Abstract
Purpose
To demonstrate the clinical utility of OCT (optical coherence tomography) in diagnosing macular structural abnormalities in patients with asteroid hyalosis.
Methods
Case series.
Results
Seven eyes from seven patients underwent OCT testing due to inadequate funduscopic visualization secondary to asteroid hyalosis. Fluorescein angiography and B-scan ultrasonography was conducted in two patients - but failed to provide diagnostic clarity. OCT provided definitive anatomic diagnoses that included macular epiretinal membrane, macular hole, traction retinal detachment, cystoid macular edema, and drusen. Based on OCT-assisted diagnoses, three patients elected to undergo surgical intervention.
Conclusion
OCT can be critical to diagnose macular conditions when retinal visualization is limited by asteroid hyalosis.
Keywords: asteroid hyalosis, optical coherence tomography
Introduction
Asteroid hyalosis is a degenerative process resulting in small, white vitreous opacities consisting of calcium phosphate and complex, layered lipid deposits1-4. Previous studies suggest a prevalence of 0.83-1.96%, bilaterality of 10%, and association with male sex and age1-4. The correlation between asteroid hyalosis and diabetes mellitus remains controversial1,3,4. Asteroid bodies rarely impair visual acuity, but they can impede funduscopic visualization because of scattered reflection of incident light off the opacities1-4. Their presence can pose difficulty for ophthalmologists requiring unobstructed retinal visualization for diagnostic purposes.
Previous studies demonstrate that fluorescein angiography (FA) can reduce asteroid distortion and improve funduscopic visualization2,3,5. FA employs barrier filters which can screen out reflected asteroid blue light scatter. However, FA suffers from a few limitations2. First, FA has limited ability to detect subtle anatomic macular abnormalities. Second, image quality is often poor for cases with relatively large aggregates of asteroid and posterior vitreous opacities. Third, quality image capture requires a higher level of technical skill as the camera must be focused on the retina, which may only be partially visible prior to FA injection.
Optical coherence tomography (OCT) offers an alternative imaging modality that creates a cross-sectional image of the retina utilizing incident light (830 nm) to detect relative changes in reflection at the optical interface6. The diagnostic utility of OCT is not well-documented for eyes with asteroid hyalosis. One report describes a case of macular edema in which OCT assisted the diagnosis7. We report here a series of cases in which OCT was useful, even essential, to diagnose macular conditions in which visualization of the retina was limited by asteroid hyalosis.
Patients and Methods
Patients with asteroid hyalosis were identified retrospectively from an OCT database from March 1998 to May 2005 at Columbia University's Harkness Eye Institute. Seven eyes of seven patients were identified, and the medical and surgical records were reviewed. The study followed the tenets of the Declaration of Helsinki and received approval by the Institutional Review Board of Columbia University.
Case Reports
Case 1
A 63-year-old diabetic male was referred for consultation due to a six month history of declining vision in his right eye. The patient had a prior history of uncomplicated cataract extraction OD and proliferative diabetic retinopathy for which he had received panretinal laser photocoagulation OU.
On initial examination, best-corrected Snellen visual acuity was 20/150 OD and 20/80 OS. Anterior segment examination revealed a well-placed posterior segment intraocular lens implant OD and 2+ nuclear sclerosis OS. There was no evidence of rubeosis iridis, and the intraocular pressures measured 15 mmHg OU. A detailed funduscopic examination was limited by prominent asteroid hyalosis OU (Figure 1A). Clinical examination suggested that the peripheral retinas were attached with moderate panretinal ablation noted, and there was no evidence of neovascularization or vitreous hemorrhage. In the macular region of the right eye, fibrotic proliferation was identified inferotemporally with the suggestion of a blunting of the retinal reflex. The central macular region itself was not well-visualized.
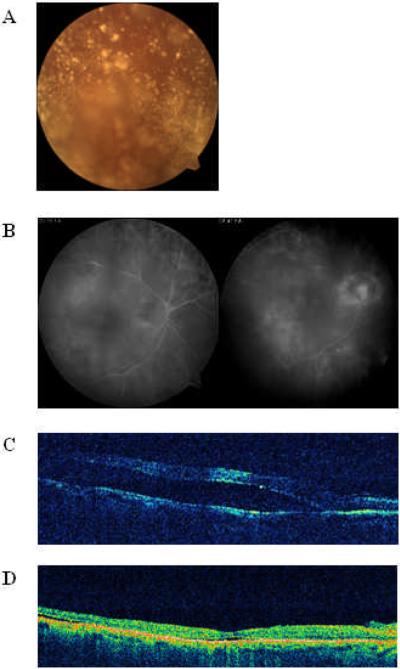
Figure 1.
Imaging Studies for Case 1. (A) Color photography demonstrates asteroid hyalosis light scatter (B) Angiographic evaluation displays a region of ill-defined inferotemporal hyperfluorescence (C) Preoperative OCT demonstrates displays a low-lying fovea-involving neurosensory detachment in the temporal macula (D) Postoperative OCT displays successful retinal detachment repair
Diagnostic testing of the right eye was performed to better evaluate the macula region. Fluorescein angiography of the posterior pole and macula was limited by the asteroid media opacities but revealed a region of ill-defined inferotemporal hyperfluorescence (Figure 1B). B-scan ultrasound (I3SYSTEM-ABD, Innovative Imaging Inc, Sacramento, CA, 10 MHz probe) demonstrated vitreous opacities, a fully attached peripheral retina, and no evidence of macular disease. Optical coherence tomography using the Stratus OCT (Carl Zeiss Meditec, Dublin, California, USA), however, revealed a low-lying fovea-involving retinal detachment in the temporal macula (Figure 1C).
The patient subsequently underwent vitrectomy to repair the retinal detachment. Intraoperatively, the low-lying traction retinal detachment involving the macula was confirmed after removal of the vitreous and asteroid particles. Segmentation and delamination of the proliferative tissue was performed, with placement of gas tamponade at the end of the procedure. The postoperative course was unremarkable, and best corrected Snellen visual acuity improved to 20/80 one month after surgery. OCT testing demonstrated successful retinal detachment repair (Figure 1D).
Case 2
A 60 year-old South-Asian female was referred for consultation due to one month of progressive loss of vision in her right eye. She had no prior ocular history.
On initial examination, Snellen visual acuity was 20/80 OD and 20/20 OS. Anterior segment examination revealed 2+ nuclear sclerosis with normal intraocular pressures OU. Funduscopic evaluation was remarkable for asteroid hyalosis in the right eye which precluded a detailed evaluation of the peripheral retina and macula. A partial separation of the posterior hyaloid was noted at the optic disc. Fundus examination of the left eye was unremarkable. OCT testing (Humphrey model 2000; Humphrey Instruments, San Leandro, California) revealed a stage III macular hole OD with separation of the hyaloid over the macular region (Figure 2A).
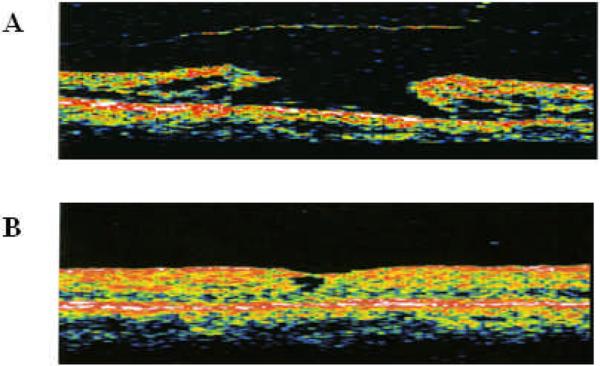
Figure 2.
Imaging Studies for Case 2. (A) Preoperative OCT demonstrates a stage III macular hole (B) Postoperative OCT reveals macular hole closure
The patient elected to undergo vitrectomy to repair the macular hole. The procedure was uncomplicated and with successful hole closure (Figure 2B). Postoperative visual acuity improved to 20/30.
Case 3
A 68 year-old Caucasian female was seen for a two year history of gradually decreasing visual acuity in her left eye following uncomplicated cataract extraction. Her ocular history was otherwise unremarkable.
The initial examination revealed best-corrected Snellen visual acuity of 20/30 OD and 20/70 OS. Anterior segment examination was significant for a well-placed posterior segment intraocular lens implant OU and intraocular pressures of 15 mmHg OD and 10 mmHg OS. Funduscopic examination was unremarkable in the right eye, but revealed severe asteroid hyalosis in the left eye that limited visualization (Figure 3A).
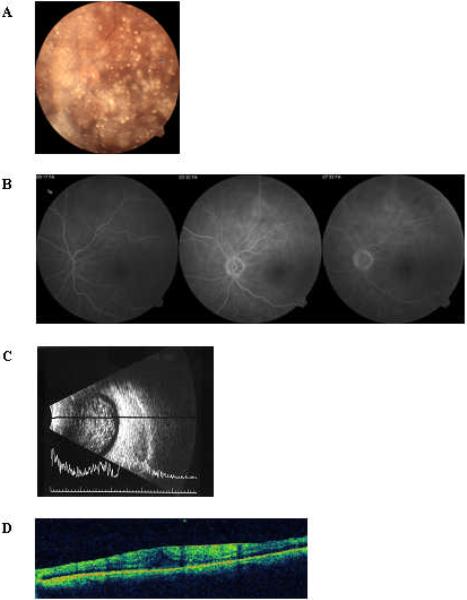
Figure 3.
Imaging Studies for Case 3. (A) Color photograph demonstrates asteroid hyalosis (B) Fluorescein angiography is unremarkable (C) B-scan ultrasound is consistent with vitreous asteroid bodies and a posterior vitreous separation (D) OCT reveals marked elevation of the macular reflex and macular pucker
Imaging studies were preformed for further characterization of the macula region. Fluorescein angiography was unremarkable and did not yield additional diagnostic information (Figure 3B). B-scan ultrasound revealed reflective signals consistent with vitreous asteroids and a posterior vitreous separation (Figure 3C). OCT testing with the Stratus system demonstrated a marked elevation of the macular reflex and an epiretinal membrane OS (Figure 3D).
The patient was counseled on the potential benefits and risks of macular pucker surgery but ultimately elected not to pursue surgical intervention.
Case 4
A 67 year-old Caucasian female referred for progressive decline in vision over the past two years. She had no prior ocular history.
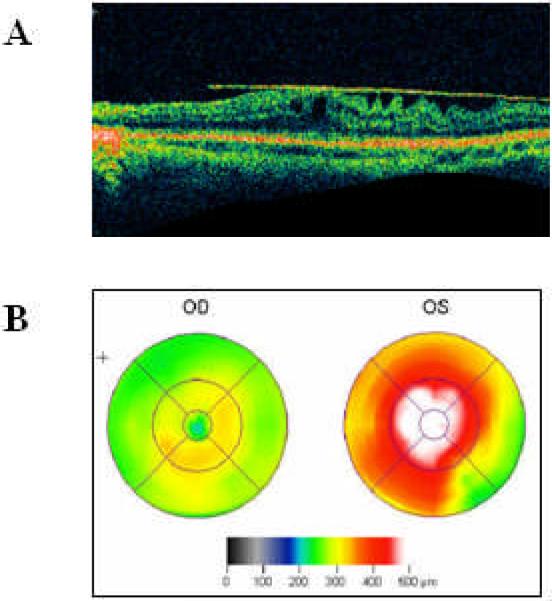
On initial examination, best-corrected Snellen visual acuity was 20/50 OU. Anterior segment examination revealed a 1+ nuclear sclerosis OD and clear lens OS. There was no evidence of rubeosis irides, and intraocular pressures measured 10 mmHg OU. Funduscopic examination was limited by moderate asteroid hyalosis OU (Figure 4A). Clinical examination revealed a slight amount of pigment proliferation in the foveal area of the right eye and loss of the foveal reflex in the left eye. Stratus OCT testing revealed a macular pucker and intraretinal edema in the left eye (Figure 4B). OCT of the fellow eye demonstrated asteroid body shadowing without macular edema (Figure 4C).
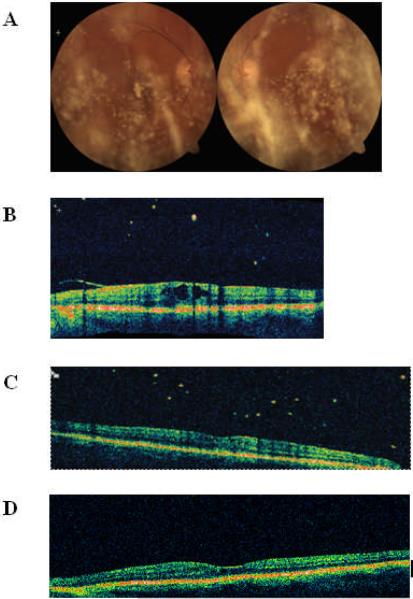
Figure 4.
Imaging Studies for Case 4. (A) Color photograph displays asteroid aggregates that limited retinal visualization OU (B) Preoperative OCT demonstrating macular pucker and intraretinal edema with asteroid body shadowing OS (C) OCT of fellow eye demonstrates asteroid body shadowing without macular edema. (D) Postoperative OCT displays the resolution of macular edema and pucker and the removal of vitreous asteroids
The patient underwent vitrectomy and membrane peeling. The postoperative course was uncomplicated, and the patient's visual acuity improved to 20/40 OS within two months. OCT testing demonstrated resolution of macular edema and pucker and improvement in the macular architecture (Figure 4D).
Results
Seven eyes from seven patients with asteroid hyalosis underwent OCT testing due to inadequate funduscopic visualization (Table 1). Ages ranged from 60-77, with 3 males and 4 females. Three of these patients were diabetic. Fluorescein angiography and B-scan ultrasonography was conducted in two patients, but these additional studies failed to provide a conclusive diagnosis. OCT diagnoses included macular epiretinal membrane, macular hole, traction retinal detachment, cystoid macular edema, and drusen. Based on OCT-assisted diagnoses, three patients elected to undergo surgical intervention. In these cases, preoperative Snellen best corrected visual acuity (BCVA) ranged from 20/50 to 20/150. Each patient experienced improvement of vision postoperatively, with BCVA ranging from 20/30 to 20/80 (mean follow-up 17 months).
Table 1.
Patient Characteristics, OCT-assisted Diagnoses, and Surgical Data
| Findings | Case Number | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
| Age (years) | 63 | 60 | 68 | 67 | 65 | 77 | 71 |
| Sex | Male | Female | Female | Female | Female | Male | Male |
| Eye | Right | Right | Left | Left | Left | Right | Right |
| Diabetes | Yes | No | Yes | No | No | No | Yes |
| Fluorescein Angiography | Yes | No | Yes | No | No | No | No |
| B-scan Ultrasonography | Yes | No | Yes | No | No | No | No |
| OCT-Assisted Diagnosis | Traction Retinal Detachment | Macular Hole | Macular Pucker | Macular Pucker / Macular Edema | Macular Pucker | Drusen | Macular Pucker |
| Pre-Operative Snellen BCVA | 20 / 150 | 20 / 100 | 20 / 70 | 20 / 50 | 20 / 60 | 20 / 80 | 20 / 100 |
| Surgical Intervention | Yes | Yes | No | Yes | No | No | Yes |
| Post-Operative Snellen BCVA | 20 / 80 | 20 / 30 | N/A | 20 / 40 | N/A | N/A | 20 / 60 |
| Post-Operative Follow-up (months) | 7 | 40 | N/A | 5 | N/A | N/A | 15 |
OCT = optical coherence tomography; BCVA = Snellen best corrected visual acuity
Discussion
This retrospective study demonstrates the utility of OCT for diagnosing macular structural abnormalities in the setting of asteroid hyalosis. Traditional methods of funduscopic visualization can be limited in these eyes, and alternative imaging modalities such as fluorescein angiography and ultrasonography may not provide adequate diagnostic capabilities to yield accurate diagnoses. In all seven cases of this study, OCT testing identified the specific retinal anatomic abnormality, allowing for definitive diagnosis. In each of these cases, fluorescein angiography and/or funduscopic evaluation assisted the diagnosis, but appropriate disease management was ultimately guided by OCT evaluation.
OCT employs an 830nm wavelength light beam that is less susceptible to distortion from asteroid bodies and other media opacities. With dense asteroids, however, the light beam can be absorbed or reflected. This degradation may occur with both the incident and reflected light beams, leading to areas of lower signal strength and shadowing of certain areas on the retina. OCT technicians can minimize these image artifacts by properly positioning the patient for the clearest OCT scan, adjusting the focus knob to the most highly saturated diopter, using the polarization function, and ensuring proper corneal lubrication. OCT in the setting of media opacity of the vitreous cavity is not always fruitful. In eyes with varying degrees of vitreous hemorrhage, the 830 nm wavelength light beam of OCT is absorbed by blood, making imaging often imprecise or impossible. Absorption of the incident light by asteroid bodies is less consequential.
Another imaging technique, the retinal thickness analyzer (Talia Technologies, Ltd., Neve Ilan, Israel), a diagnostic modality that evaluates macula/retinal thickness using 16 parallel optical cross-sections, was not as useful as OCT in a recent series of patients with moderate-to high media opacities6. This study suggested that the 830nm wavelength utilized by OCT was less likely to be absorbed by corneal and lens opacity and vitreous haze. Unlike the retinal thickness analyzer, OCT does not require a 0.2-radian angle between the incident and reflected light beams, thus allowing data capture through a smaller clear space.
OCT is currently employed to diagnose a wide array of macular architectural abnormalities including macular holes, vitreomacular traction, choroidal neovascularization, macular edema, epiretinal membrane, etc8. OCT appears to be beneficial in evaluating the macula of eyes with asteroid hyalosis when fluorescein angiography and clinical funduscopic evaluation are of limited diagnostic utility.
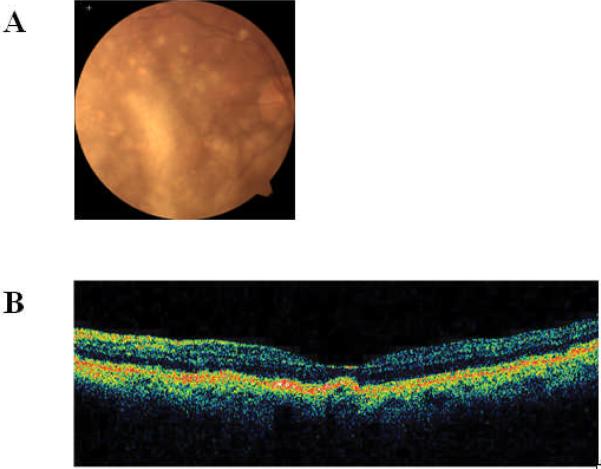
Figure 5.
Imaging Studies for Case 5. (A) OCT displays macular pucker OS (B) Retinal thickness/volume analysis demonstrates OS foveal thickness of 512 microns with a total macular volume of 10.5 mm3. OD foveal thickness measured 216 microns with a total macular volume of 7.9 mm3.
Figure 6.
Imaging Studies for Case 6. (A) Color photograph displays dense asteroid bodies that obstruct retinal visualization (B) OCT demonstrates drusen bodies
Acknowledgments
Supported by unrestricted funds from Research to Prevent Blindness.
Footnotes
The authors have no commercial, proprietary, or financial interest in any of the products or companies described in this article.
References
- 1.Fawzi AA, Vo B, Kriwanek R, Ramkumar HL, et al. Asteroid hyalosis in an autopsy population: The University of California at Los Angeles (UCLA) experience. Arch Ophthalmol. 2005;123:486–90. doi: 10.1001/archopht.123.4.486. [DOI] [PubMed] [Google Scholar]
- 2.Hampton GR, Nelsen PT, Hay PB. Viewing through the asteroids. Ophthalmology. 1981;88:669–72. doi: 10.1016/s0161-6420(81)34969-0. [DOI] [PubMed] [Google Scholar]
- 3.Feist RM, Morris RE, Witherspoon CD, et al. Vitrectomy in asteroid hyalosis. Retina. 1990;10:173–7. [PubMed] [Google Scholar]
- 4.Ikeda T, Sawa H, Koizumi K, et al. Vitrectomy for proliferative diabetic retinopathy with asteroid hyalosis. Retina. 1998;18:410–4. doi: 10.1097/00006982-199805000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Parnes RE, Zakov ZN, Novak MA, Rice TA. Vitrectomy in patients with decreased visual acuity secondary to asteroid hyalosis. Am J Ophthalmol. 1998;125:703–4. doi: 10.1016/s0002-9394(98)00031-2. [DOI] [PubMed] [Google Scholar]
- 6.Polito A, Shah SM, Haller JA, et al. Comparison between retinal thickness analyzer and optical coherence tomography for assessment of foveal thickness in eyes with macular disease. Am J Ophthalmol. 2002;134:240–51. doi: 10.1016/s0002-9394(02)01528-3. [DOI] [PubMed] [Google Scholar]
- 7.Browning DJ, Fraser CM. Optical coherence tomography to detect macular edema in the presence of asteroid hyalosis. Am J Ophthalmol. 2004;137:959–61. doi: 10.1016/j.ajo.2003.11.049. [DOI] [PubMed] [Google Scholar]
- 8.Jaffe GJ, Caprioli J. Optical coherence tomography to detect and manage retinal disease and glaucoma. Am J Ophthalmol. 2004;137:156–69. doi: 10.1016/s0002-9394(03)00792-x. [DOI] [PubMed] [Google Scholar]