Abstract
Background:
The indwelling urinary catheter is an essential part of modern medical care. Unfortunately, when poorly managed, the indwelling catheter may present a hazard to the very patients it is designed to protect. Catheter-associated urinary tract infection (CAUTI) is the most common nosocomial infection in hospitals and nursing homes.
Aims and Objectives:
The primary objective was to study the effect of amikacin sulfate bladder wash on CAUTI in neurosurgical patients. The other objectives were to study the various organisms causing CAUTI and their antibiotic sensitivity and resistance pattern.
Materials and Methods:
This was a prospective randomized controlled study performed on 60 patients who met the inclusion criteria at the neurosurgical intensive care of the All India Institute of Medical Sciences between June and December 2006. The patients were randomized into two groups – one was the trial group which received amikacin bladder wash, while the other was the control group that did not receive any bladder wash.
Results:
Forty percent of the subjects in the control group developed CAUTI, while none of the subjects in study group developed CAUTI. (Fisher's exact test, P value < 0.001) Pseudomonas aeruginosa (51%) was the commonest pathogen.
Conclusions:
Amikacin sulfate bladder wash was effective in preventing CAUTI. It can thus decrease the antibiotic usage thereby preventing the emergence of antibiotic resistance.
Keywords: Amikacin bladder irrigation, bladder wash, catherer-associated urinary tract infection
Introduction
The indwelling urinary catheter is an essential part of modern medical care and a variety of different indwelling urinary catheters can be used for various purposes. Each year, urinary catheters are inserted in more than five million patients in acute-care hospitals and extended-care facilities.[1]
Unfortunately, when poorly managed, the indwelling catheter may present a hazard to the very patients it is designed to protect. Catheter-associated urinary tract infection (CAUTI) is the most common nosocomial infection in hospitals and nursing homes, comprising >40% of all institutionally acquired infections.[2–6] Interventions such as topical meatal antimicrobials, disinfectants added to the urinary drainage bag, and antimicrobials coatings for catheters have not been shown to decrease the incidence of UTI.[7] An effective measure to prevent the CAUTI has not yet been developed. The most common organisms responsible for CAUTI are Escherichia coli, Candida spp., Klebsiella pneumoniae, Streptococcus agalactiae, Enterococcus faecalis, and Pseudomonas aeruginosa. Amikacin has proven to be the most effective antibiotic in preventing the growth of all these species.[8]
Previous studies have shown that using individualized regimens for bladder washouts minimizes the infection rate and catheter blockage, thus reducing the need for frequent recatheterization.[9] Since there is no significant systemic absorption of antibiotics used for bladder irrigation,[10] prophylactic bladder irrigations are considered to be safe. We performed an extensive review of literature which did not reveal any study done on the effectiveness of amikacin sulfate bladder wash.
Materials and Methods
This study was performed on a total of 60 catheterized patients who were admitted to the Neurosurgery Department of AIIMS, New Delhi, during June–December 2006 and met the inclusion criteria [Appendix 1]. The subject data sheet and procedure of amikacin sulfate bladder wash was developed under the guidance of a guide (Author 3) and co-guides (Authors 2 and 4), and was further validated by six experts from the Departments of Neurosurgery, Microbiology, and Nursing, AIIMS.
Informed written consent was taken from the patients or patients' relatives after providing appropriate information to the concerned. Confidentiality of the data was ensured. They were randomized after catheterization to either of the two groups – study and the control groups. Then urine samples were sent within 24 hours for culture and sensitivity (C/S), in case of positive C/S, patients were excluded from the study [Appendix 2]. Study group received amikacin sulfate bladder wash twice daily under strict aseptic precautions and the control group did not receive bladder wash [Appendix 3]. Urine C/S was performed on days 3, 7, and then weekly till the removal of catheter or discharge. Both groups received standard catheter care including perineal care; the only difference was the bladder wash. The researcher (Author 1) performed the bladder wash on all patients to eliminate bias. CAUTI was diagnosed when it met the respective criteria [Appendix 4].
Statistical methods
Descriptive and inferential statistical methods were used. Data were analyzed using SPSS-10th version. A probability of <0.05 was accepted as significant. For continuous variables having normal distribution, data were summarized using mean±SD, and the groups were compared using independent t test. Range and median were used for all continuous variables having non-normal distribution (age and duration of catheterization) and the two groups were compared using Mann-Whitney U test. Frequency and percentage were used for all categorical variables and the groups were compared using Pearson's chi-square test and Fisher's exact test.
The study was conducted following the approval of ethics committee of All India Institute of Medical Sciences (AIIMS).
Results
Demographic profile of patients
Age of the study subjects ranged from 18–68 years [Table 1]. The groups were homogenous in terms of age, sex, level of consciousness, size of catheter and duration of catheterization, and systemic usage of steroids and antibiotics. Bladder wash was well tolerated by all the subjects in the study group.
Table 1.
Age, sex, and duration of catheterization (n=60)
| Variables | Study group n = 30 | Control group n = 30 | P value |
|---|---|---|---|
| Age (years) | 19–65 (38) | 18–68 (42.5) | 0.399 |
| Males (%) | 16 (53) | 16 (53) | 1.0 |
| Females (%) | 14 (47) | 14 (47) | - |
| Duration of catheterization (days) | 3–29 (7) | 4–20 (8) | 0.823 |
Incidence of catheter-associated urinary tract infection and predisposing factors
Incidence of CAUTI was 40% in the control group [Figure 1]. None of the subjects from the bladder wash group developed CAUTI. Amikacin bladder wash was effective in preventing CAUTI (P < 0.001). Lower levels of consciousness (i.e. the Glasgow coma scale (GCS)) increased the risk of developing CAUTI (P = 0.026) [Table 2].
Figure 1.
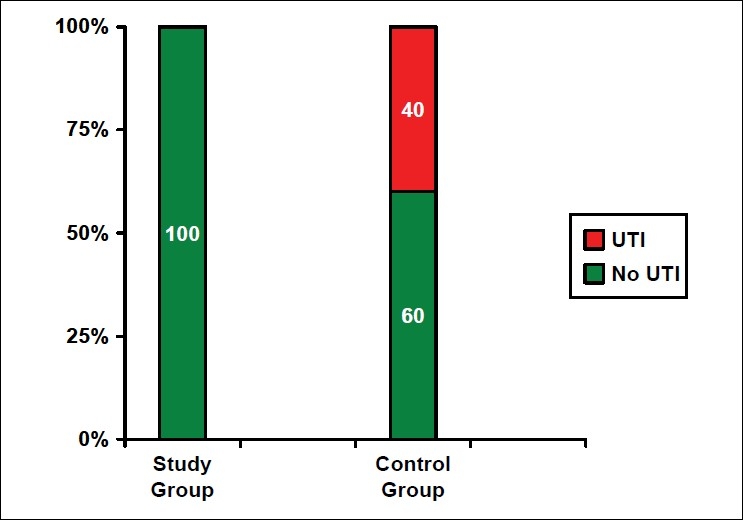
Effect of amikacin sulfate bladder wash on catheter-associated urinary tract infection
Table 2.
Risk factors for catheter-associated urinary tract infection (n=60)
| Factors | UTI-positive group n = 12 | UTI-negative group n = 18 | P value |
|---|---|---|---|
| Age (years) | 18–68 (46.5) | 20–55 (41.5) | 0.280 |
| Sex | 0.457 | ||
| Females | 7 (50) | 7 (50) | |
| Males | 5 (31.3) | 11 (68.7) | |
| Motor score of GCS | 0.026* | ||
| M 1–3 | 5 (83.4) | 1 (16.6) | |
| M 4–6 | 7 (29.2) | 17 (70.8) | |
| Catheter size | 0.131 | ||
| 12 | 0 | 2 (100) | |
| 14 | 7 (36.8) | 12 (63.2) | |
| 16 | 5 (71.4) | 2 (28.6) | |
| 18 | 0 | 2 (100) | |
| Duration of catheterization | 6–20 (9) | 4–14 (7.5) | 0.135 |
| Systemic antibiotics | 0.255 | ||
| Yes | 12 (44.4) | 15 (55.6) | |
| No | 0 | 3 (100) | |
| Steroids | 0.643 | ||
| Yes | 7 (36.8) | 12 (63.2) | |
| No | 5 (45.5) | 6 (54.5) |
Organism and sensitivity profile
P. aeruginosa was the most common organism responsible for 51% of CAUTI [Figure 2]. P. aeruginosa was completely sensitive to amikacin sulfate, cefaperazone plus sulbactam, and piperacillin plus tazobactam, while it was completely resistant towards ceftazidime.
Figure 2.
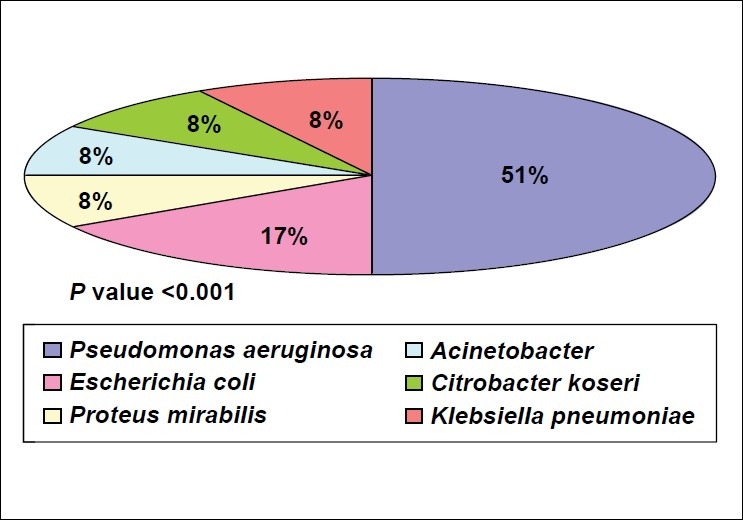
Pathogens causing catheter-associated urinary tract infection
Discussion
The present study is the first of its kind in which the effect of amikacin bladder wash has been analyzed. Efficiency of bladder irrigation using various different solutions have been studied in the past in an attempt to reduce the incidence of CAUTI, majority of the investigators found it to be a time consuming and costly procedure that did not have an impact on CAUTI.[11–15] In contrast, the present study revealed that amikacin bladder wash is effective in preventing CAUTI. In previous studies, the incidence of CAUTI ranged from 11.0–73.3%.[16,17] In the present study, incidence of CAUTI was 40% since those who were catheterized for less than three days were excluded in the study. This inclusion criterion might be the chief reason for a higher incidence of CAUTI in the present study.
CAUTI increases the burden of the patient in terms of increased morbidity and mortality, prolonged hospital stay, and cost of the tests and medicines.[17–19] Tambyah et al.,[20] found that CAUTI had been responsible for an additional of USD589 per CAUTI in diagnostic tests and in medications. The present study reveals that amikacin sulfate bladder wash is effective in preventing CAUTI. As a vial of amikacin sulfate (500 mg) costs INR58 (approximately USD1.4), this is very cost effective especially in a developing country like ours.
Puri et al.,[21] in their study said that the risk was significantly higher for females, elderly patients, critically ill patients, and those on prolonged catheterization. The present study showed only severity of the disease (low motor score of GCS) as a statistically significant risk factor. This might be since a lower GCS corresponds to the severity of tissue injury, where there is hypermetabolism and increased protein catabolism, which eventually leads to decreased immunity that makes the person more susceptible to infections. However, the present study did not show any influence of sex, age, catheter size, duration of catheterization, and systemic use of antibiotics and steroids. This might be because of the small sample size and inclusion of long-term catheterized patients only.
Pathogenic organisms responsible for CAUTI and their antibiotic sensitivity pattern vary with time. In a study, Jha et al.,[22] found that most common organisms responsible for CAUTI were E. coli (49%), S. aureus (23%), Proteus spp. (3.6%), Klebsiella (9.71%), Pseudomonas (0.8%), and Citrobacter (2.8%). Whereas in the present study, Pseudomonas (51%), E. coli (17%), Proteus spp., Citrobacter, Klebsiella, and Acinetobacter (8% each) were the most common. Similarly, antibiotic resistance pattern also varied. In their study, Taneja et al.,[23] found the highest frequency of antibiotic resistance was for ciprofloxacin (68.6%) followed by netilmicin (60.7%), ceftazidime (58.8%), imipenem (43.7%), amikacin (43.1%), and piperacillin (39.2%). In the present study, the pattern of antibiotic resistance was ceftazidime (100%), netilmicin (83%), imipenem (75%), ciprofloxacin (75%), and meropenem (60%).
In this study, we have shown that amikacin sulfate bladder wash is very effective in preventing CAUTI. Thus it can be included in the routine catheter care, especially if catheterization is needed for more than five days. It is easy to implement and cost effective. The main limitation of this study was the small sample size and the fact that the main researcher was not blinded to the study.
Conclusions
There is a varying pattern of antibiotic sensitivity and resistance in different institutions. The most important thing to note is the fact that the bacteria have started developing resistance to higher antibiotics. This is very important since the indiscriminate use of antibiotics can lead to resistance, thus potentially endangering the life of a patient. This increasing resistance calls for immediate measures to use methods other than oral or parenteral antibiotics in CAUTI. We believe that this study is important because if used can decrease the development of CAUTI.
Appendix 1
Inclusion criteria
Informed consent
Age above 18 years
Patients available within 24 hours of catheterization
Appendix 2
Exclusion criteria
Past history of recurrent UTI
Urine culture positive within 24 hours after enrolment in to the study
Immunocompromized patients (AIDS, chemotherapy)
History of diabetes
Patients with renal insufficiency
Catheter removed before third day
Appendix 3
Amikacin sulfate bladder wash
Hundred milligrams amikacin sulfate is added to 500 ml normal saline and 250 ml of this solution is instilled into the bladder through a Foleys catheter (with drainage tube clamped) using an IV set. Solution is allowed to remain in the bladder for 15 minutes and then drained. This is done twice daily.
Appendix 4
Catheter-associated urinary tract infection–
The diagnosis of catheter-associated urinary tract infection can be made when the urine culture shows 105 CFU/ml of urine from a catheterized patient.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kunnin CM. Genitourinary infections in the patient at risk: Extrinsic risk factors. Am J Med. 1984;76:31–9. doi: 10.1016/0002-9343(84)90255-9. [DOI] [PubMed] [Google Scholar]
- 2.Schaeffer AJ. Catheter associated bacteriuria. Urol Clin North Am. 1986;13:35–47. [PubMed] [Google Scholar]
- 3.Stamm WE. Catheter-associated urinary tract infections: Epidemiology, pathogenesis, and prevention. Am J Med. 1991;91:65S–71S. doi: 10.1016/0002-9343(91)90345-x. [DOI] [PubMed] [Google Scholar]
- 4.Burke JP, Riley DK. Nosocomial urinary tract infection. In: Mayhall CG, editor. Hospital epidemiology and infection control. Baltimore: Williams and Wilkins; 1996. pp. 139–53. [Google Scholar]
- 5.Warren JW. Catheter-associated urinary tract infections. Infect Dis Clin North Am. 1997;11:609–22. doi: 10.1016/s0891-5520(05)70376-7. [DOI] [PubMed] [Google Scholar]
- 6.Kunin CM. Urinary tract infections: Detection, prevention and management. 5th ed. Baltimore: Williams and Wilkins; 1997. Care of the urinary catheter; pp. 227–99. [Google Scholar]
- 7.Nicolle LE. Prevention and treatment of urinary catheter-related infections in older patients. Drugs Aging. 1994;4:379–91. doi: 10.2165/00002512-199404050-00003. [DOI] [PubMed] [Google Scholar]
- 8.Al Sweih N, Jamal W, Rotimi VO. Spectrum and antibiotic resistance of uropathogens isolated from hospital and community patients with urinary tract infections in two large hospitals in Kuwait. Med Princ Pract. 2005;14:401–7. doi: 10.1159/000088113. [DOI] [PubMed] [Google Scholar]
- 9.Rew M. Use of catheter maintenance solutions for long-term catheters. Br J Nurs. 1999;8:708–15. doi: 10.12968/bjon.1999.8.11.6585. [DOI] [PubMed] [Google Scholar]
- 10.Chamberlain G, Needham P. The absorption of antibiotics from the bladder. J Urol. 1976;116:172–3. doi: 10.1016/s0022-5347(17)58731-5. [DOI] [PubMed] [Google Scholar]
- 11.Dudley MN, Barriere SL. Antimicrobial irrigations in the prevention and treatment of catheter-related urinary tract infections. Am J Hosp Pharm. 1981;38:59–65. [PubMed] [Google Scholar]
- 12.Van Den Broek PJ, Daha TJ, Mouton RP. Bladder irrigation with povidone-iodine in prevention of urinary-tract infections associated with intermittent urethral catheterisation. Lancet. 1985;1:563–5. doi: 10.1016/s0140-6736(85)91217-6. [DOI] [PubMed] [Google Scholar]
- 13.Muncie HL, Jr, Hoopes JM, Damron DJ, Tenney JH, Warren JW. Once-daily irrigation of long-term urethral catheters with normal saline: Lack of benefit. Arch Intern Med. 1989;149:441–3. [PubMed] [Google Scholar]
- 14.Elliott TS, Reid L, Rao GG, Rigby RC, Woodhouse K. Bladder irrigation or irritation? Br J Urol. 1989;64:391–4. doi: 10.1111/j.1464-410x.1989.tb06049.x. [DOI] [PubMed] [Google Scholar]
- 15.Schneeberger PM, Vreede RW, Bogdanowicz JF, van Dijk WC. A randomized study on the effect of bladder irrigation with povidone-iodine before removal of an indwelling catheter. J Hosp Infect. 1992;21:223–9. doi: 10.1016/0195-6701(92)90079-2. [DOI] [PubMed] [Google Scholar]
- 16.Stamm AM, Coutinho MS. Urinary tract infection associated with indwelling bladder catheter: Incidence and risk factors. Rev Assoc Med Bras. 1999;45:27–33. doi: 10.1590/s0104-42301999000100007. [DOI] [PubMed] [Google Scholar]
- 17.Danchaivijit S, Dhiraputra C, Cherdrungsi R, Jintanothaitavorn D, Srihapol N. Catheter associated UTI. J Med Assoc Thai. 2005;88:S26–30. [PubMed] [Google Scholar]
- 18.Platt R, Polk BF, Murdock B, Rosner B. Mortality associated with nosocomial urinary-tract infection. N Engl J Med. 1982;307:637–42. doi: 10.1056/NEJM198209093071101. [DOI] [PubMed] [Google Scholar]
- 19.Adukauskienė D, Kinderyte A, Rimantas, Vitkauskiene A. Etiology, risk factors, and outcome of urinary tract infection. Medicina (Kaunas) 2006;42:805–9. [PubMed] [Google Scholar]
- 20.Tambyah PA, Maki DG. Catheter-associated urinary tract infection is rarely symptomatic: A prospective study of 1,497 catheterized patients. Arch Intern Med. 2000;160:678–82. doi: 10.1001/archinte.160.5.678. [DOI] [PubMed] [Google Scholar]
- 21.Puri J, Mishra B, Mal A, Murthy NS, Thakur A, Dogra V, et al. Catheter associated urinary tract infections in neurology and neurosurgical units. J Infect. 2002;44:171–5. doi: 10.1053/jinf.2002.0968. [DOI] [PubMed] [Google Scholar]
- 22.Jha N, Bapat SK. A study of sensitivity and resistance of pathogenic microorganisms causing UTI in Kathmandu valley. Kathmandu Univ Med J. 2005;3:123–9. [PubMed] [Google Scholar]
- 23.Taneja N, Meharwal SK, Sharma SK, Sharma M. Significance and characterisation of pseudomonads from urinary tract specimens. J Commun Dis. 2004;36:27–34. [PubMed] [Google Scholar]


