their participation in this focus group, participants were given additional monetary compensation. Quotes from focus group participants were analyzed by members of the research team and categorized according to theme.
Provider satisfaction was assessed using a number of methods. Providers were encouraged to send informal comments and suggestions for improvements to the research team over the course of the study. In addition, a formal focus group session was held with all four providers at the end of the study in order to assess whether they used the site, what they felt worked well, what they felt needed changed, and how they saw this application being used in the future.
Results
Study Population
The mean age of the seven subjects was 51 (range 35–65 years). All participants were white, four were female, five had at least 4 years of college education, and six were employed in full-time jobs. One subject was newly diagnosed, while the remaining six had been managing their diabetes for 5 years or more. All but one subject was on medication for diabetes, six were testing their blood glucose at least twice a day, and four regularly kept a log of their readings. All seven subjects reported moderate to high levels of comfort using the Internet and new electronic technologies.
Use of the Diabetes Connected Health Application
At the final visit, four out of seven subjects reported having kept a consistent log of their blood sugar readings, including the journal section on the diabetes Web site. Some subjects used this feature more often than others and logged many readings and comments throughout the duration of their participation in the study. When asked how often they tested their blood sugar with a glucometer, three subjects responded that their testing habits had increased since the start of the study, two decreased, and one subject reported no change. At the final visit, all pilot subjects were able to define their goal blood sugar range compared to the first visit when only five out of seven subjects were able to define a range.
Changes in Glucose Control
Mean glucose levels declined over the 3 month study period (see Table 1). The mean levels declined from 146.5 (±56.3) in Month 1 to 141.1 (±50.65) in Month 3. In addition, subjects' self-reported mean HBA1c levels decreased over the course of the study from 6.8% (range 5–13.1%) to 5.8% (range 5.7–7.9%).
Table 1.
Summary of Usage Data (n = 7)
| Month 1 (first 30 days) | Month 2 (second 30 days) | Month 3 (third 30 days) | |
|---|---|---|---|
| Mean number of readings (range) | 49.86 (28–71) | 42.43 (26–77) | 38.29 (3–108) |
| Mean number of comments (range) | 6.43 (3–12) | 11.14 (1–46) | 12.14 (3–51) |
| Mean glucose (standard deviation) | 146.53 (56.3) | 147.66 (57.2) | 141.07 (50.65) |
| Percentage low (<80 mg/dl) (range) | 3.4% (2–4) | 2.4% (2–5) | 7.1% (1–18) |
| Percentage high (>180 mg/dl) (range) | 30.1% (1–49) | 16.8% (2–19) | 23.9% (1–46) |
Survey Results
Baseline medication adherence was assessed using the Morisky scale.6 All subjects reported high levels of adherence at both baseline and study end. Subjects were also asked to report how confident they felt about their ability to control their blood sugar. On a scale of 1–10, where 10 is the highest confidence score, the mean reported score at the start of the study was 7.14 (range 7–9). This increased to 7.71 (range 5–9) by the end of the study.
Provider Satisfaction
Three of the four providers used the site on a regular basis. The nutritionist did not use the site, because her work with patients generally focused exclusively on discussions around meal planning. Of the providers who used the site, the key benefits were felt to be improved insight into how often a subject was testing, confidence that data on glucose levels was accurate, and the ability to make medication titrations without requiring the subject to come in for a clinic visit. The key shortcoming of the site was the fact that it did not integrate with the electronic medical record (EMR) and, as such, was difficult to integrate into current workflow.
Participant Satisfaction
When asked how they would rate this Web site overall, five out of seven subjects responded that they thought it was either “Excellent” or “Good,” while the remaining two responded that it was either “Average” or “Satisfactory.” All seven subjects responded that they would continue to use this program to manage their diabetes and would recommend it to a friend or family member with diabetes.
Focus Group Results
Figure 4. summarizes the key findings from the focus group.
Figure 4.

Five key themes identified during focus group discussion.
Discussion
This pilot study provided valuable feedback from diabetes patients on the utility, benefit, and limitations of a Web-based diabetes management portal. Our pilot users remained active participants of the site over the 3 month pilot period, and their mean blood glucose results showed a downward trend over the same period. Although the mean number of readings sent per month dropped over time, the number of comments per month increased, indicating ongoing engagement.
Existing literature suggests that self-monitoring of blood glucose alone may yield limited clinical benefit to patients and may actually lead to detrimental consequences, such as depressed mood.7 Such monitoring, however, is likely to be of value when test results are linked to educational or behavioral advice and changes in clinical management.8 There have been a number of reviews that have previously examined the use of telemedicine in diabetes management.9,10 The review by Jaana and Paré10 on the management of diabetic patients via telemonitoring showed significant reductions in HbA1c and complications, good receptiveness by patients, and patient empowerment and education. However, the studies included in the review were highly variable in design, and the authors concluded that larger samples and further investigation are needed to determine efficacy and cost-effectiveness over longer periods of time. Innovative systems such as this diabetes management tool may lead to better clinical outcomes by improving communication and promoting changes in patient and provider behavior. Formal evaluation in the form of a rigorous randomized clinical trial, however, is required to test this hypothesis.
Lessons Learned
Strengths
Positive feedback from our pilot patients regarding the initial iteration of this diabetes management program suggests that this type of program, if clinically validated, may be a useful tool in outpatient diabetes management. The results also indicate that participation in this program may lead to improved patient knowledge, empowerment, and accountability as well as improved patient–provider communication.
Limitations
This pilot project was limited by the small sample size and short follow-up period. In addition, the demographic characteristics of our participants (who were principally white and educated) limit the generalizability, because we did not include less-educated participants who may be less comfortable using new technology or minority groups disproportionately affected by type 2 diabetes. Despite the well-documented digital divide,11,12 there is evidence that groups less familiar with new technology may also be receptive to adopting new programs to improve their diabetes care. In one study, we noted that, although race and education are significant predictors of receptivity to technology adoption, the baseline level of interest in all groups is high.13 Although we are likely to have captured early adopters in this pilot study, on comparing the pilot subjects to all the type 2 diabetes patients in our primary care network (>6000 patients), they do not appear atypical. The pilot subject had relatively low HbA1c levels at baseline (mean = 6.8%), but the overall control within our larger population was good, with a mean HbA1c of 7.5%. All our study participants were white, as are the majority of patients in our network (67%).14 Clinical data, such as frequency of testing and HbA1c results, were obtained from patient surveys and, as a result of being self-reported, may not be accurate.
This pilot study revealed a number of shortcomings with the current platform that impacted its value to patients or providers:
The messaging feature was rarely used. This was largely due to the fact the messaging was one-way, meaning the patients could not respond to a message sent by their provider. As such, providers and patients continued to rely on familiar modes of communication, such as telephone and regular e-mails.
Providers reported finding it difficult to integrate the use of the Web site into their regular workflow, because the platform did not integrate with other sources of clinical data, such as the EMR. Critical pieces of information, such as recent HbA1c and current medications, were not displayed on the site.
Both patients and providers wanted more flexibility in how the readings were displayed in the graph. There was no consensus among providers around which glucose readings were of most interest to them.
Patients would have liked more flexibility in where and when they could upload readings. The current system required connection through a home telephone line.
Both patients and providers wanted more contextual information around high or low readings. For example, if a high reading was observed, the provider wanted to know if the patient had taken their medication or was feeling unwell. Patients also wanted to be able to “explain” outlier readings to their providers. Although the journal page allowed free text entry, the character limit of 250 was felt to be too restrictive by the participants.
Implications for Future Research
This pilot program provided us with encouraging feedback from patients and providers, but it also yielded a set of new requirements that could enhance the user experience and the value of the product. We have used these requirements to build an improved version of the Web site, which we are currently evaluating in a randomized clinical trial involving 200 patients from 6 primary care practices affiliated with either Massachusetts General Hospital or Brigham and Women's Hospital in Boston. The primary outcome measure in the trial will be change in HbA1c over the 6-month study period.
Key improvements to the Web site include the following:
Introduction of two-way messaging. The message must be initiated by the provider, but the patient can now provide a response.
Integration of the program with other data sources, such as the EMR. Information from the EMR will be displayed on the diabetes Web site, and messages sent via the Web site will be recorded as notes in the EMR.
Introduction of a population manager view for providers. A provider can now view a summary page detailing all their patients along with key metrics, such as percentage of high or low readings. This allows providers to triage care accordingly to those most in need. In addition, the provider can add patients whom they are particularly concerned about to a “watch” list.
Improvements to graphing feature. Providers and patients can now customize the appearance of the graph according to the time period and the type of readings they want to view. For example, it is possible to display only bedtime readings for the past month or all readings over the past 6 months, depending on user preference.
We are developing a new method of data upload via a computer rather than using a phone line. This offers participants more flexibility around where and when they upload data.
Participants are now directed to annotate high and low readings by answering a standard short set of questions around these readings and adding fee text information.
The Web site now displays information about current medications. Dates where medication changes were made are highlighted on the graph to help participants identify trends.
This diabetes management program requires more rigorous testing, better baseline and end-of-study biometric measures, and larger sample sizes of patients over a longer period of time to truly gauge the impact it has on diabetes health and management. Initial feedback from patients and providers, however, is encouraging. If this program is successful, it has the potential to truly impact the way diabetes care is delivered and to improve both clinical and economic outcomes.
Abbreviations
- BMG
Bulfinch Medical Group
- DCH
Diabetes Connected Health
- EMR
electronic medical record
References
- 1.Beckles GL, Engelgau MM, Narayan KM, Herman WH, Aubert RE, Williamson DF. Population-based assessment of the level of care among adults with diabetes in the U.S. Diabetes Care. 1998;21(9):1432–1438. doi: 10.2337/diacare.21.9.1432. [DOI] [PubMed] [Google Scholar]
- 2.Saaddine JB, Cadwell B, Gregg EW, Engelgau MM, Vinicor F, Imperatore G, Narayan KM. Improvements in diabetes processes of care and intermediate outcomes: United states, 1988–2002. Ann Intern Med. 2006;144(7):465–474. doi: 10.7326/0003-4819-144-7-200604040-00005. [DOI] [PubMed] [Google Scholar]
- 3.Chase HP, Pearson JA, Wightman C, Roberts MD, Oderberg AD, Garg SK. Modem transmission of glucose values reduces the costs and need for clinic visits. Diabetes Care. 2003;26(5):1475–1479. doi: 10.2337/diacare.26.5.1475. [DOI] [PubMed] [Google Scholar]
- 4.Cytryn KN, Patel VL. Reasoning about diabetes and its relationship to the use of telecommunication technology by patients and physicians. Int J Med Inform. 1998;51(2-3):137–151. doi: 10.1016/s1386-5056(98)00111-7. [DOI] [PubMed] [Google Scholar]
- 5.Heisler M, Vijan S, Anderson RM, Ubel PA, Bernstein SJ, Hofer TP. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? J Gen Intern Med. 2003;18(11):893–902. doi: 10.1046/j.1525-1497.2003.21132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krapek K, King K, Warren SS, George KG, Caputo DA, Mihelich K, Holst EM, Nichol MB, Shi SG, Livengood KB, Walden S, Lubowski TJ. Medication adherence and associated hemoglobin A1c in type 2 diabetes. Ann Pharmacother. 2004;38(9):1357–1362. doi: 10.1345/aph.1D612. [DOI] [PubMed] [Google Scholar]
- 7.O'Kane MJ, Bunting B, Copeland M, Coates VE. ESMON study group. Efficacy of self monitoring of blood glucose in patients with newly diagnosed type 2 diabetes (ESMON study): randomised controlled trial. BMJ. 2008;336(7654):1174–1177. doi: 10.1136/bmj.39534.571644.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farmer A, Gibson OJ, Tarassenko L, Neil A. A systematic review of telemedicine interventions to support blood glucose self-monitoring in diabetes. Diabet Med. 2005;22(10):1372–1378. doi: 10.1111/j.1464-5491.2005.01627.x. [DOI] [PubMed] [Google Scholar]
- 9.Mathur A, Kvedar JC, Watson AJ. Connected health: a new framework for evaluation of communication technology use in care improvement strategies for type 2 diabetes. Curr Diabetes Rev. 2007;3(4):229–234. doi: 10.2174/157339907782330003. [DOI] [PubMed] [Google Scholar]
- 10.Jaana M, Paré G. Home telemonitoring of patients with diabetes: a systematic assessment of observed effects. J Eval Clin Pract. 2007;13(2):242–253. doi: 10.1111/j.1365-2753.2006.00686.x. [DOI] [PubMed] [Google Scholar]
- 11.Brodie M, Flournoy RE, Altman DE, Blendon RJ, Benson JM, Rosenbaum MD. Health information, the Internet, and the digital divide. Health Aff (Millwood) 2000;19(6):255–265. doi: 10.1377/hlthaff.19.6.255. [DOI] [PubMed] [Google Scholar]
- 12.Wagner TH, Bundorf MK, Singer SJ, Baker LC. Free internet access, the digital divide, and health information. Med Care. 2005;43(4):415–420. doi: 10.1097/01.mlr.0000156857.14152.6e. [DOI] [PubMed] [Google Scholar]
- 13.Watson AJ, Bell AG, Kvedar JC, Grant RW. Reevaluating the digital divide: current lack of internet use is not a barrier to adoption of novel health information technology. Diabetes Care. 2008;31(3):433–435. doi: 10.2337/dc07-1667. [DOI] [PubMed] [Google Scholar]
- 14.Grant RW, Wald JS, Schnipper JL, Gandhi TK, Poon EG, Ovav EJ, Williams DH, Volk LA, Middleton B. Practice-linked online personal health record for type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2008;168(16):1776–1782. doi: 10.1001/archinte.168.16.1776. [DOI] [PMC free article] [PubMed] [Google Scholar]