Abstract
In the 21st century, eighty years after William Baer presented his groundbreaking work treating bone and soft tissue infections with live maggots, thousands of therapists around the globe have rediscovered the benefits of maggot therapy. The renaissance in maggot therapy is due in large part to recent technological advancements that have solved or minimized many of the treatment's earlier drawbacks: the need for reliable access to this perishable medical device, simplified application, and low-cost production. Modern dressing materials have simplified the procedure and minimized the risk of escaping maggots. The establishment of dozens of laboratories throughout the world, along with access to overnight courier services in many regions, has made medicinal maggots readily available to millions of people in need. Studies show that fears of patient nonacceptance are unfounded. The medical literature is rapidly growing with scientific evidence demonstrating the efficacy and safety of maggot therapy for a variety of problematic wounds. This article examines how these and other technologies are optimizing the study and application of maggot therapy for wound care.
Keywords: diabetes, larva, maggot, therapy, ulcer, wound
Introduction
While technological advances have led to significant improvements in medical care, including wound care, nonhealing wounds still remain a significant problem. The annual cost of management for these wounds exceeds $20 billion,1,2 not including the loss of two million workdays.3 Worse yet, the prevalence of nonhealing wounds is on the rise.4
Diabetic foot ulcers alone are so common (affecting approximately 15% of the diabetes patient population) that they account for over 1.5 million foot ulcers and at least 70,000 amputations annually.5,6
The rising prevalence of nonhealing wounds is due, in part, to the medical advances that have increased our life expectancy and have converted fatal diseases into chronic diseases. More people are living with conditions that increase their susceptibility to wounds and/or impair their wound healing. Additionally our antibiotic arsenal is no longer as effective at controlling skin and soft tissue infections because of the growing number and prevalence of antibiotic-resistant microbes.
Desperate to advance wound care, many clinicians and researchers are looking back into medical history and reexamining earlier technologies with the advanced tools and wisdom of the 21st century. One of these reexamined technologies is maggot therapy [also known as maggot debridement therapy (MDT), biodebridement, or simply larval therapy]. Maggot debridement therapy is the intentional application of live, “medical-grade” fly larvae to wounds in order to effect debridement, disinfection, and ultimately wound healing.
Controlled studies demonstrate the efficacy and safety of maggot therapy. Advances in medicine, materials manufacturing, and transportation now make maggot therapy readily available and relatively simple to use. As a consequence, many therapists now consider MDT as a practical solution for many nonhealing wounds. In this article I examine the basis for the current maggot therapy renaissance.
History of Maggot Therapy
Early Observations
For centuries, the beneficial effects of maggot-infested wounds were noted by military surgeons who observed that injured soldiers abandoned on the battlefield fared better and that their wounds healed faster when those wounds were infested with maggots.7 Himself having observed maggot-infested wounds during his service in World War I, the orthopedic surgeon, William Baer, was the first to apply maggots systematically to nonhealing wounds while a professor at Johns Hopkins and Children's Hospital in Baltimore, Maryland. Baer presented his preliminary results in 1929,8 and his entire work in maggot therapy—treating over 100 children with osteomyelitis and problematic soft tissue wounds—was published posthumously in 1931.9
Rise and Fall of Maggot Therapy in the 1930s
Within 5 years of Baer's groundbreaking work, over 1000 American, Canadian, and European surgeons were using maggots in their practice.10 Many hospitals operated their own insectaries for rearing and disinfecting the larvae. Those that did not have their own supply could order Surgical MaggotsTM from Lederle Laboratories (Pearl River, NY).
Over 90% of doctors using maggot therapy at that time were very pleased with it,10 although some complained about the difficulty in obtaining maggots, their expense, or the effort required to construct a sturdy maggot dressing. Then, in the 1940s, maggot therapy seemed to disappear from the scene, presumably because of the widespread availability of antibiotics and possibly also improved surgical techniques. Clearly the types of wounds that had previously been the focus of maggot therapy—osteomyelitis and soft tissue abscesses resulting from bacteremias—were suddenly much less common as a result of early treatment of infections with sulfonamides and penicillin. By 1950 maggot therapy was rarely used and, with few exceptions,11,12 almost never reported.
Maggot Therapy Today
By the end of the 1980s, antimicrobial resistance was increasingly common, pressure ulcers and diabetic foot ulcers were on the rise, and conventional wound care was noticeably inadequate for an increasing number of recalcitrant wounds. This was the backdrop for a series of research questions: How would maggot therapy compare to modern wound care treatments? Why was MDT now used only as a “last resort”?12 Should MDT be used earlier in the course of treatment, especially if it compared favorably to conventional therapy? The first controlled clinical studies of maggot therapy would address these questions. But before those studies could be carried out, and before widespread use of maggot therapy was imaginable, several technical challenges first had to be overcome.
Technological Advancements That Have Optimized Maggot Therapy
The three most common objections to maggot therapy during the 1930s were the hassle of making dressings, the difficulty in obtaining viable, germ-free maggots, and their high cost ($5 in 1933). The development of improved adhesives and synthetic fabrics now provide us with many more convenient methods for constructing cage-like dressings to hold the maggots within the wound bed.13–16 Improved disinfectants and rearing techniques have simplified the production of germ-free maggots.17 Overnight courier services have made it relatively simple to deliver the highly perishable maggots to most areas within 24 h.
The cost of medicinal maggots in America presently remains at what it was 80 years ago, adjusted for inflation ($80–100). Since the cost of most other medical and surgical treatments has escalated considerably, medicinal maggots are now relatively inexpensive by comparison. The major production costs are labor and quality control (more labor).
Medicinal Maggots, Version 2009, and How They Work
Maggot therapy is essentially a controlled therapeutic myiasis (maggot infestation on a live host). It is controlled by selecting a safe and effective species and strain, by chemical disinfection to make the maggots germ-free, by containing the maggots within special dressings that prevent them from leaving the wound unescorted, and through quality control measures throughout the breeding and production processes. Not all species are safe and effective. The maggots cleared for marketing in the United States belong to the (currently named) LB-01 strain of Phaenicia (Lucilia) sericata.
Maggots are applied to the wound at a dose of 5–10 larvae per square centimeter of wound surface area and are left within their dressing for 48–72 h. At that point they are satiated, finished working, and can be removed. Clinical and laboratory studies have identified four major actions of medicinal maggots on wounds:
Maggot Therapy for the Treatment for Diabetic Foot Ulcers
During the first half of the 20th century, prospective controlled studies were not the customary method of medical inquiry. In 1990 controlled clinical studies of maggot therapy began in earnest. Markevich and colleagues randomized 140 patients with nonhealing diabetic neuropathic foot wounds to receive either conventional treatment with debridement and hydrogel or maggot therapy and then followed subjects for 10 days.27 By day 10 nearly twice as many maggot-treated wounds were debrided and covered with healthy granulation tissue (51.1% of MDT patients versus 27% of controls, p < .05). Complete healing was seen in 7.1% of MDT patients and 2.8% of controls, but because this 10-day study was not designed to compare wound healing, it is no surprise that this difference did not achieve statistical significance.
In a controlled cohort study of 18 diabetes patients with 20 nonhealing neuropathic foot and leg wounds treated either with maggot therapy or standard medical and surgical therapy (control), maggot therapy was found to be more effective and efficient in debriding nonhealing foot and leg ulcers in male diabetes veterans than conventional medical and surgical care.31 Maggot debridement was faster and more thorough than control therapy when measured at 2 weeks (p = .02) and again at the end of the study period (p = .001). Maggot therapy was also associated with hastened growth of granulation tissue (p = .016) and wound epithelialization at just 4 weeks (p = .018).
In a case-controlled study of nonambulatory patients with mixed neuropathic ischemic foot wounds, Armstrong and associates50 demonstrated that the maggot-treated patients required fewer days of antibiotics and healed their wounds an average of 4 weeks faster than control patients, although the associated healing rate (57% in the MDT group versus 33% in the control group) was not statistically significant.
Other investigators have also reported maggot therapy to be safe and effective for diabetic foot ulcers, especially neuropathic ulcers.24,25 Although not randomized, prospective, nor controlled, these reports still offer additional safety and efficacy data in support of using MDT for wounds previously recalcitrant to conventional medical and surgical therapies.
Consistently, studies have also demonstrated the efficacy of MDT for limb salvage when used as a “last resort.” Pre-amputation maggot therapy is reported to save 40–50% of limbs, usually with complete wound healing.24,28,30,32,50,79 The reasons for these consistently high limb salvage rates are unclear but may be related to the increased oxygen perfusion,72 rapid and luscious spread of granulation tissue,23,29,31 cellular proliferation,74 fibroblast migration, and matrix remodeling77 that have been documented with maggot therapy and maggot secretions.
Most practitioners now recognize that, as with all other wound treatments, the potential for healing is greatest when maggot therapy is not withheld until infection or vascular compromise has progressed to limb-threatening levels. In the words of Jones and Thomas,80 “[Finally] maggots are being applied earlier in the disease process and are now often the first choice of treatment with some specialist practitioners.”
Maggot Therapy for Other Problematic Wounds
Controlled clinical studies have also demonstrated maggot therapy to be safe and effective in diabetes and nondiabetes subjects for many other problematic wounds, including pressure ulcers,23,29 venous stasis leg ulcers,26,51 wound bed preparation prior to surgical closure,32 and a variety of other traumatic, infectious, and vascular wounds.33
Warnings and Contraindications
Adverse events associated with MDT—both real and theoretical—have been reviewed in detail elsewhere.81 Those most likely to occur are discomfort, delivery problems, and escaping maggots.
Maggot-debridement-therapy-associated pain or discomfort is reported in 5–30% of wounds treated.28,29,31 In all cases these patients also reported wound pain before receiving maggot therapy. Thus patients likely to experience discomfort can be readily identified, warned, and treated appropriately with analgesics. Pain generally occurs after the first 24 h, as the maggots increase in size. Pain is usually well controlled with analgesics, but if not, removal of the dressing and release of the maggots will halt the discomfort immediately.
Since medicinal maggots are highly perishable, they are susceptible to transportation problems and delays. Young, starving larvae require food, water, and oxygen, and they are temperature sensitive. Therefore they must be shipped by overnight courier, and their arrival should be timed no more than 24 h before their application to the wound. Delivery delays and exposure to extreme temperatures decrease their survival. In postmarketing studies in the United States,82 1% of medicinal maggots arrived late or dead.
Occasionally the maggot dressings may come loose, especially if left in place for more than 48 h. Fugitives not rounded up will pupate and emerge from their hiding places 1–2 weeks later as adult flies. Although these flies are not yet mature enough to lay eggs, they can be a nuisance. Moreover, “used maggots” and flies are essentially mobile fomites. Therefore dressings must confine the maggots securely, and all the maggots must be collected at the end of the treatment cycle and disposed of as other infectious dressing waste. Sample policies and procedures for applying and removing maggot dressings are available from the BioTherapeutics, Education and Research (BTER) Foundation (www.BTERfoundation.org).
Patient anxiety (the “yuck factor”) is not as common as is often claimed. In studies of patients with chronic wounds, most were quite accepting of maggot therapy.29,32,83,84 A recent survey85 discovered that health care professionals and administrators are much more likely to be disgusted by the thought of maggot dressings than are patients with chronic wounds.
Maggot Therapy in Today's Regulatory Environment
In the United States, medicinal maggots are regulated by the Food and Drug Administration (FDA) as a prescription-only, single-use medical device. In some other countries, they are regulated as a drug. At least 24 laboratories currently supply medical-grade maggots to therapists and patients in more than 30 countries.
Maggot Therapy Cost and Reimbursement
While most people simply accept maggot therapy as being cost-effective, only one study actually quantified it. Wayman and coworkers26 prospectively measured the personnel and material costs of treating venous stasis ulcers with either maggot therapy or hydrogel (conventional control therapy). The cost of maggot therapy was just over half that of conventional therapy. With maggot therapy the researchers' money also bought them better outcomes: all wounds treated by MDT were completely debrided after just one 3-day cycle, but only 80% of the control wounds were debrided within 4 weeks of control debridement. Using this and other data, Thomas86 calculated conservatively that the use of maggot therapy for just 30% of nonhealing diabetic ulcers in need of debridement could save the United Kingdom approximately £50 million annually.
In the United States, the cost of MDT is generally covered by third-party payers, but this can be inconsistent. Wound care therapists and in-patient facilities reimbursed according to medical diagnosis or need (rather than by procedure) often consider maggot therapy as a fiscally prudent treatment choice, because it is inexpensive, fast, effective, simple, and safe enough to be performed by nursing or paramedical staff. Patient Assistance Grants are available from the BTER Foundation (www.BTERfoundation.org) to help patients in the United States without insurance coverage.
The Future of Maggot Therapy
The Technology of Tomorrow's Maggot Therapy
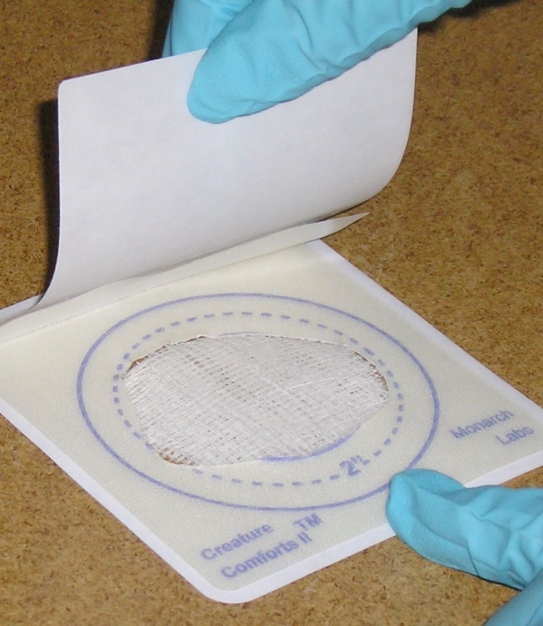
Technological advances in material design have allowed manufacturers to create single-piece, hinged, cage-like dressings that confine the maggots to the wound (Figure 1). Called “maggot confinement dressings,” these products provide the maggots with free and complete access to the wound while preventing them from escaping. These dressings are much simpler and less time-consuming to apply than the current method13,14 by which therapists construct individualized cage dressings out of materials not specifically developed for maggot therapy (Figure 2).
Figure 1.
Le Flap™ (Monarch Labs, LLC, Irvine, CA), a single-piece, dual-layered, hinged maggot confinement dressing, keeps the maggots in place but provides complete access to the wound bed below. After cutting a wound-size hole in the hydrocolloid layer and placing maggots onto the wound, the adherent top netting is gently folded over the hydrocolloid frame. Photo furnished by Monarch Labs, LLC (Irvine, CA).
Figure 2.
Medicinal maggots being applied to a diabetic foot wound. Maggots are held in place by a nylon stocking, which is here being glued to a strip of hydrocolloid, just proximal to the plantar wound. Excess stocking is trimmed, and a frame of tape is placed to further secure the cage-like dressing. Photo furnished by BTER Foundation.
“Maggot containment dressings” were also designed to prevent maggots from escaping. But unlike confinement dressings, these pouch-like dressings (Figure 3) completely contain and surround the larvae, even restricting their free access to the wound bed.15,16,87,88 This appears to decrease the risk of patient discomfort, because the maggots cannot crawl over exposed nerves, and this decreases therapist discomfort, because the care providers can apply and remove the dressings without ever having to see or handle the larvae directly.
Figure 3.
One example of the maggot containment dressing is the Biobag™ (BioMonde Laboratories, Barsbüttel, Germany). The polyester net pouch completely surrounds and contains the maggots. Available in various sizes. Photo furnished by BTER Foundation.
Since William Baer's time, many researchers have attempted to isolate the wound-healing molecules that underlie the proteolytic, antimicrobial, and growth-promoting activity of maggot therapy. Some propose that such compounds could someday replace the maggot itself. On the issue of maggot debridement dressings without the maggots, Baer had this to say: “Whether we can get the active principle, whether this is an enzyme, whether we can get out that enzyme and treat without maggots, I do not know; but I do know that [maggot therapy] is the most successful and easiest way of curing chronic osteomyelitis that I have yet had.”8
Livingston and others believed that maggot-induced wound healing was a result of more than just a few extractable chemicals.21 The secreted mixture of digestive molecules is complex and synergistic. The physical movement of the spined maggots themselves also contributes to debridement, rasping the necrotic tissue and helping the enzymes gain access to the deeper tissue. Appreciating this fact the FDA regulates medicinal maggots as a medical device rather than as a simple drug. Will synthesized molecules extracted from medicinal maggots someday replace MDT for debriding, disinfecting, and healing wounds? Perhaps. But if the purified molecules alone prove less effective than live maggots, surely someone will develop robotic maggots (not to be confused with “bot” flies) to deliver those molecules.
Conclusions
Medicinal maggots are as precise in their debridement as a highly skilled microsurgeon, as attentive to their hosts' wounds as the most dedicated wound-care nurse. It is no wonder that they have found their way into the hearts and wounds of so many.
Despite our low cultural esteem for maggots, more and more clinicians and patients are turning to medicinal maggots for assistance with their wound healing. For most, the drawbacks of maggot therapy pale in comparison to the remarkable efficacy in treating even the most recalcitrant wounds.
By combining the wisdom of the past with the technology of the present, we have solved many of maggot therapy's drawbacks. Now we are bringing medicinal maggots back into our hospitals and clinics to help us solve some of our patients' most troublesome wounds. Modern dressing materials have simplified the maggot therapy procedure and minimized the risk of escape. The establishment of laboratories throughout the world, along with access to overnight courier service in many regions, has made medicinal maggots readily available to millions of people.
Researchers continue to extend our understanding about wound healing as they explore the mechanisms by which maggots help to heal wounds. It is uncertain whether or not maggot-derived products may someday replace live larvae for wound care. But for now, this author and his patients are glad to use what nature has already provided and humans have neatly harnessed: medicinal maggots—new and improved for the 21st century.
Acknowledgments
Dr. Sherman acknowledges his wife, Julie, and his daughters, Rebecca and Hannah Leigh Sherman, who, over the past 12 years, graciously allowed so much family time and material support to be redirected to the cause of maggot therapy. Without their sacrifices, Dr. Sherman would have had to abandon this work and get a real job many years ago.
Abbreviations
- BTER
BioTherapeutics, Education and Research Foundation
- FDA
Food and Drug Administration
- MDT
maggot debridement therapy
References
- 1.Frykberg RG, Armstrong DG, Giurini J, Edwards A, Kravette M, Kravitz S, Ross C, Stavosky J, Stuck R, Vanore J. American College of Foot and Ankle Surgeons. Diabetic foot disorders: a clinical practice guideline. J Foot Ankle Surg. 2000;39(5 Suppl):S1–S60. [Updated in J Foot Ankle Surg. 2006;45(5 Suppl):S1–66.] [PubMed] [Google Scholar]
- 2.Harding KG, Morris HL, Patel GK. Science, medicine and the future: healing chronic wounds. BMJ. 2002;324(7330):160–163. doi: 10.1136/bmj.324.7330.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McGuckin M, Kerstein MD. Venous leg ulcers and the family physician. Adv Wound Care. 1998;11(7):344–346. [PubMed] [Google Scholar]
- 4.Petrie NC, Yao F, Eriksson E. Gene therapy in wound healing. Surg Clin North Am. 2003;83(3):597–616. doi: 10.1016/S0039-6109(02)00194-9. [DOI] [PubMed] [Google Scholar]
- 5.Frykberg RG, Habershaw GM, Chrzan JS. Epidemiology of the diabetic foot: ulcerations and amputations. Contemporary endocrinology: clinical management of diabetic neuropathy. In: Veves A, editor. Totowa: Humana Press; 1998. p. 273. [Google Scholar]
- 6.Centers for Disease Control and Prevention. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. National diabetes fact sheet, 2007. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf. Accessed February 22, 2009. [Google Scholar]
- 7.Pechter EA, Sherman RA. Maggot therapy: the surgical metamorphosis. Plast Reconstr Surg. 1983;72(4):567–570. doi: 10.1097/00006534-198310000-00032. [DOI] [PubMed] [Google Scholar]
- 8.Baer WS. Sacro-iliac joint—arthritis deformans—viable antiseptic in chronic osteomyelitis. Proc Int Assembly Interstate Postgrad Med Assoc North Am; 1929. pp. 365–372. [Google Scholar]
- 9.Baer WS. The treatment of chronic osteomyelitis with the maggot (larva of the blow fly) J Bone Joint Surg. 1931;13:438–475. doi: 10.1007/s11999-010-1416-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robinson W. Progress of maggot therapy in the United States and Canada in the treatment of suppurative diseases. Am J Surg. 1935;29:67–71. [Google Scholar]
- 11.Horn KL, Cobb AH, Jr, Gates GA. Maggot therapy for subacute mastoiditis. Arch Otolaryngol. 1976;102(6):377–379. doi: 10.1001/archotol.1976.00780110089013. [DOI] [PubMed] [Google Scholar]
- 12.Teich S, Myers RA. Maggot therapy for severe skin infections. South Med J. 1986;79(9):1153–1155. doi: 10.1097/00007611-198609000-00029. [DOI] [PubMed] [Google Scholar]
- 13.Sherman RA. A new dressing design for use with maggot therapy. Plast Reconstr Surg. 1997;100(2):451–456. doi: 10.1097/00006534-199708000-00029. [DOI] [PubMed] [Google Scholar]
- 14.Sherman RA, Tran JM, Sullivan R. Maggot therapy for treating venous stasis ulcers. Arch Dermatol. 1996;132(3):254–256. [PubMed] [Google Scholar]
- 15.Fleischmann W, Thoener B. Biobag: a live wound-dressing containing maggots. Presented at: Fifth International Conference on Biotherapy; Wurzburg, Germany. 2000. [Google Scholar]
- 16.Grassberger M, Fleischmann W. The biobag: a new device for the application of medicinal maggots. Dermatology. 2002;204(4):306. doi: 10.1159/000063369. [DOI] [PubMed] [Google Scholar]
- 17.Sherman RA, Wyle FA. Low-cost, low-maintenance rearing of maggots in hospitals, clinics, and schools. Am J Trop Med Hyg. 1996;54(1):38–41. doi: 10.4269/ajtmh.1996.54.38. [DOI] [PubMed] [Google Scholar]
- 18.Livingston SK, Prince LH. The treatment of chronic osteomyelitis with special reference to the use of the maggot active principle. J Am Med Assoc. 1932;98:1143–1149. [Google Scholar]
- 19.Wilson EH, Doan CA, Miller DF. The Baer maggot treatment of osteomyelitis. Preliminary report of twenty-six cases. JAMA. 1932;98:1149–1152. [Google Scholar]
- 20.Robinson W, Norwood VH. The role of surgical maggots in the disinfection of osteomyelitis and other infected wounds. J Bone Joint Surg. 1933;15:409–412. [Google Scholar]
- 21.Livingston SK. The therapeutic active principle of maggots with a description of its clinical application in 567 cases. J Bone Joint Surg. 1936;18:751–756. [Google Scholar]
- 22.Sherman RA, Wyle F, Vulpe M, Wishnow R, Iturrino J, Watson M, Martin G. Maggot therapy for treating pressure sores in spinal cord patients. J Am Paraplegia Soc. 1991;14(4):200. [Google Scholar]
- 23.Sherman RA, Wyle FA, Vulpe M. Maggot therapy for treating pressure ulcers in spinal cord injury patients. J Spinal Cord Med. 1995;18(2):71–74. doi: 10.1080/10790268.1995.11719382. [DOI] [PubMed] [Google Scholar]
- 24.Mumcuoglu KY, Ingber A, Gilead L, Stessman J, Friedmann R, Schulman H, Bichucher H, Ioffe-Uspensky I, Miller J, Galun R, Raz I. Maggot therapy for the treatment of diabetic foot ulcers. Diabetes Care. 1998;21(11):2030–2031. doi: 10.2337/diacare.21.11.2030. [DOI] [PubMed] [Google Scholar]
- 25.Fleischmann W, Russ M, Moch D, Marquardt C. Biosurgery: maggots, are they really the better surgeons? Chirurg. 1999;70(11):1340–1346. doi: 10.1007/s001040050790. [DOI] [PubMed] [Google Scholar]
- 26.Wayman J, Nirojogi V, Walker A, Sowinski A, Walker MA. The cost effectiveness of larval therapy in venous ulcers. J Tissue Viability. 2000;10(3):91–94. doi: 10.1016/s0965-206x(00)80036-4. [DOI] [PubMed] [Google Scholar]
- 27.Markevich YO, McLeod-Roberts J, Mousley M, Melloy E. Maggot therapy for diabetic neuropathic foot wounds: a randomized study. Presented at: 36th Annual Meeting of the European Association for the Study of Diabetes; Jerusalem, Israel. 2000. Sep, [Google Scholar]
- 28.Sherman RA, Sherman J, Gilead L, Lipo M, Mumcuoglu KY. Maggot débridement therapy in outpatients. Arch Phys Med Rehabil. 2001;82(9):1226–1229. doi: 10.1053/apmr.2001.24300. [DOI] [PubMed] [Google Scholar]
- 29.Sherman RA. Maggot versus conservative debridement therapy for the treatment of pressure ulcers. Wound Repair Regen. 2002;10(4):208–214. doi: 10.1046/j.1524-475x.2002.10403.x. [DOI] [PubMed] [Google Scholar]
- 30.Jukema GN, Menon AG, Bernards AT, Steenvoorde P, Rastegar AT, van Dissel JT. Amputation-sparing treatment by nature: “surgical” maggots revisited. Clin Infect Dis. 2002;35(12):1566–1571. doi: 10.1086/344904. [DOI] [PubMed] [Google Scholar]
- 31.Sherman RA. Maggot therapy for treating diabetic foot ulcers unresponsive to conventional therapy. Diabetes Care. 2003;26(2):446–451. doi: 10.2337/diacare.26.2.446. [DOI] [PubMed] [Google Scholar]
- 32.Sherman RA, Shimoda KJ. Presurgical maggot debridement of soft tissue wounds is associated with decreased rates of postoperative infection. Clin Infect Dis. 2004;39(7):1067–1070. doi: 10.1086/423806. [DOI] [PubMed] [Google Scholar]
- 33.Sherman RA, Shapiro CE, Yang RM. Maggot therapy for problematic wounds: uncommon and off-label applications. Adv Skin Wound Care. 2007;20(11):602–610. doi: 10.1097/01.ASW.0000284943.70825.a8. [DOI] [PubMed] [Google Scholar]
- 34.Hobson RP. On an enzyme from blow-fly larvae (Lucilia sericata) which digests collagen in alkaline solution. Biochem J. 1931;25(5):1458–1463. doi: 10.1042/bj0251458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hobson RP. Studies on the nutrition of blow fly larvae. III: the liquefaction of muscle. J Exp Biol. 1932;9(4):359–365. [Google Scholar]
- 36.Fletcher F, Haub JG. Digestion in blowfly larvae, Phormia regina Meigen, used in the treatment of osteomyelitis. Ohio J Science. 1933;33(2):101–109. [Google Scholar]
- 37.Slocum MA, McClellan RH, Messer FC. Investigation into the modes of action of blow fly maggots in the treatment of chronic osteomyelitis. Penn Med J. 1933;36:570–573. [Google Scholar]
- 38.Maseritz IH. Digestion of bone by larvae of Phormia regina. Arch Surg. 1934;28(3):589–607. [Google Scholar]
- 39.Gwatkin R, Fallis AM. Bactericidal and antigenic qualities of the washings of blowfly maggots. Can J Res. 1938;16:343–352. [Google Scholar]
- 40.Ziffren SE, Heist HE, May SC, Womack NA. The secretion of collagenase by maggots and its implication. Ann Surg. 1953;138(6):932–934. doi: 10.1097/00000658-195312000-00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Waterhouse DF, Irzykiewicz H. An examination of proteolytic enzymes from several insects for collagenase activity. J Ins. Physiol. 1957;1:18–22. [Google Scholar]
- 42.Fraser A, Ring RA, Stewart RK. Intestinal proteinases in an insect. Calliphora vomitoria L. Nature. 1961;192:999–1000. doi: 10.1038/192999a0. [DOI] [PubMed] [Google Scholar]
- 43.Brookes VJ. Partial purification of a proteolytic enzyme from an insect, Phormia regina. Biochim Biophys Acta. 1961;46:13–21. [Google Scholar]
- 44.Vistnes LM, Lee R, Ksander GA. Proteolytic activity of blowfly larvae secretions in experimental burns. Surgery. 1981;90(5):835–841. [PubMed] [Google Scholar]
- 45.Pendola S, Greenberg B. Substrate-specific analysis of proteolytic enzymes in the larval midgut of Calliphora vicina. Ann Entomol Soc Am. 1975;68:341–345. [Google Scholar]
- 46.Casu RE, Pearson RD, Jarmey JM, Cadogan LC, Riding GA, Tellam RL. Excretory/secretory chymotrypsin from Lucilia cuprina: purification, enzymatic specificity and amino acid sequence deduced from mRNA. Insect Mol Biol. 1994;3(4):201–211. doi: 10.1111/j.1365-2583.1994.tb00168.x. [DOI] [PubMed] [Google Scholar]
- 47.Muharsini S, Dalrymple B, Vuocolo T, Hamilton S, Willadsen P, Wijffels G. Biochemical and molecular characterization of serine proteases from larvae of Chrysomya bezziana, the Old World Screwworm fly. Insect Biochem Mol Biol. 2001;31(11):1029–1040. doi: 10.1016/s0965-1748(01)00051-0. [DOI] [PubMed] [Google Scholar]
- 48.Chambers L, Woodrow S, Brown AP, Harris PD, Phillips D, Hall M, Church JC, Pritchard DI. Degradation of extracellular matrix components by defined proteinases from the greenbottle larva Lucilia sericata used for the clinical debridement of non-healing wounds. Br J Dermatol. 2003;148(1):14–23. doi: 10.1046/j.1365-2133.2003.04935.x. [DOI] [PubMed] [Google Scholar]
- 49.Steenvoorde P, Jukema GN. The antimicrobial activity of maggots: in vivo results. J Tissue Viability. 2004;14(3):97–101. doi: 10.1016/s0965-206x(04)43005-8. [DOI] [PubMed] [Google Scholar]
- 50.Armstrong DG, Salas P, Short B, Martin BR, Kimbriel HR, Nixon BP, Boulton AJ. Maggot therapy in “lower-extremity hospice” wound care: fewer amputations and more antibiotic-free days. J Am Podiatr Med Assoc. 2005;95(3):254–257. doi: 10.7547/0950254. [DOI] [PubMed] [Google Scholar]
- 51.Contreras-Ruiz J, Arroyo-Escalante S, Fuentes-Suarez , Adominguez-Cherit J, Sosa-de-Martinez C, Maravilla-Franco E. Maggot therapy and infection control in venous ulcers: a comparative study. Presented at: Symposium on Advanced Wound Care (SAWC); April 21–24; San Diego, CA. 2005. [Google Scholar]
- 52.Tantawi TI, Gohar YM, Kotb MM, Beshara FM, El-Naggar MM. Clinical and microbiological efficacy of MDT in the treatment of diabetic foot ulcers. J Wound Care. 2007;16(9):379–383. doi: 10.12968/jowc.2007.16.9.27868. [DOI] [PubMed] [Google Scholar]
- 53.Bowling FL, Salgami EV, Boulton AJ. Larval therapy: a novel treatment in eliminating methicillin-resistant Staphylococcus aureus from diabetic foot ulcers. Diabetes Care. 2007;30(2):370–371. doi: 10.2337/dc06-2348. [DOI] [PubMed] [Google Scholar]
- 54.Robinson W, Norwood VH. Destruction of pyogenic bacteria in the alimentary tract of surgical maggots implanted in infected wounds. J Lab Clin Med. 1934;19:581–586. [Google Scholar]
- 55.Stewart MA. The role of Lucilia sericata Meig. larvae in osteomyelitis wounds. Ann Trop Med Parasitol. 1934;28:445–460. doi: 10.1126/science.79.2055.459-a. [DOI] [PubMed] [Google Scholar]
- 56.Simmons SW. The bactericidal properties of excretions of the maggot of Lucilia sericata. Bull Entomol Res. 1935;26:559–563. [Google Scholar]
- 57.Messer FC, McClellan RH. Surgical maggots. A study of their functions in wound healing. J Lab Clin Med. 1935;20:1219–1226. [Google Scholar]
- 58.Pavillard ER, Wright EA. An antibiotic from maggots. Nature. 1957;180(4592):916–917. doi: 10.1038/180916b0. [DOI] [PubMed] [Google Scholar]
- 59.Greenberg B. Model for the destruction of bacteria in the midgut of blow fly maggots. J Med Entomol. 1968;5(1):31–38. doi: 10.1093/jmedent/5.1.31. [DOI] [PubMed] [Google Scholar]
- 60.Erdmann GR, Khalil SK. Isolation and identification of two antibacterial agents produced by a strain of Proteus mirabilis isolated from larvae of the screwworm (Cochliomyia hominivorax) (Diptera: Calliphoridae) J Med Entomol. 1986;23(2):208–211. doi: 10.1093/jmedent/23.2.208. [DOI] [PubMed] [Google Scholar]
- 61.Keppi E, Zachary D, Robertson M, Hoffmann D, Hoffmann JA. Induced antibacterial proteins in the haemolymph of Phormia terranovae (Diptera): purification and possible origin of one protein. Insect Biochem. 1986;16(2):395–402. [Google Scholar]
- 62.Friedman E, Shaharabany M, Ravin S, Golomb E, Gollop N. Partially purified antibacterial agent from maggots displays a wide range of antibacterial activity. Presented at: 3rd International Conference on Biotherapy; Jerusalem, Israel. 1998. [Google Scholar]
- 63.Thomas S, Andrews AM, Hay NP, Bourgoise S. The anti-microbial activity of maggot secretions: results of a preliminary study. J Tissue Viability. 1999;9(4):127–132. doi: 10.1016/s0965-206x(99)80032-1. [DOI] [PubMed] [Google Scholar]
- 64.Mumcuoglu KY, Miller J, Mumcuoglu M, Friger M, Tarshis M. Destruction of bacteria in the digestive tract of the maggot of Lucilia sericata (Diptera: Calliphoridae) J Med Entomol. 2001;38(2):161–166. doi: 10.1603/0022-2585-38.2.161. [DOI] [PubMed] [Google Scholar]
- 65.Lerch K, Linde HJ, Lehn N, Grifka J. Bacteria ingestion by blowfly larvae: an in vitro study. Dermatology. 2003;207(4):362–366. doi: 10.1159/000074115. [DOI] [PubMed] [Google Scholar]
- 66.Bexfield A, Nigam Y, Thomas S, Ratcliffe NA. Detection and partial characterisation of two antibacterial factors from the excretions/secretions of the medicinal maggot Lucilia sericata and their activity against methicillin-resistant Staphylococcus aureus (MRSA) Microbes Infect. 2004;6(14):1297–1304. doi: 10.1016/j.micinf.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 67.Huberman L, Gollop N, Mumcuoglu KY, Block C, Galun R. Antibacterial properties of whole body extracts and haemolymph of Lucilia sericata maggots. J Wound Care. 2007;16(3):123–127. doi: 10.12968/jowc.2007.16.3.27011. [DOI] [PubMed] [Google Scholar]
- 68.Huberman L, Gollop N, Mumcuoglu KY, Breuer E, Bhusare SR, Shai Y, Galun R. Antibacterial substances of low molecular weight isolated from the blowfly, Lucilia sericata. Med Vet Entomol. 2007;21(2):127–131. doi: 10.1111/j.1365-2915.2007.00668.x. [DOI] [PubMed] [Google Scholar]
- 69.Daeschlein G, Mumcuoglu KY, Assadian O, Hoffmeister B, Kramer A. In vitro antibacterial activity of Lucilia sericata maggot secretions. Skin Pharmacol Physiol. 2007;20(2):112–115. doi: 10.1159/000097983. [DOI] [PubMed] [Google Scholar]
- 70.Bexfield A, Bond AE, Roberts EC, Dudley E, Nigam Y, Thomas S, Newton RP, Ratcliffe NA. The antibacterial activity against MRSA strains and other bacteria of a <500 Da fraction from maggot excretions/secretions of Lucilia sericata (Diptera: Calliphoridae) Microbes Infect. 2008;10(4):325–333. doi: 10.1016/j.micinf.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 71.Nigam Y, Bexfield A, Thomas S, Ratcliffe NA. Maggot therapy: the science and implication for CAM. Part II: maggots combat infection. Evid Based Complement Alternat Med. 2006;3(3):303–308. doi: 10.1093/ecam/nel022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wollina U, Liebold K, Schmidt WD, Hartmann M, Fassler D. Biosurgery supports granulation and debridement in chronic wounds: clinical data and remittance spectroscopy measurement. Int J Dermatol. 2002;41(10):635–639. doi: 10.1046/j.1365-4362.2002.01354.x. [DOI] [PubMed] [Google Scholar]
- 73.Robinson W. Stimulation of healing in non-healing wounds by allantoin occurring in maggot secretions and of wide biological distribution. J Bone Joint Surg. 1935;17:267–271. [Google Scholar]
- 74.Prete P. Growth effects of Phaenicia sericata larval extracts on fibroblasts: mechanism for wound healing by maggot therapy. Life Sci. 1997;60(8):505–510. doi: 10.1016/s0024-3205(96)00688-1. [DOI] [PubMed] [Google Scholar]
- 75.Horobin AJ, Shakesheff KM, Woodrow S, Robinson C, Pritchard DI. Maggots and wound healing: an investigation of the effects of secretions from Lucilia sericata larvae upon interactions between human dermal fibroblasts and extracellular matrix components. Br J Dermatol. 2003;148(5):923–933. doi: 10.1046/j.1365-2133.2003.05314.x. [DOI] [PubMed] [Google Scholar]
- 76.Horobin AJ, Shakesheff KM, Pritchard DI. Maggots and wound healing: an investigation of the effects of secretions from Lucilia sericata larvae upon the migration of human dermal fibroblasts over a fibronectin-coated surface. Wound Repair Regen. 2005;13(4):422–433. doi: 10.1111/j.1067-1927.2005.130410.x. [DOI] [PubMed] [Google Scholar]
- 77.Horobin AJ, Shakesheff KM, Pritchard DI. Promotion of human dermal fibroblast migration, matrix remodelling and modification of fibroblast morphology within a novel 3D model by Lucilia sericata larval secretions. J Invest Dermatol. 2006;126(6):1410–1418. doi: 10.1038/sj.jid.5700256. [DOI] [PubMed] [Google Scholar]
- 78.Van der Plas MJ, Jukema GN, Wai SW, Dogterom-Ballering HC, Lagendijk EL, van Gulpen C, van Dissel JT, Bloemberg GV, Nibbering PH. Maggot excretions/secretions are differentially effective against biofilms of Staphylococcus aureus and Pseudomonas aeruginosa. J Antimicrob Chemother. 2008;61(1):117–122. doi: 10.1093/jac/dkm407. [DOI] [PubMed] [Google Scholar]
- 79.Sherman RA, Hall MJ, Thomas S. Medicinal maggots: an ancient remedy for some contemporary afflictions. Annu Rev Entomol. 2000;45:55–81. doi: 10.1146/annurev.ento.45.1.55. [DOI] [PubMed] [Google Scholar]
- 80.Jones M, Thomas S. Larval therapy. Nurs Stand. 2000;14(20):47–51. doi: 10.7748/ns2000.02.14.20.47.c2757. [DOI] [PubMed] [Google Scholar]
- 81.Sherman RA. Maggot therapy for foot and leg wounds. Int J Low Extrem Wounds. 2002;1(2):135–142. doi: 10.1177/1534734602001002009. [DOI] [PubMed] [Google Scholar]
- 82.Nguyen H, Sherman RA. Adverse events associated with maggot therapy: phase 4 post-marketing study. Presented at: Clinical Symposium on Advances in Skin and Wound Care; September 28–October 1; Orlando, FL. 2006. [Google Scholar]
- 83.Thomas S, Jones M, Wynn K, Fowler T. The current status of maggot therapy in wound healing. Br J Nurs. 2001;10(22 Suppl):S5–S8. doi: 10.12968/bjon.2001.10.Sup5.12322. S10, S12. [DOI] [PubMed] [Google Scholar]
- 84.Steenvoorde P, Buddingh TJ, van Engeland A, Oskam J. Maggot therapy and the “yuk” factor: an issue for the patient? Wound Repair Regen. 2005;13(3):350–352. doi: 10.1111/j.1067-1927.2005.130319.x. [DOI] [PubMed] [Google Scholar]
- 85.Sherman RA, Nguyen H, Sullivan R, Mendez S, Carmean M. Why not maggots? Factors affecting therapists' decisions about using maggot debridement therapy. Presented at: 20th Annual Symposium on Advanced Wound Care and Wound Healing Society Meeting; April 28–May 1; Tampa, FL. 2007. [Google Scholar]
- 86.Thomas S. Cost of managing chronic wounds in the U.K., with particular emphasis on maggot debridement therapy. J Wound Care. 2006;15(10):465–469. doi: 10.12968/jowc.2006.15.10.26973. [DOI] [PubMed] [Google Scholar]
- 87.Lodge A, Jones M, Thomas S. Maggots 'n' chips: a novel approach to the treatment of diabetic ulcers. Br J Community Nurs. 2006;11(12) suppl:23–26. doi: 10.12968/bjcn.2006.11.Sup6.22431. [DOI] [PubMed] [Google Scholar]
- 88.Steenvoorde P, Jacobi CE, Oskam J. Maggot debridement therapy: free-range or contained? An in vivo study. Adv Skin Wound Care. 2005;18(8):430–435. doi: 10.1097/00129334-200510000-00010. [DOI] [PubMed] [Google Scholar]