Abstract
Objective
To evaluate the impact of policies for removing women before the recommended age of 64 from screening programmes for cervical cancer in the United Kingdom.
Design
A mathematical model of the clinical course of precancerous lesions which accounts for the influence of infection with the human papillomavirus, the effects of screening on the progression of disease, and the accuracy of the testing procedures. Two policies are compared: one in which women are withdrawn from the programme if their current smear is negative and they have a recent history of regular, negative results and one in which women are withdrawn if their current smear test is negative and a simultaneous test is negative for exposure to high risk types of human papillomavirus.
Setting
United Kingdom cervical screening programme.
Main outcome measures
The incidence of invasive cervical cancer and the use of resources.
Results
Early withdrawal of selected women from the programme is predicted to give rise to resource savings of up to 25% for smear tests and 18% for colposcopies when withdrawal occurs from age 50, the youngest age considered in the study. An increase in the incidence of invasive cervical cancer, by up to 2 cases/100 000 women each year is predicted. Testing for human papillomavirus infection to determine which women should be withdrawn from the programme makes little difference to outcome.
Conclusions
This model systematically analyses the consequences of screening options using available data and the clinical course of precancerous lesions. If further audit studies confirm the model’s forecasts, a policy of early withdrawal might be considered. This would be likely to release substantial resources which could be channelled into other aspects of health care or may be more effectively used within the cervical screening programme to counteract the possible increase in cancer incidence that early withdrawal might bring.
Key messages
In the United Kingdom there is concern that the cervical screening programme uses a large amount of resources to screen postmenopausal women who are at low risk of cervical cancer
There may be advantages to withdrawing these women from the screening programme before they reach the recommended age of 64
A mathematical modelling approach can be used to evaluate the effectiveness of different policies for early withdrawal from screening with or without an additional test for human papillomavirus DNA
Early withdrawal could lead to a substantial reduction in the resources devoted to screening which could be channelled more effectively into other aspects of health care
Early withdrawal is likely to increase the overall incidence of cervical cancer unless other steps are taken to compensate
Introduction
The UK’s national coordinating network for cervical screening recommends that all women between the ages of 21 and 64 attend for screening once every 3 to 5 years.1 It has been suggested, however, that some women could be withdrawn from the screening programme before age 642 because although over half of all cases of invasive cervical cancer occur among women aged over 50,3 few have been found in women with histories of regular smear tests with normal results.2 Additionally, there is evidence that women with certain types of human papillomavirus infection are at high risk of developing high grade precancerous lesions.4–6 The risk of acquiring new human papillomavirus infection is believed to decrease as women get older, so postmenopausal women without previous human papillomavirus infection may have little risk of developing invasive cancer.7 Therefore, by taking account of recent smear test results or the results of human papillomavirus tests, a sizeable population of older women at low risk of cervical disease might be identified, and their early removal from the screening programme would have little impact on the incidence of invasive cancer.2,7 Such measures might also release valuable health service resources in terms of screening and follow up tests and reduce needless anxiety among women.
The purpose of this study is to evaluate the effect on resource savings and on the incidence of invasive cancer of strategies for the early withdrawal from the screening programme of women at low risk of cervical cancer. We used a mathematical model which we have developed and have used in previous studies.8,9 Trials of screening are expensive, and it takes many years before results are known, by which time technological advances may have lessened the relevance of their findings. Trials are also hampered by the difficulty of evaluating long term outcomes and the restricted number of alternative screening policies that can be compared. Moreover, it is not feasible to assess directly the potential effects on the incidence of invasive cancer and instead surrogate end points would need to be used. Mathematical modelling provides an alternative means of investigation, and is a comparatively quick method for assessing a range of screening options. Although dependent on the validity of the assumptions made, it has a useful role in complementing the results of trials and audit studies.
Methods
The main elements of our model are the clinical course of the disease, age related mortality from all causes, the accuracy of the screening tests, and the clinical management policy adopted for women with positive test results. Our methods rely on stochastic analysis—that is, we use methods from probability theory to represent the considerable variability inherent in the screening process.
The clinical course of the disease and the development of invasive cancer are the result of a sequence of transitions through three grades of cervical intraepithelial neoplasia. We assume that most cases of cervical intraepithelial neoplasia are preceded by human papillomavirus infection,4 although the possibility that neoplasia can occur without prior infection is also considered. The human papillomavirus is classified into low risk and high risk types. The high risk types (16, 18, 31, and 33) are more strongly associated with high grade precancerous lesions and invasive cancer, and the low risk types (6 and 11) are associated with low grade disease. This model of the clinical course is stochastic in that the transition between disease states is assumed to be a chance process with each transition made with a specified probability. Starting with a cohort of women who are free from disease and using age related death rates from other causes, the model predicts the number of women in each disease category at all later times. If women are screened then the chances of detecting any precancerous lesion will depend on the accuracy of the screening test. Successful detection and treatment of precancerous lesions is modelled by assuming that women revert to being disease free. Screening occurs at different ages depending on the programme and the policy for the follow up of abnormal results. Options for early withdrawal from the screening programme are included.
Estimates used to calibrate the model have been derived from the medical literature. The role of human papillomavirus infection in relation to the development and progression of premalignant conditions has been studied.6 Sources used to estimate parameters used by the model have been described.9 Because of the uncertainty in some of these parameters, particularly in relation to the clinical course of precancerous disease, we have investigated the consequences of using different values for the same parameter. For example, we have varied the rate that disease progresses in the absence of any external intervention by 20%. The prevalence of human papillomavirus infection in older women has been little studied, and our estimates for incidence rates are derived from a study in which the oldest women were aged 50 to 54.10 Beyond the age of 50, we have assumed that the incidence of infection declines gradually. To reflect the uncertainty in this assumption we have also investigated outcomes if the incidence of infection was such that its prevalence among women aged over 50 were 50% lower.
We have considered a programme of screening every 3 years starting at the age of 21. Mildly abnormal and borderline results are followed up according to recommendations for repeat cytology in the United Kingdom.1 We have also compared a policy of screening all women up to the age of 64 with two policies for early withdrawal. Policy 1 is based on the work of Van Wijngaarden and Duncan2: a woman is withdrawn from screening if she is over a specified age, her smear result is negative, and her previous three smears were negative and taken regularly three years apart. Policy 2 is based on Schiffman and Sherman7: a woman is withdrawn if she is over a specified age, her smear result is negative, and a test for human papillomavirus DNA is negative for high risk types.
These policies have been investigated with the specified age for the earliest possible recommended withdrawal ranging from 50 to 60.
We have assumed that 85% of eligible women are screened, similar to current coverage rates in the United Kingdom,11 and that this is the same for all ages at which women are screened. Currently, coverage within the United Kingdom is higher among younger women than older women but is expected to become more evenly distributed over time. This study analyses situations in which there is a more even distribution. Women who do not attend for screening are assumed to have the same risk of acquiring human papillomavirus infection and developing premalignant lesions as those who do,12 although non-attenders implicitly have a much higher risk of their disease progressing undetected. We have also considered the effects of assuming a 20% increase in the risk of acquiring human papillomavirus infection among non-attenders.
Results
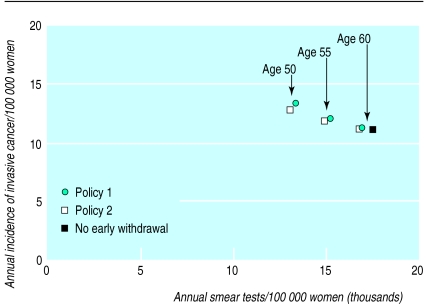
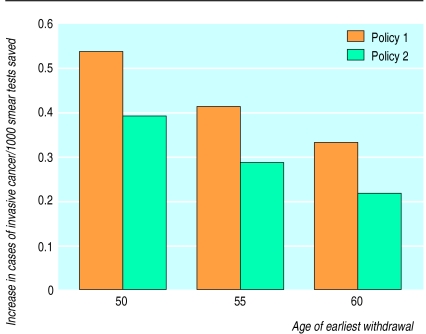
The predicted annual incidence of invasive cervical cancer and the use of resources under different policies for the early withdrawal of women from screening are shown in table 1. These predictions are per 100 000 screened and unscreened women in the female population. Reducing the age of the earliest withdrawal increases the incidence of invasive cancer. Slightly smaller increases are predicted to occur if policy 2 is used. Both policies give substantial and similar reductions in resource use in terms of smear tests and colposcopies, although policy 2 requires additional testing for human papillomavirus infection. In figure 1 the predicted incidence of invasive cancer under each policy is plotted against the number of required smear tests. The increase in the number of cases of invasive cancer for every 1000 smear tests saved by withdrawing women early is shown in figure 2. This ratio increases with a decreasing age of earliest withdrawal and is greater under policy 1.
Table 1.
Predicted annual use of resources and incidence of invasive cancer when women are screened every three years and 85% of eligible women are screened
| Screening policy | Annual resources used/100 000 women (% decrease from policy of no early withdrawal)
|
Incidence of invasive cancer/100 000 women (% increase over policy of no early withdrawal) | ||
|---|---|---|---|---|
| Smear test | Colposcopy* | Test for HPV | ||
| No early withdrawal | 17 600 | 218 | 0 | 10.8 |
| Withdrawal from age 60: | ||||
| Policy 1 | 17 000 (3.6) | 213 (2.5) | 0 | 11.0 (1.9) |
| Policy 2 | 16 900 (4.0) | 213 (2.6) | 1030 | 10.9 (1.4) |
| Withdrawal from age 55: | ||||
| Policy 1 | 15 300 (13.3) | 198 (9.4) | 0 | 11.8 (9.0) |
| Policy 2 | 15 000 (14.5) | 197 (9.6) | 1110 | 11.5 (6.8) |
| Withdrawal from age 50: | ||||
| Policy 1 | 13 400 (23.8) | 180 (17.6) | 0 | 13.1 (21.1) |
| Policy 2 | 13 100 (25.3) | 180 (17.5) | 1160 | 12.5 (16.0) |
HPV=human papillomavirus; in Policy 1 a woman is withdrawn from screening if she is over a specified age, her smear test result is negative, and her previous three smears were negative and taken regularly three years apart; in Policy 2 a woman is withdrawn if she is over a specified age, her smear test result is negative, and a test for HPV infection is negative for high risk types of the virus.
Rounded to nearest integer.
Figure 1.
Comparison of number of annual smear tests and annual incidence of invasive cancer under two screening policies by youngest age of withdrawal of women from screening programme. See text for complete description of policies
Figure 2.
Increase in the number of cases of invasive cancer by resources saved per 1000 smear tests under the two screening policies by youngest age of withdrawal of women from screening programme. See text for complete description of policies
With a policy of withdrawing women from the age of 50 the implications of different assumptions about the clinical course of the disease, the prevalence of detected human papillomavirus infection, and of a reduction in cytological accuracy are shown in table 2. Altering these assumptions has little effect on the number of smear tests and human papillomavirus tests. There are larger changes in the number of colposcopies required yet the percentage reductions caused by early withdrawal are the same as those made under the baseline assumptions. There are also changes in the incidence of invasive cancer but the percentage increases caused by early withdrawal are similar to those made under the baseline assumptions.
Table 2.
Effects of modelling different assumptions about cervical cancer and screening when women are withdrawn from screening from age 50, are screened every three years, and 85% of eligible women are screened
| Model | Annual resources used/100 000 women (% decrease from policy of no early withdrawal)
|
Incidence of invasive cancer/100 000 women (% increase over policy of no early withdrawal) | ||
|---|---|---|---|---|
| Smear test | Colposcopy* | Test for HPV | ||
| Baseline assumptions: | ||||
| No early withdrawal | 17 600 | 218 | 0 | 10.8 |
| Policy 1 | 13 400 (23.8) | 180 (17.6) | 0 | 13.1 (21.1) |
| Policy 2 | 13 100 (25.3) | 180 (17.5) | 1160 | 12.5 (16.0) |
| Progression of disease reduced by 20%: | ||||
| No early withdrawal | 17 600 | 197 | 0 | 6.6 |
| Policy 1 | 13 400 (24.0) | 161 (18.4) | 0 | 8.0 (21.1) |
| Policy 2 | 13 100 (25.4) | 161 (18.5) | 1160 | 7.7 (15.7) |
| Progression of disease increased by 20%: | ||||
| No early withdrawal | 17 600 | 239 | 0 | 15.8 |
| Policy 1 | 13 400 (23.8) | 199 (16.8) | 0 | 19.1 (21.1) |
| Policy 2 | 13 200 (25.3) | 199 (16.6) | 1160 | 18.4 (16.5) |
| Prevalence of HPV infection beyond age 50†: | ||||
| No early withdrawal | 17 500 | 184 | 0 | 7.1 |
| Policy 1 | 13 300 (24.0) | 149 (18.9) | 0 | 8.6 (20.8) |
| Policy 2 | 13 100 (25.5) | 148 (19.5) | 1140 | 8.4 (17.8) |
| Cytology sensitivity 30% lower: | ||||
| No early withdrawal | 17 600 | 208 | 0 | 14.2 |
| Policy 1 | 13 400 (23.8) | 169 (18.8) | 0 | 16.7 (17.6) |
| Policy 2 | 13 100 (25.3) | 171 (17.8) | 1160 | 15.9 (12.0) |
| 30% more false positives as a proportion of women without precancerous lesions: | ||||
| No early withdrawal | 17 900 | 275 | 0 | 10.8 |
| Policy 1 | 13 700 (23.4) | 224 (18.5) | 0 | 13.0 (20.4) |
| Policy 2 | 13 300 (25.3) | 223 (19.1) | 1160 | 12.5 (15.7) |
HPV=human papillomavirus; in Policy 1 a woman is withdrawn from screening if she is over a specified age, her smear test result is negative, and her previous three smears were negative and taken regularly three years apart; in Policy 2 a woman is withdrawn if she is over a specified age, her smear test result is negative, and a test for HPV infection is negative for high risk types of the virus.
Rounded to nearest integer.
Prevalence = ½ × baseline assumption.
Discussion
The impact of early withdrawal
This study has investigated two policies for removing women from a cervical screening programme before age 64. Because there is a possibility that new disease may be contracted by women who are removed from the programme early, or that existing disease may be missed by their final smear test, both of these policies are predicted to increase the incidence of invasive cancer. In the extreme case, in which women are withdrawn at the age of 50, the incidence is predicted to increase by around two extra cases per 100 000 women, or about 600 new cases each year in the United Kingdom. These policies would reduce annual rates of smear testing and colposcopy because the investigations with negative results that occur among women who are regularly screened and are aged between 50 and 64 would be avoided. These reductions in resource use are of the order of 25% for smear tests and 18% for colposcopies, or approximately 1.3 million smear tests and 11 400 colposcopies each year. Both policies would also reduce the psychological stress associated with screening. There is little difference between the two policies in the increase in the incidence of invasive cancer and the number of smear tests and colposcopies required.
Under both policies the ratio of the increase in cases of invasive cancer to the number of smear tests saved by early withdrawal increases as the age of earliest withdrawal decreases. This suggests that the earlier the age of withdrawal, the greater the impact of released resources on the incidence of invasive cancer. This impact is greater under policy 1.
However, there are ethical and pragmatic issues associated with a decision to modify a screening programme which are beyond the scope of this study. For example, it might be that even though substantial resources would be saved in terms of screening and follow up tests, such a modification in screening would be unacceptable to the community. Or it could be that such savings might be better diverted to other aspects of the screening programme or better invested in other areas of the NHS. Alternatively, it might be acceptable to use the resources released to reduce the incidence of cervical cancer by improving coverage or by more efficient targeting of high risk groups.
Assumptions of the model
The feasibility of withdrawing women early from screening programmes will depend on a number of factors for which complete information is not available: the clinical course of the disease in older women, the probability of high risk women satisfying the withdrawal criteria, and the rate of false negative results. To reflect some of the uncertainty about the clinical course we have varied the progression rates by 20% and assessed the changes in results. This has little impact on the comparative effectiveness of the two policies. To reflect some of the uncertainty over the accuracy of cytology, and to assess the implications among centres with higher rates of false positive and false negative results, we independently reduced the sensitivity of cytology and increased the rate of false positives by 30%. In neither case was there much impact on the comparative effectiveness of the two policies.
It is possible that women who are withdrawn early are those who would be at lowest risk of contracting any subsequent disease. We have, therefore, examined different scenarios in which the female population is stratified according to our estimates of their risk of infection with the human papillomavirus. This had little effect on the results. We have assumed that the risk of disease is the same among women who attend for screening and women who do not. This is in accordance with findings on the impact of screening rates of over 80%.12,13 However, increasing the risk among those who do not attend by up to 20% has little effect on the results.
We assumed that the accuracy of cytology and human papillomavirus testing is the same for all ages. Although there is some debate over the changes in the accuracy of cytology with age,14 there is evidence to support our assumption.15
Human papillomavirus testing
Recent evidence about the link between human papillomavirus infection and cervical cancer4,5,16 has suggested that testing for infection within cervical screening programmes, particularly as a triage measure for women presenting with mildly abnormal smears, could be effective.17,18 The identification of older women at low risk of developing precancerous cervical lesions is another possible use for this technology.
Previous studies
Van Wijngaarden and Duncan studied the screening histories of all women aged over 50 in the Dundee and Angus health districts who presented with cervical intraepithelial neoplasia or invasive cervical cancer over four years.2,19 In 47 women with invasive cancer and 40 cases of intraepithelial neoplasia occurring in women aged over 50, only one microinvasive cancer and one case of cervical intraepithelial neoplasia grade III were found in women who would have satisfied the authors’ criteria for early withdrawal. The rest had inadequate screening histories. Cruickshank et al studied the smear test histories of all women aged 50 to 60 in the Grampian region who presented with significant cytological abnormalities over five years.20 Of the 9000 women who had adequate smear histories before age 50, and who would have satisfied the criteria for early withdrawal, one case of cervical intraepithelial neoplasia grade III and one of invasive cervical cancer were found. The results of both these studies agree with our forecasts that early removal from screening would lead to a small increase in the incidence of cervical cancer. These studies are steps towards answering the question about withdrawing women aged between 50 and 60 and towards more rigorous audit studies in which the screening histories of women with cervical disease are compared with those from a control group.21
Our analysis shows that a policy of withdrawing selected women early from screening has the potential to save considerable resources, albeit with a potential increase in the incidence of cervical cancer. The ethical questions arising from whether the benefit of saving resources is worth the potential increases in overall incidence are beyond the scope of this study. Even dispassionate health economic analysis is difficult. Calculations based on the “cost per case of cancer avoided” depend on estimates in which the denominator (the number of cases of cancer) is comparatively small and thus inevitably involves considerable uncertainty.
Acknowledgments
The authors thank Dr Ian Duncan from Ninewells Hospital and Medical School, Dundee, for his helpful comments on an earlier draft of this paper.
Footnotes
Funding: Funds for this project are covered by a Department of Health Core Grant (No 1212226).
Competing interests: DJ was invited by Digene to attend a symposium, which was organised by the European Research Organisation on Genital Infection and Neoplasia, on testing for the human papillomavirus.
References
- 1.Duncan ID, editor. Guidelines for clinical practice and programme management: national coordinating network of the NHS cervical screening programme. Oxford: Oxford Regional Health Authority; 1992. [Google Scholar]
- 2.Van Wijngaarden WJ, Duncan ID. Rationale for stopping screening in women over 50. BMJ. 1993;306:967–971. doi: 10.1136/bmj.306.6883.967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Office for National Statistics. Estimates of newly diagnosed cases of cancer: England and Wales 1993-1997. London: DoH; 1998. (Monitor MB1 98/2.) [Google Scholar]
- 4.Bosch FX, Manos MM, Muñoz N, Sherman M, Jansen AM, Peto J, et al. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. J Natl Cancer Inst. 1995;87:796–802. doi: 10.1093/jnci/87.11.796. [DOI] [PubMed] [Google Scholar]
- 5.Koutsky LA, Holmes KK, Critchlow CW, Stevens CE, Paavonen J, Beckmann AM, et al. A cohort study of the risk of cervical intraepithelial neoplasia grade 2 or 3 in relation to papillomavirus infection. N Engl J Med. 1992;327:1272–1278. doi: 10.1056/NEJM199210293271804. [DOI] [PubMed] [Google Scholar]
- 6.Jenkins D, Sherlaw-Johnson C, Gallivan S. Assessing the role of HPV testing in cervical cancer screening. Papillomavirus Rep. 1998;9:89–101. [Google Scholar]
- 7.Schiffman MH, Sherman ME. HPV testing to improve cervical cancer screening. In: Srivastava S, Lippman SM, Hong WK, Mulshine JL, editors. Early detection of cancer: molecular markers. Armonk, New York: Futura Publishing; 1994. pp. 265–277. [Google Scholar]
- 8.Sherlaw-Johnson C, Gallivan S, Jenkins D, Jones MH. Cytological screening and management of abnormalities in prevention of cervical cancer: an overview with stochastic modelling. J Clin Pathol. 1994;47:430–435. doi: 10.1136/jcp.47.5.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jenkins D, Sherlaw-Johnson C, Gallivan S. Can papillomavirus testing be used to improve cervical cancer screening? Int J Cancer. 1996;65:768–773. doi: 10.1002/(SICI)1097-0215(19960315)65:6<768::AID-IJC10>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 10.Melkert PW, Hopman E, van den Brule AJC, Risse EJK, van Diest PJ, Bleker OP, et al. Prevalence of HPV in cytomorphologically normal cervical smears, as determined by the polymerase chain reaction, is age-dependent. Int J Cancer. 1993;53:919–923. doi: 10.1002/ijc.2910530609. [DOI] [PubMed] [Google Scholar]
- 11.Department of Health. Cervical screening programme, England: 1995-96. London: DoH; 1996. (Statistical Bulletin 1996/26.) [Google Scholar]
- 12.Orbell S, Crombie I, Robertson A, Johnston G, Kenicer M. Assessing the effectiveness of a screening campaign: who is missed by 80% cervical screening coverage. J R Soc Med. 1995;88:389–394. [PMC free article] [PubMed] [Google Scholar]
- 13.Austoker J. Screening for cervical cancer. BMJ. 1994;309:241–248. doi: 10.1136/bmj.309.6949.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mandelblatt J, Schechter C, Fahs M, Muller C. Clinical implications of screening for cervical cancer under Medicare. The natural history of cervical cancer in the elderly: what do we know? What do we need to know? Am J Obstet Gynecol. 1991;164:644–651. doi: 10.1016/s0002-9378(11)80040-2. [DOI] [PubMed] [Google Scholar]
- 15.Parkin DM, Leach K, Cobb P, Clayden AD. Cervical cytology screening in two Yorkshire areas: results of testing. Public Health. 1982;96:3–14. doi: 10.1016/s0033-3506(82)80023-1. [DOI] [PubMed] [Google Scholar]
- 16.Rozendaal L, Walboomers JMM, van der Linden JC, Voorhorst FJ, Kenemans P, Helmerhorst TJM, et al. PCR-based high-risk HPV test in cervical cancer screening gives objective risk assessment of women with cytomorphologically normal cervical smears. Int J Cancer. 1996;68:766–769. doi: 10.1002/(SICI)1097-0215(19961211)68:6<766::AID-IJC13>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 17.Mansell ME, Ho L, Terry G, Singer A, Cuzick J. Semi-quantitative human papillomavirus DNA detection in the management of women with minor cytological abnormality. Br J Obstet Gynaecol. 1994;101:807–809. doi: 10.1111/j.1471-0528.1994.tb11952.x. [DOI] [PubMed] [Google Scholar]
- 18.Cox JT, Lorincz AT, Schiffman MH, Sherman ME, Cullen A, Kurman RJ. Human papillomavirus testing by hybrid capture appears to be useful in triaging women with a cytological diagnosis of atypical squamous cells of undetermined significance. Am J Obstet Gynecol. 1995;172:946–954. doi: 10.1016/0002-9378(95)90026-8. [DOI] [PubMed] [Google Scholar]
- 19.Van Wijngaarden WJ, Duncan ID. Upper age limit for cervical screening. BMJ. 1993;306:1409–1410. doi: 10.1136/bmj.306.6889.1409-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cruickshank ME, Angus V, Kelly M, McPhee S, Kitchener HC. The case for stopping screening at age 50. Br J Obstet Gynaecol. 1997;104:586–589. doi: 10.1111/j.1471-0528.1997.tb11537.x. [DOI] [PubMed] [Google Scholar]
- 21.Sasieni PD, Cuzick J, Lynch-Farmery E. National Co-ordinating Network for Cervical Screening Working Group: estimating the efficacy of screening by auditing smear histories of women with and without cervical cancer. Br J Cancer. 1996;73:1001–1005. doi: 10.1038/bjc.1996.196. [DOI] [PMC free article] [PubMed] [Google Scholar]