Abstract
Aortopulmonary fistula is an uncommon but often fatal condition resulting as a late complication of an aortic aneurysm. The most common cause is erosion of a false aneurysm of the descending thoracic aorta into the pulmonary artery, resulting in the development of a left-to-right shunt and leading to acute pulmonary edema and right heart failure. We report an our experience with aortopulmonary fistula as a rare complication associated with thoracic aortic aneurysm and high output heart failure.
Keywords: Fistula, Aortic aneurysm, Heart failure
Introduction
Thoracic aortic aneurysm is less common than abdominal aortic aneurysms. Aortic aneurysm in the aortic arch or the descending aorta is caused mainly by arteriosclerosis, is usually asymptomatic, and is diagnosed incidentally. Associated symptoms include chest pain, dyspnea, and hoarseness resulting from compression of the surrounding organs by the dilated aorta, and dysphagia.
The major complications of thoracic aortic aneurysm include aortic rupture, aortic dissection, and congestive heart failure, which are the main causes of death.1-3)
Aortopulmonary fistula is an uncommon, late complication of an aortic aneurysm that is most commonly caused by aneurysmatic erosion. Aortopulmonary fistula subsequently leads to several complications such as rapid left-to-right shunt and right heart failure.4)
We report a case of aortopulmonary fistula associated with thrombosed thoracic aortic aneurysm, with a literature review.
Case
An 81-year-old female patient with exertional dyspnea visited the emergency room of our hospital and complained of aggravated dyspnea and chest pain. She was diagnosed with hypertension 6 years ago, and has taken medicine without any additional examination since she was hospitalized for congestive heart failure 2 years ago.
At the time of her visit, her blood pressure was 150/95 mmHg, pulse rate 150 beats/min, respiratory rate 35 breaths/min, and body temperature 36.5℃. She was conscious and but looked ill. Thoracic auscultation revealed a Grade IV/VI pansystolic murmur at the apex, a continuous murmur along the left third sternal border, and a rale in both the lung fields.
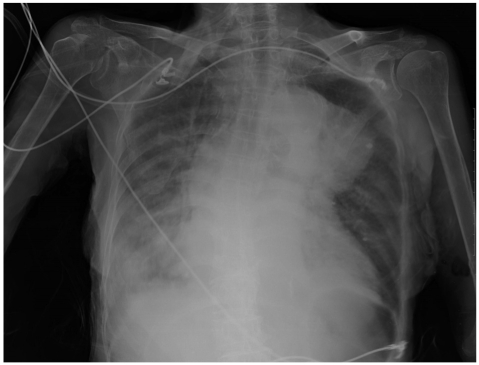
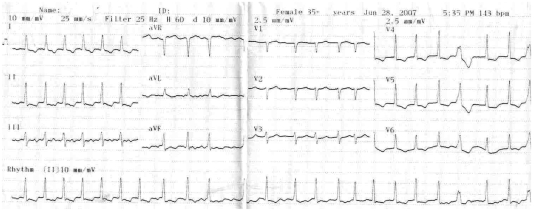
No significant findings were seen in the abdomen, and 1+pitting edema was found in both the legs. The hemoglobin level was 12.9 g/dL, leukocyte 7,600/mm3, and blood platelet 235,000 mm3, and in arterial blood gas analysis, pH was 7.355, PCO2 28.7 mmHg, PO2 91.7 mmHg, HCO- 316.2 mM/L, and oxygen saturation 96.9%. Biochemical analysis was Na 141 mEq/L, K 5.2 mEq/L, Cl 109 mEq/L, blood urea nitrogen (BUN) 32.9 mg/ dL, creatinine 1.9 mg/dL with high N-terminal pro-B-type natruretic peptide (NT-proBNP) >35,000 pg/mL. Serological analysis showed creatine phosphokinase 108 IU/L, creatinine kinase-MB isoenzyme 7.5 ng/mL, troponin-I 0.58 µg/L, total cholesterol 218 mg/dL, low density lipoprotein 186 mg/dL, high density lipoprotein 30 mg/dL, and triglyceride 55 mg/dL. Chest X-ray showed dilatation of the left mediastinum accompanied by right axis deviation of the bronchus, and right costophrenic (CP) angle blunting with medium cardiomegaly, suggesting pleural effusion (Fig. 1). The electrocardiogram showed transient atrial fibrillation with approximately 150 beats/min pulse rate and left ventricular hypertrophy, and T wave inversion accompanied by ST-segment depression (2 mm-3 mm) in V3-V6 (Fig. 2).
Fig. 1.
Chest AP showed cardiomegaly with right pleural effusion. An aneurysm of the arch of the aorta is seen, causing mediastinal widening. AP: anterioposterior.
Fig. 2.
The electrocardiogram showed atrial fibrillation, left ventricular hypertrophy and T wave inversion accompanied by ST-segment depression in V3-V6.
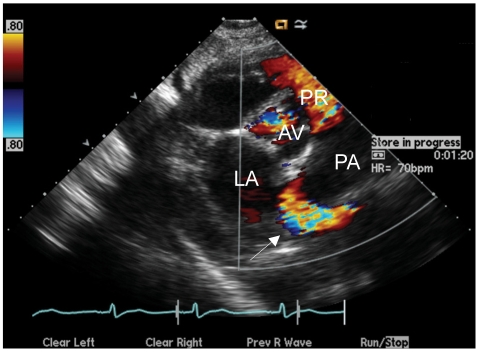
In transthoracic echocardiography, left ventricle function was normal as 64% of ejection fraction, and no sign of regional wall motion abnormality. Left ventricle end-diastolic dimension was dilated as big as 52 mm (3.7 cm/m2) and the size of the left atrium was dilated as big as 42 mm (3 cm/m2) by M-mode. Doppler echocardiography showed a thick mitral valve and moderate mitral regurgitation and moderate pulmonary hypertension (right ventricle systolic pressure=60 mmHg) accompanied by tricuspid regurgitation. The aortic root was also dilated as big as 41 mm, abnormal blood flow from the aorta to the dilated pulmonary artery (31 mm) was suspected at the aortic root level on the parasternal short axis view, and aliasing flow (Vmax=2.3 m/s) was detected around the pulmonary artery (Fig. 3).
Fig. 3.
At the aortic root level on the parasternal short axis view (color doppler) showing abnormal blood flow around the pulmonary artery (white arrow). AV: aortic valve, PR: pulmonic regurgitation, LA: Left atrium, PA: pulmonary artery.
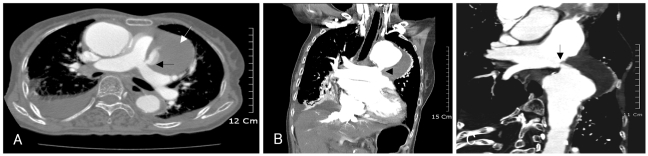
In the chest multi-detector CT, pulmonary edema was present in both lungs, with a slight pleural effusion in both thoracic cavities resulting in subsegmental atelectasis in the right lower and middle lobes. A large aortic aneurysm (about 7 cm) from the aortic arch out and downward was detected. The core was filled with low density thrombus, and the downside of aortic aneurysm connected with the main pulmonary artery, resulting in aortopulmonary fistula. Both the ascending aorta and pulmonary artery were also dilated to about 4.7 cm and 4.2 cm respectively. No compression of the surrounding organs, aortic dissection, or aortic rupture were detected (Fig. 4).
Fig. 4.
The CT scan shows thrombosed aortic aneurysm (white arrow) and aortic aneurysm is communicated with pulmonary artery resulting in aortopulmonary fistula (black arrow) (A). coronal reformated image demonstrates communication from aortic aneurysm to main pulmonary artery (black arrow) (B). 3D reconstructed image shows the aortopulmonary fistula (black arrow) (C).
This aortopulmonary fistula by an aortic aneurysm caused heart failure. Although medical treatment was given before surgical treatment, heart failure worsened and pulmonary edema and pleural effusion were aggravated in the chest X-ray. She refused surgery because of her age and lack of a direct guardian. Though we tried medical treatment and thoracentesis, she died from refractory heart failure without aortic dissection or rupture 13 days after she was hospitalized.
Discussion
The morbidity of thoracic aortic aneurysm is 5.9 of 100,000 persons but the rate is not as high as abdominal aortic aneurysm, which shows 2-4% morbidity in adults.1),2) The causes of thoracic aortic aneurysm include arteriosclerosis, cystic medial necrosis, Marfan's syndrome, Ehlers-Danlos syndrome, hypertension, aortic bicuspid valve, syphilis, infectious aortitis, giant cell aortitis, and aortic trauma.
The symptoms of aortic aneurysm are chest pain, dyspnea, congestive heart failure by dilation of aortic root and aortic regurgitation, cerebral infarction by thromboembolism, renal infarction, peripheral artery ischemia, dysphagia due to compression of the esophagus, hoarseness due to recurrent laryngeal nerve compression, Hornor's Syndrome by compression of the superior cervical ganglion, and obstructive pneumonitis by compression of the trachea.5) The complications of thoracic aortic aneurysm include aortic dissection and rupture, congestive heart failure, and aortopulmonary fistula.
Here, aortopulmonary fistula is an unusual complication associated with aortic aneurysm. Aortopulmonary fistula can be found during the development of chronic diseases such as pneumonia, lung abscess, and mycotic aortic aneurysm. However, they usually occur after erosion or rupture of a degenerative or false aneurysm of the distal aortic arch or descending thoracic aorta into the lung,8-10),12) but can also be caused by trauma or post-operative complications after aortic surgery, including aortic valve replacement.11)
The common symptoms of aortopulmonary fistula include chest pain, hemoptysis, and dyspnea or other respiratory symptoms. The hemoptysis, which is characteristically intermittent or recurrent, occurs when developed hematoma "leaks" into the bronchopulmonary tree due to aortic rupture.4)
In this case, there was neither surgical history nor hemoptysis, and aortopulmonary fistula might have formed due to erosion from continuous pulsatile friction between the pulmonary artery and the aortic aneurysm wall, but it remains unclear how long the aortic aneurysm had been present.11),12)
Moreover, high output heart failure due to a left-to-right shunt (ejection fraction: 64%) resulted in pulmonary edema and pleural effusion, leading to left ventricle heart failure, pitting edema, and moderate pulmonary hypertension, which ultimately led to right ventricle heart failure.
As a rule, aortopulmonary fistula should be treated surgically and percutaneous coil embolization has shown favorable outcomes.13) In addition, endovascular stent-graft repair of aortopulmonary fistula appears to be safe and well tolerated.14),15) In this case the guardian of the patient rejected surgery because of her age, and despite medication and conservative treatment, she died from refractory heart failure 13 days after she was hospitalized.
Aortopulmonary fistula is an uncommon complication of aortic aneurysm, and we report this case with a literature review because of the few reports of high-output heart failure associated with aortopulmonary fistula in aged patients without a history of ruptured aortic aneurysm, aortic dissection, or surgery.
References
- 1.Bickerstaff LK, Pairolero PC, Hollier LH, et al. Thoracic aortic aneurysms: a population based study. Surgery. 1982;92:1103–1108. [PubMed] [Google Scholar]
- 2.Spurgeon D. US screening programme shows high prevalence of aortic aneurysm. BMJ. 2004;328:852. doi: 10.1136/bmj.328.7444.852-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zips DP, Libby P, Bonow RO, Braunwald E. Braunwald's Heart disease: A textbook of cardiovascular medicine. 7th ed. Philadelphia: Sauders; 2005. pp. 1410–1415. [Google Scholar]
- 4.Belgi A, Altekin E, Yalcinkaya S, Tüzüner FE. Acquired aortopulmonary fistula: a case of ruptured aneurysm of the thoracic aorta. Anadolu Kardiyol Derg. 2003;3:275–278. [PubMed] [Google Scholar]
- 5.Halperin JL, Olin JW. Disease of the aorta. In: Fuster V, editor. Hurst's The Heart. 11th ed. New York: McGraw-Hil; 2004. p. 2304. [Google Scholar]
- 6.Elefteriades JA. Thoracic aortic aneurysm: current approach to surgical timing. ACC Curr J Rev. 2002;11:82–88. [Google Scholar]
- 7.Jang YS, Jin SW, Park HC, et al. A case of thoracic aortic aneurysm presenting as hoarseness of voice: Ortner's syndrome. Korean J Med. 2003;64:105–108. [Google Scholar]
- 8.Killen DA, Muehlebach GF, Wathanacharoen S. Aortopulmonary fistula. South Med J. 2000;93:195–198. [PubMed] [Google Scholar]
- 9.Fernandez Gonzales AL, Montero JA, Luna D, Gil O, Sanjuan VM, Monzonis AM. Aortobronchial fistula secondary to chronic post-traumatic thoracic aneurysm. Tex Heart Inst J. 1996;23:174–177. [PMC free article] [PubMed] [Google Scholar]
- 10.Favre J, Gournier J, Adham M, Rosset E, Barral X. Aortobronchial fistula: report of three cases and review of the literature. Surgery. 1994;115:264–270. [PubMed] [Google Scholar]
- 11.Bol A, Missault L, Dossche KM, Delanote J. Aortopulmonary artery fistula in atherosclerotic pseudoaneurysm presenting with congestive heart failure after aortic valve replacement. Acta Chir Belg. 2006;106:240–242. doi: 10.1080/00015458.2006.11679882. [DOI] [PubMed] [Google Scholar]
- 12.Kim TH, Moon CI, Choi JW, Choi MJ. Congenital aortopulmonary fistula presenting as an exertional dyspnea. Korean Circ J. 2000;30:1291–1294. [Google Scholar]
- 13.Mukadam M, Barraclough J, Riley P, Bonser R. Acquired aortopulmonary artery fistula following proximal aortic surgery. Interact Cardiovasc Thorac Surg. 2005;4:388–390. doi: 10.1510/icvts.2005.106245. [DOI] [PubMed] [Google Scholar]
- 14.Kochi K, Okada K, Watari M, Orihashi K, Sueda T. Hybrid endovascular stent grafting for aortic arch aneurysm with aortopulmonary fistula. J Thoracic Cardiovasc Surg. 2002;123:363–364. doi: 10.1067/mtc.2002.119061. [DOI] [PubMed] [Google Scholar]
- 15.Wheatley GH, 3rd, Nunez A, Preventza O, et al. Have we gone too far?: endovascular stent-graft repair of aortobronchial fistulas. J Thorac Cardiovasc Surg. 2007;133:1277–1285. doi: 10.1016/j.jtcvs.2006.11.066. [DOI] [PubMed] [Google Scholar]