Abstract
Backround
Diabetic retinopathy in Alberta and throughout Canada is common, with a prevalence up to 40% in people with diabetes. Unfortunately, due to travel distance, time, and expense, a third of patients with diabetes do not receive annual dilated eye examinations by ophthalmologists, despite universal health care access. In an effort to improve access, a teleophthalmology program was developed to overcome barriers to eye care. Prior to clinical implementation, teleophthalmology technology was clinically validated for the identification of treatable levels of diabetic retinopathy.
Method
Patients undergoing a teleophthalmology assessment underwent stereoscopic digital retinal photographs following pupillary dilation. Digital images were then packaged into an encrypted password-protected compressed file for uploading onto a secure server. Images were digitally unpackaged for review as a stereoscopic digital slide show and graded with a modified Early Treatment Diabetic Retinopathy Study algorithm. Reports were then generated automatically as a PDF file and sent back to the referring physician.
Results
Teleophthalmology programs in Alberta have assessed more than 5500 patients (9016 visits) to date. Nine hundred thirty patients have been referred for additional testing or treatment. Approximately 2% of teleophthalmology assessments have required referral for in-person examination due to ungradable image sets, most commonly due to cataract, corneal drying, or asteroid hyalosis.
Conclusions
In Alberta and throughout Canada, many patients with diabetes do not receive an annual dilated eye examination. Teleophthalmology is beneficial because patients can be assessed within their own communities. This decreases the time to treatment, allows treated patients to be followed remotely, and prevents unnecessary referrals. Health care costs may be reduced by the introduction of comprehensive teleophthalmology examinations by enabling testing and treatment to be planned prior to the patient's first visit.
Keywords: diabetic retinopathy, ETDRS, Early Treatment Diabetic Retinopathy Study, screening, teleophthalmology
Background
Alberta is a Canadian province with a population of approximately 3.45 million people spread out over 661,190 square kilometers.1 Much of the province is uninhabited; many Albertans live in rural communities, a few of which are accessible only by air, water, or seasonal ice highways. Health care is funded by the provincial government and is universal. Most rural Albertans have local access to family physicians, whereas subspecialists are largely located in urban areas, with the greatest concentration in Edmonton and Calgary.
The health of Albertans mirrors the health status of other Canadians, with diabetes being common.2 Diabetic retinopathy is therefore also common, with one Canadian study demonstrating a prevalence as high as 40%.3 Unfortunately up to a third of patients with diabetes do not receive an annual dilated eye examination by an ophthalmologist, despite universal access to health care.4 Many rural patients do not access ophthalmologic care because of difficulties related to travel distance, time, and expense.5In an effort to improve adherence to recommended screening guidelines for diabetic retinopathy and to overcome geographic barriers to eye care, the University of Alberta, Department of Ophthalmology, developed a teleophthalmology program in 1998.
Pilot Program
The goal of this pilot program was to create a teleophthalmology solution that was as sensitive and specific as Early Treatment Diabetic Retinopathy Study (ETDRS) stereoscopic slide film photography in identifying diabetic retinopathy, while also enabling the diagnosis of other ocular pathology. Visual acuity with and without pinhole was measured, while intraocular pressure was tested by Tono-Pen (Reichert Ophthalmic Instruments, Depew, NY). All patients underwent pupillary dilation with 2.5% phenylephrine and 1.0% tropicamide. Seven-field 30° digital retinal photographs were captured with a mydriatic retinal camera (Zeiss FF450, Jena, Germany) linked to a 6 megapixel digital back (DCS560, Eastman Kodak, Rochester, NY). Nonsimultaneous stereo pairs were captured of the disc and macula, while monoscopic images were captured of the remaining five fields. Additional stereoscopic photographs of the anterior chamber were included to assess for media opacity such as cataract or corneal abnormalities.
The pilot project had two outcomes: the correlation of stereoscopic digital imaging with ETDRS film photography and the feasibility of electronic transmission of retinal images via satellite between Fort Vermilion in Northern Alberta and Edmonton.5 One hundred twenty-one patients were assessed between October 1999 and June 2000. Stereoscopic digital retinal imaging, transmitted by satellite, was found to have a high level of correlation with slide film for the identification of most features of diabetic retinopathy (Pearson's correlation coefficient: 0.92 for microaneurysms, 0.80 for hemorrhages, 0.45 for intraretinal microvascular abnormalities, 0.32 for venous beading, 1.00 for neovascularization of the disc, 1.00 for neovascularization elsewhere in the retina, and 0.97 for clinically significant macular edema [CSME] [p < .001]).6
Clinical Validation
The success of the pilot was the impetus for additional research studies to validate the ability of the tele-ophthalmology system to identify treatable diabetic retinopathy. Specifically, clinical validation of the system's ability to identify discrete ETDRS levels of diabetic retinopathy7 and detection of clinically significant macular edema were undertaken.8
The first of these two validation papers compared clinical contact-lens biomicroscopic identification of CSME to high-resolution stereoscopic digital images.8 The study compared 207 eyes from 105 patients who were examined clinically and underwent same-day photography. Correlation was high, with k = 0.812 (0.732, 0.893) for CSME and k = 0.722 (0.628, 0.816) for nonclinically significant retinal thickening. This indicated that an ophthalmologist could have a high degree of confidence in the ability of teleophthalmology to identify patients in need of focal laser treatment.
The second study7 looked at the identification of discrete levels of diabetic retinopathy, with a special emphasis on detecting treatable/threshold disease. The study compared 204 eyes from 102 consecutive diabetes patients who underwent two sets of photographs: standard ETDRS stereoscopic film and high-resolution JPEG-compressed (16X) stereoscopic digital imaging (using stereo photographs of fields 1 and 2, with monoscopic capture of fields 3 through 7). In this paper the referral threshold was defined as having at least one eye with an ETDRS grade ≥61 and/or CSME. There was significant correlation between standard ETDRS stereoscopic film and University of Alberta digital teleophthalmology, with k ranging from 0.78 to 0.84 (Table 1). However, with respect to high-risk proliferative diabetic retinopathy (HRPDR), the two formats demonstrated excellent correlation (k = 0.83), but the sensitivity of digital imaging to detect HRPDR was lower (80.0%). A possible explanation for lower sensitivity was that there were only 10 eyes identified by standard slide film with HRPDR; these same 10 eyes were graded as HRPDR by digital imaging, while the other 2 eyes were graded with a lower level of (i.e., less than high-risk) proliferative diabetic retinopathy (PDR). In both cases the disagreement related to the severity of neovascularization, with digital imaging measuring a smaller area covered than did slide-film photographs. Given that the slide-film photographs could only be measured with overlays that cannot be calibrated to a specific photograph, the digital image area calculation may in fact be more accurate. With both formats referral recommendations were highly correlated, with k = 0.78. Furthermore, this study confirmed that there was also high correlation between film and digital formats when identifying CSME, with k = 0.80.
Table 1.
Comparison between ETDRS Film Photography and the University of Alberta Digital Teleophthalmology Photographic Protocol7
| Pathology | Kappa | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) |
|---|---|---|---|---|---|
| PDR (<HRPDR) | 0.84 | 93.8 | 93.2 | 79.0 | 99.5 |
| HRPDR | 0.83 | 80.0 | 99.5 | 88.9 | 99.0 |
| Refer patienta | 0.78 | 90.2 | 87.8 | 91.7 | 85.7 |
| Refer eyeb | 0.80 | 89.7 | 91.6 | 90.6 | 90.7 |
| CSME | 0.80 | 87.2 | 92.8 | 90.4 | 90.4 |
Refers to whether, for each format, at least one of the eyes was graded as having threshold disease for referral for clinical examination/treatment and was analyzed with n = 102.
Refers to whether, for each format, the eyes were graded as having threshold disease for referral for clinical examination/treatment and were analyzed with n = 204.
Secondary analysis of the population8 used to compare contact-lens biomicroscopy to digital stereoscopic retinal imaging was performed because of a debate within the teleophthalmology community as to whether stereopsis was a necessary feature of a teleophthalmology system.9 This analysis indicated that specificity improved from 81.6% to 92.9% when stereopsis was incorporated.10 Although this result did not solve the controversy, our group believes that a more specific evaluation is vital in a geographically broad country such as Canada, where travel distances may routinely be greater than a thousand kilometers for referral and treatment. The sensitivity and specificity results for the described teleophthalmology system are in keeping with American Telemedicine Association category 3 or 4 diabetic retinopathy telemedicine system.11
Teleophthalmology Program
Teleophthalmology assessments are performed in many communities throughout Alberta based on the positive results of the validation studies. No longer a pilot project, teleophthalmology has grown into a program that provides eye care to many communities across Alberta. The program is based at the University of Alberta; however, funding is provided via both the provincial and the federal government. A teleophthalmology coordinator oversees all aspects of the program, including training of new teleophthalmology technicians; patient appointments, including missed appointments, referrals, and follow-up; as well as the troubleshooting of technical difficulties.
Teleophthalmology Technician Training
All teleophthalmology technicians in Alberta undergo one week of specialized training overseen by the teleophthalmology coordinator. This training includes three days of photography instruction, one day of software training, and one day of ophthalmic skills practice. Technicians are taught to recognize diabetic retinopathy, angle closure glaucoma, cataract, as well as other common eye diseases. The training includes how to instill dilating and anesthetic drops, as well as how to perform tonometry via Tono-Pen. Once the technician is in the field, a physician is available 24 hours per day to review potential angle closure occurring as a result of pupillary dilation, while the teleophthalmology coordinator is available to troubleshoot camera, computer, or software problems. Direct feedback is provided regarding photo quality by physicians to the photographers via the teleophthalmology coordinator.
Teleophthalmology Examination Process
Remote Site
Following informed consent, a medical history is taken, while visual acuity and intraocular pressures are recorded. Mydriatic digital photographs are captured, using a variety of different mydriatic and nonmydriatic fundus cameras, including Zeiss, Canon, Nidek, and Topcon models. It is unknown whether or not there is a difference in sensitivity or specificity utilizing different camera systems; sensitivity and specificity has been assessed using a Zeiss FF450 nonmydriatic camera with an attached 6 megapixel digital back. Other systems have not been assessed in this manner, although 6 megapixel digital cameras are utilized with all systems. Based on the University of Alberta photograph protocol, stereoscopic photographs of the anterior segment, disc, and macula are captured, while an additional five fields of the periphery are captured monoscopically. These five fields are oriented according to the modified Airlie House Classification protocol when captured as 30° photographs. If a 45° photograph is obtained, the photographer attempts to center the photograph as if he or she were following the modified Airlie House protocol with 30° field. If a specific ocular pathology is identified by the photographer, additional photographs of the area of interest can be captured stereoscopically. The digital images are then sorted, packaged, named automatically (depending on camera manufacturer), or sorted by the technician with drag and drop software. Proprietary software then compresses the photographs 16 times with JPEG compression and encrypts it with password protection.
Electronic Transfer and Processing
The single encrypted, compressed file is then uploaded onto a password-protected secure server (www.teleophthalmology.com) that requires two-factor authentication (Etoken, Aladdin, Chicago, Il).
The Linux-based server is housed in a secure setting with mirrored drives both on and off site. The Web server runs Apache software (http://httpd.apache.org/), while the server-based applications run Tomcat software (http://tomcat.apache.org/). The Web server features 128-bit encryption and is compliant with the Health Information Act of Alberta that requires both password protection and two-factor authentication. The server receives all image packager uploads and validates the incoming file utilizing a Message Digest 5 checksum algorithm. The single file is then uncompressed and extracted into subfiles (images and metadata). The image files are processed with ImageJ software (http://rsbweb.nih.gov/ij/features.html), then sorted by image field and organized for Web-based stereoscopic presentation in slide show format for the physician grader to review. Metadata, stored as an XML file, is extracted and entered into an open-source database (PostgreSQL, http://www.postgresql.org/).
Physician Review
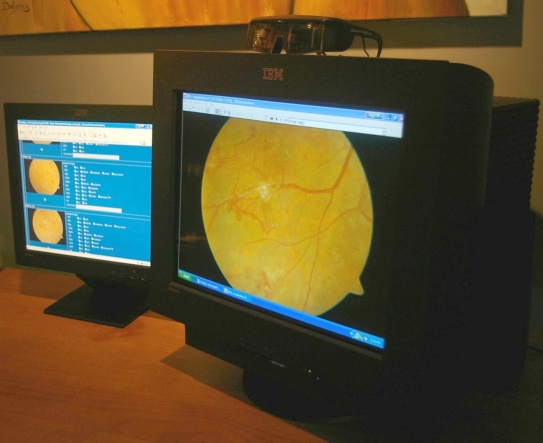
Stereo viewing is achieved by viewing images on a dual monitor workstation, where stereo images are displayed on a cathode ray tube monitor at a minimum resolution of 1024 × 768 pixels at 100 Hz refresh rate and observed through RealD (Beverly Hills, CA) liquid crystal shutter glasses that are sequenced to the display's refresh rate. The proprietary software (SDI Stereo Viewer, Secure Diagnostic Imaging, Inc., Edmonton, Canada) automatically aligns all stereo image pairs both vertically and horizontally. Grading of images is then performed with a check box University of Alberta Protocol ETDRS grading algorithm on one monitor, while stereoscopic images are viewed on the other monitor as a slide show (Figure 1). The grader is able to zoom, realign, reverse stereo, and adjust brightness as necessary to maximize visualization of diabetic retinopathy pathology. Both distance and area measurements can be performed once the image has been calibrated utilizing a standard distance (3840 µm) between the center of the fovea and the center of the optic disc. Once graded, the server automatically creates a PDF report including a photograph of the retina, ETDRS level of retinopathy grade, diabetic retinopathy level descriptor (e.g., mild, moderate, or non-PDR), treatment recommendations, visit comments, and follow-up and referral recommendations. This PDF can then be faxed or e-mailed as a password-protected Web link to the referring physician. Physician graders are able to assess and grade patient photos with efficiency. All patient images are graded by an ophthalmologist who is compensated via a fee-for-service arrangement with the provincial health care provider (Alberta Health and Wellness).
Figure 1.
Dual-monitor workstation with liquid crystal shutter glasses.
Licensing, Liability, and Remuneration
Physicians providing teleophthalmology services within Canada must have a license in the jurisdiction where the patient is assessed. In Canada, physician liability coverage is provided through the Canadian Medical Protective Association for both conventional physician–patient encounters and telemedicine. Liability coverage must therefore also be carried in the jurisdiction where the patient accesses telemedicine services. Physician remuneration is the purview of each province and, to date, is only provided in the Provinces of Alberta, Manitoba, and Ontario. In other provinces, monies for providing teleophthalmology services may be available through special grants.
Alberta Teleophthalmology
As a result of this early work, teleophthalmology has expanded from one center to many located throughout the province. To date, more than 3000 patients have been assessed, for a total of approximately 6000 patient visits (Table 2). Over 1000 patients have subsequently been referred on for additional testing or treatment. The majority of referrals have been for diseases other than diabetic retinopathy (primarily cataract and glaucoma). Approximately 2% of all teleophthalmology visits have required referral for in-person examination because of ungradable photographs. This is most commonly due to cataract, corneal drying (either preexisting or topical anesthetic related), asteroid hyalosis, or incomplete photographic sets. Unfortunately, due to the sensitive nature of research within a First Nations population, we are unable to provide specific disease-related results such as ETDRS levels (non-PDR and PDR), diabetic macular edema, and other ocular abnormalities (e.g., retinal vascular disorders, glaucoma, and age-related macular degeneration) at this time. Adaptive modeling has allowed programs to be implemented in a variety of ways, including mobile and/or fixed location retinal cameras. All programs are overseen by the teleophthalmology coordinator, who is located at the University of Alberta, and a number of ophthalmologists currently participate in reading of images. In the future it is hoped that all ophthalmologists in Alberta will participate in the provision of care via teleophthalmology.
Table 2.
Teleophthalmology Programs for the Assessment of Diabetic Retinopathy in Alberta
| Teleophthalmology program (year started) | Patients | Eye examinations | Referrals (% total referrals) [% diabetic-retinopathy-related referrals] | Incomplete or ungradable photo sets |
|---|---|---|---|---|
| Screening for Limbs, Eyes, Cardiac, and Kidneys–or SLICK (2000) | 1949 | 4135 | 601 (30.1%) [11.7%] | 124 (2.9%) |
| Aspen Health Region (2005) | 589 | 983 | 137 (23.3%) [6.4%] | 26 (2.6%) |
| Capital Health Region (2004) | 351 | 468 | 77 (23.4%) [6.5%] | 5 (1.1%) |
| Aboriginal Diabetes Wellness Program (2005) | 214 | 321 | 41 (19.1%) [7.9%] | 2 (0.6%) |
| Mobile Diabetes Screening Initiative (2003) | 270 | 466 | 74 (27.4%) [6.1%] | 14 (3.0%) |
| Pharmacy-based teleophthalmology (2006) | 138 | 154 | 34(24.6%) [4.6%] | 2 (1.3%) |
Teleophthalmology Programs for Diabetic Retinopathy
Screening for Limbs, Eyes, Cardiac, and Kidneys
The Screening for Limbs, Eyes, Cardiac, and Kidneys—or SLICK—program is the most comprehensive teleophthalmology program in Alberta.12 In operation since 2000, this program provides a comprehensive assessment of diabetes complications in First Nations individuals who live on one of the 44 reserves in the province. With respect to the diabetic retinopathy component, the program utilizes three mobile cameras and trained photographers. Cameras have been stationed within a few of the larger communities to allow year-round photography to take place. In these locations, local people have been trained as photographers.
Aspen Health Region
This hospital-based teleophthalmology program encompasses two small communities within the region: Edson and Lac La Biche. Local nurses were trained as photographers and given ophthalmic technical training, such that they can measure intraocular pressure and visual acuity. Patients are referred by their family doctor, although self-referral is also possible and encouraged.
Capital Health Region
Capital Health is the largest health region in Alberta, where 27 ophthalmologists currently practice. Although teleophthalmology services are more commonly provided in rural communities, there are many patients with diabetes who live in Edmonton who have not undergone a diabetic eye examination. In an effort to improve their care, a teleophthalmology program was instituted at the regional eye center. Photographs are captured by ophthalmic photographers following referrals from family physicians, internists, endocrinologists, or ophthalmologists who do not follow patients with diabetic retinopathy.
Aboriginal Diabetes Wellness Program
The purpose of the Aboriginal Diabetes Wellness Program is to improve the health of aboriginal peoples with diabetes. Using a holistic approach, First Nations individuals spend one week in Edmonton undergoing training in the care of diabetes, as well as medical testing. As part of this mandate, patients who have not had a dilated retinal examination in the preceding year undergo retinal photographs.
Mobile Diabetes Screening Initiative
The Mobile Diabetes Screening Initiative program is a collaboration between the University of Alberta and the Province of Alberta focusing on screening for diabetes in rural communities. Once a person is identified as having diabetes, they are offered a dilated eye examination by teleophthalmology. To date, this program has not been particularly effective, as the majority of patients screened do not have diabetes.
Pharmacy-Based Teleophthalmology
This program has been instituted as a collaborative effort within Safeway pharmacies. It enables people with diabetes to undergo a dilated eye examination with retinal photographs at their local grocery store. This not only encourages a multidisciplinary approach to the care of a diabetes patient, but also increases the possibility that patients will undergo yearly evaluation, as they will be in contact with pharmacists for their medications on a regular basis. A mobile unit travels on a rotating basis between Safeway stores within Alberta.
Comprehensive Eye Care Teleophthalmology Programs
Optometry-Based Teleophthalmology
Because many optometrists' offices are already equipped with digital retinal cameras, a program to triage referrals more efficiently was instituted in 2004. The program accepts all retinal referrals, a portion of which are for assessment and treatment of diabetic retinopathy.
As of December 31, 2008, 1039 patients have been assessed, with approximately 50% of patients referred for further testing and treatment. The program has been successful at reducing unnecessary patient travel while maximizing testing and treatment efficiency for patients who are forced to travel.13,14
Northwest Territtories Consultation Service
The University of Alberta, Department of Ophthalmology, provides consultation services to the Northwest Territories via teleophthalmology. Referrals are made by a general ophthalmologist based in Yellowknife. The service triages patients more efficiently by enabling prebooking of all necessary tests on the day of the referral visit. In most cases, patients can undergo testing, assessment, and treatment in one day. This improves efficiency while decreasing the cost of travel and accommodations, all of which are the responsibility of the territorial government. As of December 31, 2008, 364 patients have been assessed in this manner.
Discussion
In Alberta, as in other provinces across Canada, patients with diabetes face many barriers to an annual dilated eye examination. As a result, many Albertans with diabetes do not undergo an annual eye examination.4 In order to increase the percentage of patients with diabetes who undergo annual eye examinations, improved delivery paradigms must be developed. Teleophthalmology offers one solution by which patients can be assessed within their own communities in an accurate, efficient fashion, without the need for travel.
The Alberta teleophthalmology program is different from teleophthalmology programs in other countries, where screening is the primary objective.15–19 Instead the Alberta system enables physicians to provide standard of care evaluation and diagnosis via teleophthalmology. It does this by utilizing high-resolution stereoscopic digital imaging coupled with a medical history, visual acuity testing, and intraocular pressure measurement. Rural patients should not have to accept an examination that is of lesser quality than can be accessed by urban patients with diabetes.
Despite ongoing controversy regarding the necessity of stereopsis,9 we feel it is important to provide an examination as close in quality as an in-person examination by an ophthalmologist. Although there was a small reduction in sensitivity when foregoing stereopsis (81.6% versus 92.9%), the study found that a monoscopic system would refer 8.7% more patients than a stereoscopic system. Given that teleophthalmology systems are currently employed for patients at a great distance from ophthalmologists, this represents significantly increased costs for a chronic disease requiring annual evaluation.
Eye assessment by teleophthalmology, when compared to a screening examination, is beneficial for three reasons:
Unnecessary referrals are reduced or eliminated. As an example, diabetes patients with diabetic retinopathy need only be referred once they develop PDR with high-risk characteristics or CSME.
Following treatment, patients can be followed at a distance without the need for further travel. For example, having undergone focal laser treatment for CSME, a patient can be followed by teleophthalmology and only requires an in-person clinical evaluation should they need re-treatment.
A comprehensive teleophthalmology examination enables the consultant to plan for necessary testing and treatment at the time of a patient's first visit. As an example, if a patient is found to have elevated intraocular pressure and enlarged cup-to-disc ratio, a visual field and diurnal tension curve can be ordered for the day of the patient's clinical referral. The teleophthalmology visit becomes the first contact visit with the patient, while the second “office” visit enables the ophthalmologist to review the findings of diagnostic testing and make expedient management decisions.
This improvement in efficiency decreases time to treatment as well as cost to health care systems. It also decreases the number of patients traveling to a consultant's office, while increasing the ability of a consultant to treat patients effectively, efficiently, and expediently.
It is our hope that one day all people will have access to eye care within their own community, however small or remote. This hope can be realized with the development of a global teleophthalmology initiative that does not replace optometrists or ophthalmologists, but instead complements their contribution in meeting the eye care needs of all people with diabetes.
Abbreviations
- CSME
clinically significant macular edema
- ETDRS
Early Treatment Diabetic Retinopathy Study
- HRPDR
high-risk proliferative diabetic retinopathy
- PDR
proliferative diabetic retinopathy
References
- 1.Watkinson S, Seewoodhary R. Ocular complications associated with diabetes mellitus. Nurs Stand. 2008;22(27):51–57. doi: 10.7748/ns2008.03.22.27.51.c6429. quiz 8, 60. [DOI] [PubMed] [Google Scholar]
- 2.Millar WJ, Young TK. Tracking diabetes: prevalence, incidence and risk factors. Health Rep. 2003;14(3):35–47. [PubMed] [Google Scholar]
- 3.Ross SA, McKenna A, Mozejko S, Fick GH. Diabetic retinopathy in native and nonnative Canadians. Exp Diabetes Res. 2007;2007:76271. doi: 10.1155/2007/76271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tennant MT, Rudnisky CJ, Johnson JA. Diabetes and eye disease in Alberta. In: Johnson JA, editor. Alberta diabetes atlas. 1st ed. Vol. 1. Edmonton: Alberta Health and Wellness; 2007. [Google Scholar]
- 5.Tennant MT, Rudnisky CJ, Hinz BJ, MacDonald IM, Greve MD. Tele-ophthalmology via stereoscopic digital imaging: a pilot project. Diabetes Technol Ther. 2000;2(4):583–587. doi: 10.1089/15209150050502005. [DOI] [PubMed] [Google Scholar]
- 6.Tennant MT, Greve MD, Rudnisky CJ, Hillson TR, Hinz BJ. Identification of diabetic retinopathy by stereoscopic digital imaging via teleophthalmology: a comparison to slide film. Can J Ophthalmol. 2001;36(4):187–196. doi: 10.1016/s0008-4182(01)80039-9. [DOI] [PubMed] [Google Scholar]
- 7.Rudnisky CJ, Tennant MT, Weis E, Ting A, Hinz BJ, Greve MD. Web-based grading of compressed stereoscopic digital photography versus standard slide film photography for the diagnosis of diabetic retinopathy. Ophthalmology. 2007;114(9):1748–1754. doi: 10.1016/j.ophtha.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Rudnisky CJ, Hinz BJ, Tennant MT, de Leon AR, Greve MD. High-resolution stereoscopic digital fundus photography versus contact lens biomicroscopy for the detection of clinically significant macular edema. Ophthalmology. 2002;109(2):267–274. doi: 10.1016/s0161-6420(01)00933-2. [DOI] [PubMed] [Google Scholar]
- 9.Current state and future direction of tele-ophthalmology in Canada: first Canadian ophthalmic telemedicine symposium. Can J Ophthalmol. 2003;38(5):349–351. doi: 10.1016/s0008-4182(03)80044-3. [DOI] [PubMed] [Google Scholar]
- 10.Rudnisky CJ, Tennant MT, de Leon AR, Hinz BJ, Greve MD. Benefits of stereopsis when identifying clinically significant macular edema via teleophthalmology. Can J Ophthalmol. 2006;41(6):727–732. doi: 10.3129/i06-066. [DOI] [PubMed] [Google Scholar]
- 11.Cavallerano J, Lawrence MG, Zimmer-Galler I, Bauman W, Bursell S, Gardner WK, Horton M, Hildebrand L, Federman J, Carnahan L, Kuzmak P, Peters JM, Darkins A, Ahmed J, Aiello LM, Aiello LP, Buck G, Cheng YL, Cunningham D, Goodall E, Hope N, Huang E, Hubbard L, Janczewski M, Lewis JW, Matsuzaki H, McVeigh FL, Motzno J, Parker-Taillon D, Read R, Soliz P, Szirth B, Vigersky RA, Ward T American Telemedicine Association, Ocular Telehealth Special Interest Group, National Institute of Standards and Technology Working Group. Telehealth practice recommendations for diabetic retinopathy. Telemed J E Health. 2004;10(4):469–482. doi: 10.1089/tmj.2004.10.469. [DOI] [PubMed] [Google Scholar]
- 12.Virani S, Strong D, Tennant M, Greve M, Young H, Shade S, Kanji M, Toth E Implementation Committee of the Aboriginal Diabetes Initiative. Rationale and implementation of the SLICK project: Screening for Limb, I-Eye, Cardiovascular and Kidney (SLICK) complications in individuals with type 2 diabetes in Alberta's First Nations communities. Can J Public Health. 2006;97(3):241–247. doi: 10.1007/BF03405595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanson C, Tennant MT, Rudnisky CJ. Optometric referrals to retina specialists: evaluation and triage via teleophthalmology. Telemed J E Health. 2008;14(5):441–445. doi: 10.1089/tmj.2007.0068. [DOI] [PubMed] [Google Scholar]
- 14.Swindale NV. Feedback decoding of spatially structured population activity in cortical maps. Neural Comput. 2008;20(1):176–204. doi: 10.1162/neco.2008.20.1.176. [DOI] [PubMed] [Google Scholar]
- 15.Boucher MC, Nguyen QT, Angioi K. Mass community screening for diabetic retinopathy using a nonmydriatic camera with telemedicine. Can J Ophthalmol. 2005;40(6):734–742. doi: 10.1016/S0008-4182(05)80091-2. [DOI] [PubMed] [Google Scholar]
- 16.Al Sabti K, Raizada S, Wani VB, Al Ajmi M, Gayed I, Sugathan TN. Efficacy and reliability of fundus digital camera as a screening tool for diabetic retinopathy in Kuwait. J Diabetes Complications. 2003;17(4):229–233. doi: 10.1016/s1056-8727(03)00007-2. [DOI] [PubMed] [Google Scholar]
- 17.Mash B, Powell D, du Plessis F, van Vuuren U, MIchalowska M, Levitt N. Screening for diabetic retinopathy in primary care with a mobile fundal camera: evaluation of a South African pilot project. S Afr Med J. 2007;97(12):1284–1288. [PubMed] [Google Scholar]
- 18.Massin P, Aubert JP, Eschwege E, Erginay A, Bourovitch JC, BenMehidi A, Nougarède M, Bouée S, Fagnani F, Tcherny MS, Jamet M, Bouhassira M, Marre M. Evaluation of a screening program for diabetic retinopathy in a primary care setting Dodia (Dépistage ophtalmologique du diabète) study. Diabetes Metab. 2005;31(2):153–162. doi: 10.1016/s1262-3636(07)70181-7. [DOI] [PubMed] [Google Scholar]
- 19.Leese GP, Morris AD, Olson J. A national retinal screening programme for diabetes in Scotland. Diabet Med. 2003;20(12):962–964. doi: 10.1111/j.1464-5491.2003.01078.x. [DOI] [PubMed] [Google Scholar]