Abstract
In Korea, the incidence of acute myocardial infarction has been increasing rapidly. Twelve-month clinical outcomes for 13,133 patients with acute myocardial infarction enrolled in the nationwide prospective Korea Acute Myocardial Infarction Registry study were analyzed according to the presence or absence of ST-segment elevation. Patients with ST-segment elevation myocardial infarction (STEMI) were younger, more likely to be men and smokers, and had poorer left ventricular function with a higher incidence of cardiac death compared to patients with non-ST-segment elevation myocardial infarction (NSTEMI). NSTEMI patients had a higher prevalence of 3-vessel and left main coronary artery disease with complex lesions, and were more likely to have co-morbidities. The in-hospital and 1-month survival rates were higher in NSTEMI patients than in STEMI patients. However, 12-month survival rates was not different between the two groups. In conclusion, NSTEMI patients have worse clinical outcomes than STEMI patients, and therefore should be treated more intensively during clinical follow-up.
Keywords: Myocardial infarction, Coronary artery disease, Prognosis
Introduction
The present study reveals 12-month clinical outcomes for 13,133 patients with acute myocardial infarction (AMI) who were enrolled in the nationwide prospective Korea Acute Myocardial Infarction Registry (KAMIR) between November 2005 and December 2007. Launched in November 2005, the KAMIR is the first nationwide, population based, multicenter data collection registry in Korea designed to track outcomes of patients presenting with AMI. The registry includes 52 community and teaching hospitals that enroll more than 10,000 patients annually. As of March 2009, the registry contained data on 21,871 patients. Centers included in the registry were chosen based on a careful evaluation of local demographics and care facilities. Since treatment decisions for patients included in the KAMIR are at the discretion of the patient's physician, data collected in the registry reflect a real-world approach to the diagnosis and treatment of AMI in Korea. The KAMIR is supported by a research grant from the Korean Society of Circulation in commemoration of its 50th Anniversary and aims to improve patient care by providing a greater understanding of patient management and outcomes in the rapidly evolving field of AMI treatment.
Recently in Korea the proportion of non-ST-segment elevation myocardial infarction (NSTEMI) has been increasing, compared with acute ST-segment elevation myocardial infarction (STEMI). We sought to evaluate differences between STEMI and NSTEMI in laboratory and clinical outcomes through the KAMIR in Korean patients.
Comparison of Clinical Outcomes Between ST-Segment Elevation Myocardial Infarction and Non-ST-Segment Elevation Myocardial Infarction
Patients entered into the registry were ≥18 years of age at the time of hospital presentation, had to be admitted with an AMI as the presumptive diagnosis, and had ≥1 of the following: electrocardiographic changes consistent with an AMI, serial increases in serum biochemical markers of myocardial necrosis, and/or documentation of coronary artery disease.
The primary clinical end point was the composite of major adverse cardiac events (MACE), including death from any cause, myocardial infarction, target vessel/lesion revascularization, and coronary artery bypass grafting (CABG) during a 12-month clinical follow-up.
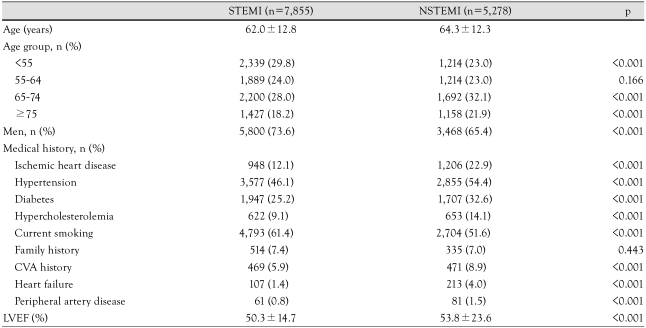
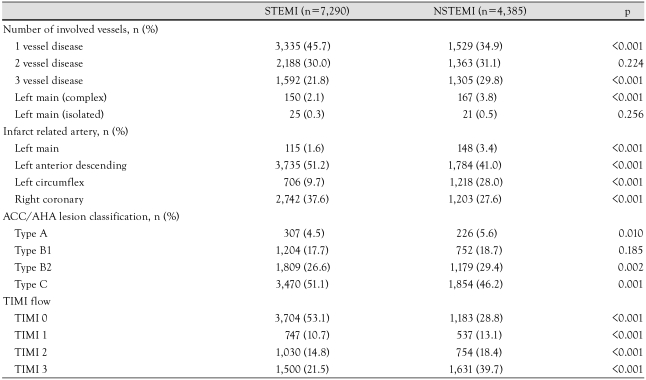
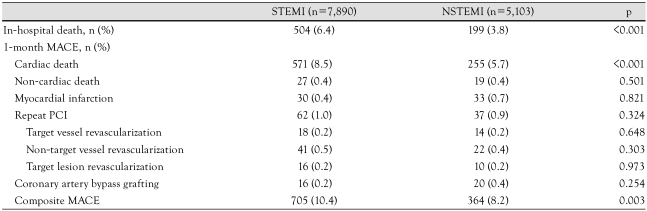
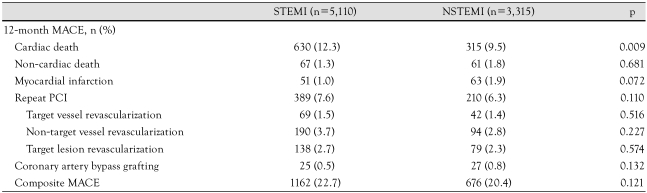
Characteristics were examined separately for STEMI and NSTEMI patients (Table 1 and 2). STEMI patients were younger, more likely to be men and smokers, and had poorer left ventricular function with a higher incidence of cardiac death, compared to NSTEMI patients (Table 3 and 4). NSTEMI patients had a higher prevalence of 3-vessel and left main coronary artery disease with complex lesions, and were more likely to have comorbidities (Table 1 and 2).
Table 1.
Baseline clinical characteristics
CVA: cerebrovascular accident, LVEF: left ventricular ejection fraction, STEMI: ST-segment elevation myocardial infarction, NSTEMI: non-ST-segment elevation myocardial infarction.
Table 2.
Coronary angiographic findings
STEMI: ST-segment elevation myocardial infarction, NSTEMI: non-ST-segment elevation myocardial infarction, ACC/AHA: American College of Cardiology/American Heart Association, TIMI: thrombolysis in myocardial infarction
Table 3.
In-hospital mortality and one-month MACEs
PCI: percutaneous coronary intervention, STEMI: ST-segment elevation myocardial infarction, NSTEMI: non-ST-segment elevation myocardial infarction, MACEs: major adverse cardiac events
Table 4.
Twelve-month MACEs
PCI: percutaneous coronary intervention, STEMI: ST-segment elevation myocardial infarction, NSTEMI: non-ST-segment elevation myocardial infarction, MACEs: major adverse cardiac events
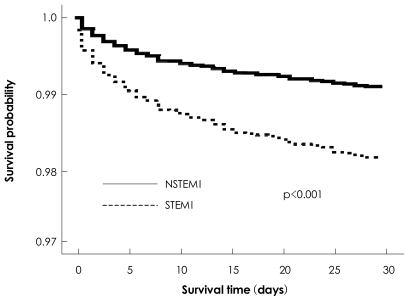
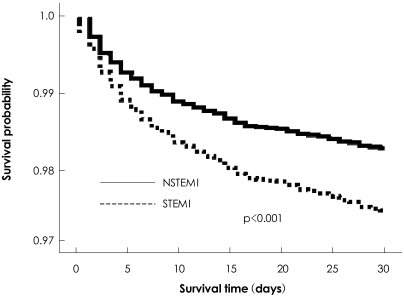
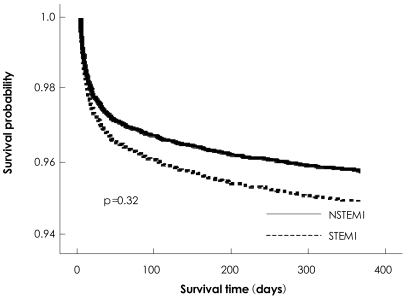
The in-hospital and 1-month survival rates were higher in patients with NSTEMI than in patients with STEMI (Figs. 1 and 2). However, 12-month survival rate was not different between patients with NSTEMI and STEMI (Fig. 3).
Fig. 1.
In-hospital survival rate was higher in non-ST-segment elevation myocardial infarction (NSTEMI) patients than in ST-segment elevation myocardial infarction (STEMI) patients.
Fig. 2.
One-month survival rate was higher in non-ST-segment elevation myocardial infarction (NSTEMI) patients than in ST-segment elevation myocardial infarction. (STEMI) patients.
Fig. 3.
Twelve-month survival rates were not different between non-ST-segment elevation myocardial infarction (NSTEMI) patients and ST-segment elevation myocardial infarction (STEMI) patients.
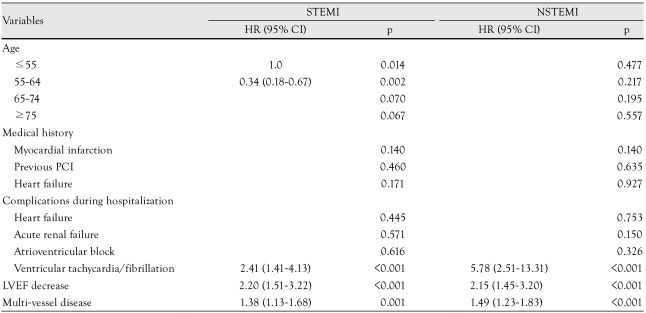
Predictors of mortality in STEMI patients during 12-month follow up were presence of ventricular tachycardia/fibrillation, decreased left ventricular function, multi-vessel disease, and age (Table 5). In NSTEMI patients, ventricular tachycardia/fibrillation, decreased left ventricular function, and multi-vessel disease were associated with 12-month all-cause mortality (Table 5).
Table 5.
Predictors of mortality during 12-month clinical follow-up in NSTEMI and STEMI patients
STEMI: ST-segment elevation myocardial infarction, NSTEMI: non-ST-segment elevation myocardial infarction, PCI: percutaneous coronary intervention, LVEF: left ventricular ejection fraction, HR: hazard ratio, CI: confidence interval
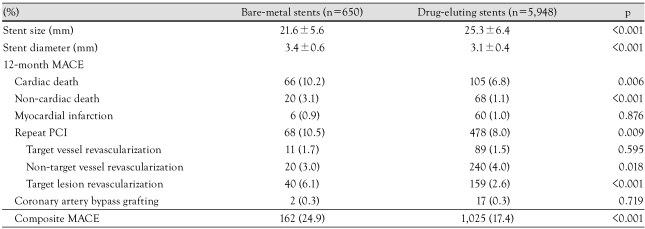
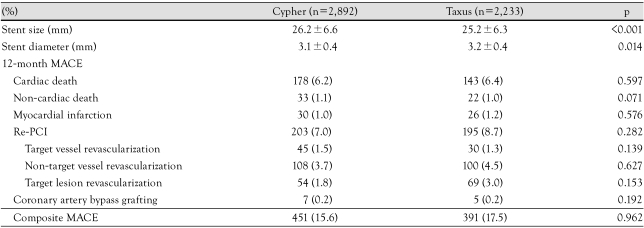
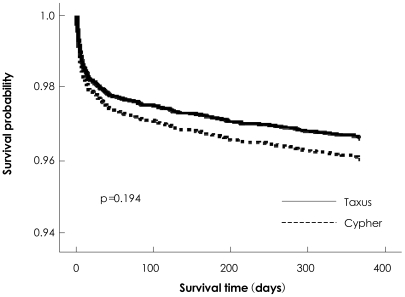
In both groups, a high percentage of patients received drug-eluting stents (DES), the outcomes of which were superior to those of bare-metal stents (BMS) with significantly lower rates of death and target lesion revascularization at 12-month follow-up (Table 6). Among patients who underwent DES implantation, 12-month clinical outcomes were similar between patients treated with sirolimus-eluting stents (Cypher stent, Cordis, Johnson & Johnson, Miami Lakes, FL, USA) and paclitaxel-eluting stents (Taxus stent, Boston Scientific Corp, Natick, MA, USA) (Table 7) (Fig. 4).
Table 6.
Twelve-month MACEs between bare-metal and drug-eluting stents
PCI: percutaneous coronary intervention, MACEs: major adverse cardiac events
Table 7.
Twelve-month MACEs between Cypher and Taxus stents
MACEs: major adverse cardiac events, PCI: percutaneous coronary intervention
Fig. 4.
Post-discharge survival at 12 months after implantation of Cypher and Taxus stents was not different between the two drug-eluting stents.
One of the main limitations of this study is that the proportion of patients followed up was relatively low with 63.0% at 6 months and 52.5% at 12 months. Although our follow-up rate was less than the rate typically observed in randomized trials, the characteristics of patients lost to follow-up were relatively similar to those remaining under observation.
Discussion
According to the KAMIR, the in-hospital survival rate was higher in NSTEMI patients than in STEMI patients. However, the 1-year survival rate was not different between the two groups, indicating that in the Korean population NSTEMI patients should be treated as intensively as STEMI patients during clinical follow-up.
The KAMIR study, launched in commemoration of the 50th anniversary of the Korean Society of Circulation, is the first large-scale, nationwide multicenter trial in Korea and has value in helping clinicians understand the real-world epidemiology and management status of AMI in the Korean population. Intensive follow-up and surveillance of the enrollees, as suggested above, is an essential requisite for the ultimate goal of the KAMIR, i.e., establishment of a validated prediction model for mortality risk and prognosis in patients with AMI.
Since its inception in 2005, this study has generated over 100 published papers and invited high-profile international conference presentations. So far, as many as 11 scientific papers have been published in leading international journals. Lee et al.1) proved that the rates of MACE and stent thrombosis at 6 months after discharge were not different between the two types of DES, i.e. Cypher and Taxus stents, indicating that DES can be safely used in patients with AMI. Song et al.2) reported that 1-month mortality was not associated with initial time variables to reperfusion, suggesting that patient prognosis may not depend on the initial treatment delay in the current practice of primary percutaneous coronary intervention (PCI) in Korea. Jeong et al.3) indicated that intensive pharmacologic treatment may improve short-term clinical outcomes in NSTEMI patients who were not indicated for PCI. Lee et al.4) reported that clinical outcomes were dependent on the status of estimated glomerular filtration rate (GFR) in patients who underwent invasive treatment. They also suggested that high waist-to hip ratio and underweight are mortality risk factors in STEMI patients.5) Lee et al.6) observed that the success rate of PCI for NSTEMI was lower and 1-month MACE for both STEMI and NSTEMI were higher in females than males, even though there was no gender difference in the initial treatment of strategy AMI. Kwon et al.7) reported that baseline N-terminal pro-B type natriuretic peptide (NT-proBNP) level was associated with shortterm mortality in STEMI patients who underwent primary PCI, and that NT-proBNP level on admission could be used as a prognostic factor in STEMI patients treated with primary PCI. Lee et al.8) reported that the incidence of AMI showed seasonal and monthly variations and that meteorological parameters had a significant influence on the occurrence of AMI, particularly in females and in patients of younger age. They also reported that predictors of 6-month MACE in 30-day survivors of AMI included body mass index, severity of left ventricular systolic dysfunction, residual myocardial ischemia, and electrical instability.9) Furthermore, Chen et al.10) demonstrated that triple anti-platelet including aspirin, clopidogrel, and cilostazol was superior to conventional dual anti-platelet therapy in preventing MACE without increasing bleeding complications in pa-tients with AMI undergoing PCI. Sim et al.11) evaluated the safety and benefit of early, elective PCI after thrombolytic therapy for AMI and reported that PCI within 48 hours of successful fibrinolysis was safe and more beneficial compared with PCI performed later. Cho et al.12) identified risk factors for AMI in young Korean patients. Lee et al.13) reported that hypertensive AMI patients with diabetes had worse prognoses than those without diabetes.
Analyses and research continue to the present day. The results have also provided impetus for a subsequent study, the Korea Working Group on Myocardial Infarction (KorMI). The KorMI, which is a continuation of the KAMIR, is an ongoing, open-ended registry that captures data on the complete spectrum of patients experiencing AMI, including long-term clinical follow-up. The KAMIR Scientific Committee and the Korean Society of Cardiology are actively discussing the transformation of the KorMI into a regular working group to ensure continuity and stability. It is the strong feeling of the KAMIR Scientific Committee that the KorMI should evolve into a regular society immediately, based on the success of the KAMIR from 2005 and on the fruitful results it has since achieved.
A clear understanding of the key messages the KAMIR delivers to the cardiology community will serve as a stepping stone to better care and treatment of AMI in the Korean population. The observation that hypertension and smoking were the most prevalent risk factors in the KAMIR population warrants establishing more aggressive management of hypertension and a more vigorous country-level campaign against cigarette smoking. In addition, it is mandatory to promote continuous public awareness about the importance of early access to treatment in order to reduce the time delay in seeking medical attention from the onset of perceived symptoms.
Conclusion
The number of patients surviving AMI is on a steady rise with the use of new drug therapies and non-drug interventions. Overall in-hospital mortality of AMI patients is about 5% in Korea. The proportion of NSTEMI patients is increasing and there is a growing need for intensive surveillance and rehabilitation programs, especially for this subset of AMI patients. The KAMIR, with continued expansion and successful growth, will make an invaluable contribution to the long-term care and monitoring of outcomes in Korean patients with AMI.
Footnotes
Korea Acute Myocardial Infarction (KAMIR) Investigators: Myung Ho Jeong, MD, Young Keun Ahn, MD, Shung Chull Chae, MD, Jong Hyun Kim, MD, Seung Ho Hur, MD, Young Jo Kim, MD, In Whan Seong, MD, Dong Hoon Choi, MD, Jei Keon Chae, MD, Taek Jong Hong, MD, Jae Young Rhew, MD, Doo Il Kim, MD, In Ho Chae, MD, Jung Han Yoon, MD, Bon Kwon Koo, MD, Byung Ok Kim, MD, Myoung Yong Lee, MD, Kee Sik Kim, MD, Jin Yong Hwang, MD, Myeong Chan Cho, MD, Seok Kyu Oh, MD, Nae Hee Lee, MD, Kyoung Tae Jeong, MD, Seung Jea Tahk, MD, Jang Ho Bae, MD, Seung Woon Rha, MD, Keum Soo Park, MD, Chong Jin Kim, MD, Kyoo Rok Han, MD, Tae Hoon Ahn, MD, Moo Hyun Kim, MD, Ki Bae Seung, MD, Wook Sung Chung, MD, Ju Young Yang, MD, Chong Yun Rhim, MD, Hyeon Cheol Gwon, MD, Seong Wook Park, MD, Young Youp Koh, MD, Seung Jae Joo, MD, Soo Joong Kim, MD, Dong Kyu Jin, MD, Jin Man Cho, MD, Yang Soo Jang, MD, Jeong Gwan Cho, MD and Seung Jung Park, MD
References
- 1.Lee SR, Jeong MH, Ahn YK, et al. Clinical safety of drug-eluting stents in the Korea acute myocardial infarction registry. Circ J. 2008;72:392–398. doi: 10.1253/circj.72.392. [DOI] [PubMed] [Google Scholar]
- 2.Song YB, Hahn JY, Gwon HC, Kim JH, Lee SH, Jeong MH. The impact of initial treatment delay using primary angioplasty on mortality among patients with acute myocardial infarction: from the Korea acute myocardial infarction registry. J Korean Med Sci. 2008;23:357–364. doi: 10.3346/jkms.2008.23.3.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeong HC, Ahn YK, Jeong MH, et al. Intensive pharmacologic treatment in patients with acute non ST-segment elevation myocardial infarction who did not undergo percutaneous coronary intervention. Circ J. 2008;72:1403–1409. doi: 10.1253/circj.cj-08-0048. [DOI] [PubMed] [Google Scholar]
- 4.Lee SH, Kim YJ, Kim W, et al. Clinical outcomes and therapeutic strategy in patients with acute myocardial infarction according to renal function: data from the Korean Acute Myocardial Infarction Registry. Circ J. 2008;72:1410–1418. doi: 10.1253/circj.cj-08-0088. [DOI] [PubMed] [Google Scholar]
- 5.Lee SH, Park JS, Kim W, et al. Impact of body mass index and waist-to-hip ratio on clinical outcomes in patients with ST-segment elevation acute myocardial infarction (from the Korean Acute Myocardial Infarction Registry) Am J Cardiol. 2008;102:957–965. doi: 10.1016/j.amjcard.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 6.Lee KH, Jeong MH, Ahn YK, et al. Gender differences of success rate of percutaneous coronary intervention and short term cardiac events in Korea Acute Myocardial Infarction Registry. Int J Cardiol. 2008;130:227–234. doi: 10.1016/j.ijcard.2007.08.044. [DOI] [PubMed] [Google Scholar]
- 7.Kwon TG, Bae JH, Jeong MH, et al. N-terminal pro-B-type natriuretic peptide is associated with adverse short-term clinical outcomes in patients with acute ST-elevation myocardial infarction underwent primary percutaneous coronary intervention. Int J Cardiol. 2009;133:173–178. doi: 10.1016/j.ijcard.2007.12.022. [DOI] [PubMed] [Google Scholar]
- 8.Lee JH, Chae SC, Yang DH, et al. Influence of weather on daily hospital admissions for acute myocardial infarction (from the Korea Acute Myocardial Infarction Registry) Int J Cardiol. 2009 doi: 10.1016/j.ijcard.2009.03.122. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Lee JH, Park HS, Chae SC, et al. Predictors of six-month Major adverse cardiac events in 30-day survivors after acute myocardial infarction (from the Korea Acute Myocardial Infarction Registry) Am J Cardiol. 2009;104:182–189. doi: 10.1016/j.amjcard.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 10.Chen KY, Rha SW, Li YJ, et al. Triple versus dual anti-platelet therapy in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Circulation. 2009;119:3168–3170. doi: 10.1161/CIRCULATIONAHA.108.822791. [DOI] [PubMed] [Google Scholar]
- 11.Sim DS, Jeong MH, Ahn YK, et al. Safety and benefit of early elective percutaneous coronary intervention after successful thrombolytic therapy for acute myocardial infarction. Am J Cardiol. 2009;103:1333–1338. doi: 10.1016/j.amjcard.2009.01.339. [DOI] [PubMed] [Google Scholar]
- 12.Cho JY, Jeong MH, Ahn YK, et al. Predictive factors of major adverse cardiac events and clinical outcomes of acute myocardial infarction in young Korean patients. Korean Circ J. 2008;38:161–169. [Google Scholar]
- 13.Lee MG, Jeong MH, Ahn YK, et al. Comparison of clinical outcomes in hypertensive patients with acute myocardial infarction according to the presence of diabetes. Korean Circ J. 2009;39:243–250. doi: 10.4070/kcj.2009.39.6.243. [DOI] [PMC free article] [PubMed] [Google Scholar]