Abstract
Background
A single nucleotide polymorphism on chromosome 9p21, rs10757274 (9p21 allele), has been shown to predict coronary heart disease (CHD) in whites. We evaluated whether adding the 9p21 allele to traditional risk factors (RF) improved CHD risk prediction in whites from the Atherosclerosis Risk in Communities (ARIC) study, and whether changes in risk prediction would modify lipid therapy recommendations.
Methods and Results
Whites (n=9,998) in the ARIC study for whom the 9p21 genotype and traditional RF information was available were included. Using Cox proportional hazards models, the ARIC Cardiovascular Risk Score (ACRS) which is based on traditional RF, was determined. A total of 1,349 individuals (13.5%) developed incident CHD events during a period of 14.6 years. Adding the 9p21 allele to traditional RF was associated with hazard ratio (HR) of incident CHD of 1.2 per allele (p<0.000003) and a significant increase in the area under the curve of the receiver operating characteristic from 0.782 to 0.786 (95% CI= [0.001, 0.007]). The 9p21 allele’s greatest influence to the ACRS was observed in the intermediate-low (>5% to ≤10% 10-year CHD risk) and intermediate-high (>10% to ≤20% 10-year CHD risk) categories with 12.1% and 12.6% reclassified, respectively. This may impact therapy since 90% of these reclassified individuals had LDL-C>100 mg/dL.
Conclusion
Adding the 9p21 allele to traditional RF in whites in the ARIC study modestly improved CHD risk prediction in the intermediate categories.
Keywords: genetics, heart disease, risk factors, lipids
Introduction
Although coronary heart disease (CHD) is the leading cause of death in the western world, a large number of CHD events could be avoided if risk factors could be modified in the whole population (population approach) or if individuals with increased risk for CHD were identified and appropriately treated through lifestyle modification and/or drug therapy aimed at risk factor modification (high-risk individual approach).1 A fundamental concept in all national guidelines is matching the intensity of risk factor modification to the individual’s risk probability for developing a CHD event. Therefore, the stratification of CHD risk is a key initial step in order to target therapies for CHD prevention. Large population studies, such as the Framingham Heart Study and Atherosclerosis Risk in Communities (ARIC) study have been used to develop a “risk score,” which includes traditional risk factors (RF) such as age, gender, total cholesterol, systolic blood pressure, high-density lipoprotein cholesterol (HDL-C), and smoking. The Framingham risk score serves as the basis for the risk assessment algorithm proposed by the widely-accepted Adult Treatment Panel (ATP) III guidelines.1, 2 Treatment modalities, including lifestyle modification and lipid-lowering agents, are based on the calculated ATP III risk.
Recent application of genome-wide association studies (GWAS) has accelerated the pace of gene discovery for CHD.3 Two recently reported single nucleotide polymorphisms (SNPs) in the 58-kilobase interval on chromosome 9p21, have been shown to be associated with CHD in the white participants of multiple large cohorts.4–6 Rs10757274 and rs2383206 define a single allele and were found to be associated with an estimated 20% increase in CHD risk in heterozygotes and 40% increase in CHD risk in homozygotes. However, the practical application of this new genomic information by practicing physicians remains uncertain.7
In this study, we used the ARIC Cardiovascular Risk Score (ACRS), which presents a quantitative approach for global risk assessment based on traditional RF for CHD. We hypothesize that adding the 9p21 allele to the model using traditional RF will result in a statistically significant improvement of overall prediction for CHD, and in the shifting of a significant number of subjects from one risk category to another. This, in turn, may result in a change of treatment recommendation by either altering the decision to begin pharmacotherapy or changing the goal of therapy.
Methods
The study sample was chosen from the large, ongoing Atherosclerosis Risk in Communities (ARIC) study which included 15,792 US individuals aged 45–64 years at recruitment (1987–1989) who were followed for the development of clinical CHD or other vascular events. A full description of the ARIC study design and methods has been published previously.8, 9
Of the 15,792 individuals initially enrolled in the ARIC study, we excluded individuals who had prevalent CHD or stroke at the baseline ARIC study visit (1987–89) and individuals with missing CHD prevalence data (1,446 individuals), those who belonged to any race group other than “white” (3,918 individuals), participants with missing information on risk factors (including age, gender, systolic blood pressure, antihypertensive medication use, diabetes, total cholesterol, HDL-C, and current tobacco use/smoking), those missing rs10757274 (9p21 allele) genotype information (423 individuals), and those who withdrew consent for the use or storage of their DNA (7 individuals). A total of 9,998 white participants for whom the ARIC risk score was calculated at the baseline visit were eligible for the analysis presented here.
Incident CHD events were determined by annually contacting each participant in the study population and reviewing hospital discharge lists and death certificates for incident CHD events. Follow up time was determined as the interval between the date of the first clinical visit and the date of the first CHD event, death or end of follow up on December 31, 2004. Detailed descriptions of quality assurance for ascertainment and classification of CHD events have been published previously.9 A CHD event was defined as definite or probable myocardial infarction, a silent myocardial infarction between examinations (indicated by electrocardiogram), a definite CHD death, or a coronary revascularization.
Blood pressure measurements were performed 3 times with the participant seated with a random-zero sphygmomanometer, and the last 2 measurements were averaged. Questionnaires were administered to assess current use of antihypertensive medication. Plasma total cholesterol was measured by an enzymatic method,10 while HDL-C was measured after dextran-magnesium precipitation of non–high-density lipoproteins.11 Diabetes was defined as a fasting glucose level ≥126 mg/dL or a nonfasting glucose level ≥200 mg/dL, or a self-reported physician diagnosis of diabetes or use of diabetic medication. Cigarette smoking status was classified as current or not current.
Statistical Methods
Baseline population characteristics of the 10,004 white individuals eligible for this study were compared across 9p21 genotypes using ANOVA for the continuous variables (age, BMI, blood pressure, etc.) and chi-square contingency table for the categorical variables. Analysis of incident CHD was carried-out using Cox proportional hazards modeling of time-to-event. All eligible subjects, as described above, were scored according to the ARIC Cardiovascular Risk Score (ACRS) which is based on the following: age, gender, smoking, diabetes, systolic blood pressure, antihypertensive medication use, total cholesterol and HDL-C.12 Each subject was evaluated by Cox proportional hazards model for time-to-incident CHD, and this calculation was completed for the entire white population. As covariates representing traditional RF used in the Cox proportional hazards model, we used age, gender, smoking, diabetes, systolic blood pressure, antihypertensive medication use, total cholesterol and HDL-C. For each covariate a beta-coefficient was determined by regression analysis. These coefficients were then used to construct the ACRS that is based on traditional RF only. The ACRS was then calculated for each subject by multiplying each model coefficient by the subject’s associated risk-variable value and then deriving the predicted 10-year CHD risk. A separate calculation was performed to determine the beta-coefficient for each of the traditional RF and the 9p21 genotype information variables. These beta-coefficients were then used to construct an ACRS which includes the 9p21 information. A second calculation of the ACRS was performed after adding the 9p21 allele. A value of 1, 0, and −1 was given for the genotypes GG, AG, AA, of the rs10757274, respectively. The area under curve of the receiver operating characteristic (AROC) was calculated for each model, one with traditional RF alone (ACRS) and one with the 9p21 allele added to traditional RF (ACRS+9p21).
The beta-coefficients for each model (with and without the 9p21 allele) were determined separately using the same dataset. This enabled direct comparison between the two models.
Classification of participants with and without adding the 9p21 allele was performed by first classifying each individual by traditional RF-only (ACRS or Framingham risk score [FRS]) into the following risk categories: low (0–5% 10-year CHD risk), intermediate-low (>5% to ≤10% 10-year CHD risk), intermediate-high (>10% to ≤20% 10-year CHD risk), and high (>20% 10-year CHD risk). The same classification process was then repeated with the addition of the 9p21 allele to the ACRS. We then used the net reclassification index (NRI)13 to examine correct movement between risk categories after adding the 9p21 allele in the ACRS model. Both the total NRI and clinical NRI (NRI for intermediate-risk [>5% to ≤10% and >10% to ≤20% 10-year CHD risk] categories only) were preformed as recently suggested.14 NRI calculations were preformed taking into account censored data at a time point of 10 years. The integrated discrimination index (IDI) which examines model performance independent of risk categories choice was also calculated.13 Calculations of IDI, and NRI were completed for events before a defined follow-up period and accounted for censoring by rewriting the formula in terms of the survival function, using Bayes' Law and then using survival analysis methods to estimate the survival function while accounting for censoring.
A baseline LDL-C level for study participants in the intermediate-low (>5% to ≤10%) and intermediate-high (>10% to ≤20%) 10-year CHD risk groups was also examined, as calculated by traditional RF alone (ACRS without 9p21 allele). The proportion of individuals that were reclassified to different risk categories after adding the 9p21 allele information to the ACRS calculation, along with their LDL-C levels, were determined. The 10-year CHD event rate was determined according to the Kaplan-Meier survival curve for 10-year incident CHD per 100 individuals.
Because most physicians use the Framingham risk score (FRS) in clinical practice and it does not differ significantly from the ACRS for white men (and is similar for white women15), we also calculated the FRS for each ARIC participant based on age, gender, smoking, systolic blood pressure, antihypertensive medication use, total cholesterol and HDL-C as covariates.16 For each covariate, a beta-coefficient was determined by regression analysis in a way that was similar to the analysis for the ACRS described above. A second calculation of the FRS was performed after including the 9p21 allele. A value of 1, 0, and −1 was given for the genotypes GG, AG, AA, of the rs10757274, respectively. NRI and IDI were then calculated for the FRS based reclassification. .
We further calculated the Grønnesby-Borgan statistic, an overall goodness-of-fit test for the Cox proportional hazards model.
Results
Baseline characteristics of the 9,998 white participants in ARIC who were eligible for the study and classified according to the 9p21 genotype are presented in Supplemental Table 1. As previously reported, we observed no association between the 9p21 genotype and traditional RF. However, there was a significant association (P=0.014) between lower body mass index (BMI) and the AG/GG genotype in ARIC. Supplemental Table 2 shows the baseline characteristics of the ARIC white population in relation to the development of incident CHD. As expected, a significant difference was observed for the traditional RF and other risk factors between incident CHD cases and noncases.
The frequencies of the G and A alleles for the entire study population were 0.49 and 0.51, respectively. There was no significant difference (P=0.37) in the G allele frequency between men (0.48) and women (0.49). A significantly higher frequency of the G allele was found in the CHD cases (0.52) than noncases (0.48), P=0.0017. The GG genotype was more frequent in cases (26.2%) than noncases (23.4%), P<0.002 (Supplemental Table 2).
Of the 9,998 subjects eligible for the study followed for 14.6 years, 1,349 (13.5%) developed an incident CHD event. The hazard ratio (HR) for the 9p21 allele with only age and gender as covariates was 1.17 (P=4.705 E-05). After taking into account traditional RF and ACRS model covariates, the 9p21 allele was still significantly associated with incident CHD with a HR of 1.20 (P<3E-06). The HR for CHD-related procedures was 1.22 (P<5E-06); the HR for MI (either fatal or non fatal) and fatal CHD was 1.20 (P<0.0004).
When calculated for the traditional RF-only (ACRS–only: age, gender, systolic blood pressure, total cholesterol, HDL-C, antihypertensive medication, diabetes and smoking), the area under the curve of the receiver operating characteristic (AROC) for incident CHD was 0.782 for the entire cohort. Adding the 9p21 allele increased the AUC to 0.786 (95% confidence interval [0.001, 0.007]). Furthermore, in evaluating the goodness-of-fit, the 9p21 allele + traditional RF model did better than the traditional RF-only model using the Grønnesby-Borgan test (see Supplemental Table 4). However, both models did not demonstrate good fit.
Reclassification
When the 9p21 allele was added to traditional RF, 12–13% in the intermediate-low (>5% to ≤10% 10-year risk) and intermediate-high (>10% to ≤20% 10-year risk) categories were reclassified in both ACRS and FRS models.
All of the individuals reclassified were placed into adjacent risk groups, the immediately higher or lower risk category. Table 1 and 2 describe the resulting risk reclassification after adding the 9p21 allele to the ACRS and FRS, respectively.
Table 1.
Reclassification of the different ARIC Cardiovascular Risk Score (ACRS) categories after adding the 9p21 allele to the traditional risk factors
| Classification Using ACRS + 9p21 Allele | ||||||
|---|---|---|---|---|---|---|
| Classification using ACRS alone |
0–5% | >5% to ≤10% |
>10% to ≤20% |
>20% | Total number reclassified for category |
|
| (percent of total cohort) |
Low | Intermediate -low |
Intermediate -high |
High | ||
| 10-year CHD Risk Category |
(%*) | (%*) | (%*) | (%*) | (%*) | |
| 0–5% Low | 4,617 | 4,460 | 157 | 0 | 0 | 157 |
| (3.4) | (3.4) | |||||
| Observed event rate† | 1.6 | 3.3 | 0 | 0 | 1.6 | |
| >5% to ≤10% | 2,763 | 188 | 2,429 | 146 | 0 | 334 |
|
Intermediate- Low |
(6.8) | (5.3) | (12.1) | |||
| Observed event rate | 2.7 | 8.0 | 11.4 | 0 | 7.8 | |
| >10% to ≤20% | 1,992 | 0 | 160 | 1,741 | 91 | 251 |
|
Intermediate- High |
(8) | (4.6) | (12.6) | |||
| Observed event rate | 0 | 11.5 | 14.8 | 21.2 | 14.8 | |
| >20% High | 626 | 0 | 0 | 66 | 560 | 66 |
| (10.5) | (10.5) | |||||
| Observed event rate | 20.5 | 30.0 | 29.0 | |||
| TOTAL | 9,998 | 4,648 | 2,746 | 1,953 | 651 | |
| Observed event rate | 1,349 | 1.6 | 7.9 | 14.7 | 28.8 | 7.6 |
Percentage of individuals reclassified from traditional risk factor based risk model after adding 9p21 allele to risk calculation.
Observed 10-year rate event rate calculation is based on Kaplan-Meier survival curve at 10 years per a 100 individuals
Table 2.
Reclassification of the different Framingham Risk Score (FRS) categories after adding the 9p21 allele to the traditional risk factors
| Classification Using ACRS + 9p21 Allele | ||||||
|---|---|---|---|---|---|---|
| Classification using ACRS alone |
0–5% | >5% to ≤10% |
>10% to ≤20% |
>20% | Total number reclassified for category |
|
| (percent of total cohort) |
Low | Intermediate -low |
Intermediate -high |
High | ||
| 10-year CHD Risk Category |
(%*) | (%*) | (%*) | (%*) | (%*) | |
| 0–5% Low | 4,691 | 4,581 | 110 | 0 | 0 | 110 |
| (2.3) | (2.3) | |||||
| Observed event rate† | 1.7 | 8.5 | 0 | 0 | 1.9 | |
| >5% to ≤10% | 2,483 | 148 | 2,155 | 180 | 0 | 328 |
|
Intermediate- Low |
(6.0) | (7.2) | (13.2) | |||
| Observed event rate | 4.1 | 6.9 | 12.1 | 0 | 7.1 | |
| >10% to ≤20% | 2,159 | 0 | 186 | 1,867 | 106 | 292 |
|
Intermediate- High |
(8.6) | (4.9) | (13.5) | |||
| Observed event rate | 0 | 10.8 | 14.5 | 21.6 | 14.5 | |
| >20% High | 665 | 0 | 0 | 82 | 583 | 82 |
| (12.3) | (12.3) | |||||
| Observed event rate | 24.6 | 28.9 | 28.4 | |||
| TOTAL | 9,998 | 4,648 | 2,746 | 1,953 | 651 | |
| Observed event rate | 1,349 | 1.8 | 7.3 | 14.7 | 27.8 | 7.6 |
Percentage of individuals reclassified from traditional risk factor based risk model after adding 9p21 allele to risk calculation.
Observed 10-year rate event rate calculation is based on Kaplan-Meier survival curve at 10 years (% failure)
The ACRS total NRI after adding the 9p21 allele showed minimal change (0.8% improvement, P=0.31) that was not statistically significant. The clinical NRI was 6.2% which was statistically significant (P = 0.03). The IDI was 0.002 which was statistically significant (P<0.015). The clinical NRI and IDI for the FRS model were 6.8% and 0.021 respectively.
From the ACRS high group (>20% 10-year risk), 66 (10.5%) individuals were reclassified down to the intermediate-high category. For these individuals, although reclassified to a lower risk group, after adding 9p21 genotype information, it would seem reasonable not to change treatment since they already have considerable risk from traditional RF. From the low-risk group (0–5% 10-year risk), only 157 (3.4%) were reclassified to the intermediate-low risk category. According to ATP III guideline, these subjects do not change risk category, and therefore, no treatment change would be recommended for them.
The Adult Treatment Panel (ATP) III update published in 2004 recommends an optional target LDL-C goal of <100 mg/dL for the >10% to ≤20% 10-year CHD risk group, especially in the presence of abnormal “emerging” risk factors.17 We evaluated the baseline LDL-C distribution in the >5% to ≤10% (intermediate-low) and >10% to ≤20% (intermediate-high) 10-year CHD risk groups based on traditional RF, prior to reclassification (Table 3). In the intermediate-high group (>10% to ≤20% 10-year CHD risk), based on traditional RF alone, 94.1% of subjects had LDL-C ≥100 mg/dL, which is above the optimal LDL-C target level by the updated ATP III recommendation. In the intermediate-low category (>5% to ≤10% 10-year risk), based on traditional RF alone, 89.3% of subjects had LDL-C levels ≥100 mg/dL.
Table 3.
Distribution of LDL-C in the intermediate-low and intermediate-high risk categories according to traditional risk factors, prior to reclassification (Risk categories calculated based on traditional risk factor-only model)
| 10-year CHD risk | ||
|---|---|---|
| >10% to ≤20% | ||
| >5% to ≤10% | ||
| Intermediate- low |
Intermediate- high |
|
| LDL-C in mg/dL | Total n=2742 % (n) |
Total n=1928 % (n) |
| <100 | 10.7 (293) | 5.9 (113) |
| 100–129 | 27.6 (757) | 17.6 (340) |
| ≥130 | 61.7 (1692) | 76.5 (1475) |
| ≥ 130–159 | 32.1 (880) | 36.9 (712) |
| ≥ 160 | 29.6 (812) | 39.6 (763) |
The majority of individuals who were reclassified from the intermediate-low group (>5% to ≤10% 10-year risk) and intermediate-high group (>10% to ≤20% 10-year risk) had LDL-C levels above optimal. The decision regarding lifestyle modification, initiation of drug therapy, or the target goal of therapy may be clarified by adding the 9p21 genotype information, and a more detailed discussion of how reclassification may alter clinical decisions is provided in the Electronic Supplement and Supplemental Table 3.
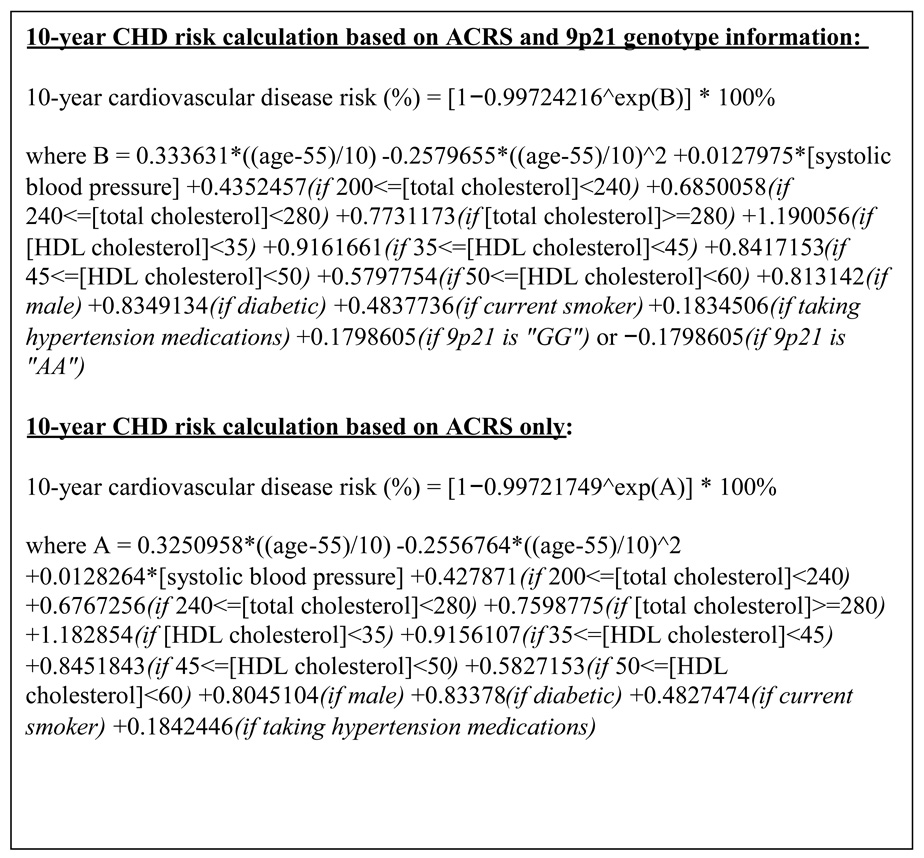
The case examples in Table 4 demonstrate the practical clinical implication (which is further expanded in the Supplement) of the 9p21 genotype for individuals in the intermediate-low and intermediate-high risk groups. The formulas which were used for the calculation of 10-year CHD risk based on ACRS only and ACRS + 9p21 genotype information are detailed in Figure 1.
Table 4.
Case examples for adding 9p21 genotype to traditional risk factors based ARIC Cardiovascular Risk Score (ACRS) risk model
| Subject # | 1 | 1 | 1 | 2 | 2 | 2 |
|---|---|---|---|---|---|---|
| Sex | Male | Male | Male | Female | Female | Female |
| Age | 51 | 51 | 51 | 55 | 55 | 55 |
| Current smoking | No | No | No | Yes | Yes | Yes |
| Total cholesterol (mg/dL) |
200 | 200 | 200 | 240 | 240 | 240 |
| HDL-C (mg/dL) | 40 | 40 | 40 | 40 | 40 | 40 |
| LDL-C (mg/dL) | 135 | 135 | 135 | 150 | 150 | 150 |
| Family history | No | No | No | No | No | No |
| Antihypertensive medication use |
No | No | No | Yes | Yes | Yes |
| Systolic blood pressure (mm Hg) |
120 | 120 | 120 | 155 | 155 | 155 |
| Diabetes mellitus |
No | No | No | No | No | No |
| ACRS risk (%) | 9.0 | 9.0 | 9.0 | 17.7 | 17.7 | 17.7 |
| 9p21 genotype | AA | AG | GG | AA | AG | GG |
|
ACRS+9p21 risk (%) |
7.5 | 9.0 | 10.6 | 15.0 | 17.6 | 20.7 |
Figure 1.
10-year CHD risk calculation based on ACRS and 9p21 genotype information & 10-year CHD risk calculation based on ACRS only.
Reclassification from the intermediate-low (>5% to ≤10% 10-year risk) category in the ACRS model
Subject 1 (Table 4) is a male with an initial 10-year CHD risk of 9.0% and LDL-C level of 135 mg/dL. According to ATP III guidelines, in an individual with <10% 10-year risk and 2 risk factors (in this case, male age ≥45 and HDL-C <40 mg/dL), one considers initiation of drug therapy if LDL-C ≥160 mg/dL with a LDL-C goal of <130 mg/dL. Adding the 9p21 genotype to traditional RF will increase, decrease or have no major influence on his 10-year CHD risk to 10.6%, 7.5%, and 9.0%, respectively. In the case of the GG genotype increasing his risk to 10.3%, the ATP III guidelines would recommend drug therapy initiation at LDL-C levels ≥130 mg/dL, and target LDL-C goal <130 mg/dL with an optional target LDL-C goal <100 mg/dL.
Reclassification from the intermediate-high (>10% to ≤20% 10-year risk) category in the ACRS model
Subject 2 (Table 4) is a female with an initial 10-year CHD risk of 17.7% and LDL-C level of 150 mg/dL. According to ATP III guidelines, she would be placed in the >10% to ≤20% 10-year risk with at least 2 risk factors (in this case, female age ≥55 and hypertensive medication use), and initiation of drug therapy would be recommended at LDL-C ≥130 mg/dL, with a LDL-C goal <130 mg/dL and an optional target LDL-C goal <100 mg/dL. Adding the 9p21 GG genotype to traditional RF will increase her 10-year CHD risk to 20.7%, changing the recommendation for therapy initiation to LDL-C ≥100 mg/dL and target goal to LDL-C <100 mg/dL.
Discussion
In this study, we demonstrated that adding the 9p21 genotype to traditional RF statistically significantly improved CHD risk prediction, with 12–13% of individuals reclassified in the intermediate-low and intermediate-high risk categories of both the ACRS and FRS models. For a large proportion of those reclassified, LDL-C target goals would be altered and thus, therapy recommendations would be changed. We present a simple way to utilize the 9p21 information for calculating the 10-year CHD risk for an individual based on the formula detailed in Figure 1.
The use of traditional risk factors to predict CHD risk is a well-established clinical tool. The ATP III CHD risk classification is generally accepted by most clinicians as a guideline for both risk prediction and for determining preventive therapy for CHD. Adding certain biomarkers to risk prediction calculations has been shown to modestly improve CHD risk prediction.18, 19 However, in recent years, extensive research has concentrated on associations between genetic markers and CHD.3
In this study, the 9p21 genotype had no association with blood pressure, lipid levels or other traditional RF. A modest association between the GG genotype and a lower BMI was observed in ARIC whites, but this observation has not been replicated in other studies.6 However, the AG/GG genotype’s possible tendency towards a lower BMI would not explain an increased risk for CHD.
The 9p21 variant had a HR of 1.20 per allele (P<3E-06). in ARIC whites, and adding the 9p21 allele to the traditional RF model resulted in a statistically significant improvement of the AROC. In a study by Talmud et al, although the AROC was modestly larger for 10-year risk prediction by adding the 9p21 genotype to traditional RF, it was not statistically significant.6 The statistically significant improvement in the AROC in our study may be related to the larger number of participants (9,998 vs. 2,742) or to the fact that we were examining both men and women vs. men only.6 In the study by Paynter et al, conducted on 22,129 white females, there was no significant improvement in C-statistics in either an ATP III-based risk model or the Reynolds score. The total NRI for the ATP III-based risk score was modestly better (2.7% improvement, P=0.02) after adding the 9p21 allele, and the clinical NRI was not calculated for that model.20
Although the total NRI in our study, which specifically examines correct movement between risk categories, did not show significant improvement between the model with and without the 9p21 allele, the clinical NRI, which examines the intermediate-risk categories in particular, was significantly better for the 9p21 allele model. The clinical NRI results may be useful, because the individuals in the intermediate-risk categories would most benefit from clarifying their risk status by testing “emerging” risk factors, such as the 9p21 allele.
The IDI, which examines improvement in model performance independent of choice of risk categories, was also significantly better for the model with the 9p21 allele. In evaluating the goodness-of-fit, the 9p21 allele + traditional RF model did better than the traditional RF-only model using the Grønnesby-Borgan test. However, both models did not provide a good fit.
The fact that adding the 9p21 allele to the ACRS model had the highest effect on the intermediate-low (~12% reclassified) and intermediate-high (~12% reclassified) risk categories is useful because patients in these “middle” categories are usually the most challenging for clinical evaluation. ATP III guidelines and other guidelines recommend consideration of additional testing, such as imaging and biomarkers, for the >10% to ≤20% 10-year risk group to aid in clinical evaluation and therapeutic strategy.21–23 We suggest that the 9p21 allele genotype may serve as one of these additional modalities.
Although the ATP III guidelines focus on >10% to ≤20% 10-year CHD risk as an intermediate-low risk category, others have expanded this category to either 6–20% or 5–20%.18, 24, 25 In the current study, another consideration for expanding to 5–20% risk category is that the 10-year absolute CHD risk dramatically underestimates the lifetime risk for CHD events. For example, individuals from the intermediate-low category (>5% to ≤10% 10-year risk) who were reclassified to the intermediate-high category (>10% to ≤20% 10-year risk), by adding the 9p21 genotype to the traditional RF model, had an 11.4 CHD event rate per 100 individuals over 10 years of follow up. However, a longer follow up period of 14.6 years in ARIC for the same reclassified population showed a much higher event rate of 19.6 CHD events per 100 individuals. This demonstrated the potential advantage of adding 9p21 testing to traditional RF in defining a group of individuals who would especially benefit from longterm preventive therapy.
In contrast to the intermediate-low and intermediate-high risk groups, the utility of the 9p21 genotype for risk calculation for subjects in the low (0–5% 10-year CHD risk) and high (>20 10-year CHD risk) categories is unclear. In both risk categories, few subjects were reclassified, and for those who were reclassified, no treatment change would seem appropriate.
In summary, we have shown that the 9p21 genotype added to traditional risk factors modestly improved risk classification in the intermediate-low (>5% to ≤10% 10-year CHD risk) and intermediate-high (>10% to ≤20% 10-year CHD risk) categories.. Future studies should be designed to test whether a strategy of altering therapy by virtue of a single SNP or combination of SNP’s could improve clinical outcome.
Limitations
The 9p21 allele association with CHD events has been shown in multiple cohorts in whites but was not demonstrated in blacks. Thus, the black population of the ARIC study was not included in this analysis. Although there are reports of association between the 9p21 allele and CHD in ethnicities other than whites and blacks, most of these reports include a relatively small number of participants, and further studies are required for verification.26 The ARIC study includes a relatively small number of individuals of ethnicities other than whites and blacks which did not supply enough statistical power to test our hypothesis in these populations. The fact that no other ethnicities other than whites were used for the current analysis, suggests that the results may not be generalized to other populations other than those like the one tested.
Another limitation is the use of a single SNP vs. the use of several SNPs which could have augmented the results of the current analysis. Finally, we did not examine the question of whether the 9p21 allele provided additional information to improve risk assessment if newer biomarkers such as high-sensitivity C-reactive protein, or imaging tests for subclinical atherosclerosis such as carotid intima-media thickness, are included in the multivariate models, and this needs to be addressed in future studies.
In recent years, multiple studies have identified a large number of single nucleotide polymorphisms (SNP’s) associated with coronary heart disease (CHD). Although many of these genetic markers are available commercially, their clinical utility and the appropriate populations for testing are largely unclear. In the current study, we examined the clinical utility of a single SNP in the 9p21 region, which was associated with CHD in multiple studies to address the questions noted above.
Addition of the 9p21 allele to traditional risk factors (RF) modestly improved the 10-year CHD risk prediction in the intermediate risk groups (defined as absolute 10-year CHD risk of 5–20%). Reclassification of an individual from the intermediate risk category to either a lower or higher CHD risk group may influence management base on Adult Treatment Panel (ATP) III guidelines. On the other hand, adding the 9p21 allele to traditional RF for individuals in the low (10-year risk <5%) or high-risk (10-year risk >20%) groups did not demonstrate clinical utility in this study.
In summary, this study demonstrates the clinical utility of adding the 9p21 allele to traditional RF when limited to individuals in the intermediate CHD risk categories. Future studies should be designed to test whether a strategy of altering therapy by virtue of adding a single or combination of SNPs to CHD risk prediction algorithms could improve clinical outcomes.
Supplementary Material
Acknowledgments
The authors thank the staff and participants of the ARIC study for their important contributions. The authors acknowledge the editorial assistance of Joanna Brooks, BA.
Funding Sources
The ARIC Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts N01-HC-55015, N01-HC-55016, N01-HC-55018, N01-HC-55019, N01-HC-55020, N01-HC-55021, and N01-HC-55022.
Footnotes
Disclosures:
None
References
- 1.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 2.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 3.Samani NJ, Erdmann J, Hall AS, Hengstenberg C, Mangino M, Mayer B, Dixon RJ, Meitinger T, Braund P, Wichmann HE, Barrett JH, Konig IR, Stevens SE, Szymczak S, Tregouet DA, Iles MM, Pahlke F, Pollard H, Lieb W, Cambien F, Fischer M, Ouwehand W, Blankenberg S, Balmforth AJ, Baessler A, Ball SG, Strom TM, Braenne I, Gieger C, Deloukas P, Tobin MD, Ziegler A, Thompson JR, Schunkert H. Genomewide association analysis of coronary artery disease. N Engl J Med. 2007;357:443–453. doi: 10.1056/NEJMoa072366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McPherson R, Pertsemlidis A, Kavaslar N, Stewart A, Roberts R, Cox DR, Hinds DA, Pennacchio LA, Tybjaerg-Hansen A, Folsom AR, Boerwinkle E, Hobbs HH, Cohen JC. A common allele on chromosome 9 associated with coronary heart disease. Science. 2007;316:1488–1491. doi: 10.1126/science.1142447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schunkert H, Gotz A, Braund P, McGinnis R, Tregouet DA, Mangino M, Linsel-Nitschke P, Cambien F, Hengstenberg C, Stark K, Blankenberg S, Tiret L, Ducimetiere P, Keniry A, Ghori MJ, Schreiber S, El Mokhtari NE, Hall AS, Dixon RJ, Goodall AH, Liptau H, Pollard H, Schwarz DF, Hothorn LA, Wichmann HE, Konig IR, Fischer M, Meisinger C, Ouwehand W, Deloukas P, Thompson JR, Erdmann J, Ziegler A, Samani NJ. Repeated replication and a prospective meta-analysis of the association between chromosome 9p21.3 and coronary artery disease. Circulation. 2008;117:1675–1684. doi: 10.1161/CIRCULATIONAHA.107.730614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Talmud PJ, Cooper JA, Palmen J, Lovering R, Drenos F, Hingorani AD, Humphries SE. Chromosome 9p21.3 coronary heart disease locus genotype and prospective risk of CHD in healthy middle-aged men. Clin Chem. 2008;54:467–474. doi: 10.1373/clinchem.2007.095489. [DOI] [PubMed] [Google Scholar]
- 7.Topol EJ. Genome scanning and cardiovascular disease. Heart. 2008;94:1361–1363. doi: 10.1136/hrt.2008.150847. [DOI] [PubMed] [Google Scholar]
- 8.ARIC Investigators. The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 9.White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, Higgins M, Williams OD, Tyroler HA. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years' experience. J Clin Epidemiol. 1996;49:223–233. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 10.Siedel J, Hagele EO, Ziegenhorn J, Wahlefeld AW. Reagent for the enzymatic determination of serum total cholesterol with improved lipolytic efficiency. Clin Chem. 1983;29:1075–1080. [PubMed] [Google Scholar]
- 11.Warnick GR, Benderson J, Albers JJ. Dextran sulfate-Mg2+ precipitation procedure for quantitation of high-density-lipoprotein cholesterol. Clin Chem. 1982;28:1379–1388. [PubMed] [Google Scholar]
- 12.Chambless LE, Folsom AR, Sharrett AR, Sorlie P, Couper D, Szklo M, Nieto FJ. Coronary heart disease risk prediction in the Atherosclerosis Risk in Communities (ARIC) study. J Clin Epidemiol. 2003;56:880–890. doi: 10.1016/s0895-4356(03)00055-6. [DOI] [PubMed] [Google Scholar]
- 13.Pencina MJ, D'Agostino RB, Sr, D'Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–172. doi: 10.1002/sim.2929. discussion 207–112. [DOI] [PubMed] [Google Scholar]
- 14.Cook NR. Comments on 'Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond' by M. J. Pencina et al., Statistics in Medicine. Stat Med. 2008;27:191–195. doi: 10.1002/sim.2987. [DOI] [PubMed] [Google Scholar]
- 15.D'Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286:180–187. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 16.Hard Coronary heart Disease (10-year risk) [Accessed 29 October 2008]; Available at: http://www.framinghamheartstudy.org/risk/hrdcoronary.html.
- 17.Grundy SM, Cleeman JI, Bairey Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Jr, Stone NJ. Coordinating Committee of the National Cholesterol Education Program. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 18.Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA. 2007;297:611–619. doi: 10.1001/jama.297.6.611. [DOI] [PubMed] [Google Scholar]
- 19.Folsom AR, Chambless LE, Ballantyne CM, Coresh J, Heiss G, Wu KK, Boerwinkle E, Mosley TH, Jr, Sorlie P, Diao G, Sharrett AR. An assessment of incremental coronary risk prediction using C-reactive protein and other novel risk markers: the Atherosclerosis Risk in Communities Study. Arch Intern Med. 2006;166:1368–1373. doi: 10.1001/archinte.166.13.1368. [DOI] [PubMed] [Google Scholar]
- 20.Paynter NP, Chasman DI, Buring JE, Shiffman D, Cook NR, Ridker PM. Cardiovascular disease risk prediction with and without knowledge of genetic variation at chromosome 9p21.3. Ann Intern Med. 2009;150:65–72. doi: 10.7326/0003-4819-150-2-200901200-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor AJ, Merz CN, Udelson JE. 34th Bethesda Conference: Executive summary--can atherosclerosis imaging techniques improve the detection of patients at risk for ischemic heart disease? J Am Coll Cardiol. 2003;41:1860–1862. doi: 10.1016/s0735-1097(03)00363-2. [DOI] [PubMed] [Google Scholar]
- 22.Greenland P, Abrams J, Aurigemma GP, Bond MG, Clark LT, Criqui MH, Crouse JR, III, Friedman L, Fuster V, Herrington DM, Kuller LH, Ridker PM, Roberts WC, Stanford W, Stone N, Swan HJ, Taubert KA, Wexler L. Prevention Conference V: Beyond secondary prevention: identifying the high-risk patient for primary prevention: noninvasive tests of atherosclerotic burden. Circulation. 2000;101:e16–e22. doi: 10.1161/01.cir.101.1.e16. [DOI] [PubMed] [Google Scholar]
- 23.Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, III, Criqui M, Fadl YY, Fortmann SP, Hong Y, Myers GL, Rifai N, Smith SC, Jr, Taubert K, Tracy RP, Vinicor F. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 24.Greenland P, Smith SC, Jr, Grundy SM. Improving coronary heart disease risk assessment in asymptomatic people: role of traditional risk factors and noninvasive cardiovascular tests. Circulation. 2001;104:1863–1867. doi: 10.1161/hc4201.097189. [DOI] [PubMed] [Google Scholar]
- 25.Pasternak RC, Abrams J, Greenland P, Smaha LA, Wilson PW, Houston-Miller N. 34th Bethesda Conference: Task force #1--Identification of coronary heart disease risk: is there a detection gap? J Am Coll Cardiol. 2003;41:1863–1874. doi: 10.1016/s0735-1097(03)00358-9. [DOI] [PubMed] [Google Scholar]
- 26.Assimes TL, Knowles JW, Basu A, Iribarren C, Southwick A, Tang H, Absher D, Li J, Fair JM, Rubin GD, Sidney S, Fortmann SP, Go AS, Hlatky MA, Myers RM, Risch N, Quertermous T. Susceptibility locus for clinical and subclinical coronary artery disease at chromosome 9p21 in the multi-ethnic ADVANCE study. Hum Mol Genet. 2008;17:2320–2328. doi: 10.1093/hmg/ddn132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.