Abstract
Background
Depression and anxiety are highly co-morbid disorders. Two latent trait models have been proposed to explain the nature of the relationship between these disorders. The first posits that depressive and anxiety disorders are both manifestations of a single internalizing factor. The second model, based on a tripartite model proposed by Clark & Watson [Journal of Abnormal Psychology (1991) 100, 316–336], proposes that depressive and anxiety disorders reflect a combination of shared and disorder-specific factors.
Method
We directly compared the two models in a sample of 891 individuals from the Oregon Adolescent Depression Project who participated in up to four diagnostic assessments over approximately 15 years. Structural equation models were used to examine the relationship between depressive and anxiety disorders across different developmental periods (<14, 14–18, 19–23, 24–30 years of age).
Results
The one- and three-factor models were hierarchically related. Thus, a direct comparison between the one- and three-factor models was possible using a χ2 difference test. The result found that the three-factor model fit the data better than the one-factor model.
Conclusions
The three-factor model, positing that depressive and anxiety disorders were caused by a combination of shared and disorder-specific factors, provided a significantly better fit to the data than the one-factor model postulating that a single factor influences the development of both depressive and anxiety disorders.
Keywords: Anxiety, co-morbidity, depression, internalizing psychopathology, structural equation modeling
Introduction
High rates of co-morbidity between depressive disorders and anxiety disorders have been documented in clinical and community samples of adults and children (for reviews, see Brady & Kendall, 1992; Mineka et al. 1998). Investigators commonly reported that over half of patients with depressive disorders also have an anxiety disorder, and over half of patients with anxiety disorders also have a depressive disorder (Clark, 1989; Mineka et al. 1998; Brown et al. 2001). This high level of co-morbidity raises important questions about the boundaries between depressive and anxiety disorders (Krueger, 1999; Watson, 2005; Watson et al. 2006), and has important implications for prognosis and treatment (Brown et al. 1996; Barlow et al. 2004; Belzer & Schneier, 2004).
The nature of the relationship between depressive and anxiety disorders is not well understood. Several models posit that common, or shared, etiological processes account for the observed co-morbidity between anxiety and depressive disorders. The first model proposes that depressive and anxiety disorders are manifestations of the same underlying processes. For example, Andrews’ (1996) concept of ‘the general neurotic syndrome’ and Tyrer’s (2001) concept of ‘cothymia’ hypothesize that anxiety and depressive disorders are variants of a single condition. Krueger and colleagues have reported a series of studies using latent structure techniques in large community samples that have revealed that depressive and anxiety disorders load on a single ‘internalizing’ factor (Krueger et al. 1998; Krueger, 1999; Krueger & Finger, 2001). Similar results have also been reported in several large community-based samples of children (Lahey et al. 2004) and adults (Vollebergh et al. 2001; Kendler et al. 2003; Kessler et al. 2005a; Slade & Watson, 2006).1,†
A second latent factor model that attempts to explain the co-morbidity between depressive and anxiety disorders was proposed by Clark & Watson (1991). Their tripartite model posits that shared and unique factors are involved in depressive and anxiety disorders: both groups of disorders are characterized by high negative affectivity; depressive disorders are characterized by low positive affectivity; and anxiety disorders are characterized by high physiological arousal. More recently, Mineka et al. (1998) suggested that each of the anxiety disorders is characterized by a unique factor that differentiates the various anxiety disorders from one another. A number of studies in clinical and community samples of adults and children (e.g. Clark et al. 1994; Watson et al. 1995; Joiner et al. 1996; Brown et al. 1998; Chorpita & Daleiden, 2002) have reported that depressed and anxious participants exhibit the predicted differences in positive affectivity and physiological arousal, but are similar with respect to negative affectivity.
The literature on latent variable models of the association between depressive and anxiety disorders has several limitations. First, previous studies have generally focused on only one model of co-morbidity, and no studies have directly compared the one- and three-factor models in the same sample. Second, most studies of latent factor models have used cross-sectional designs, and therefore have not examined whether these models can account for the relationship between depressive and anxiety disorders over time. Third, these studies have not considered the relationship between depressive and anxiety disorders across different developmental periods. There are several plausible ways in which latent trait models could differ as a function of development. For example, anxiety and depression may become increasingly differentiated during childhood and early adolescence. Thus, a common factor may have greater influence earlier in development. Alternatively, there is evidence that anxiety may be a risk factor for later depression (Costello et al. 2003; Merikangas et al. 2003). Hence, an anxiety-specific factor may be more prominent earlier in development, and a common factor may become stronger over time. Finally, many of these studies have analyzed lifetime diagnoses in samples that were heterogeneous with respect to age. As Kraemer et al. (2006) demonstrated recently, the use of lifetime diagnoses in mixed-age samples can bias the assessment of co-morbidity and create pseudo-co-morbidity.
Fergusson et al. (2006) recently addressed several of these limitations. They examined the structure of internalizing psychopathology in a large community sample that was assessed on three occasions between the ages of 18 and 25. Using dimensional symptom scores, they found that a general internalizing factor and several disorder-specific factors accounted for the relationships between and within major depressive disorder, generalized anxiety disorder, phobias and panic disorder.
In the present paper, we extend the previous literature by directly comparing the one- and three-factor models of internalizing disorders in a large community sample of adolescents who received up to four semi-structured diagnostic assessments over approximately 15 years. Unlike most previous studies, we used diagnoses rather than symptom scores, and because of the intensity and duration of the follow-up, we were able to examine the association between the period-incidence2 of anxiety and depressive disorders across four developmentally meaningful periods: childhood (age ≤13); adolescence (ages 14–18); emerging adulthood (ages 19–23); and young adulthood (ages 24–30). We focused on period-incidence rather than period-prevalence to examine the development of new episodes of depressive and anxiety disorders. Period-prevalence rates cannot distinguish the onset of new episodes from the persistence of prior episodes that may have emerged in earlier developmental periods.
Method
Participants
We used data from the Oregon Adolescent Depression Project (OADP; Lewinsohn et al. 1993), a longitudinal study of a large cohort of high school students who were assessed twice during adolescence, a third time when the average age was 24, and a fourth time when the average age was 30. A total of 1709 adolescents (ages 14–18; mean age 16.6, S.D. = 1.2) completed the initial (T1) assessment. The participation rate at T1 was 61%. Approximately 1 year later, 1507 of the adolescents (88%) returned for a second evaluation (T2). Differences between the sample and the larger population from which it was selected, and between participants and those who declined to participate or dropped out of the study before T2, were small (Lewinsohn et al. 1993).
For the third assessment, all adolescents with a history of psychopathology by T2 (n = 644) and a random sample of adolescents with no history of psychopathology by T2 (n = 457) were invited to participate in a third (T3) evaluation. All non-white T2 participants were retained in the T3 sample to maximize ethnic diversity. Of the 1101 T2 participants selected for a T3 interview, 941 (85%) completed the age 24 evaluation. Of subjects selected for the T3 there were few differences between those who did and did not participate (Lewinsohn et al. 2003). At age 30, all T3 participants were asked to complete another interview assessment. Of the 941 who participated in the T3 assessment, 816 (87%) completed the T4 assessment. Of subjects who completed the T3 assessment, those who also completed the T4 evaluation were more likely to be female [χ2 (1) = 4.17, p = 0.04] and slightly younger at T1 [F(1, 890) = 4.58, p < 0.05], but did not differ on ethnicity, parental education, whether they lived with both biological parents at T1 and depressive and anxiety disorders at T1.
Participants who completed the T3 assessment were eligible for inclusion in the present study (regardless of whether they participated at T4). The 50 probands with a lifetime diagnosis of a bipolar spectrum and/or psychotic disorder were excluded, yielding a final n of 891. A total of 770 participants were assessed at all four time points; 119 at three time points; and 2 at two time points. All participants had diagnostic information up to at least age 24.
Measures
At T1 and T2, offspring were interviewed with a version of the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Orvaschel et al. 1982), which combined features of the Epidemiologic and Present Episode versions, and included additional items to derive DSM-III-R diagnoses. At T3 and T4, offspring were interviewed using the Longitudinal Interval Follow-up Evaluation (LIFE; Keller et al. 1987), which elicited detailed information about the onset and course of psychiatric disorders since the previous evaluation. Diagnoses were based on DSM-III-R (APA, 1987) criteria for T1 and T3 and DSM-IV (APA, 1994) criteria for T4. Interviews at T3 and T4 were conducted by telephone, which generally yields comparable results to face-to-face interviews (Sobin et al. 1993; Rohde et al. 1997). Most interviewers had advanced degrees in a mental health field and several years of clinical experience. The inter-rater reliability (expressed as k) for depressive disorders (major depressive disorder or dysthymia) was 0.82 (n = 233) at T1, 1.00 (n = 166) at T2, 0.86 (n = 190) at T3 and 0.81 (n = 124) at T4. The inter-rater reliability for anxiety disorders, which included generalized anxiety disorder, overanxious disorder of childhood, post-traumatic stress disorder, panic with/without agoraphobia, agoraphobia without panic, social phobia, simple phobia, obsessive–compulsive disorder, and separation anxiety disorder, was 0.76 (n = 233) at T1, 0.80 (n = 166) at T2, 0.87 (n = 190) at T3 and 0.76 (n = 124) at T4.
Data analysis
For each participant, a record was created indicating whether a depressive or anxiety disorder onset occurred, as either first episodes or recurrences, during each of the following developmentally meaningful periods: childhood (up to age 13); adolescence (ages 14–18); emerging adulthood (ages 19–23); and young adulthood (ages 24–30). Caucasian OADP participants with no history of psychopathology up to T2 were undersampled in the T3 follow-up; hence all statistical analyses were weighted as a function of their probability of being selected at T3. The numbers and proportions of participants, presented here for descriptive purposes, are unweighted, except where noted.
Structural equation modeling was performed using Mplus, version 3.13 (Muthén & Muthén, 1998–2004). Because observed variables were dichotomous, the weighted least squares estimator with a diagonal weight matrix and robust standard errors and a mean-and variance-adjusted χ2 test statistic (WLSMV) and theta parameterization (Muthén & Muthén, 2004) were implemented. Recently, a simulation study found that the WLSMV estimator performed well under a variety of sample sizes (250–1000) and a range of observed indicators (2–8; Nussbeck et al. 2006) and performed better than the standard weighted least squares estimator in identifying correct models (Flora & Curran, 2004).
Models were evaluated on several indices of goodness of fit, as well as whether theoretical predictions, as indicated by specific paths within the model, were supported. The overall fit of the models was evaluated using the χ2 test, the comparative fit index (CFI; Bentler, 1990), and the root mean square error of approximation (RMSEA; Steiger, 1989). Although existing guidelines are somewhat arbitrary (Marsh et al. 2004), according to current conventions good fit is indicated by a non-significant χ2, a CFI greater than 0.95 (Hu & Bentler, 1999), and an RMSEA below 0.05 (MacCallum et al. 1996). In WLMSV, differences between observed χ2 values are not distributed as χ2. For comparisons of nested models, the Mplus difftest procedure was used, which appropriately computes differences in χ2 of nested models (Asparouhov & Muthén, 2006). Structural equation modeling analyses presented here used data based on casewise deletion. However, the results were the same when missing data were imputed.
Results
We examined differences between the sample used here and the full, T1 sample. Because of the stratified sampling strategy introduced at the T3 assessment, participants with a history of psychopathology and members of ethnic minority groups were over-sampled. For the participants included in the present sample, 57.5% (n = 512) had some form of psychopathology at T1 or T2 and 11.1% (n = 99) were members of ethnic minority groups. We compared the participants in the present sample to the non-participants on other demographic characteristics collected at T1 (Table 1). Participants did not differ from non-participants on whether they lived with both their biological parents at T1 or family socio-economic status (SES), as indicated by whether at least one parent completed a BA or BS. However, the present sample differed from the overall initial sample on gender [χ2(1) = 8.48, p < 0.01] and age at T1 [F(1, 1707) = 8.65, p < 0.01]. The proportion of females was greater among those included in the present sample than among those who were not included. Participants in the present sample were slightly older at T1 than those who were not included.
Table 1.
Comparisons of participants and non-participants
| Characteristic at T1 | T1 participant not included in the present study (n = 818) |
T1 participant included in the present study (n = 891) |
|---|---|---|
| Live with biological parents, n (%) | 419 (51.3) | 490 (55.2) |
| Socio-economic status (BA/BS), n (%) | 352 (46.2) | 383 (45.1) |
| Female sex, n (%) | 381 (46.5)a | 510 (57.2)b |
| Age, mean (S.D.) | 16.5 (1.15)a | 16.6 (1.22)b |
s.d., Standard deviation.
Different superscripts reflect significant differences at p < 0.05.
The number of participants with depressive and anxiety disorder onsets in each developmental period is shown in Table 2. Table 2 includes un-weighted period-incidence data for overall and specific forms of depressive and anxiety disorders and the weighted period-incidence of overall depressive and anxiety disorders. The associations between depressive and anxiety disorder onsets at each developmental period are shown in Table 3. These data take the complex sampling design of the study into account by weighting participants according to their probability of selection for the T3 assessment.
Table 2.
Frequencies and percentages of anxiety and depressive disorders across developmental periods
| Childhood | Adolescence | Emerging adulthood |
Young adulthood |
|
|---|---|---|---|---|
| Unweighted period incidence | ||||
| Any depressive disorder | 86 (9.7) | 270 (30.3) | 268 (30.1) | 257 (28.8) |
| MDD | 68 (7.6) | 264 (29.6) | 267 (30.0) | 255 (28.6) |
| Dysthymia | 23 (2.6) | 17 (1.9) | 4 (0.4) | 5 (0.6) |
| Any anxiety disorder | 101 (11.3) | 59 (6.6) | 52 (5.8) | 72 (8.1) |
| GAD | 0 (0) | 0 (0) | 0 (0) | 16 (1.8) |
| Overanxious disorder | 10 (1.1) | 6 (0.7) | 0 (0) | 0 (0) |
| PTSD | 16 (1.8) | 16 (1.8) | 28 (3.1) | 12 (1.3) |
| Panic w/o agoraphobia | 1 (0.1) | 7 (0.8) | 12 (1.3) | 20 (2.2) |
| Panic with agoraphobia | 1 (0.1) | 5 (0.6) | 3 (0.3) | 12 (1.3) |
| Agoraphobia w/o panic | 1 (0.1) | 2 (0.2) | 2 (0.2) | 0 (0) |
| Social phobia | 13 (1.5) | 8 (0.9) | 5 (0.6) | 9 (1.0) |
| Simple phobia | 19 (2.1) | 13 (1.5) | 6 (0.7) | 11 (1.2) |
| OCD | 3 (0.3) | 3 (0.3) | 0 (0) | 8 (0.9) |
| Separation anxiety | 50 (5.6) | 4 (0.4) | 0 (0) | 0 (0) |
| Weighted period incidence | ||||
| Any depressive disorder | 6.9 | 22.4 | 26.8 | 25.9 |
| Any anxiety disorder | 8.3 | 5.4 | 4.6 | 7.3 |
n = 891. Values are given as n (%).
MDD, Major depressive disorder; GAD, generalized anxiety disorder; PTSD, post-traumatic stress disorder; OCD, obsessive–compulsive disorder.
Childhood includes onsets up to age 13. Adolescence includes onsets between ages 14 and 18. Emerging adulthood includes onsets between ages 19 and 23. Young adulthood includes onsets between ages 24 and 30.
Table 3.
Observed tetrachoric correlations between measured variables used in the structural equation models
| Depressive disorders | Anxiety disorders | |||||||
|---|---|---|---|---|---|---|---|---|
| Childhood | Adolescent | Emerging adulthood |
Young adulthood |
Childhood | Adolescent | Emerging adulthood |
Young adulthood |
|
| Depressive disorders | ||||||||
| Childhood | – | |||||||
| Adolescent | 0.29*** | – | ||||||
| Emerging adulthood | 0.28*** | 0.34*** | – | |||||
| Young adulthood | 0.31*** | 0.39*** | 0.47*** | – | ||||
| Anxiety disorders | ||||||||
| Childhood | 0.48*** | 0.32*** | 0.21** | 0.25*** | – | |||
| Adolescent | 0.26* | 0.40*** | 0.22** | 0.12 | 0.35*** | – | ||
| Emerging adulthood | 0.31** | 0.25** | 0.41*** | 0.22* | 0.48*** | 0.38*** | – | |
| Young adulthood | 0.29** | 0.14 | 0.31*** | 0.51*** | 0.28** | 0.28** | 0.26* | – |
p < 0.05
p < 0.01
p < 0.001. Associations are weighted according to the complex sampling design.
Measurement models
We began our model estimation process using fully constrained models. We then used a model trimming approach in which we systematically removed constraints and examined change in model fit. The one-factor model specified a single latent factor that constrained factor loadings within and between depressive and anxiety disorders; threshold parameters within and between depressive and anxiety disorders; and covariance paths between concurrent depressive and anxiety disorders to be equal. However, the estimates were not constrained to be equal across the type of parameter (e.g. factor loading parameters were not constrained to be equal to threshold parameters). The three-factor model specified a depressive, an anxiety, and a common latent factor. The factor loadings within and between depressive and anxiety disorders for the depressive and anxiety factors were constrained to be equal and the factor loadings for the common factor to the depressive and anxiety disorders indicators were constrained to be equal. Threshold parameters within and between depressive and anxiety disorders and covariance paths between concurrent depressive and anxiety disorders were constrained to be equal. No equality constraints were placed on the residual terms.
Fit for the fully constrained models was poor. Table 4 outlines the sequence of modifications to the models that were made to improve model fit. These modifications were guided by theoretical and empirical considerations. Importantly, the same modifications optimized model fit for both the one-factor and the three-factor models.
Table 4.
Measurement model construction
| One-factor | Three-factor | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model | χ2 | df | CFI | RMSEA | Test | Test difference | χ2 | df | CFI | RMSEA | Test | Test difference | ||
| 1 | 482.73*** | 27 | <0.01 | 0.14 | – | – | 483.87*** | 27 | <0.001 | 0.14 | – | – | ||
| 2 | 211.68*** | 27 | 0.58 | 0.09 | 2 v. 1 | 329.60a | <0.0001 | 197.06*** | 26 | 0.62 | 0.09 | 2 v. 1 | 329.60a | <0.0001 |
| 3 | 52.17** | 26 | 0.94 | 0.03 | 3 v. 2 | 193.24a | <0.0001 | 38.86** | 25 | 0.97 | 0.03 | 3 v.2 | 193.24a | <0.0001 |
| 4 | 46.71** | 25 | 0.95 | 0.03 | 4 v. 3 | 6.64a | <0.01 | 33.55** | 24 | 0.98 | 0.02 | 4 v.3 | 6.65a | <0.01 |
| 5 | 130.18 | 25 | 0.76 | 0.07 | 5 v. 4 | 127.70a | <0.0001 | 116.27 | 24 | 0.79 | 0.07 | 5 v. 4 | 127.70a | <0.0001 |
| 6 | 38.59* | 24 | 0.97 | 0.03 | 6 v. 5 | 10.32a | <0.01 | 25.63* | 23 | 0.99 | 0.01 | 6 v. 5 | 10.32a | <0.01 |
| 7 | 33.15 | 23 | 0.98 | 0.02 | 7 v. 6 | 6.17a | <0.05 | 20.31 | 22 | 1.00 | <0.0001 | 7 v. 6 | 6.17a | <0.05 |
| 8 | 34.00 | 24 | 0.98 | 0.02 | 8 v. 7 | 0.72a | 0.39 | 21.07 | 23 | 1.00 | <0.0001 | 8 v. 7 | 0.72a | 0.39 |
| 9 | 33.27 | 22 | 0.97 | 0.02 | 9 v. 8 | 1.91b | 0.59 | 19.98 | 21 | 1.00 | <0.0001 | 9 v. 8 | 1.91b | 0.59 |
| 10 | 33.83 | 24 | 0.98 | 0.02 | 10 v. 8 | 1.53a | 0.22 | 22.39 | 23 | 1.00 | <0.0001 | 10 v. 8 | 0.08a | 0.77 |
df, Degrees of freedom; CFI, comparative fit index; RMSEA, root mean square error of approximation.
A 1-df test.
A 2-df test. χ2 difference testing was conducted using the difftest option in Mplus.
Model 1: factor loadings within and between depressive and anxiety disorders, threshold parameters within and between depressive and anxiety disorders, and covariance paths between concurrent depressive and anxiety disorders constrained to be equal. Model 2: same constraints as Model 1 except threshold parameters across depressive and anxiety disorders are different. Model 3: same constraints as Model 2 except the threshold parameter for childhood depressive disorder is free to vary. Model 4: same constraints as Model 3 except the threshold parameters for adolescent depressive disorder is free to vary. Model 5: same constraints as Model 4 except the threshold parameters for childhood and adolescent depressive disorder are constrained to be equal. Model 6: same constraints as Model 4 except the threshold parameter for childhood anxiety disorder is free to vary. Model 7: same constraints as Model 6 except the threshold parameters for young adulthood anxiety disorder is free to vary. Model 8: same constraints as Model 7 except the threshold parameters for childhood and young adulthood anxiety disorders are constrained to be equal. Model 9: same constraints as Model 8 except covariance paths between concurrent depressive and anxiety disorders are allowed to vary. Model 10: same constraints as Model 8 except factor loadings between depressive and anxiety disorders are allowed to vary.
Model modifications examined the influence of allowing threshold parameters to be free to vary. In the context of these models, threshold parameters are highly influenced by the rates of psychopathology. Thus, it is expected that these parameters will differ over the course of time, reflecting the developmental trajectories of depressive and anxiety disorders (Byrne et al. 1989; Pentz & Chou, 1994). Indeed, the threshold parameters were found to be different, both within and between depressive and anxiety disorders. Within depressive disorders, the threshold for childhood was significantly higher than the threshold for adolescence, which, in turn, was higher than the threshold for emerging adulthood and young adulthood. However, there was no significant difference between the thresholds for emerging adulthood and young adulthood. Within anxiety disorders, the threshold for childhood was similar to the threshold for young adulthood, and the threshold for adolescence was similar to the threshold for emerging adulthood. However, the thresholds for childhood and young adulthood were lower than the thresholds for adolescence and emerging adulthood.
As a result of these modifications to the threshold parameters, the best-fitting of the one-factor and three-factor models is Model 8 in Table 4. Although Model 8 does not provide an improvement in model fit over Model 7, Model 8 is the more parsimonious of the two models, and is therefore the preferred model. Both the one- and three-factor models fit the data well based on the non-significant χ2, high CFI, and low RMSEA values. Allowing covariance paths between contemporaneous depressive and anxiety disorders at each time to vary, and permitting factor loadings to depressive and anxiety disorders to differ, did not improve model fit.
Substantive model tests
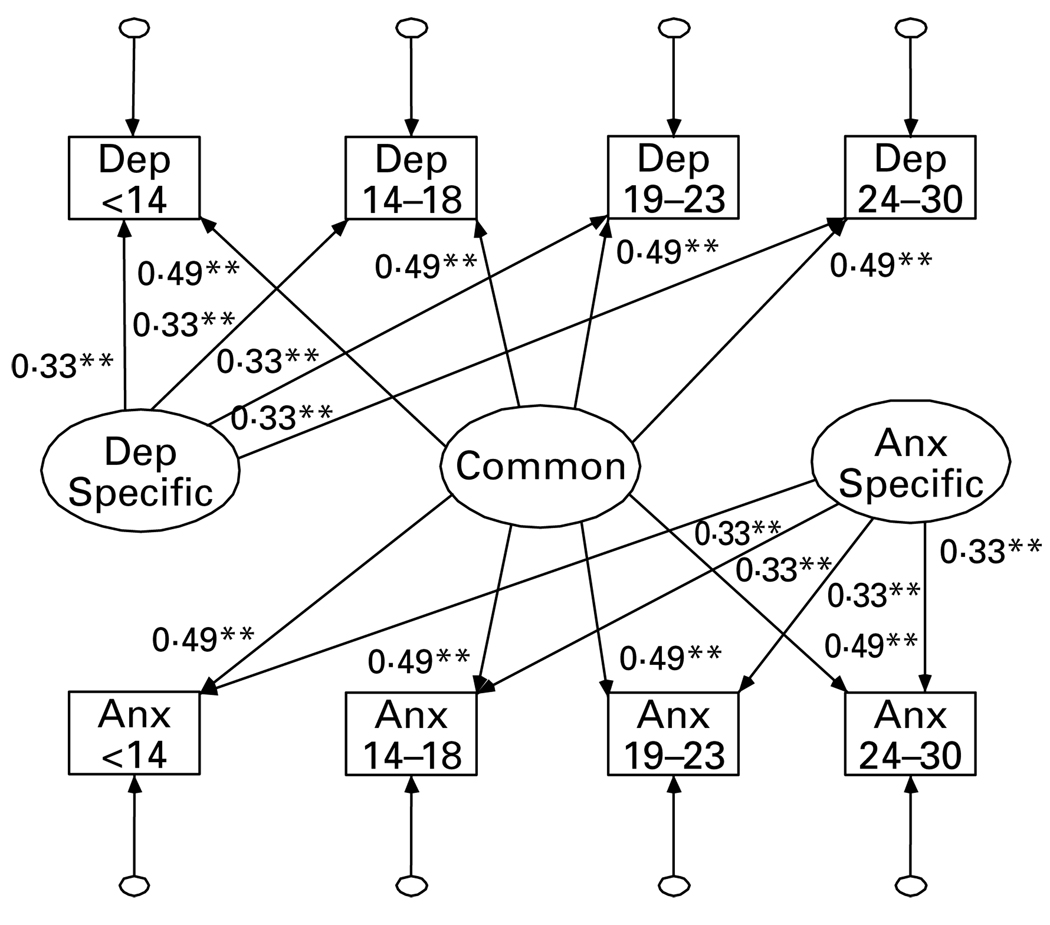
The one- and three-factor models that resulted from the model constraints described above are nested, allowing a direct comparison of model fit by a χ2 difference test using the Mplus difftest procedure (Asparouhov & Muthén, 2006). This test examined whether the three-factor model better accounted for the data than the one-factor model. The results indicated that the three-factor model (Fig. 1) fit the data significantly better than the one-factor model [χ2(1) = 16.44, p < 0.0001].
Fig. 1.
The three-factor model. ** p < 0.001. Dep <14, depressive diagnosis lifetime up to age 13; Dep 14–18, depressive diagnosis between ages 14 and 18; Dep 19–23, depressive diagnosis between ages 19 and 23; Dep 24–30, depressive diagnosis between ages 24 and 30; Anx <14, anxiety diagnosis lifetime up to age 13; Anx 14–18, anxiety diagnosis between ages 14 and 18; Anx 19–23, anxiety diagnosis between ages 19 and 23; Anx 24–30, anxiety diagnosis between ages 24 and 30; Dep Specific, depressive disorder specific latent factor; Anx Specific, anxiety disorder specific latent factor; Common, Common latent factor. For the three-factor model: χ2(23) = 21.07, p = 0.58; comparative fit index (CFI) = 1.00; root mean square error of approximation (RMSEA) <0.0001. Not shown in the model are covariance paths between the error terms for diagnoses (r’s = 0.21, p < 0.001).
Given that the three-factor model provided the better fit, we conducted a series of additional comparisons. First, we examined whether factor loadings between the common factor and the unique factors were significantly different. Model comparisons found that they were indeed different [χ2(1) = 6.18, p < 0.05], such that the magnitude of the factor loadings for the common factor were stronger than the factor loadings for each of the unique factors. Second, we compared the model that constrained the factor loadings to the depressive-specific and anxiety-specific factors to be equal to each other over time and constrained the factor loadings to the common factor to be equal over time to a model that did not impose the those equality constraints. Model fit did not differ significantly [χ2(12) = 11.92, p = 0.45]. Thus, we retained the more parsimonious model. Third, we examined whether direct associations within depressive disorders at adjacent developmental periods and anxiety disorders at adjacent developmental periods would improve model fit. Including these paths did not improve model fit [χ2(6) = 4.57, p = 0.60]; hence, we retained the more parsimonious model.3 Fourth, we examined the possibility that there are gender differences in the relationship between depressive and anxiety disorders. In this multigroup analysis, significant gender differences were seen in the thresholds [χ2(4) = 119.19, p < 0.0001]. These effects reflect differences in the prevalence rates between men and women. After the thresholds were allowed to vary between groups, no significant gender differences were seen between factor loadings on any of the factors [χ2(2) = 0.01, p > 0.99].
Discussion
In order to understand the high co-morbidity between depressive and anxiety disorders, recent investigators have proposed one- and three-factor variable models of depression and anxiety (Clark & Watson, 1991; Krueger & Finger, 2001). The present study extended this literature by directly comparing these models using a large community sample that was relatively homogeneous with respect to age and a longitudinal design that spanned multiple developmental periods.
The one-factor model posited that a single latent factor accounts for the longitudinal associations between depressive and anxiety disorders. This latent factor is similar to the internalizing dimension of psychopathology described by Krueger (1999; Krueger et al. 1998; Krueger & Finger, 2001) and others (Vollebergh et al. 2001; Kendler et al. 2003; Lahey et al. 2004). The three-factor model posited that depressive disorders and anxiety disorders are both influenced by a common factor, but each is also influenced by a disorder-specific factor. This is analogous to Clark & Watson’s (1991) tripartite model, although we did not specify the content of the common and disorder-specific factors. Additionally, Clark & Watson (1991) do not require the three factors to be orthogonal. In contrast, because our common factor was based on the covariance between depressive and anxiety disorders, we were forced to assume that the factors were independent.
The three-factor model fit the data extremely well, and provided a significantly better fit than the one-factor model. The depressive and anxiety disorders had similar loadings on the common factor, and the loadings from the depressive disorder latent factor to the depression indicators were similar in magnitude to the loadings from the anxiety disorder latent factor to the anxiety indicators. In addition, the factor loadings did not differ significantly across males and females. However, the magnitude of the factor loadings for the common factor were significantly larger than the factor loadings for the disorder-specific factors.
We expected that there might be developmental differences in the role of common versus specific factors over time. A common factor could be more prominent earlier in development, with internalizing psychopathology becoming more differentiated over time. This would be reflected by observing significant decreases in the factor loadings from the common factor to the indicators, and increases in the factor loadings from the specific factors to the indicators, over the course of development. Alternatively, given evidence that anxiety disorders have an earlier onset than depressive disorders (Mineka et al. 1998), an anxiety-specific factor could be more prominent earlier in development, and a common factor would become increasingly influential over time. This would be reflected by observing significant decreases in the factor loadings from the anxiety-specific factor to the indicators, and significant increases in the factor loadings from the common factor to the indicators across developmental periods. However, these patterns were not observed. Instead, the factor loadings to the depressive and anxiety disorder indicators from all three latent factors were not significantly different across developmental periods. This suggests that depression and anxiety may reflect stable, trait-like characteristics from childhood to young adulthood, and suggests that there is considerable developmental continuity in depressive and anxiety disorders. However, it should be noted that the data on childhood psychopathology were retrospective, and participants were only followed to age 30. Hence, we cannot rule out the possibility of subtle developmental changes in childhood or after young adulthood.
To achieve satisfactory fit of the models, almost all a priori constraints that were removed were related to the threshold parameters of the indicators. In these models, threshold parameters are related to the prevalence of the disorder. Thus, threshold parameter differences reflect the rates of depressive and anxiety disorders across the four developmental periods. The constraints on these parameters indicate that the rates of depressive disorders increased significantly from childhood to adolescence and from adolescence to emerging adulthood. However, there was no difference in rates of depressive disorder between emerging adulthood and young adulthood. These data are consistent with most data on the epidemiology of depressive disorders (Roberts et al. 1998).
Model modifications to the threshold parameters for anxiety disorders reflected a different pattern. Higher rates of anxiety disorders were observed during childhood and young adulthood than during adolescence and emerging adulthood. This pattern appears to reflect the mix of specific anxiety disorders in our sample, and is also fairly consistent with epidemiological data (Costello et al. 2003; Kessler et al. 2005b). As can be seen in Table 2, the rate of separation anxiety disorder peaks during childhood, and diminishes from adolescence to young adulthood. This appears to contribute to the lower period-incidence of anxiety disorder during adolescence and emerging adulthood. However, during young adulthood, rates of generalized anxiety disorder and panic disorder increase, contributing to the higher period-incidence rates during this developmental period.
In another recent community-based longitudinal study, Fergusson et al. (2006) found evidence for a single internalizing factor as well as disorder-specific paths at each of three assessments. Their results are highly consistent with those of the present study even though we specified somewhat different structural models, used diagnoses rather than dimensional symptom scores, and examined a broader segment of development.
The present study had a number of significant strengths, including the use of a prospective longitudinal design spanning multiple developmental periods, a large community sample, and semi-structured diagnostic interviews to assess depressive and anxiety disorders. Additionally, we formally tested two competing latent variable models of the relationship between depressive and anxiety disorders over time, and used a statistical approach that took into account our complex sampling and allowed for the examination of categorical diagnoses, as opposed to symptom counts.
However, our findings should be interpreted with some caution. First, we examined summary categories of depressive and anxiety disorders. The anxiety disorder category included a variety of specific anxiety disorders and the depressive disorder category included both major depressive and dysthymic disorders. Unfortunately, examining specific diagnoses, especially within the anxiety disorders, was not feasible as small numbers of participants met criteria for most of the specific anxiety disorders at any particular assessment. Thus, the findings may not apply equally well to every anxiety and depressive disorder category (Mineka et al. 1998).
Second, the rates of anxiety disorders in the OADP are lower than some other large community samples consisting mainly of adults (e.g. Kessler et al. 2005a). However, other community-based studies of adolescents and young adults have reported markedly similar rates of anxiety disorders in their samples (e.g. Costello et al. 2003; Merikangas et al. 2003). Nonetheless, it is possible that samples with a higher prevalence or different distribution of specific anxiety disorders could yield different findings.
Third, we cannot rule out the possibility that other models might provide a better fit to the data. In particular, we did not fully test models that posit direct influences between anxiety disorders and depressive disorders (e.g. anxiety causes subsequent depression; Merikangas et al. 2003). We examined one plausible model (see footnote 2); however, this model did not fit the data adequately.
Fourth, over the course of the OADP the DSM was revised. However, the changes in depressive and anxiety disorder criteria were generally minor. Additionally, two different interviews were used to assess psychopathology, and early assessments were conducted face-to-face, while later assessments were conducted by telephone. If there was a systematic effect of changing diagnostic criteria, interviews or assessment procedures, the residual correlations between the observed indicators should differ with developmental period. However, this was not the case as Model 9 did not fit the data significantly better than Model 8. Thus, it is unlikely that the results are biased based on differences between diagnostic criteria, instruments or assessment procedures.
Fifth, attrition occurred between each of the four waves of assessments. The sample used in the current study had a higher proportion of females and was slightly older than the other subjects in the initial assessment, but did not differ on parental education or whether they lived with both biological parents. Although we cannot rule out the possibility of attrition biases, it is important to note that the results were almost identical whether or not missing data were imputed in the analysis.
In conclusion, our findings indicate that the co-morbidity between depressive and anxiety disorders over time is best explained by a combination of common and unique influences that are stable over the course of development from childhood to young adulthood. This three-factor model is similar in form to Clark & Watson’s (1991) tripartite model, although we did not examine the specific content of the factors (negative and positive affect and physiological arousal) posited in their model. Determining the nature and etiopathogenesis of the common and unique factors that underlie internalizing psychopathology is an important priority for future studies. Finally, the present findings support the development of unified intervention models, such as the approach outlined by Barlow et al. (2004), that target shared aspects of depressive and anxiety disorders, but also tailor treatment to address disorder-specific features.
Acknowledgments
This work was partially supported by National Institute of Mental Health Grants RO1 MH66023 (Dr Klein), RO1 MH40501, RO1 MH50522 and RO1 MH52858 (Dr Lewinsohn).
Footnotes
Portions of these findings were presented at the Virtual Meeting of the Society for Research in Psychopathology, October 2005. The actual meeting was cancelled due to hurricanes.
The notes appear on p. 361.
Declaration of Interest
None.
Some of these studies have also provided support for two first-order factors, generally labeled as anxious-misery and fear. We did not estimate a two-level model with lower-order anxious-misery and fear factors because it could not be compared to the three-factor model discussed later (i.e. the lower-order constructs would change from exogenous latent factors to endogenous latent factors). In addition, the distribution of cases of specific anxiety disorders in our sample was such that the distinction between anxious-misery and fear factors overlapped almost entirely with the distinction between depressive and anxiety disorders.
We use the term period-incidence to include first and recurrent episodes of disorders during each time frame, rather than the more traditional definition of only new incident cases.
We also examined a direct-effects model. This model specified direct longitudinal paths between depression at adjacent time points, anxiety at adjacent time points, and the cross-lagged paths. This model provided a marginal fit to the data [χ2(11) = 46.23, p < 0.001, CFI = 0.91, RMSEA = 0.06]. Although no formal model comparisons are possible between the direct-effects model and the three-factor model, each of the three fit indices suggests that the three-factor model fits the data better than the direct-effects model.
References
- Andrews G. Comorbidity and the general neurotic syndrome. British Journal of Psychiatry. 1996;168 Suppl. 30:76–84. [PubMed] [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 3rd edn. Washington, DC: American Psychological Association; 1987. revised. [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 4th edn. Washington, DC: American Psychological Association; 1994. revised. [Google Scholar]
- Asparouhov T, Muthén B. Robust chi square difference testing with mean and variance adjusted test statistics. Mplus Web Notes: No. 10. 2006 ( http://www.statmodel.com/download/webnotes/webnote10.pdf).
- Barlow DA, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Belzer K, Schneier FR. Co-morbidity of anxiety and depressive disorders : issues in conceptualization, assessment, and treatment. Journal of Psychiatric Practice. 2004;10:296–306. doi: 10.1097/00131746-200409000-00003. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Brady EU, Kendall PC. Comorbidity of anxiety and depression in children and adolescents. Psychological Bulletin. 1992;111:244–255. doi: 10.1037/0033-2909.111.2.244. [DOI] [PubMed] [Google Scholar]
- Brown C, Schulberg HC, Madonia MJ, Shear MK, Houck PR. Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. American Journal of Psychiatry. 1996;153:1293–1300. doi: 10.1176/ajp.153.10.1293. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology. 2001;110:585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Byrne BM, Shavelson RJ, Muthén B. Testing for the equivalence of factor covariance and mean structures: the issue of partial measurement invariance. Psychological Bulletin. 1989;105:456–466. [Google Scholar]
- Chorpita BF, Daleiden EL. Tripartite dimensions of emotion in a child clinical sample: measurement strategies and implications for clinical utility. Journal of Consulting and Clinical Psychology. 2002;70:1150–1160. doi: 10.1037//0022-006x.70.5.1150. [DOI] [PubMed] [Google Scholar]
- Clark LA. The anxiety and depressive disorders: descriptive psychopathology and differential diagnosis. In: Kendall PC, Watson D, editors. Anxiety and Depression: Distinctive and Overlapping Features. San Diego: Academic Press; 1989. pp. 83–129. [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology. 1994;103:103–116. [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Boden JM. Structure of internalising symptoms in early adulthood. British Journal of Psychiatry. 2006;189:540–546. doi: 10.1192/bjp.bp.106.022384. [DOI] [PubMed] [Google Scholar]
- Flora DB, Curran PJ. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychological Methods. 2004;9:466–491. doi: 10.1037/1082-989X.9.4.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling: An Interdisciplinary Journal. 1999;6:1–55. [Google Scholar]
- Joiner TE, Jr, Catanzaro SJ, Laurent J. Tripartite structure of positive and negative affect, depression, and anxiety in child and adolescent psychiatric inpatients. Journal of Abnormal Psychology. 1996;105:401–409. doi: 10.1037//0021-843x.105.3.401. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and co-morbidity of 12-month DSM-IV disorders in the National Co-morbidity Survey Replication. Archives of General Psychiatry. 2005a;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age of onset distributions of DSM-IV disorders in the National Co-morbidity Survey Replication. Archives of General Psychiatry. 2005b;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson KA, Hayward C. Lifetime prevalence and pseudo-co-morbidity in psychiatric research. Archives of General Psychiatry. 2006;63:604–608. doi: 10.1001/archpsyc.63.6.604. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Finger MS. Using item response theory to understand co-morbidity among anxiety and unipolar mood disorders. Psychological Assessment. 2001;13:140–151. [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: generating new hypotheses. Journal of Abnormal Psychology. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Psychosocial characteristics of young adults who have experienced and recovered from major depressive disorder during adolescence. Journal of Abnormal Psychology. 2003;112:353–363. doi: 10.1037/0021-843x.112.3.353. [DOI] [PubMed] [Google Scholar]
- MacCullum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130–149. [Google Scholar]
- Marsh HW, Hau KT, Wen Z. In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Structural Equation Modeling: An Interdisciplinary Journal. 2004;11:320–341. [Google Scholar]
- Merikangas KR, Zhang HP, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study: the Zurich Cohort Study. Archives of General Psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Co-morbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus version 3.13. Los Angeles, CA: Muthén & Muthén; 1998–2004. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 3rd edn. Los Angeles, CA: Muthén & Muthén; 2004. [Google Scholar]
- Nussbeck FW, Eid M, Lischetzke T. Analysing multitrait-multimethod data with structural equation models for ordinal variables applying the WLSMV estimator: what sample size is needed for valid results? British Journal of Mathematical and Statistical Psychology. 2006;59:195–213. doi: 10.1348/000711005X67490. [DOI] [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MA, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. Journal of the American Academy of Child and Adolescent Psychiatry. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- Pentz MA, Chou CP. Measurement invariance in longitudinal clinical research assuming change from development and intervention. Journal of Consulting and Clinical Psychology. 1994;62:450–462. doi: 10.1037//0022-006x.62.3.450. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Attkisson CC, Rosenblatt A. Prevalence of psychopathology in children and adolescents. American Journal of Psychiatry. 1998;155:715–725. doi: 10.1176/ajp.155.6.715. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. American Journal of Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- Sobin C, Weissman MM, Goldstein RB, Adams P, Wickramaratne P, Warner V, Lish JD. Diagnostic interviewing for family studies : comparing telephone and face-to-face methods for the diagnosis of lifetime psychiatric disorders. Psychiatric Genetics. 1993;3:227–233. [Google Scholar]
- Steiger JH. Structural model evaluation and modification: an Interval estimation approach. Multivariate Behavioral Research. 1989;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Tyrer P. The case for cothymia: mixed anxiety and depression as a single diagnosis. British Journal of Psychiatry. 2001;179:191–193. doi: 10.1192/bjp.179.3.191. [DOI] [PubMed] [Google Scholar]
- Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders : the NEMESIS Study. Archives of General Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking mood and anxiety disorders : a quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Weber K, Assenheimer JS, Strauss ME, McCormick RA. Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. Journal of Abnormal Psychology. 1995;104:15–25. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- Watson D, Kotov R, Gamez W. Basic dimensions of temperament in relation to personality and psychopathology. In: Krueger RF, Tackett JL, editors. Personality and Psychopathology. New York: Guilford Press; 2006. pp. 7–38. [Google Scholar]