Abstract
CONTEXT:
The prevalence of type 2 diabetes is increasing in the Bangladeshi population. However, there is little information available on the prevalence of glucose intolerance, ie, type 2 diabetes, impaired glucose tolerance, and impaired fasting glucose.
AIMS:
The main aim of this study is to determine the prevalence of different categories of glucose intolerance and their relationship with different anthropometric and demographic characteristics.
SETTINGS AND DESIGN:
This cross-sectional study was performed in a rural area of Bangladesh.
MATERIALS AND METHODS:
A random sample of 5000 persons aged ≥ 20 years was included in this study. Fasting blood glucose was measured in 3981 individuals and 2-h post-glucose blood glucose was measured in 3954 subjects after the known cases of diabetes (n = 27) were excluded. Height, weight, waist and hip circumference, and blood pressure were measured.
STATISTICAL ANALYSIS:
Pearson Chi-squared test and correlation test were used for analysis as appropriate.
RESULTS:
The prevalence of impaired fasting glucose (IFG), impaired glucose tolerance (IGT) and diabetes (DM) were 1.3, 2.0, and 7.0%, respectively. IFG, IGT, and IFG + IGT were more prevalent in females. Age showed a significant positive relationship with increasing levels of glucose intolerance. Body mass index, waist circumference, and waist-to-hip ratio were higher in the glucose-intolerant group than in the normal glucose tolerance (NGT) group. There was a positive correlation between FBG and 2-h BG in NGT and DM subjects.
CONCLUSION:
The FBG value identified more people with glucose intolerance than the 2-h BG. These findings will help developing diabetes preventive strategy in rural populations.
Keywords: Body mass index, fasting blood glucose, glucose intolerance, rural Bangladesh
Introduction
The prevalence of type 2 diabetes mellitus (T2DM) is projected to increase radically during the forthcoming decades in both developed and developing countries.[1] However, the prevalence of various stages of glucose intolerance, ie, T2DM, impaired fasting glucose (IFG) and impaired glucose tolerance (IGT), differ noticeably between countries and populations. It has been suggested that differential prevalence in the stages of glucose intolerance is related to the diet and genetic susceptibility of individuals, the age structure of the population, and the stage of economic development and level of urbanization of a country.[2] Bangladesh is a developing country which has experienced rapid urbanization, rural to urban migration, and increase in employment with limited economic development.[3] At the same time, the county has experienced a demographic transition with a slow but gradual increase in the proportion of the older age-groups.[4]
Some population-based studies conducted in urban and rural areas of Bangladesh have attempted to estimate the prevalence of diabetes mellitus. These studies, conducted at different time points, show a trend for increase in the prevalence of diabetes; the prevalence rates in these studies have ranged from 2.2 to 8.1% both in rural and urban communities.[5–7] A high prevalence of diabetes and chronic heart disease (CHD) has also been reported among Bangladeshis settled in the UK as compared to the native population.[8] Some other recent studies have shown a high prevalence of diabetes, IGT, and IFG in native Indians and in Asian Indians settled in Europe and in the USA.[9–11] IFG or IGT is now considered as pre-diabetes and is suggested to be a strong risk factor for cardiovascular disease (CVD).[12]
In Bangladesh, studies related to diabetes and IGT in urban areas have reported different prevalence rates.[6,13] The inconsistencies may have been due to variations in the sample sizes and the different methods used for blood glucose estimation. To the best of our knowledge, no study has yet been conducted in the Bangladeshi population to estimate the prevalence of glucose intolerance (T2DM, IFG, and IGT) using the American Diabetic Association (ADA) and World Health Organization (WHO) criteria.[14,15] Evidence suggests that in Pakistan, India, and Bangladesh, the risk factors for diabetes and CVD vary with the region being studied[16] The purpose of the present study was to use the new WHO - 1999 criteria to estimate the prevalence of different categories of glucose intolerance[15] and to identify the demographic and anthropometric characteristics of the sample population.
Materials and Methods
This analysis was carried out with the data collected from a population-based cross- sectional survey conducted in 2004 in a rural community 40 km to the north of Dhaka city. The details of the study population have been described elsewhere.[17] In brief, a randomly selected population of 5,000 persons (both males and females; aged ≥20 years) were invited to participate in the study. Fasting blood glucose (FBG) was estimated in 3981 subjects and 2-h PG BG (post-glucose blood-glucose) was estimated in 3954 individuals; known cases of diabetes (n= 27) were excluded.
Weight, height, waist and hip circumferences were measured with the study participants in a standing position, wearing light clothes and no shoes. The weight was measured to the nearest 0.1 kg by a modern digital bathroom scale and the height was measured to the nearest 0.1 cm. Body mass index (BMI) was calculated by dividing the weight (in kilograms) by the height in meters squared. Waist circumference was measured at the level of the minimum circumference between the lower border of ribs and iliac crest. Hip circumference was measured at the greatest protrusions of the buttocks just below the iliac crest. The waist-hip ratio (WHR) was calculated as waist circumference / hip circumference.
Blood pressure (BP) was recorded after the subjects had rested for at least 5 min. The pressure was measured on the right arm using a mercury sphygmomanometer with a standard cuff for adults; the stethoscope bell was placed lightly over the brachial artery and the blood pressure was recorded to the nearest 2 mm Hg, reading from the top of the mercury meniscus. Systolic blood pressure (SBP) was recorded at the first appearance of Korotkoff sounds and diastolic blood pressure (DBP) was measured at phase V, ie, the disappearance of the sounds.
Capillary whole blood was taken for measurement of FBG, which was measured in all individuals (n = 3981) using a HemoCue glucose analyzer. The machine was calibrated every day with standard glucose solution to minimize the measuring error. After estimation of FBG, all participants (n = 3954), except the known diabetic cases, had a 2-h post-glucose BG estimation done.
Diabetes, IFG, and IGT were defined using the new WHO criteria 1999,[15] which are as follows:
| FBG (mmol/l) | 2-h post BG (mmol/l) | ||
|---|---|---|---|
| Normal (NGT) | < 5.5 | and | < 7.7 |
| Impaired fasting glucose | 5.6–6.0 | and | 0.0< 7.7 |
| Impaired glucose tolerance (IGT) | 0.0< 5.5 | and | 7.8–11.0 |
| *IFG + IGT | 5.6–6.0 | and | 7.8–11.0 |
| Diabetes | >6.1 | and/or | >11.1 |
Not mentioned in the WHO criteria
BMI > 25 kg/m2 was taken to indicate obesity for both sexes. The cut-off values for waist circumference for men and women were > 90 and > 80 cm, respectively and WHR for men was > 0.90 and > 0.85 for women.[18]
Statistical analysis
The prevalence of diabetes, IFG, and IGT was determined by calculating the simple percentages. Comparisons between the groups was done using the χ2 test and Student's t test was used for continuous variables. Pearson correlation test was done to calculate the correlation between the variables. A P-value of < 0.05 was considered statistically significant. All P-values presented are two-tailed. We used SPSS, version 11.0, for analysis.
Ethics
As most of the participants were illiterate, verbal consent was secured from each individual prior to inclusion in the study. They were also verbally informed of their right to withdraw from the study at any stage or to restrict their data from the analysis. The protocol was approved by both the Norwegian and Bangladeshi ethical committees for medical research.
Results
The prevalence of IFG, IGT, IFG + IGT, and diabetes were 1.3, 2.0, 4.3, and 7.0%, respectively. IFG, IGT, and IFG + IGT were more prevalent in females than males, however the difference was significant only for IFG + IGT (5.0% in females vs 3.1% in males; P < 0.001) group. No significant sex difference was found in the diabetic or other groups. BMI was higher in the IGT, IFG + IGT, and DM groups, and increased waist circumference was observed in the IGT and DM groups [Table 1].
Table 1.
Prevalence of different categories of glucose tolerance (by sex) and percentage of the sample with increased body mass index, waist circumference, and waist-hip ratio
| NGT | IFG | IGT | IFG + IGT | DM | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | (%) | No. | (%) | No. | (%) | No. | (%) | No. | (%) | |
| Total | 3,387 | (85.4) | 53 | (1.3) | 79 | (2.0) | 169 | (4.3) | 279 | (7.0) |
| Male | 1,383 | (86.9) | 17 | (1.1) | 23 | (1.4) | 50 | (3.1)*** | 119 | (7.5) |
| Female | 2,004 | (84.2) | 36 | (1.5) | 56 | (2.4) | 119 | (5.0)*** | 160 | (6.7) |
| Increased BMI | 321 | (9.5) | 5 | (9.4) | 11 | (14.1) | 26 | (15.2) | 60 | (21.5) |
| Increased waist circumference | 481 | (14.2) | 7 | (13.2) | 23 | (29.1) | 41 | (24.0) | 79 | (28.3) |
| Increased WHR | 1,950 | (57.5) | 33 | (62.2) | 55 | (69.6) | 113 | (66.8) | 203 | (72.7) |
NGT (FBG = 0.0–5.5 mmol/l and 2–h BG = 0.0–7.7 mmol/l), IFG (FBG = 5.6–6.0 mmol/l and 2–h BG = 0.0–7.7 mmol/l), IGT (FBG = 0.0–5.5 mmol/l and 2–h BG = 7.8–11.0 mmol/l), IFG + IGT (FBG = 5.6–6.0 mmol/l and 2–h BG = 7.8–11.0 mmol/l), DM (FBG ≥ 6.1 mmol/l or 2–h BG ≥ 11.0 mmol/l)
P<0.001
The mean age of the subjects increased with increasing degree of glucose intolerance in both sexes. BMI, WHR, and waist circumference were higher in the glucose intolerant groups than in the NGT group, while the highest mean values were found in the diabetes group for both sexes. WHR was significantly higher among males in all groups. Waist circumference was significantly higher in males in the IFG and DM groups [Table 2].
Table 2.
Mean ± 2SD of age, BMI, waist, WHR, SBP, and DBP by different categories of glucose tolerance (males and females)
| NGT | IFG | IGT | IFG + IGT | DM | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | 2SD | Mean | 2SD | Mean | 2SD | Mean | 2SD | Mean | 2SD | |
| Age | ||||||||||
| Male | 37.9*** | ± 14.6 | 37.2 | ± 14.9 | 44.6 | ± 17.3 | 43.9 | ± 16.9 | 49.2*** | ± 16.1 |
| Female | 34.9*** | ± 12.9 | 41.3 | ± 19.7 | 40.4 | ± 17.0 | 41.2 | ± 15.3 | 42.6*** | ± 14.8 |
| BMI (kg/m2) | ||||||||||
| Male | 20.4* | ± 2.9 | 20.8 | ± 2.6 | 20.7 | ± 3.0 | 20.7 | ± 3.2 | 22.1 | ± 4.2 |
| Female | 20.7* | ± 3.3 | 20.0 | ± 3.7 | 20.6 | ± 3.6 | 21.0 | ± 4.3 | 21.3 | ± 4.6 |
| Waist (cm) | ||||||||||
| Male | 73.8*** | ± 8.5 | 76.6* | ± 9.2 | 75.2 | ± 11.7 | 75.9 | ± 9.7 | 79.6* | ± 11.6 |
| Female | 72.0*** | ± 9.1 | 70.0* | ± 9.5 | 72.9 | ± 10.6 | 73.9 | ± 11.4 | 75.3* | ± 10.4 |
| WHR | ||||||||||
| Male | 0.88*** | ± 0.06 | 0.89 | ± 0.05 | 0.88* | ± 0.09 | 0.89*** | ± 0.07 | 0.92*** | ± 0.07 |
| Female | 0.83*** | ± 0.06 | 0.83 | ± 0.05 | 0.85* | ± 0.07 | 0.85*** | ± 0.06 | 0.86*** | ± 0.07 |
| SBP (mm Hg) | ||||||||||
| Male | 118.6 | ± 15.4 | 123.5 | ± 18.5 | 128.2 | ± 21.6 | 124.9 | ± 20.9 | 129.7 | ± 22.0 |
| Female | 118.4 | ± 17.5 | 121.6 | ± 18.7 | 123.4 | ± 20.5 | 123.6 | ± 20.3 | 127.8 | ± 21.8 |
| DBP (mm Hg) | ||||||||||
| Male | 76.6 | ± 9.9 | 80.8 | ± 10.4 | 81.0 | ± 10.4 | 80.7 | ± 12.5 | 82.9 | ± 11.6 |
| Female | 76.3 | ± 11.1 | 78.6 | ± 10.1 | 79.1 | ± 13.4 | 79.8 | ± 10.5 | 80.9 | ± 11.9 |
P <0.001
Age has a significant positive relationship with the degree of glucose intolerance and this is observed in both males and females [Figure 1A and B].
Figure 1A.
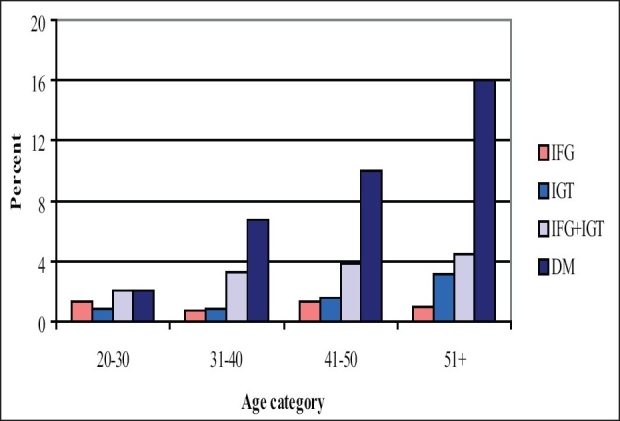
Prevalence of different categories of glucose intolerance by age (males)
Figure 1B.
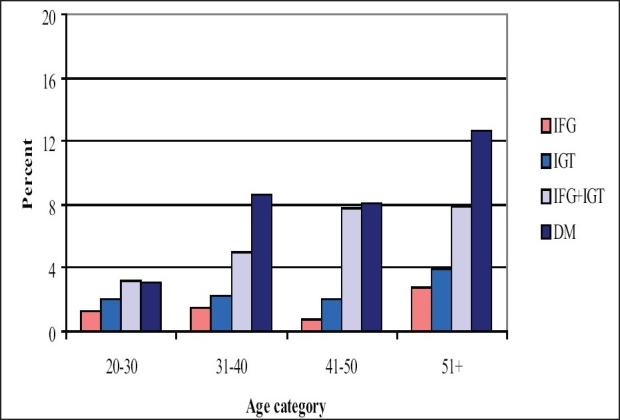
Prevalence of different categories of glucose intolerance by age (females)
Among the subjects with FBG value in the range of 5.6–6.0 mmol/l, 23.2% turned out to have NGT, 74.1% had IGT, and 2.6% were diabetic as assessed by the 2-h post-glucose BG values. Among the 258 diabetic subjects having an FBG of ≥ 6.1 mmol/l, 128 (49.6%) had 2-h PG BG ≥11.1 mmol/l and 44.6% had 2-h PG BG level in the range of 7.8–11.0 mmol/l. Among the total of 266 subjects with diabetes, 128 subjects had 2-h PG BG values of ≥_11.1 mmol/l and the remaining 130 subjects satisfied only the FBG criterion for diagnosis of diabetes (ie, FBG ≥ 6.1 mmol/l) [Table 3].
Table 3.
Distribution of subjects according to fasting blood glucose and 2–h post-glucose BG categories
| FBG (mmol/l) | 2–h Post-glucose blood glucose (mmol/l) | |||||||
|---|---|---|---|---|---|---|---|---|
| NGT (0.0–7.7) | IGT (7.8–11.00) | DM (11.1+) | Total | |||||
| No. | % | No. | % | No. | % | No. | % | |
| NGT (0.0–5.5) | 3,387 | 97.7 | 79 | 2.3 | 2 | 0.1 | 3,468 | 87.7 |
| IFG (5.6–6.0) | 53 | 23.2 | 169 | 74.1 | 6 | 2.6 | 228 | 5.7 |
| DM (6.1+) | 16 | 6.2 | 114 | 44.6 | 128 | 49.6 | 258 | 6.7 |
| Total | 3,456 | 87.4 | 362 | 9.2 | 136 | 3.4 | 3,954 | 100 |
FBG and 2-h post-glucose BG values were positively correlated in NGT and DM subjects. The correlation (Pearson) values and significance levels between FBG and 2-h post-glucose BG values for NGT and DM for males, females, and all subjects are presented in Table 4.
Table 4.
Mean values of fasting blood glucose and corresponding 2–h post-glucose BG for different categories of glucose tolerance (male and female)
| Mean value | NGT | IFG | IGT | IFG + IGT | DM | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| (mmol/l) | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female |
| FBG | 4.4** | 4.5** | 5.7 | 5.7 | 4.7* | 5.0* | 5.8** | 5.7** | 8.1 | 8.0 |
| 2-h BG | 4.9*** | 5.4*** | 5.0** | 6.1** | 8.5 | 8.3 | 8.5 | 8.5 | 12.4 | 12.6 |
| n | 1,383 | 2,004 | 17 | 36 | 23 | 56 | 50 | 119 | 114 | 152 |
P < 0.05;
P < 0.01;
P < 0.001;
Note: P values indicate significance of the difference in mean values of FBG and 2-h BG by gender among different groups of glucose tolerance.
Discussion
Our data showed that the prevalence of IGT was significantly higher than that of IFG. The prevalence of IGT was slightly higher in females but no such sex difference was observed for IFG. Female subjects showed significantly higher prevalence of IFG + IGT, whereas the prevalence of diabetes did not vary between male and female subjects. However, earlier data has shown a higher prevalence of diabetes among female subjects.[19] The prevalence of IFG and IGT was found to vary in terms of its ascendancy across studies. IGT was found to be more prevalent compared to IFG in Mauritius,[20] USA,[21] and in Pima Indians.[22] However, studies conducted in the Netherlands,[23] Finland,[24] India,[9] and among Asian Indians[11] did not find any difference in the prevalence of IFG and IGT. Our results showed similar levels of IFG and IGT in men; however, IGT was higher in women compared to IFG, and this finding is consistent with previous studies in Bangladesh.[7,13] A sex difference in the prevalence of IGT has been reported in other countries.[25] The prevalence of IGT was found to be similar in both sexes in an urban Indian study.[26] Some other studies have shown a higher prevalence of IFG among men and a higher prevalence of IGT among women.[21,27]
Adverse anthropometric features are more prevalent among subjects having impaired glucose regulation, ie, those with IFG, IGT, IFG + IGT, and DM. Our data suggests that IGT and DM were more common among older participants. A similar finding on IFG was also observed in India.[11] Contrary to this finding, a report from Austria showed that age-related increase in FBG was particularly seen in subjects with IFG.[28] This difference between the findings of our study and that from India as compared to the studies conducted elsewhere are likely due to ethnic differences.
Our data showed that when FBG > 6.1 mmol/l was used as the diagnostic criterion, the prevalence of diabetes was 6.7%, whereas it was 3.4% when the 2-h post glucose BG values were used. This finding is an agreement with an Indian study where the prevalence of diabetes was 5.2% according to the FBG criteria and 4.3% according to 2-h post-glucose BG threshold.[29] Furthermore, our data showed that the agreement between the two procedures (FBG and 2-h post-glucose BG) for the identification of diabetic cases was around 50%. Concern has been expressed that IFG might not identify the same subjects as IGT.[29] However, the prevalence of glucose intolerance by either procedure was similar [(by FBG (IFG + DM) was 12.4% or 2-h post-glucose BG (IGT + DM)] was 12,6%)).
Conclusion
The prevalence of glucose intolerance varied significantly, depending on the diagnostic criterion used, namely, FBG or 2-h post-glucose BG estimates. However, it is very important to detect the larger number of subjects with glucose intolerance to prevent diabetes. Our findings need to be verified in other settings for the development of an intervention strategy for the prevention and early management of abnormal glucose tolerance.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Wild H, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes, estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.International Diabetes Federation. Diabetes atlas. Brussels: International Diabetes Federation; 2006. [Google Scholar]
- 3.Laskar SI. Urbanization in Bangladesh: Some contemporary observations. Bangladesh Dev Stud. 1996;24:207–16. [PubMed] [Google Scholar]
- 4.Bangladesh Bureau of statistics. Statistical Pocket Book of Bangladesh. Statistical Division, Ministry of Planning, Government of the Peoples Republic of Bangladesh; 2004. [Google Scholar]
- 5.Hussain A, Rahim MA, Azad Khan AK, Ali SM. Type 2 diabetes in rural and urban population: Diverse prevalence and associated risk factors in Bangladesh. Diabetes Med. 2005;22:931–7. doi: 10.1111/j.1464-5491.2005.01558.x. [DOI] [PubMed] [Google Scholar]
- 6.Sayeed MA, Hussain MZ, Banu A, Ali SM, Rumi MA, Azad Khan AK. Effect of socioeconomic risk factor on differences between rural and urban in the prevalence of diabetes in Bangladesh. Diabetes Care. 1997;20:551–5. doi: 10.2337/diacare.20.4.551. [DOI] [PubMed] [Google Scholar]
- 7.Sayeed MA, Mahtab H, Khanum PA, Latif ZA, Ali SM, Banu A, et al. Diabetes and Impaired fasting glycaemia in rural population of Bangladesh. Diabetes Care. 2003;26:1034–9. doi: 10.2337/diacare.26.4.1034. [DOI] [PubMed] [Google Scholar]
- 8.McKeigue PM, Bela S, Marmot MG. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet. 1991;337:382–6. doi: 10.1016/0140-6736(91)91164-p. [DOI] [PubMed] [Google Scholar]
- 9.Ramachandran A, Snehalatha C, Satyavani K, Vijay V. Impaired fasting glucose and impaired glucose tolerance in urban population in India. Diabet Med. 2003;20:220–4. doi: 10.1046/j.1464-5491.2003.00904.x. [DOI] [PubMed] [Google Scholar]
- 10.Qiao Q, Nakagami T, Tuomilehto J, Borch-Johnsen K, Balkau B, Iwamoto Y, et al. Comparison of the fasting and the 2-h glucose criteria for diabetes in different Asian cohorts. Diabetologia. 2000;43:1470–5. doi: 10.1007/s001250051557. [DOI] [PubMed] [Google Scholar]
- 11.Marguerite J, Neely MC, Edward J. Type 2 diabetes prevalence in Asian Americans. Diabetes Care. 2004;27:66–9. doi: 10.2337/diacare.27.1.66. [DOI] [PubMed] [Google Scholar]
- 12.Larsson H, Berglund G, Lindgarde F, Ahren B. Comparison of ADA and WHO criteria for diagnosis of diabetes and glucose intolerance. Diabetologia. 1998;41:1124–5. doi: 10.1007/s001250051040. [DOI] [PubMed] [Google Scholar]
- 13.Sayeed MA, Hossain MZ, Banu A, Rumi MA, Azad Khan AK. Prevalence of diabetes in a suburban population of Bangladesh. Diabetes Res Clin Pract. 1997;34:149–55. doi: 10.1016/s0168-8227(96)01337-x. [DOI] [PubMed] [Google Scholar]
- 14.Expert Committee on diagnosis and classification of diabetes mellitus. Report of the expert committee on diagnosis and classification of diabetes mellitus. Diabetes Care. 1997;20:1183–97. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Diagnosis and Classification of Diabetes Mellitus. Geneva: Department of Non-communicable Disease Surveillance, WHO; 1999. Definition Diagnosis and Classification of Diabetes Mellitus and its Complications; Part1. [Google Scholar]
- 16.Barnett AH, Dixon AN, Bellary S, Hanif MW, Hare JP, Raymond NT, et al. Type 2 diabetes and cardiovascular risk in UK south Asian community. Diabetologia. 2006;49:2234–46. doi: 10.1007/s00125-006-0325-1. [DOI] [PubMed] [Google Scholar]
- 17.Rahim MA, Hussain A, Azad Khan AK, Sayeed MA, Ali SM, Vaaler S. Rising prevalence of type 2 diabetes in rural Bangladesh: A population based study. Diabetes Res Clin Pract. 2007;77:300–5. doi: 10.1016/j.diabres.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. WHO Recommendation. Obesity preventing and managing the Global Epidemic. Geneva: World Health Organ; (Tec,Rep,Ser,no.894) [PubMed] [Google Scholar]
- 19.Hussain A, Stein V, Sayeed MA, Hajera M, Ali SM, Azad Khan AK. Type 2 diabetes and impaired fasting blood glucose in rural Bangladesh: A population based study. Eur J Pub Health. 2007;17:291–6. doi: 10.1093/eurpub/ckl235. [DOI] [PubMed] [Google Scholar]
- 20.Shaw J, Zimmet P, Courten M. Impaired fasting glucose or impaired glucose tolerance: What best predicts future diabetes in Mauritius? Diabetes Care. 1999;22:399–402. doi: 10.2337/diacare.22.3.399. [DOI] [PubMed] [Google Scholar]
- 21.Harris MI, Goldstein DE, Flegal KM, Little RR, Cowie CC, Wiedmeyer HM, et al. Prevalence of diabetes, impaired fasting glucose and impaired glucose tolerance in US adults: The third National Health and Nutrition Examination 1988–1994. Diabetes Care. 1998;21:518–24. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- 22.Gabir MM, Hanson RL, Dabelea D, Imperatore G, Roumain J, Bennett PH, et al. The 1997 American Diabetes Association and 1999 World Health Organization criteria for hyperglycemia in the diagnosis and prediction of diabetes. Diabetes Care. 2000;23:1108–12. doi: 10.2337/diacare.23.8.1108. [DOI] [PubMed] [Google Scholar]
- 23.De Vegt F, Nijpels G, Dekker JM, Bouter LM, Stehouwer CD, Heine RJ. The 1997 American Diabetes Association criteria versus the 1985 World Health Organization criteria for the diagnosis of abnormal glucose tolerance: Poor agreement in the Hoorn study. Diabetes Care. 1998;21:1686–90. doi: 10.2337/diacare.21.10.1686. [DOI] [PubMed] [Google Scholar]
- 24.Yliharsila H, Lindstrom J, Eriksson JG, Jousilahti P, Valle TT, Sundvall J, et al. Prevalence of diabetes and impaired glucose regulation in 45-to 640 year old individuals in three of Finland. Diabetic Med. 2005;22:88–91. doi: 10.1111/j.1464-5491.2005.01420.x. [DOI] [PubMed] [Google Scholar]
- 25.Ministry of Health. Diabetes Mellitus. Singapore: Ministry of Health; 1999. Ministry of Health Clinical practice Guidelines 4/99; p. 123. [Google Scholar]
- 26.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al. High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey (INUDS) Diabetologia. 2001;44:1094–101. doi: 10.1007/s001250100627. [DOI] [PubMed] [Google Scholar]
- 27.Tripathy DC, Almgren P, Isomaa B, Taskinen M, Tuomi T, Groop L. Insulin secretion and insulin sensitivity in relation to glucose tolerance: Lessons from the Botnia Study. Diabetes. 2000;49:975–80. doi: 10.2337/diabetes.49.6.975. [DOI] [PubMed] [Google Scholar]
- 28.Botas P, Delgado E, Castano G, Diaz de Grenut C, Prieto J, Diaz- Cadorniga FJ. Comparison of the diagnostic criteria for diabetes mellitus, WHO-1985, ADA- 1997 and WHO- 1999 in the adult population of Austria's (Spain) Diabetic Med. 2003;20:904–8. doi: 10.1046/j.1464-5491.2003.01006.x. [DOI] [PubMed] [Google Scholar]
- 29.Ramachandran A, Snehalatha C, Latha E, Vijay V. Evaluation of the use of fasting plasma glucose as a new diagnostic criteria for diabetes in Asian Indian population. Diabetes Care. 1998;21:666–7. doi: 10.2337/diacare.21.4.666. [DOI] [PubMed] [Google Scholar]


