Abstract
Summary: Much remains to be learned about the pathogenesis of the different manifestations of dengue virus (DENV) infections in humans. They may range from subclinical infection to dengue fever, dengue hemorrhagic fever (DHF), and eventually dengue shock syndrome (DSS). As both cell tropism and tissue tropism of DENV are considered major determinants in the pathogenesis of dengue, there is a critical need for adequate tropism assays, animal models, and human autopsy data. More than 50 years of research on dengue has resulted in a host of literature, which strongly suggests that the pathogenesis of DHF and DSS involves viral virulence factors and detrimental host responses, collectively resulting in abnormal hemostasis and increased vascular permeability. Differential targeting of specific vascular beds is likely to trigger the localized vascular hyperpermeability underlying DSS. A personalized approach to the study of pathogenesis will elucidate the basis of individual risk for development of DHF and DSS as well as identify the genetic and environmental bases for differences in risk for development of severe disease.
INTRODUCTION
Dengue virus (DENV) belongs to the family Flaviviridae, genus Flavivirus, and is transmitted to humans by Aedes mosquitoes, mainly Aedes aegypti. Based on neutralization assay data, four serotypes (DENV-1, DENV-2, DENV-3, and DENV-4) can be distinguished. DENV infection is a major cause of disease in tropical and subtropical areas, with an estimated 50 million infections occurring each year and more than 2.5 billion people being at risk of infection (75). Infection with any of the DENV serotypes may be asymptomatic in the majority of cases or may result in a wide spectrum of clinical symptoms (87), ranging from a mild flu-like syndrome (known as dengue fever [DF]) to the most severe forms of the disease, which are characterized by coagulopathy, increased vascular fragility, and permeability (dengue hemorrhagic fever [DHF]). The latter may progress to hypovolemic shock (dengue shock syndrome [DSS]). In Asia the risk of developing severe disease is greater in DENV-infected children (≤15 years) than in adults (30, 80, 109, 172). In contrast, in the Americas mainly the adult population is affected, resulting in mild disease (84, 186, 188), although an increasing trend of cases progressing toward DHF/DSS has also been observed in adults there (75, 79, 87, 126, 186). DF is manifested as an incapacitating disease in older children, adolescents, and adults. It is characterized by the rapid onset of fever in combination with severe headache, retro-orbital pain, myalgia, arthralgia, gastrointestinal discomfort, and usually rash. Minor hemorrhagic manifestations may occur in the form of petechiae, epistaxis, and gingival bleeding. Leukopenia is a common finding, whereas thrombocytopenia may occasionally be observed in DF, especially in those with hemorrhagic signs (76, 109). The World Health Organization (WHO) classifies DHF in four grades (I to IV). DHF grades I and II represent relatively mild cases without shock, whereas grade III and IV cases are more severe and accompanied by shock. DHF is characterized by all the symptoms of DF, in combination with hemorrhagic manifestations (positive tourniquet test or spontaneous bleeding), thrombocytopenia, and evidence of increased vascular permeability (increased hemoconcentration or fluid effusion in chest or abdominal cavities). The life-threatening DSS stage occurs at the time of or shortly after defervescence, which is characterized by a rapid, weak pulse (≤20 mm Hg) or hypotension with cold, clammy skin in the early stage of shock (grade III). If patients do not receive prompt and appropriate treatment, a stage of profound shock may set in, in which pulse and blood pressure become undetectable (grade IV), resulting in death within 12 to 36 h after onset of shock (262a). It is important to realize that the WHO case definition was originally proposed as a tool for clinical diagnosis using the results of repeated clinical tests. The WHO classification system poses a problem for everyday clinical practice, because it may be not sufficiently accurate in correctly classifying disease severity and may lack good agreement with clinical practice (213). Consequently, the WHO classification system is currently being reconsidered, and a new classification system is to be expected soon. The stage of prolonged shock may trigger or accelerate the development of disseminated intravascular coagulation (DIC) (228). Data that support or refute the occurrence of DIC in severe dengue are inconclusive, so better studies using prospective cohorts are needed to show the frequency of DIC in DHF/DSS patients and its association with clinical outcome (30, 152, 262). Massive loss of blood is rare in DHF and DSS and if present it is largely restricted to the gastrointestinal tract. This is usually due to prolonged shock resulting in blood being shunted away from the gastrointestinal tract, leading to anoxia, cell death, and gastrointestinal bleeding. In contrast, the mild forms of hemorrhages seen early in infection, such as petechiae, result from different mechanisms related to virus infection in combination with the release of vasculogenic cytokines. Understanding the mechanism underlying the development of shock is crucial for the development of novel strategies to improve patient management. It is worth noting that patients classified as having DHF and DSS have no generalized edema; rather, a selective plasma leakage tends to occur in the pleural and abdominal cavities (12, 230, 246, 252, 256), which is detectable by means of radiology or sonography. Ultrasonographic examinations have revealed that plasma leakage occurs before defervescence or changes in hemoconcentration become apparent (12, 230, 252). Attempts to explain the pathogenesis of dengue in all its complexity must consider all the clinical, immunological, pathological, and epidemiological features of DENV infection. The aim of this review is to outline the current views of DHF/DSS pathogenesis and to identify the gaps in our knowledge that represent critical challenges for the future.
THE PATHOGENESIS OF DENV INFECTIONS: CURRENT HYPOTHESES
DENV Tropism
Cell and tissue tropism of DENV may have a major impact on the outcome of DENV infections. The absence of an appropriate animal disease model largely hampers our understanding of the role played by DENV tropism. In vitro data and autopsy studies suggest that three organ systems play an important role in the pathogenesis of DHF/DSS: the immune system, the liver, and endothelial cell (EC) linings of blood vessels. The tropism of DENV for cells of the respective systems, the corresponding pathological effects of DENV infection of these systems, and the relevance of these events for the overall pathogenesis of DENV infection will be described.
Cells of the immune system.
During the feeding of mosquitoes on humans, DENV is presumably injected into the bloodstream, with spillover in the epidermis and dermis, resulting in infection of immature Langerhans cells (epidermal dendritic cells [DC]) (136, 263), and keratinocytes (136). Infected cells then migrate from site of infection to lymph nodes, where monocytes and macrophages are recruited, which become targets of infection. Consequently, infection is amplified and virus is disseminated through the lymphatic system. As a result of this primary viremia, several cells of the mononuclear lineage, including blood-derived monocytes (59), myeloid DC (20, 91, 92, 123, 133), and splenic and liver macrophages (18, 54d, 96, 101, 117) are infected. DENV has also been shown to have tropism for circulating mononuclear cells in blood and for cells residing in the spleen, lymph nodes, and bone marrow of infected AG129 mice (124). Leukocytes also have been shown to be infected with DENV in experimentally infected nonhumans primates (156). It should be noted that during secondary infections with heterologous DENV, high concentrations of DENV-specific immunoglobulin G (IgG) will complex newly produced virus that adheres to and is taken up by mononuclear cells. Following infection, mononuclear cells predominantly die by apoptosis (61, 182), while abortively infected or bystander DC are stimulated to produce the bulk of mediators that are involved in inflammatory (22, 47, 91, 133, 145) and hemostatic (48, 60, 97, 120, 236) responses of the host. In this regard, factors that influence the amount of target cells infected, and consequently the levels of viremia, may determine the ratio of different proinflammatory and anti-inflammatory cytokines, chemokines, and other mediators, as well as the way in which the inflammatory response affects the hemostatic system (35, 59). Bone marrow stromal cells have also been shown to be susceptible to infection with DENV (124, 171, 202).
Organ pathology.
Although thousands of patients with confirmed dengue have been recognized in Southeast Asia and the Americas in the past 60 years, autopsies have been performed on only a small number of these patients, and whether those cases are representative in reflecting the viral tropism in the acute phase of infection is unclear. Histopathological research is difficult to perform because fatal cases of DHF/DSS are rare and occur mainly in remote parts of the world where appropriate laboratory technology is largely lacking and thus fresh or frozen patient materials are rare. In addition, due to cultural and religious practices, autopsy is not conducted on the majority of fatal cases, and usually families opt for rapid burial or cremation. The interpretation of the pathological findings in fatal cases of DHF/DSS in relation to viral tropism described in the literature is complicated by a skewed age distribution, different times of sample collection, and the range of different techniques used to confirm the presence of virus in affected tissues. DENV cell tropism can be inferred from studies that had used in situ hybridization, immunohistochemistry, or a combination of PCR and virus isolation techniques. A review of the literature describing findings on autopsy samples from a total of 160 fatal cases, mostly children or young adolescents (4 to 18 years old) who died within 36 h of developing shock, revealed, in order of frequency, the presence of DENV in cells in the skin (104), liver (13, 14, 53, 54d, 69, 96, 101, 104, 137, 164, 173, 199, 208), spleen (13, 14, 101, 164, 199, 208), lymph node (13, 14, 101, 104, 173, 199, 208), kidney (14, 78, 101), bone marrow (13, 78, 101, 173), lung (13, 78, 101, 137, 164, 173), thymus (106), and brain (164). The presence of infectious virus in these samples was not always investigated, but in general virus could be isolated only from liver and peripheral blood mononuclear cells. The failure to isolate virus from most organ samples may indicate that those tissues contained primarily degraded virus or virus complexed with antibodies that prevent infection of cells in vitro. In general, the presence of DENV in several organs was not associated with gross or microscopic evidence of severe organ pathology (17), which is in agreement with the pathogenesis of DHF/DSS. Similar organ tropism has been observed in the primate model, with high concentrations of virus isolated from the skin and gastrointestinal tract whereas low concentrations of virus were recovered from the spleen, thymus, and several peripheral lymph nodes (157). DENV has been recovered from the spleen, liver, peripheral lymph nodes, and central nervous system in alpha/beta interferon (IFN-α/β)-deficient mice (13, 267). One notable difference between humans and the mouse model is the tropism of DENV for neuronal cells.
It is interesting to note that a generally used argument in the literature is that when shock sets in, virus is no longer detectable in blood and therefore the host response should play a key role in pathogenesis (134, 166). Most autopsy data did not specifically compare the presence of viral antigens or nucleic acid in blood and autopsy samples, but the limited evidence suggests that DENV replication may occur in some organs, while viremia is no longer detectable (199). In agreement with these findings it was shown in the rhesus macaque model that DENV could be recovered from some autopsy samples but not from blood.
The liver is commonly involved in DENV infections in humans and mouse models (181, 212), with some reports suggesting an association between elevated liver enzyme levels and spontaneous bleeding tendencies (54e, 124, 261). Cases of dengue-associated hepatitis have been described, which were characterized by moderate midzonal hepatocyte necrosis, microvesicular steatosis, and councilman bodies (63, 78, 124, 181, 254). Although DENV was found in a significant proportion of human hepatocytes and Kupffer cells, little inflammation was seen within the liver, indicating that much of the observed apoptosis and necrosis was virally induced. The higher prevalence of apoptosis over necrosis could explain the limited inflammation seen in the liver, a picture similar to what is observed in the early phase of yellow fever or Rift Valley fever (57, 190, 191). It has been proposed that the severe hepatic damage seen, for instance, in yellow fever, Rift Valley fever, and late Ebola virus infections results in decreased liver function, which could account for the decreased synthesis of coagulation factors and development of coagulopathy (43, 269). Although severe hepatic damage is not common in DENV infections, elevated liver enzymes suggest that the liver is affected, but the role of hepatic damage in coagulopathy and disease severity remains to be established.
EC.
EC play an important role in the coagulation response upon severe systemic inflammation. The integrity of the EC bed is physiologically regulated by many factors. The tropism of DENV for EC in vivo remains controversial. Early studies of skin biopsy specimens indicated that the microvasculature located in the dermal papillae is the main site affected, although DENV antigen was not detected in EC but was detected in cells surrounding the microvasculature (21, 203). In contrast, there is evidence for the presence of DENV antigen in the pulmonary vascular endothelium (101). It is important to realize, however, that the mere presence of viral RNA or antigen in EC is no proof for viral replication. In contrast to mononuclear cells, EC do not carry Fc receptors and thus will not take up immune-complexed virus. Therefore, the presence of viral RNA in these cells would more likely be explained by a mechanism of pinocytosis (101). In vitro studies have shown that all DENV serotypes can actively replicate in EC (7, 19, 95), and infection results in functional rather than morphological damage. It is not clear whether EC of different vascular-bed systems have different susceptibilities to DENV infection. In this regard, it has been proposed that the coagulation responses upon severe systemic inflammation by EC in different parts of the vascular-bed system are not the same (200, 201). Similarly, DENV infection patterns in microvascular cells in vitro suggest that EC from different tissues have different activation patterns (184). Although increased peripheral microvascular permeability has been shown to occur in both DHF and DSS patients (16), it is conceivable that EC from the pulmonary and abdominal territories react in a specific way to either infection with or the response to DENV infection (28, 39), resulting in the selective vascular leakage syndrome characteristic of DHF/DSS. Several studies suggest that vascular damage or dysfunction is central in the pathogenesis of DHF/DSS (26, 29, 39, 115, 168). It is interesting to note that selective apoptosis of the microvascular EC in pulmonary and intestinal tissues has been detected in fatal cases of DHF/DSS (137), providing a possible explanation for the profound plasma leakage seen in pleural and peritoneal cavities. In this regard, it is worth mentioning that the major nonstructural protein 1 (NS1) of DENV has been shown to bind preferentially to EC of lung and liver tissues (9). It has been hypothesized that recognition of NS1 by anti-NS1 antibodies could then contribute to the selective pulmonary vascular leakage.
Virus Virulence
According to the virus virulence hypothesis, certain DENV strains are responsible for more severe disease. DENV serotypes can be further classified into different genotypes on the basis of nucleotide variations. Viral genetic differences have been associated with differences in virulence (51, 131, 206, 248). Remarkably, the first outbreak of DHF in the Americas occurred in 1981, which coincided with the introduction of the possibly more virulent DENV-2 Southeast Asian genotype, while the less virulent indigenous DENV-2 genotype was already circulating in the region (118, 195-197). It has also been proposed that intraepidemic evolution of the circulating DENV might be responsible for increased severity of disease. During the 1981 DENV-2 epidemic in Cuba, it was noted that severity of disease manifestations and case-fatality rates were increased toward the end of the epidemic (118, 119), suggesting that the circulating DENV-2 might have become more virulent through passage in hosts during the epidemic. A similar situation was observed in the 1992 DENV epidemic in Townsville, Australia (234), and again in Cuba during the 1997 epidemic (81). Analysis of DENV genomes has shown that DENV indeed evolves during an epidemic (42, 198); however, more data are needed to establish an association between intraepidemic virus evolution and increased disease severity. Epidemiological observations in the Americas and in Singapore suggested that the sequence of infection with particular serotypes and the time interval between primary infection and secondary infection may play an important role in the development of DHF. Epidemics with high incidences of DHF have been linked to primary infection with DENV-1 followed by infection with DENV-2 or DENV-3 (79, 83, 178). Furthermore, these studies indicated that the longer the interval between primary and secondary infections, the higher the risk of developing severe disease. In addition, age has been shown to influence the outcome of disease following a secondary infection with heterologous DENV (80). In Asia, the risk of severe disease is greater in children than in adults, in contrast to the Americas, where the adult population is mainly affected and infection results in milder disease. This difference in disease severity caused by Asian and American genotypes correlated with structural differences in the two strains of DENV (51, 131). It has also been shown that different geographical DENV strains or different serotypes may vary in their ability to infect different cell types or cause severe disease (56, 251). However, the observation that DHF/DSS is seen primarily in a relative small percentage of secondary DENV infections and to a much lesser extent in primary infections even with allegedly virulent strains suggests that host factors must be crucial determinants of severe disease development. It is important to realize that virulence has traditionally been considered a microbial property, evaluated independently of the host or only in vitro or in often inbred animals. However, an increasing body of evidence incriminates the host immune response in the pathogenesis of many microbial infections (31). Therefore, in studying DENV virulence, both host and viral factors should be considered.
Activation of the Complement System
The complement system is one of the main humoral components of the innate immunity and interacts closely with the hemostatic system to provide the first line of defense against pathogens. These innate immune mechanisms provide the host with the time needed to maximally induce the more slowly developing adaptive immunity. With regard to DENV, investigators noticed that around the time of defervescence, when plasma leakage may become apparent, high levels of the activation products C3a and C5a are measured in the plasma, followed by an accelerated consumption and a marked reduction of the complement components in patients with DSS (50, 174, 214). Therefore, it was hypothesized that complement activation plays an important role in the pathogenesis of dengue. Comparison of global gene expression profiles in peripheral blood mononuclear cells of DF and DHF/DSS patients also suggests the involvement of the complement system in disease severity (249). However, many aspects of complement activation and its role in DENV pathogenesis remain to be investigated.
It has been proposed that NS1 is an important trigger for complement activation (122). Binding of heterotypic antibodies to NS1 expressed on infected cells may result in complement activation (8, 142). In addition, it is believed that NS1 released from infected cells can directly activate complement factors present in the fluid phase (122). Production of the C5b-C9 complex could then trigger cellular reactions and stimulate the production of inflammatory cytokines that are associated with development of DHF/DSS (8). Alternatively, the C5b-C9 complex could independently trigger other local and systemic effects (158), which may be implicated in intravascular coagulation. It is important to realize that coagulation enzymes can also activate the complement system, illustrating the extensive interaction that exists between the complement and the coagulation system.
Several groups have shown that both IgG1 and IgG3 were the predominant subclasses involved in the specific antibody response in human DENV infections (116, 242). Both IgG subclasses can fix and activate the complement system effectively, whereas IgG2 and IgG4 are less effective in this respect (90). Although IgG1, IgG2, and IgG4 are able to activate the classical complement pathway, they require the unlikely event of two IgG molecules binding close to the antigen in order to promote C1q binding (90). IgG3, on the other hand, has the capacity to self-associate into multivalent complexes, thereby increasing functional affinity and the likelihood of C1q binding. The presence of sialic acid in the glycans of IgG subclasses could also affect their complement-fixing properties (100) and possibly their infection-enhancing activity (65, 163, 266). It is important to understand what determines the threshold of activation needed and how activation participates in development of DHF/DSS.
Transient Autoimmunity
Antibodies produced during a DENV infection have been shown to cross-react with some self-antigens, but it is not clear if production of these antibodies is associated with secondary DENV infections. For instance, antibodies recognizing a linear epitope in the E protein have been shown to bind human plasminogen and inhibit plasmin activity (49, 64, 94, 159). The presence of serum antibodies specific to NS1 also has been shown to correlate with disease severity (134, 218). Cross-reaction of anti-NS1 with cells of the liver, EC, and platelets (33, 140, 177, 237) could be at the basis of this observation. Anti-NS1 antibodies cross-reactive with EC could trigger these cells to express nitric oxide (NO) and undergo apoptosis (141). Although NO has been shown to inhibit DENV replication (239), its overproduction could also lead to cell damage (141, 215). It is worth reiterating that morphological damage is not a common observation in lethal cases of DHF/DSS. Anti-NS1 antibodies have also been shown to enhance expression of interleukin-6 (IL-6), IL-8, and intracellular adhesion molecule 1 (ICAM-1) (138). Further studies are needed to see if cross-reactivity of anti-NS1 with EC could lead to the increased permeability that is characteristic of DSS. In addition, anti-NS1 antibodies were also shown to cross-react with human and mouse platelets and were able to cause transient thrombocytopenia and hemorrhage in mice (142, 237), indicating that such cross-reactive antiplatelet antibodies are pathogenic. This observation may have implications for vaccine development, especially for live-attenuated vaccines. Therefore, it is important to understand why the autoimmune phenomenon observed in some DENV-infected patients does not persist. Since the kinetics of anti-NS1 antibodies is difficult to reconcile with the short duration of the sudden hyperpermeabilty event that leads to shock, the autoimmune hypothesis has remained controversial. Although it is likely that the cross-reactive antibodies to self-antigens are of the short-lived IgM isotype (139, 204), vaccination strategies should not result in memory IgG responses to such antigens. Clearly, more efforts should be deployed in identifying the putative self-antigens that are recognized by anti-DENV antibodies and in understanding their role, if any, in dengue pathogenesis.
Host Genetic Factors
Differences in disease severity can be seen at both the individual and population levels. Several epidemiological studies indicated that genetic factors constitute important components in disease susceptibility. Several human HLA class I and II alleles are associated with development of DHF (Table 1). Polymorphism in the tumor necrosis factor alpha (TNF-α), Fcγ receptor, vitamin D receptor, CTLA-4, and transforming growth factor β (TGF-β) genes has been associated with development of DHF/DSS. Certain host factors, such as glucose-6-phosphate dehydrogenase (G6PD) deficiency, may also contribute to increased replication of DENV in monocytes. Deficiency in G6PD, a ubiquitous X-linked enzyme, is the most common enzyme deficiency worldwide, with high prevalence seen in the African population (175). G6PD deficiency causes abnormal cellular redox, thereby affecting production of nitric oxide, superoxide, and hydrogen peroxide. Oxidative stress is known to affect viral proliferation and virulence by increasing viral receptors on target cells or increasing production of viral particles (264). Although, it is possible that G6PD deficiency provides a more suitable milieu for viral replication, it is worth noting that a low incidence of severe disease was reported in populations of African origin in studies conducted in Cuba and Haiti (54b, 54c). Polymorphism in the mannose-binding lectin 2 (MBL2) gene was shown to be associated with thrombocytopenia and an increased risk for developing DHF. MBL is a member of the collectin family and is assumed to play an important role in pattern recognition and innate immune defense. Mutation in the promoter region of MBL results in low serum levels of MBL, resulting in a common immunodeficiency syndrome present in up to 10% of the U.S. population (243). Polymorphism in transporters associated with antigen presentation and human platelet antigen has also been associated with increased risk for developing DHF (224). The risk to develop DHF and DSS following infection with DENV is likely to be determined by a combination of multiple common genetic traits, each with mild to moderate effects, predisposing to a more severe form of disease. It remains to be determined whether single gene defects that confer profound susceptibility to DENV infection exist, as has been identified for a number of common pathogens, such as pneumococci and mycobacteria (185). In this respect, individuals who develop DHF or DSS but are otherwise healthy may serve as a pool to identify polymorphism and single-gene defects predisposing to the development of the most severe forms of DENV infection.
TABLE 1.
Summary of non-HLA and HLA-associated genetic factors involved in the development of DHF/DSS
| Genetic factor | Reference(s) |
|---|---|
| Vitamin D receptor polymorphism | 143 |
| FcγRIIa polymorphism | 143 |
| G6PD | 35 |
| MBL2 | 1 |
| TGF-β | 45 |
| TNF-α308A polymorphism | 66 |
| CTLA-4 | 45 |
| Transporters associated with antigen presentation and human platelet antigen | 224, 225 |
| DC-SIGN polymorphism | 205 |
| HLA class I alleles A*01, A*0207, A*24, B*07, B*46, B*51 | 144, 232, 270 |
| HLA class II alleles DQ*1, DR*1, DR*4 | 125, 187 |
Antibody-Dependent Enhancement
In most acute virus infection models, the presence of antibodies, both neutralizing and nonneutralizing, correlates with control, elimination, and eventually protection. However, a possible detrimental role of virus-specific antibodies has been described for several viruses as measured by in vitro enhancement of infection of cells (72, 73, 93, 98, 189, 235, 238, 240, 255), a phenomenon that is not restricted to viral pathogens only (150). This in vitro phenomenon was also described for DENV infection (86), and epidemiological studies have shown an increased risk of developing DHF/DSS after a secondary DENV infection (74, 111, 207, 245). Halstead and colleagues observed that the incidence of DHF and DSS peaked in two populations of young children. One peak occurred in infants (at the age of 6 to 9 months) who were infected with a DENV serotype different from that which had infected their mothers. The key observation there was that severe disease occurred in infants for whom maternal antibodies had declined to low, subneutralizing levels. The other peak was observed in young children who had experienced an earlier, usually mild or subclinical, infection and were later infected with a different DENV serotype. These observations led to the conclusion that subsequent infection of preimmune individuals with a different DENV serotype could exacerbate rather than mitigate disease, a phenomenon that was claimed to be caused by antibodies and termed antibody-dependent enhancement (ADE) of disease (85). Several subsequent epidemiological studies provided further circumstantial evidence for the role of preimmunity in the pathogenesis of DHF (25, 80, 82, 112). ADE could result in infection of a higher number of target cells, which could lead to the high viral load observed in many studies (132, 221, 245, 251, 258, 259). Despite several clinical studies, evidence for the role of ADE in human disease, such as in DENV infections, remains circumstantial. Although some studies have shown a correlation between enhancing activity of serum, high levels of viremia, and an increased risk for DHF/DSS (38), not all cases of severe disease are associated with ADE or preceded by infection with a heterologous serotype or by high viral loads. In some cases, when DHF/DSS is seen, the presence of viral RNA became undetectable (132). In general, however, a high viral load and the presence of virus on the day of defervescence are important risk factors for the development of severe disease. As stated above, it is not completely clear whether the absence of viremia always correlates with clearance of virus from infected tissues (155, 199).
An alternative or complementary hypothesis is that FcγR-mediated entry suppresses the antiviral immune response. For instance, a study with Ross River virus showed that viral entry via the FcγR pathway could suppress antiviral genes and enhance IL-10 production in murine macrophages, while entry via the normal cellular receptor did not change the antiviral environment (135, 151). Furthermore, it was shown that virus replication was necessary in order to promote IL-10 expression. Unfortunately, the Fc receptor that was involved in ADE was not identified. It was also shown that DENV infection of THP-1 cells via FcR suppressed the transcription and production of IL-12, IFN-γ, TNF-α, and NO but enhanced expression of the anti-inflammatory cytokines IL-6 and IL-10 (36), indicating that ADE of DENV infection also resulted in a milieu that promoted viral replication. These results must be interpreted with caution, however, since the effect of ADE of infection on gene expression may be cell dependent (20). This effect of FcγR-mediated entry on the antiviral state is not unique to viral pathogens. For instance, FcγR-mediated infection of murine macrophages with Leishmania amastigotes was required to sustain persistent infection (108, 180, 244). Infection of humans and mice with Leishmania major in the presence of antibodies resulted in development of chronic infection. In this regard, increased levels of IL-10 have been associated with visceral and cutaneous leishmaniases, and IL-10 has been flagged as having an important role in the regulation of the immune response to this parasite, thereby linking ADE to Th2 immune responses. This immunosuppressive effect of FcγR-mediated infection is in agreement with the decrease in the proliferative responses to mitogen and recall antigens that can be measured during acute DENV infection, which is associated with both quantitative and qualitative defects in the antigen-presenting cell (APC) population (148, 161).
The role of preimmunity conferred by vaccination against DENV or other flaviviruses in the pathogenesis of DENV infections has been studied in limited numbers of subjects. Most clinical trials with candidate DENV vaccines were conducted in areas where the disease is not endemic and the chance of acquiring a natural infection is limited. One study conducted in Thailand reported no differences in the incidence of DHF in children who had received a live-attenuated DENV vaccine and unvaccinated controls at 6 to 8 years after vaccination (34). Experimental infection of monkeys with DENV-1 or DENV-4 followed by a secondary infection with DENV-3 a year later did not result in increased viremia or disease (113). The efficacy of DENV candidate vaccines was also not influenced by preimmunity to DENV or other flaviviruses (77, 114). The results from these experimental studies should be interpreted with caution, however, since the interval between primary and secondary infection may have been too short.
Cross-Reactive T-Cell Response
Although memory T cells cross-reactive with a heterologous virus can provide partial protective immunity, they can also cause substantial immunopathology (210). The role of CD8+ T cells during DENV infection is not entirely clear, but they may play a role in clearing infection as well as in immunopathogenesis (3, 166). It is worth noting that a consistent finding in all examples of T-cell-mediated pathology during acute or persistent viral infections is morphological tissue damage as a result of cytolysis or inflammation induced by the high numbers of effector T cells. The efficiency of activated T cells in clearing virus-infected cells is dependent on the avidity of the T-cell receptor (TCR) for the HLA-peptide complex (222), and it is assumed that cross-reactive T cells of low avidity for heterologous virus are not protective (110). Yet, there are only a handful of virus-animal models where heterologous immunity has been shown to cause pathology. These include the combinations of infections with lymphocytic choriomeningitis virus (LCMV) and vaccinia virus (VV), as well as influenza A virus (IAV) and murine cytomegalovirus (MCMV) (209). In one study, peripheral VV infection of LCMV-immune mice resulted in immune-mediated panniculitis (211), whereas respiratory VV challenge of LCMV-immune mice resulted in recruitment of LCMV-specific CD8+ T cells into the lung, causing bronchiolitis obliterans (40). In the IAV-MCMV model it was shown that IAV-immune mice challenged with MCMV developed severe consolidating mononuclear pneumonia as a result of increased viral replication in the lungs (41, 209). One example of cross-reactivity leading to disease in humans has also been described (250, 260). The authors of those studies reported two cases of fulminant hepatitis C virus infection associated with an unusually high frequency of CD8+ T cells. These T cells were shown to recognize a single epitope within the hepatitis C virus NS3 that also cross-reacted with an epitope in the IAV neuraminidase protein. These findings suggest that cross-reactive memory T cells can modify the primary immune response and modulate the immunopathologic response to subsequent infection with other pathogens.
During the acute phase of a secondary infection of humans with heterologous DENV, highly cross-reactive CD8+ T cells with high avidity for the infecting virus are preferentially activated (58, 99). The majority of these cross-reactive T cells produce high concentrations of pro- and anti-inflammatory cytokines such as IFN-γ, TNF-α, and IL-13 but somewhat lower levels of IL-10. These high-avidity cross-reactive CD8+ T cells die through apoptosis, but it is not clear whether cells die as a result of activation-induced cell death or whether apoptosis is selectively induced by cross-reactive epitopes. Other studies have also suggested that epitopes can regulate the level of proinflammatory cytokines produced by T cells (146, 147). Alternatively, low-avidity cross-reactive CD8+ T cells would be preferentially expanded (165, 166). These cross-reactive T cells react differently to the heterologous epitopes than to homologous epitopes by producing high levels of proinflammatory cytokines, but they lose their cytolytic activity. Delayed virus clearance would prolong activation of such cross-reactive CD8+ T cells, which then results in the production of high levels of cytokines such as TNF-α, IL-6, or other soluble factors that affect vascular permeability. The phenomenon where cross-reactive memory T cells for the primary infecting virus are more efficiently activated, due to the increased frequency and higher activation state of memory cells, has been called original antigenic sin (OAS). This phenomenon has also been described for LCMV in mice (110). During a secondary infection with a heterologous serotype, cross-reactive epitopes preferentially reactivate the larger number of memory T cells against the priming virus more effectively than they activate naïve T cells. However, in accordance to what has been described for several other systems, it is possible that during a heterologous DENV infection, only a very small subset of cross-reactive memory T cells will be stimulated to expand because of a narrowing TCR repertoire. This narrowing of the TCR repertoire in combination with the fact that each individual has a unique TCR specificity (private TCR [52, 107]) would result in dominant responses that are unique for individuals. This could explain the variability seen in disease outcome upon secondary infection with heterologous DENV. Much less is known about the CD4+ T-cell response during DENV infection. However, evidence exists that sequential infection with different DENV serotypes may also alter the cytokine response of cross-reactive CD4+ T cells, resulting in production of proinflammatory cytokines (154) that may contribute, together with the CD8+ T-cell response, to a detrimental cytokine release.
Soluble Factors
It is strongly believed by many scientists studying dengue pathogenesis that a high viral load and activation of high numbers of nonprotective T cells result in a “storm” of inflammatory cytokines and other mediators, leading to the increased plasma leakage characteristic of DHF/DSS. One of the most daunting challenges in DENV research is the identification of soluble factors that can mediate, either alone or in combination, the functional changes induced in EC that are associated with the increased plasma leakage. Several studies have shown that concentrations of multiple cytokines and other mediators, as well as soluble receptors, are significantly increased during severe dengue infections (reviewed in reference 15). Higher plasma levels of IL-1β, IL-2, IL-4, IL-6, IL-7, IL-8, IL-10, IL-13, IL-18, TGF-1β, TNF-α, and IFN-γ have been found in patients with severe DENV infections, in particular in patients with DSS (10, 23, 32, 103, 128, 169, 172, 183, 192, 194, 236). These studies analyzed samples from infants, children, and adults infected with different DENV serotypes. It is reasonable to assume that synergistic interactions between these cytokines will occur. Other mediators and soluble factors found to be increased in severe disease include vascular endothelial growth factor (VEGF), granulocyte-macrophage colony-stimulating factor, monocyte chemoattractant protein 1 (MCP-1), macrophage migration inhibitory factor, thrombopoietin, soluble vascular cell adhesion molecule 1 (VCAM-1), soluble ICAM-1, von Willebrand factor antigen, thrombomodulin, E-selectin, tissue factor (TF), plasminogen activator inhibitor 1 (PAI-1), and tissue plasminogen activator (23, 26, 27, 29, 44, 46, 115, 130, 153, 223, 229). Analyses of several studies reveal conflicting results, as some studies report increased levels of plasma cytokines while others do not. These discrepancies are attributed mainly to the study design and experimental setup, the laboratory tests used to measure cytokines, and the statistical tests applied for the analyses of the results. Furthermore, the time of sampling during infection is difficult to standardize, and this may explain some of the discrepant results. The observation that plasma leakage occurs mainly in the pulmonary and peritoneal cavities justifies the question whether levels of cytokines and mediators in plasma indeed reflect concentrations in different compartments. Infection of humans and animals with seasonal IAV (H1N1 or H3N2) indicated that levels of cytokines and chemokines were much higher locally, at the site of infection, than in plasma or serum (68, 71, 88). In contrast, H5N1 causes fulminant disease in humans, characterized by diffuse alveolar damage and progression to multiorgan dysfunction. In this case disease severity correlates strongly with cytokine levels, both locally and systemically (54a, 129). For instance, hemophagocytic syndrome has been proposed as a cause of the multiorgan dysfunction observed in patients with confirmed H5N1 fatal infections (247, 268). Notably, hemophagocytic syndrome in fulminant virus infections or autoimmune diseases as well as macrophage activation syndrome in hematopoietic cell transplantation has been associated with excessive cytokine production (127, 193, 227). The production and actions of cytokines are thus critically dependent on the context in which they occur. More specifically designed studies are needed to dissect the relationships between levels of several cytokines in the pulmonary (pleural fluid) and peritoneal (ascites) regions compared to plasma or serum in severe DENV infections. It is conceivable that differences in viral replication and damage to selective EC in vivo may account for a differential cytokine profile, resulting in different vascular permeability patterns.
Some evidence to support a role for cytokines comes from animal models of increased vascular permeability and hemorrhage during DENV infections (39, 217). TNF-α, IL-1β, IL-6, and IL-10 levels have been shown to be high in sera of DENV-infected mice (6). In addition, several in vitro experiments have demonstrated high levels of cytokines in culture supernatants of DENV-infected (primary) DC (20), monocytic cells (47, 162), and EC (11). In the presence of anti-NS1 antibodies, EC produce MCP-1, IL-6, and IL-8 in vitro (138). T cells interacting with DENV-infected cells may also produce TNF-α, IFN-γ, IL-4, and/or IL-10 (91).
The biological roles of some cytokines and soluble factors and the implication in the development of hemorrhage have been inferred and are summarized in Table 2. The cytokines TNF-α and IL-10 are of particular interest. For instance, in one study a positive correlation between soluble TNF-α concentrations and thrombocytopenia was found (23). Furthermore, the TNF-α308A allele, which leads to overproduction of the cytokine, is more commonly found in DHF patients (66). These observations, together with experiments showing that TNF-α is capable of increasing EC permeability in vitro (55), suggest its possible role in pathogenesis of DHF. In a mouse model of DENV-induced hemorrhage, high levels of TNF-α in tissues correlated with EC apoptosis and hemorrhage (39). It is worth noting that in most models of immunopathology, pathology is mediated via direct lysis of infected cells by TNF-α, and it has been shown that CD8+ T-cell cytotoxicity can be mediated exclusively by TNF-α. Plasma levels of IL-10 were shown to correlate with platelet decay in DENV-infected patients (10, 132) and may modulate the activation of coagulation. IL-6 is a major mediator of fever and acute-phase reactions and is produced by macrophages and activated EC. Furthermore, IL-6 and IL-8 mediate derangement of coagulation and fibrinolysis, whereas TNF-α and VEGF act synergistically to induce expression of TF on EC (216). TNF-α has a direct effect on production of IL-6 and thus an indirect effect on coagulation and fibrinolysis. IL-2 plays a central role in the regulation of the immune response, as it induces potent proliferation of T cells and to a lesser extent of B cells, stimulates synthesis of IFN-γ and TNF-α, and may damage the integrity of EC. IL-8 has an effect on the expression of adhesion molecules such as ICAM-1 and VCAM-1. MCP-1 causes EC tight-junction openings in vitro (231) and elevates endothelial permeability changes in vivo (265). IL-13 is a pleiotropic type 2 cytokine, and its receptor is expressed on vascular EC. IL-13 downregulates expression of proinflammatory cytokines IL-1, IL-6, IL-8, and IL-12. Furthermore, IL-13 is a potent stimulator of matrix metalloproteinase 9 (MMP-9) and cathepsins and plays important roles in the pathogenesis of emphysema in animal models of respiratory infections. Interestingly, DENV-infected cells have been shown to produce MMP-9, which increases vascular permeability in vitro (145). IL-18 is a type 1 cytokine, produced mainly by monocytes, macrophages, and DC, and has a strong proinflammatory activity. In vitro, IL-18 upregulates expression of adhesion molecules (E- and P-selectins) on EC, which may contribute to a procoagulant state (167). High levels of IL-18 may be associated with neutropenia, thrombocytopenia, and elevated levels of liver enzymes. During DENV infection, CD4+ T cells have been shown to produce a unique cytokine called the cytotoxic factor, with peak amounts measured in DHF/DSS cases (2, 37). The validity of these observations has to be confirmed by independent experiments.
TABLE 2.
Summary of soluble factors that are or are likely to be associated with development of DHF/DSS
| Soluble factor | Biological function in relation to pathogenesis |
|---|---|
| Thrombin | Thrombin is thought to act near the site at which it is produced. Thrombin converts circulating fibrinogen to fibrin and triggers platelet activation, which results in platelet aggregation. Thrombin activates EC and increases EC permeability, leading to plasma leakage and edema formation. Thrombin is chemotactic for monocytes and is mitogenic for lymphocytes and mesenchymal cells. Activated platelets release several soluble factors with inflammatory, antimicrobial, and immune modulating activity, such as MMP-9, which enhances EC permeability. Activated platelets also secrete soluble CD40 ligand, which can induce EC to produce reactive oxygen species, adhesion molecules, chemokines, and TF. Thrombin also inhibits IL-12 production by mononuclear cells. |
| C3a and C5a | C3a activates platelets and enhances their activation and adhesion properties. C5a enhances blood thrombogenicity by upregulating TF and PAI-1 expression on various cell types. C5a stimulates monocytes to produce IL-1, IL-6, IL-8, and TNF-α. Activation of these complement factors is enhanced by thrombin, which cleaves C3 and C5 to C3a/b and C5a/b, respectively. Activated platelets are also involved in C3 cleavage, which induces activation of the classical complement pathway. |
| C4b | C4b binds to protein S and thereby inhibit the anticoagulant properties of activated protein C-protein S complexes. |
| IL-1 | IL-1β is major mediator of platelet-induced activation of EC, causing enhanced chemokine release and upregulation of VCAM-1. VCAM-1 promotes adhesion of monocytes to the endothelium. IL-1 increases the expression of TF on EC and suppresses the cell surface anticoagulant activity of EC. Depending on its concentration, it may upregulate TNF-α production or downregulate TNF-receptors. IL-1 stimulates the hypothalamus and, as a consequence, the pituitary gland to produce anti-inflammatory mediators such as endorphins, melanocyte-stimulating hormone, and adrenocorticotropic hormone. |
| IL-6 | Together with other proinflammatory cytokines, IL-6 potentiates the coagulation cascade. It can downregulate production of TNF-α and TNF receptors. IL-6, together with IL-1, is a potent inducer of fever. |
| IL-8 | IL-8 is a chemokine that is abundantly produced by monocytes, EC, and hepatocytes. EC damage in the liver may elevate systemic concentrations. Activation of the coagulation system results in increased expression of IL-6 and IL-8 by monocytes, while the APC-PS anticoagulation pathway downregulates production of IL-8 by EC. |
| IL-10 | IL-10 is produced by monocytes and regulatory T helper cells and may cause platelet decay. Thrombin can stimulate IL-10 production by monocytes. The cytokine downregulates the inflammatory response and creates a proviral survival milieu. IL-10 promotes OAS by inhibiting development of effector T cells to new epitopes. IL-10 also inhibits the expression of TF and inhibits fibrinolysis. |
| TNF-α | TNF-α in a potent activator of EC and enhances capillary permeability. TNF-α upregulates expression of TF on monocytes and EC and downregulates expression of thrombomodulin on EC. It also activates the fibrinolysis system. TNF-α enhances expression of NO and mediates activation-induced death of T cells, and it has therefore been implicated in peripheral T-cell deletion. |
| TGF-β | TGF-β may act as a proinflammatory or anti-inflammatory cytokine, depending on its concentration. Early in infection, low levels of TGF-β may trigger secretion of IL-1 and TNF-α. However, later in infection, the cytokine inhibits the Th1 response and enhances production of Th2 cytokines such as IL-10. TGF-β increases expression of TF on EC and upregulates expression and release of PAI-1. |
| NO | NO has a multifaceted role in inflammatory reactions. It enhances vasodilatation and formation of edema. It upregulates TNF-α production in monocytes. At low concentrations it protects cells from apoptosis, while at high concentrations it induces apoptosis. NO downregulates expression of MHC class II and suppresses expansion of Th1 cells. Maintenance of the EC barrier requires a basal level of NO. Both a lack of NO and high NO levels destabilize EC junctions. |
| VEGF | VEGF is a key driver of vascular permeability. It reduces EC occludins, claudins, and VE-cadherin content, all of which are components of EC junctions. Upon activation, VEGF stimulates expression of ICAM-1, VCAM-1, and E-selectin in EC. |
Clearly, there is a substantial redundancy between cytokines (i.e., the lack of one specific cytokine may be compensated for by another cytokine with overlapping activities), making it difficult to explain DHF/DSS pathogenesis on the basis of a single cytokine. It is more likely that multiple cytokines contribute simultaneously in a complex way to the development of DHF/DSS. Apart from any other considerations, it is reasonable to assume that cytokines and other soluble mediators of the functional, and to a lesser degree the morphological, pathology characteristic of DHF/DSS are also essential for efficient viral clearance. The fact that DSS patients recover extremely rapidly after appropriate fluid therapy suggests that cytokines do not cause tissue destruction like in many immunopathology models but rather cause a reversible EC dysfunction.
THE INTERGRATED VIEW
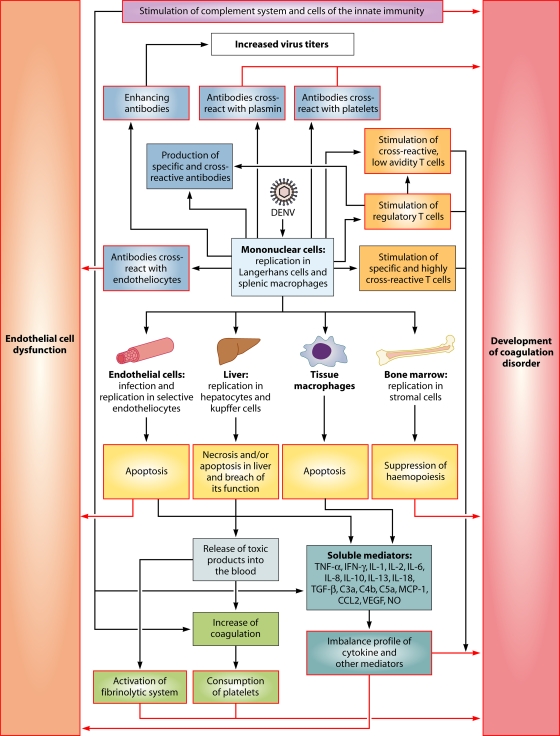
The mechanisms leading to the severe manifestations of DENV infections are still not completely understood but are likely to be multifactorial (Fig. 1). The genetic background of the host influences the way that the immune response reacts to DENV infection. Upon inoculation of DENV into the dermis, Langerhans cells and keratinocytes will primarily be infected. The virus subsequently spreads via the blood (primary viremia) and infects tissue macrophages in several organs, especially the macrophages in the spleen. The replication efficiency of DENV in DC, monocytes, and macrophages, as well as its tropism for and replication efficiency in EC, bone marrow stromal cells, and liver cells, collectively determine the viral load measured in blood. This viral load represents an important risk factor for development of severe disease. Essentially, infection of macrophages, hepatocytes, and EC influences the hemostatic and the immune responses to DENV. Infected cells die predominantly through apoptosis and to a lesser extent through necrosis. Necrosis results in release of toxic products, which activate the coagulation and fibrinolytic systems. Depending on the extent of infection of bone marrow stromal cells and the levels of IL-6, IL-8, IL-10, and IL-18, hemopoiesis is suppressed, resulting in decreased blood thrombogenicity. Platelets interact closely with EC, and a normal number of functioning platelets is necessary to maintain vascular stability. A high viral load in blood and possibly viral tropism for EC, severe thrombocytopenia, and platelet dysfunction may result in increased capillary fragility, clinically manifested as petechiae, easy bruising, and gastrointestinal mucosal bleeding (170), which is characteristic of DHF. At the same time, infection stimulates development of specific antibody and cellular immune responses to DENV. When IgM antibodies that cross-react with EC, platelets, and plasmin are produced, the loop that results in increased vascular permeability and coagulopathy is amplified. In addition, enhancing IgG antibodies bind heterologous virus during secondary infection and enhance infection of APCs, thereby contributing to the increased viral load that is seen during secondary viremia in some patients. Furthermore, a high viral load overstimulates both low- and high-avidity cross-reactive T cells. In the context of certain HLA haplotypes, cross-reactive T cells delay virus clearance, while producing high levels of proinflammatory cytokines and other mediators. Ultimately, these high levels of soluble factors, many of which still remain to be identified, induce changes in EC leading to the coagulopathy and plasma leakage characteristic of DSS.
FIG. 1.
Proposed model for the pathogenesis of DF, DHF, and DSS, based on an integrated view of the data presented (see section The Integrated View in the text). Black arrows, processes leading to the indicated event; colored boxes with white centers, pathological events. Each event will ultimately affect the EC or the hemostatic system (purple arrows).
DISCUSSION
Here we review and discuss the plethora of hypotheses about DHF and DSS pathogenesis presented in the literature. Most of these hypotheses are not mutually exclusive, and together they harbor multiple elements that collectively may explain most of the phenomena observed in the multiple presentations of DENV infection. Table 3 addresses major challenges to the hypotheses described in this review. The pathogenesis of both DHF grades I/II and DSS is complicated and multifactorial, involving both viral and host factors. However, necessary and/or sufficient factors have still not been identified. It may be questioned whether factors that explain the pathogenesis of DHF and DSS in all patients do exist. Genetic predisposition may have a significant effect on disease outcome. Only a few studies have studied host genetics with regard to the severity of DENV infection. Most commonly, clinically significant genetic variations consist of single-nucleotide polymorphisms within genes that affect disease pathways. Many polymorphisms have small and independent effects on disease outcome and often act in concert with other polymorphisms and environmental risk factors (24). This eventually results in complex and variable disease outcomes. Studies using a combination of genomics (transcriptomics, proteomics, and metabolomics), single-nucleotide polymorphism genotyping, and careful phenotypic disease characterization in well-defined cohorts should be adopted to identify individual molecular markers of DHF/DSS.
TABLE 3.
Challenges for DENV research
| Challenge |
|---|
| Developing an animal model of dengue disease |
| Understanding the role of several DENV strains and serotypes in DENV tropism in vivo |
| Elucidating the role of intrahost evolution of DENVs in emergence of virulent strains and the role of genetic variants and different serotypes in promoting OAS, ADE, transient autoimmunity, and unbalanced T-cell responses |
| Elucidating the role of DENV proteins, especially NS1 in pathogenesis |
| Understanding the interplay between the hemostatic and the complement systems in DENV infection |
| Elucidating the mechanisms by which innate immunity regulates memory B- and T-cell generation, maintenance, and activation during primary and secondary DENV infections |
| Elucidating the role of autoimmunity in dengue pathogenesis |
| Identifying serotype-specific linear and conformational B-cell epitopes and understanding their role in primary and anamnestic B-cell responses |
| Understanding the role of DENV immune complexes in the signaling network within target cells, especially APCs, and how it influences virus replication and priming of immune responses |
| Elucidating the role of the T-helper and T-cytotoxic cell repertoire, especially the private repertoire, on evolution of T-cell responses during primary and sequential heterologous DENV infections |
| Understanding the role of OAS in T-cell-mediated immunity in heterologous DENV infections and elucidating the factors that determine occurrence of OAS for T cells and its role in pathogenesis |
| Identifying soluble factors that are necessary or sufficient to induce endothelial cell dysfunction and coagulopathy seen in DHF/DSS |
| Identifying critical components of tight junctions and adherent junctions present in the vascular beds affected during DHF/DSS and elucidating the role that different soluble factors play in expression and functions of the several components of these junctions |
| Investigating the effect of demographic history of infection on the type of B- and T-cell responses elicited during primary and secondary DENV infections and on pathogenesis |
| Elucidating the role of host gene polymorphism, such as FcR, cytokines, chemokines, etc., in DHF/DSS pathogenesis |
| Understanding race- and age-dependent susceptibility to severe DENV infection |
As discussed in this review, the pathways to DHF involve both viral and host-specific elements. The following points can be summarized.
In contrast to what is generally believed, the involvement of liver and of EC in different organ systems seems to be an important factor in the pathogenesis of dengue. In this respect, it is of paramount importance to understand how EC lining the thoracic and peritoneal cavities are affected. It is worth noting that despite the increased vascular permeability measured in both DHF and DSS patients (16), plasma leakage is highly restricted to the pleural and peritoneal cavities, while no generalized edema is seen. No specific vascular lesions are found in fatal cases of DENV infections. Viruses known to cause hemorrhagic fever, such as viruses belonging to the families Arenaviridae (Junin virus and Lassa virus), Filoviridae (Ebola virus and Marburg virus), Bunyaviridae (Hanta virus and Rift Valley virus), and Flaviviridae (yellow fever virus), are also not associated with EC damage (43, 70). In these cases, the pathogenesis of hemorrhagic diathesis is the result of severe liver damage leading to decreased production of coagulation proteins and albumin. Increased vascular permeability as a result of hypercytokinemia and a reduction of plasma osmotic pressure due to severe liver damage contribute to edema formation, as is seen in severe cases of Lassa fever (67). In addition, replication of most of these viruses in the adrenal gland contributes to hypotension and sodium loss, which collectively result in hypovolemic shock. The shock syndrome associated with DSS, however, is unique to DENV infection, and it is of paramount importance to understand how the EC lining the thoracic and peritoneal cavities are affected.
Hemorrhagic manifestations as seen in DF and DHF grades I/II are usually mild and manifested as petechiae disseminated in the skin, with an increased tendency of bleeding upon bruising. These manifestations are found early after onset of fever and coincide with the window of viremia and degree of thrombocytopenia (121). The pathogenesis of mild hemorrhages seen in DF and DHF grades I/II may be explained by increased capillary fragility as a result of thrombocytopenia or platelet dysfunction, virus infection of EC, and high concentrations of cytokines that disrupt vascular integrity (54, 170, 257). Most mediators that increase vascular permeability affect the organization of the adherens junctions (AJ), a complex network of adhesion proteins that are linked to intracellular cytoskeleton (54), causing retraction of EC and opening of intercellular gaps. Alternatively, the stability of the junctions may be weakened, resulting in vascular fragility. Weakness of the junctions is not reflected by morphological changes, as is exemplified by the fact that internalization of VE-caherin or phosphorylation of AJ proteins reduces junction stability without the opening of intercellular gaps (4, 62). It is noteworthy that the major anatomical sites of bleeding in patients with severe thrombocytopenia are the intercellular gaps in the postcapillary venules, which are rich in AJ (170). Platelets play a role in maintaining the integrity of AJ by constitutively releasing an array of factors such as platelet-activating factor and sphingosine-1-phosphate, which are released as a result of fluid shear stress (5). Therefore, interruption of platelet-EC interaction by severe thrombocytopenia or platelet dysfunction may lead to increased vascular fragility, resulting in hemorrhages or increased tendencies for hemorrhages.
Several studies have shown that plasma leakage occurs before defervescence or hemoconcentration. As mentioned before, the WHO case definition has mainly a clinical diagnostic purpose and is not an appropriate selection criterion for pathogenesis studies. Pathogenesis studies should be designed to understand the differences between (i) no bleeding tendencies, (ii) increased manifestations of bleeding or tendencies for bleeding, or (iii) plasma leakage as measured by sonography and hemoconcentration. It is crucial to study the pleural fluid in order to understand the pathophysiological cause of plasma leakage and why it is restricted to or more pronounced in thoracic and peritoneal areas.
Antibody-mediated enhancement of infection either results in a high viral load or represents the link to type 2 cytokine responses.
In some viral systems, cross-reactive CD8+ T-cell responses are involved in the development of pathological changes during secondary infection with a related but heterologous virus. DENV cross-reactive T cells, however, lose their cytolytic activity, while producing high levels of proinflammatory cytokines and other mediators. The role that preexisting immunity to other flaviviruses plays in the development of severe dengue should be investigated.
Soluble host factors seem to be central in the pathogenesis of both DHF grades I/II and DSS. Although several of these have been associated with severe disease, their concentrations are also elevated in other viral infections without resulting in plasma leakage. High concentrations of cytokines such TNF-α, IL-6, and IL-8 have been implicated in capillary leakage and development of hypovolemic shock in patients with anaphylaxis, meningococcal sepsis, and Jarish Herxheimer reaction (105, 176, 233). Similarly, high concentrations of cytokines have been associated with unfavorable outcomes of filovirus (253), arenavirus (89, 160), and yellow fever virus (241) infections. However, the shock syndrome associated with DSS does not occur in these conditions. Therefore, it may be speculated that soluble factors incriminated in the increased vascular permeability seen in DSS must be qualitatively and quantitatively different from those involved in the conditions described above.
Acknowledgments
We thank Peter Fraaij, Rik de Swart, and Bart Haagmans for providing valuable comments.
Biography
 Byron Martina studied biomedical sciences and graduated as a Master in Immunology of Infectious Diseases at De Montfort University in Leicester (United Kingdom) in 1998. He then joined the Department of Virology at Erasmus Medical Center in Rotterdam (The Netherlands), to obtain his Ph.D. degree in 2003. During this period he worked on the development and testing of vaccine candidates against herpesviruses. He subsequently joined the “Emerging Viruses” team of the same department, where he worked on the pathogenesis of severe acute respiratory syndrome coronavirus. In doing so he developed an animal model for severe acute respiratory syndrome, in which he evaluated several intervention strategies, including antiviral treatment and new generations of vaccines. He has a broad interest in virus pathogenesis and intervention strategies, but his current research focuses on the pathogenesis of vector-borne diseases and the development of vaccines against these viruses.
Byron Martina studied biomedical sciences and graduated as a Master in Immunology of Infectious Diseases at De Montfort University in Leicester (United Kingdom) in 1998. He then joined the Department of Virology at Erasmus Medical Center in Rotterdam (The Netherlands), to obtain his Ph.D. degree in 2003. During this period he worked on the development and testing of vaccine candidates against herpesviruses. He subsequently joined the “Emerging Viruses” team of the same department, where he worked on the pathogenesis of severe acute respiratory syndrome coronavirus. In doing so he developed an animal model for severe acute respiratory syndrome, in which he evaluated several intervention strategies, including antiviral treatment and new generations of vaccines. He has a broad interest in virus pathogenesis and intervention strategies, but his current research focuses on the pathogenesis of vector-borne diseases and the development of vaccines against these viruses.
 Penelope Koraka obtained her B.Sc. in laboratory technology in the Technological Educational Institute, Athens (Greece), and subsequently her M.Sc. in Immunology of Infectious Diseases in Leicester (United Kingdom). She obtained her Ph.D. degree at the Department of Virology at Erasmus Medical Center in Rotterdam (The Netherlands) in 2007 studying dengue virus infections in humans and nonhuman primates. As a junior postdoc she joined the “Virus Discovery” team at the same department, focusing on the identification of new respiratory pathogens. Recently, she joined the “Emerging Viruses” team of the same department, with a main focus on dengue viruses. During the past 10 years, she has gained broad experience working on emerging pathogens, being involved in the characterization of immune responses and development of animal models and vaccines. Currently, her research focuses on virulence factors of vector-borne viruses.
Penelope Koraka obtained her B.Sc. in laboratory technology in the Technological Educational Institute, Athens (Greece), and subsequently her M.Sc. in Immunology of Infectious Diseases in Leicester (United Kingdom). She obtained her Ph.D. degree at the Department of Virology at Erasmus Medical Center in Rotterdam (The Netherlands) in 2007 studying dengue virus infections in humans and nonhuman primates. As a junior postdoc she joined the “Virus Discovery” team at the same department, focusing on the identification of new respiratory pathogens. Recently, she joined the “Emerging Viruses” team of the same department, with a main focus on dengue viruses. During the past 10 years, she has gained broad experience working on emerging pathogens, being involved in the characterization of immune responses and development of animal models and vaccines. Currently, her research focuses on virulence factors of vector-borne viruses.
 Albert Osterhaus graduated as a veterinarian in 1974 and obtained a Ph.D. degree in virology in 1978, both at Utrecht University (The Netherlands). After working at the National Institute of Health of The Netherlands, he became Professor of Environmental Virology at Utrecht University and Professor/Head of Department of Virology at Erasmus MC in Rotterdam in 1992 and 1994, respectively. He is particularly interested in viruses that affect animals and humans and cross species barriers. He and his team have identified more than a dozen “new” viruses (e.g., human metapneumovirus and a novel human coronavirus) and proved that the severe acute respiratory syndrome coronavirus is the cause of severe acute respiratory syndrome. His studies focused on virus outbreaks in wildlife, mechanisms of transmission and pathogenesis of zoonotic viruses, natural and vaccine-induced immune responses, and antiviral drugs. He acted as Ph.D. supervisor for more than 40 students, authored about 800 academic articles, created biotech companies, and held several editorial positions.
Albert Osterhaus graduated as a veterinarian in 1974 and obtained a Ph.D. degree in virology in 1978, both at Utrecht University (The Netherlands). After working at the National Institute of Health of The Netherlands, he became Professor of Environmental Virology at Utrecht University and Professor/Head of Department of Virology at Erasmus MC in Rotterdam in 1992 and 1994, respectively. He is particularly interested in viruses that affect animals and humans and cross species barriers. He and his team have identified more than a dozen “new” viruses (e.g., human metapneumovirus and a novel human coronavirus) and proved that the severe acute respiratory syndrome coronavirus is the cause of severe acute respiratory syndrome. His studies focused on virus outbreaks in wildlife, mechanisms of transmission and pathogenesis of zoonotic viruses, natural and vaccine-induced immune responses, and antiviral drugs. He acted as Ph.D. supervisor for more than 40 students, authored about 800 academic articles, created biotech companies, and held several editorial positions.
REFERENCES
- 1.Acioli-Santos, B., L. Segat, R. Dhalia, C. A. Brito, U. M. Braga-Neto, E. T. Marques, and S. Crovella. 2008. MBL2 gene polymorphisms protect against development of thrombocytopenia associated with severe dengue phenotype. Hum. Immunol. 69:122-128. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal, R., U. C. Chaturvedi, A. Misra, R. Mukerjee, S. Kapoor, R. Nagar, R. Tandon, and A. Mathur. 1998. Production of cytotoxic factor by peripheral blood mononuclear cells (PBMC) in patients with dengue haemorrhagic fever. Clin. Exp. Immunol. 112:477-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.An, J., D. S. Zhou, J. L. Zhang, H. Morida, J. L. Wang, and K. Yasui. 2004. Dengue-specific CD8+ T cells have both protective and pathogenic roles in dengue virus infection. Immunol. Lett. 95:167-174. [DOI] [PubMed] [Google Scholar]
- 4.Andriopoulou, P., P. Navarro, A. Zanetti, M. G. Lampugnani, and E. Dejana. 1999. Histamine induces tyrosine phosphorylation of endothelial cell-to-cell adherens junctions. Arterioscler. Thromb. Vasc. Biol. 19:2286-2297. [DOI] [PubMed] [Google Scholar]
- 5.Aoki, S., M. Osada, M. Kaneko, Y. Ozaki, and Y. Yatomi. 2007. Fluid shear stress enhances the sphingosine 1-phosphate responses in cell-cell interactions between platelets and endothelial cells. Biochem. Biophys. Res. Commun. 358:1054-1057. [DOI] [PubMed] [Google Scholar]
- 6.Atrasheuskaya, A., P. Petzelbauer, T. M. Fredeking, and G. Ignatyev. 2003. Anti-TNF antibody treatment reduces mortality in experimental dengue virus infection. FEMS Immunol. Med. Microbiol. 35:33-42. [DOI] [PubMed] [Google Scholar]
- 7.Avirutnan, P., P. Malasit, B. Seliger, S. Bhakdi, and M. Husmann. 1998. Dengue virus infection of human endothelial cells leads to chemokine production, complement activation, and apoptosis. J. Immunol. 161:6338-6346. [PubMed] [Google Scholar]
- 8.Avirutnan, P., N. Punyadee, S. Noisakran, C. Komoltri, S. Thiemmeca, K. Auethavornanan, A. Jairungsri, R. Kanlaya, N. Tangthawornchaikul, C. Puttikhunt, S. N. Pattanakitsakul, P. T. Yenchitsomanus, J. Mongkolsapaya, W. Kasinrerk, N. Sittisombut, M. Husmann, M. Blettner, S. Vasanawathana, S. Bhakdi, and P. Malasit. 2006. Vascular leakage in severe dengue virus infections: a potential role for the nonstructural viral protein NS1 and complement. J. Infect. Dis. 193:1078-1088. [DOI] [PubMed] [Google Scholar]
- 9.Avirutnan, P., L. Zhang, N. Punyadee, A. Manuyakorn, C. Puttikhunt, W. Kasinrerk, P. Malasit, J. P. Atkinson, and M. S. Diamond. 2007. Secreted NS1 of dengue virus attaches to the surface of cells via interactions with heparan sulfate and chondroitin sulfate E. PLoS Pathog. 3:e183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Azeredo, E. L., S. M. Zagne, M. A. Santiago, A. S. Gouvea, A. A. Santana, P. C. Neves-Souza, R. M. Nogueira, M. P. Miagostovich, and C. F. Kubelka. 2001. Characterisation of lymphocyte response and cytokine patterns in patients with dengue fever. Immunobiology 204:494-507. [DOI] [PubMed] [Google Scholar]
- 11.Azizan, A., J. Sweat, C. Espino, J. Gemmer, L. Stark, and D. Kazanis. 2006. Differential proinflammatory and angiogenesis-specific cytokine production in human pulmonary endothelial cells, HPMEC-ST1.6R infected with dengue-2 and dengue-3 virus. J. Virol. Methods 138:211-217. [DOI] [PubMed] [Google Scholar]
- 12.Balasubramanian, S., L. Janakiraman, S. S. Kumar, S. Muralinath, and S. Shivbalan. 2006. A reappraisal of the criteria to diagnose plasma leakage in dengue hemorrhagic fever. Indian Pediatr. 43:334-339. [PubMed] [Google Scholar]
- 13.Balsitis, S. J., J. Coloma, G. Castro, A. Alava, D. Flores, J. H. McKerrow, P. R. Beatty, and E. Harris. 2009. Tropism of dengue virus in mice and humans defined by viral nonstructural protein 3-specific immunostaining. Am. J. Trop. Med. Hyg. 80:416-424. [PubMed] [Google Scholar]
- 14.Basilio-de-Oliveira, C. A., G. R. Aguiar, M. S. Baldanza, O. M. Barth, W. A. Eyer-Silva, and M. V. Paes. 2005. Pathologic study of a fatal case of dengue-3 virus infection in Rio de Janeiro, Brazil. Braz. J. Infect. Dis. 9:341-347. [DOI] [PubMed] [Google Scholar]
- 15.Basu, A., and U. C. Chaturvedi. 2008. Vascular endothelium: the battlefield of dengue viruses. FEMS Immunol. Med. Microbiol. 53:287-299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bethell, D. B., J. Gamble, P. L. Pham, M. D. Nguyen, T. H. Tran, T. H. Ha, T. N. Tran, T. H. Dong, I. B. Gartside, N. J. White, and N. P. Day. 2001. Noninvasive measurement of microvascular leakage in patients with dengue hemorrhagic fever. Clin. Infect. Dis. 32:243-253. [DOI] [PubMed] [Google Scholar]
- 17.Bhamarapravati, N., P. Tuchinda, and V. Boonyapaknavik. 1967. Pathology of Thailand haemorrhagic fever: a study of 100 autopsy cases. Ann. Trop. Med. Parasitol. 61:500-510. [DOI] [PubMed] [Google Scholar]
- 18.Blackley, S., Z. Kou, H. Chen, M. Quinn, R. C. Rose, J. J. Schlesinger, M. Coppage, and X. Jin. 2007. Primary human splenic macrophages, but not T or B cells, are the principal target cells for dengue virus infection in vitro. J. Virol. 81:13325-13334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonner, S. M., and M. A. O'Sullivan. 1998. Endothelial cell monolayers as a model system to investigate dengue shock syndrome. J. Virol. Methods 71:159-167. [DOI] [PubMed] [Google Scholar]
- 20.Boonnak, K., B. M. Slike, T. H. Burgess, R. M. Mason, S. J. Wu, P. Sun, K. Porter, I. F. Rudiman, D. Yuwono, P. Puthavathana, and M. A. Marovich. 2008. Role of dendritic cells in antibody-dependent enhancement of dengue virus infection. J. Virol. 82:3939-3951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boonpucknavig, S., V. Boonpucknavig, N. Bhamarapravati, and S. Nimmannitya. 1979. Immunofluorescence study of skin rash in patients with dengue hemorrhagic fever. Arch. Pathol. Lab. Med. 103:463-466. [PubMed] [Google Scholar]
- 22.Bosch, I., K. Xhaja, L. Estevez, G. Raines, H. Melichar, R. V. Warke, M. V. Fournier, F. A. Ennis, and A. L. Rothman. 2002. Increased production of interleukin-8 in primary human monocytes and in human epithelial and endothelial cell lines after dengue virus challenge. J. Virol. 76:5588-5597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bozza, F. A., O. G. Cruz, S. M. Zagne, E. L. Azeredo, R. M. Nogueira, E. F. Assis, P. T. Bozza, and C. F. Kubelka. 2008. Multiplex cytokine profile from dengue patients: MIP-1beta and IFN-gamma as predictive factors for severity. BMC. Infect. Dis. 8:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bracken, M. B. 2005. Genomic epidemiology of complex disease: the need for an electronic evidence-based approach to research synthesis. Am. J. Epidemiol. 162:297-301. [DOI] [PubMed] [Google Scholar]
- 25.Burke, D. S., and S. Kliks. 2006. Antibody-dependent enhancement in dengue virus infections. J. Infect. Dis. 193:601-603. (Author reply, 193:603-604.) [DOI] [PubMed] [Google Scholar]
- 26.Butthep, P., S. Chunhakan, K. Tangnararatchakit, S. Yoksan, K. Pattanapanyasat, and A. Chuansumrit. 2006. Elevated soluble thrombomodulin in the febrile stage related to patients at risk for dengue shock syndrome. Pediatr. Infect. Dis. J. 25:894-897. [DOI] [PubMed] [Google Scholar]
- 27.Cardier, J. E., V. Balogh, C. Perez-Silva, E. Romano, B. Rivas, N. Bosch, and A. L. Rothman. 2006. Relationship of thrombopoietin and interleukin-11 levels to thrombocytopenia associated with dengue disease. Cytokine 34:155-160. [DOI] [PubMed] [Google Scholar]
- 28.Cardier, J. E., E. Marino, E. Romano, P. Taylor, F. Liprandi, N. Bosch, and A. L. Rothman. 2005. Proinflammatory factors present in sera from patients with acute dengue infection induce activation and apoptosis of human microvascular endothelial cells: possible role of TNF-alpha in endothelial cell damage in dengue. Cytokine 30:359-365. [DOI] [PubMed] [Google Scholar]
- 29.Cardier, J. E., B. Rivas, E. Romano, A. L. Rothman, C. Perez-Perez, M. Ochoa, A. M. Caceres, M. Cardier, N. Guevara, and R. Giovannetti. 2006. Evidence of vascular damage in dengue disease: demonstration of high levels of soluble cell adhesion molecules and circulating endothelial cells. Endothelium 13:335-340. [DOI] [PubMed] [Google Scholar]
- 30.Carlos, C. C., K. Oishi, M. T. Cinco, C. A. Mapua, S. Inoue, D. J. Cruz, M. A. Pancho, C. Z. Tanig, R. R. Matias, K. Morita, F. F. Natividad, A. Igarashi, and T. Nagatake. 2005. Comparison of clinical features and hematologic abnormalities between dengue fever and dengue hemorrhagic fever among children in the Philippines. Am. J. Trop. Med. Hyg. 73:435-440. [PubMed] [Google Scholar]
- 31.Casadevall, A., and L. A. Pirofski. 1999. Host-pathogen interactions: redefining the basic concepts of virulence and pathogenicity. Infect. Immun. 67:3703-3713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chakravarti, A., and R. Kumaria. 2006. Circulating levels of tumour necrosis factor-alpha & interferon-gamma in patients with dengue & dengue haemorrhagic fever during an outbreak. Indian J. Med. Res. 123:25-30. [PubMed] [Google Scholar]
- 33.Chang, H. H., H. F. Shyu, Y. M. Wang, D. S. Sun, R. H. Shyu, S. S. Tang, and Y. S. Huang. 2002. Facilitation of cell adhesion by immobilized dengue viral nonstructural protein 1 (NS1): arginine-glycine-aspartic acid structural mimicry within the dengue viral NS1 antigen. J. Infect. Dis. 186:743-751. [DOI] [PubMed] [Google Scholar]
- 34.Chanthavanich, P., C. Luxemburger, C. Sirivichayakul, K. Lapphra, K. Pengsaa, S. Yoksan, A. Sabchareon, and J. Lang. 2006. Immune response and occurrence of dengue infection in Thai children three to eight years after vaccination with live attenuated tetravalent dengue vaccine. Am. J. Trop. Med. Hyg. 75:26-28. [DOI] [PubMed] [Google Scholar]
- 35.Chao, Y. C., C. S. Huang, C. N. Lee, S. Y. Chang, C. C. King, and C. L. Kao. 2008. Higher infection of dengue virus serotype 2 in human monocytes of patients with G6PD deficiency. PLoS One 3:e1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chareonsirisuthigul, T., S. Kalayanarooj, and S. Ubol. 2007. Dengue virus (DENV) antibody-dependent enhancement of infection upregulates the production of anti-inflammatory cytokines, but suppresses anti-DENV free radical and pro-inflammatory cytokine production, in THP-1 cells. J. Gen. Virol. 88:365-375. [DOI] [PubMed] [Google Scholar]
- 37.Chaturvedi, U. C., E. A. Elbishbishi, R. Agarwal, and A. S. Mustafa. 2001. Cytotoxic factor-autoantibodies: possible role in the pathogenesis of dengue haemorrhagic fever. FEMS Immunol. Med. Microbiol. 30:181-186. [DOI] [PubMed] [Google Scholar]
- 38.Chau, T. N., N. T. Quyen, T. T. Thuy, N. M. Tuan, D. M. Hoang, N. T. Dung, B. Lien le, N. T. Quy, N. T. Hieu, L. T. Hieu, T. T. Hien, N. T. Hung, J. Farrar, and C. P. Simmons. 2008. Dengue in Vietnamese infants—xresults of infection-enhancement assays correlate with age-related disease epidemiology, and cellular immune responses correlate with disease severity. J. Infect. Dis. 198:516-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen, H. C., F. M. Hofman, J. T. Kung, Y. D. Lin, and B. A. Wu-Hsieh. 2007. Both virus and tumor necrosis factor alpha are critical for endothelium damage in a mouse model of dengue virus-induced hemorrhage. J. Virol. 81:5518-5526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen, H. D., A. E. Fraire, I. Joris, M. A. Brehm, R. M. Welsh, and L. K. Selin. 2001. Memory CD8+ T cells in heterologous antiviral immunity and immunopathology in the lung. Nat. Immunol. 2:1067-1076. [DOI] [PubMed] [Google Scholar]
- 41.Chen, H. D., A. E. Fraire, I. Joris, R. M. Welsh, and L. K. Selin. 2003. Specific history of heterologous virus infections determines anti-viral immunity and immunopathology in the lung. Am. J. Pathol. 163:1341-1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen, H. L., S. R. Lin, H. F. Liu, C. C. King, S. C. Hsieh, and W. K. Wang. 2008. Evolution of dengue virus type 2 during two consecutive outbreaks with an increase in severity in southern Taiwan in 2001-2002. Am. J. Trop. Med. Hyg. 79:495-505. [PubMed] [Google Scholar]
- 43.Chen, J. P., and T. M. Cosgriff. 2000. Hemorrhagic fever virus-induced changes in hemostasis and vascular biology. Blood Coagul. Fibrinolysis 11:461-483. [DOI] [PubMed] [Google Scholar]
- 44.Chen, L. C., H. Y. Lei, C. C. Liu, S. C. Shiesh, S. H. Chen, H. S. Liu, Y. S. Lin, S. T. Wang, H. W. Shyu, and T. M. Yeh. 2006. Correlation of serum levels of macrophage migration inhibitory factor with disease severity and clinical outcome in dengue patients. Am. J. Trop. Med. Hyg. 74:142-147. [PubMed] [Google Scholar]
- 45.Chen, R. F., L. Wang, J. T. Cheng, H. Chuang, J. C. Chang, J. W. Liu, I. C. Lin, and K. D. Yang. 2009. Combination of CTLA-4 and TGFbeta1 gene polymorphisms associated with dengue hemorrhagic fever and virus load in a dengue-2 outbreak. Clin. Immunol. 131:404-409. [DOI] [PubMed] [Google Scholar]
- 46.Chen, R. F., K. D. Yang, L. Wang, J. W. Liu, C. C. Chiu, and J. T. Cheng. 2007. Different clinical and laboratory manifestations between dengue haemorrhagic fever and dengue fever with bleeding tendency. Trans. R. Soc. Trop. Med. Hyg. 101:1106-1113. [DOI] [PubMed] [Google Scholar]
- 47.Chen, Y. C., and S. Y. Wang. 2002. Activation of terminally differentiated human monocytes/macrophages by dengue virus: productive infection, hierarchical production of innate cytokines and chemokines, and the synergistic effect of lipopolysaccharide. J. Virol. 76:9877-9887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Choi, G., M. J. Schultz, M. Levi, and T. van der Poll. 2006. The relationship between inflammation and the coagulation system. Swiss Med. Wkly. 136:139-144. [DOI] [PubMed] [Google Scholar]
- 49.Chungue, E., L. Poli, C. Roche, P. Gestas, P. Glaziou, and L. J. Markoff.s. 1994. Correlation between detection of plasminogen cross-reactive antibodies and hemorrhage in dengue virus infection. J. Infect. Dis. 170:1304-1307. [DOI] [PubMed] [Google Scholar]
- 50.Churdboonchart, V., N. Bhamarapravati, and P. Futrakul. 1983. Crossed immunoelectrophoresis for the detection of split products of the third complement in dengue hemorrhagic fever. I. Observations in patients' plasma. Am. J. Trop. Med. Hyg. 32:569-576. [DOI] [PubMed] [Google Scholar]
- 51.Cologna, R., and R. Rico-Hesse. 2003. American genotype structures decrease dengue virus output from human monocytes and dendritic cells. J. Virol. 77:3929-3938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cornberg, M., A. T. Chen, L. A. Wilkinson, M. A. Brehm, S. K. Kim, C. Calcagno, D. Ghersi, R. Puzone, F. Celada, R. M. Welsh, and L. K. Selin. 2006. Narrowed TCR repertoire and viral escape as a consequence of heterologous immunity. J. Clin. Investig. 116:1443-1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Couvelard, A., P. Marianneau, C. Bedel, M. T. Drouet, F. Vachon, D. Henin, and V. Deubel. 1999. Report of a fatal case of dengue infection with hepatitis: demonstration of dengue antigens in hepatocytes and liver apoptosis. Hum. Pathol. 30:1106-1110. [DOI] [PubMed] [Google Scholar]
- 54.Dejana, E., E. Tournier-Lasserve, and B. M. Weinstein. 2009. The control of vascular integrity by endothelial cell junctions: molecular basis and pathological implications. Dev. Cell 16:209-221. [DOI] [PubMed] [Google Scholar]
- 54a.de Jong, M. D., C. P. Simmons, T. T. Thanh, V. M. Hien, G. J. Smith, T. N. Chau, D. M. Hoang, N. V. Chau, T. H. Khanh, V. C. Dong, P. T. Qui, B. V. Cam, Q. Ha do, Y. Guan, J. S. Peiris, N. T. Chinh, T. T. Hien, and J. Farrar. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat. Med. 12:1203-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54b.de la C Sierra, B., G. Garcia, A. B. Perez, L. Morier, M. Alvarez, G. Kouri, and M. G. Guzman. 2006. Ethnicity and difference in dengue virus-specific memory T cell responses in Cuban individuals. Viral Immunol. 19:662-668. [DOI] [PubMed] [Google Scholar]
- 54c.de la C Sierra, B., G. Kouri, and M. G. Guzman. 2007. Race: a risk factor for dengue hemorrhagic fever. Arch. Virol. 152:533-542. [DOI] [PubMed] [Google Scholar]
- 54d.de Macedo, F. C., A. F. Nicol, L. D. Cooper, M. Yearsley, A. R. Pires, and G. J. Nuovo. 2006. Histologic, viral, and molecular correlates of dengue fever infection of the liver using highly sensitive immunohistochemistry. Diagn. Mol. Pathol. 15:223-228. [DOI] [PubMed] [Google Scholar]
- 54e.de Souza, L. J., R. M. Nogueira, L. C. Soares, C. E. Soares, B. F. Ribas, F. P. Alves, F. R. Vieira, and F. E. Pessanha. 2007. The impact of dengue on liver function as evaluated by aminotransferase levels. Braz. J. Infect. Dis. 11:407-410. [DOI] [PubMed] [Google Scholar]
- 55.Dewi, B. E., T. Takasaki, and I. Kurane. 2004. In vitro assessment of human endothelial cell permeability: effects of inflammatory cytokines and dengue virus infection. J. Virol. Methods 121:171-180. [DOI] [PubMed] [Google Scholar]
- 56.Diamond, M. S., D. Edgil, T. G. Roberts, B. Lu, and E. Harris. 2000. Infection of human cells by dengue virus is modulated by different cell types and viral strains. J. Virol. 74:7814-7823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ding, X., F. Xu, H. Chen, R. B. Tesh, and S. Y. Xiao. 2005. Apoptosis of hepatocytes caused by Punta Toro virus (Bunyaviridae: Phlebovirus) and its implication for Phlebovirus pathogenesis. Am. J. Pathol. 167:1043-1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dong, T., E. Moran, N. Vinh Chau, C. Simmons, K. Luhn, Y. Peng, B. Wills, N. Phuong Dung, L. Thi Thu Thao, T. T. Hien, A. McMichael, J. Farrar, and S. Rowland-Jones. 2007. High pro-inflammatory cytokine secretion and loss of high avidity cross-reactive cytotoxic T-cells during the course of secondary dengue virus infection. PLoS One 2:e1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Durbin, A. P., M. J. Vargas, K. Wanionek, S. N. Hammond, A. Gordon, C. Rocha, A. Balmaseda, and E. Harris. 2008. Phenotyping of peripheral blood mononuclear cells during acute dengue illness demonstrates infection and increased activation of monocytes in severe cases compared to classic dengue fever. Virology 376:429-435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Esmon, C. T. 2005. The interactions between inflammation and coagulation. Br. J. Haematol. 131:417-430. [DOI] [PubMed] [Google Scholar]
- 61.Espina, L. M., N. J. Valero, J. M. Hernandez, and J. A. Mosquera. 2003. Increased apoptosis and expression of tumor necrosis factor-alpha caused by infection of cultured human monocytes with dengue virus. Am. J. Trop. Med. Hyg. 68:48-53. [PubMed] [Google Scholar]
- 62.Esser, S., M. G. Lampugnani, M. Corada, E. Dejana, and W. Risau. 1998. Vascular endothelial growth factor induces VE-cadherin tyrosine phosphorylation in endothelial cells. J. Cell Sci. 111:1853-1865. [DOI] [PubMed] [Google Scholar]
- 63.Fabre, A., A. Couvelard, C. Degott, C. Lagorce-Pages, F. Bruneel, E. Bouvet, and F. Vachon. 2001. Dengue virus induced hepatitis with chronic calcific changes. Gut 49:864-865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Falconar, A. K. 1997. The dengue virus nonstructural-1 protein (NS1) generates antibodies to common epitopes on human blood clotting, integrin/adhesin proteins and binds to human endothelial cells: potential implications in haemorrhagic fever pathogenesis. Arch. Virol. 142:897-916. [DOI] [PubMed] [Google Scholar]
- 65.Feng, J. Q., K. Mozdzanowska, and W. Gerhard. 2002. Complement component C1q enhances the biological activity of influenza virus hemagglutinin-specific antibodies depending on their fine antigen specificity and heavy-chain isotype. J. Virol. 76:1369-1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fernandez-Mestre, M. T., K. Gendzekhadze, P. Rivas-Vetencourt, and Z. Layrisse. 2004. TNF-alpha-308A allele, a possible severity risk factor of hemorrhagic manifestation in dengue fever patients. Tissue Antigens 64:469-472. [DOI] [PubMed] [Google Scholar]
- 67.Frame, J. D. 1989. Clinical features of Lassa fever in Liberia. Rev. Infect. Dis. 11(Suppl. 4):S783-S789. [DOI] [PubMed] [Google Scholar]
- 68.Fritz, R. S., F. G. Hayden, D. P. Calfee, L. M. Cass, A. W. Peng, W. G. Alvord, W. Strober, and S. E. Straus. 1999. Nasal cytokine and chemokine responses in experimental influenza A virus infection: results of a placebo-controlled trial of intravenous zanamivir treatment. J. Infect. Dis. 180:586-593. [DOI] [PubMed] [Google Scholar]
- 69.Gasperino, J., J. Yunen, A. Guh, K. E. Tanaka, V. Kvetan, and H. Doyle. 2007. Fulminant liver failure secondary to haemorrhagic dengue in an international traveller. Liver Int. 27:1148-1151. [DOI] [PubMed] [Google Scholar]
- 70.Geisbert, T. W., and P. B. Jahrling. 2004. Exotic emerging viral diseases: progress and challenges. Nat. Med. 10:S110-S121. [DOI] [PubMed] [Google Scholar]
- 71.Gentile, D., W. Doyle, T. Whiteside, P. Fireman, F. G. Hayden, and D. Skoner. 1998. Increased interleukin-6 levels in nasal lavage samples following experimental influenza A virus infection. Clin. Diagn. Lab. Immunol. 5:604-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ghiasi, H., G. C. Perng, A. B. Nesburn, and S. L. Wechsler. 2000. Antibody-dependent enhancement of HSV-1 infection by anti-gK sera. Virus Res. 68:137-144. [DOI] [PubMed] [Google Scholar]
- 73.Girn, J., M. Kavoosi, and J. Chantler. 2002. Enhancement of coxsackievirus B3 infection by antibody to a different coxsackievirus strain. J. Gen. Virol. 83:351-358. [DOI] [PubMed] [Google Scholar]
- 74.Graham, R. R., M. Juffrie, R. Tan, C. G. Hayes, I. Laksono, C. Ma'roef, Erlin, Sutaryo, K. R. Porter, and S. B. Halstead. 1999. A prospective seroepidemiologic study on dengue in children four to nine years of age in Yogyakarta, Indonesia I. studies in 1995-1996. Am. J. Trop. Med. Hyg. 61:412-419. [DOI] [PubMed] [Google Scholar]
- 75.Guha-Sapir, D., and B. Schimmer. 2005. Dengue fever: new paradigms for a changing epidemiology. Emerg. Themes Epidemiol. 2:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Guilarde, A. O., M. D. Turchi, J. B. Siqueira, Jr., V. C. Feres, B. Rocha, J. E. Levi, V. A. Souza, L. S. Boas, C. S. Pannuti, and C. M. Martelli. 2008. Dengue and dengue hemorrhagic fever among adults: clinical outcomes related to viremia, serotypes, and antibody response. J. Infect. Dis. 197:817-824. [DOI] [PubMed] [Google Scholar]
- 77.Guirakhoo, F., S. Kitchener, D. Morrison, R. Forrat, K. McCarthy, R. Nichols, S. Yoksan, X. Duan, T. H. Ermak, N. Kanesa-Thasan, P. Bedford, J. Lang, M. J. Quentin-Millet, and T. P. Monath. 2006. Live attenuated chimeric yellow fever dengue type 2 (ChimeriVax-DEN2) vaccine: phase I clinical trial for safety and immunogenicity: effect of yellow fever pre-immunity in induction of cross neutralizing antibody responses to all 4 dengue serotypes. Hum. Vaccin. 2:60-67. [DOI] [PubMed] [Google Scholar]
- 78.Guzman, M. G., M. Alvarez, R. Rodriguez, D. Rosario, S. Vazquez, L. Valds, M. V. Cabrera, and G. Kouri. 1999. Fatal dengue hemorrhagic fever in Cuba, 1997. Int. J. Infect. Dis. 3:130-135. [DOI] [PubMed] [Google Scholar]
- 79.Guzman, M. G., and G. Kouri. 2003. Dengue and dengue hemorrhagic fever in the Americas: lessons and challenges. J. Clin. Virol. 27:1-13. [DOI] [PubMed] [Google Scholar]
- 80.Guzman, M. G., G. Kouri, J. Bravo, L. Valdes, S. Vazquez, and S. B. Halstead. 2002. Effect of age on outcome of secondary dengue 2 infections. Int. J. Infect. Dis. 6:118-124. [DOI] [PubMed] [Google Scholar]
- 81.Guzman, M. G., G. Kouri, and S. B. Halstead. 2000. Do escape mutants explain rapid increases in dengue case-fatality rates within epidemics? Lancet 355:1902-1903. [DOI] [PubMed] [Google Scholar]
- 82.Guzman, M. G., G. Kouri, L. Valdes, J. Bravo, M. Alvarez, S. Vazques, I. Delgado, and S. B. Halstead. 2000. Epidemiologic studies on dengue in Santiago de Cuba, 1997. Am. J. Epidemiol. 152:793-799. (Discussion, 152:804.) [DOI] [PubMed] [Google Scholar]
- 83.Halstead, S. B. 2007. Dengue. Lancet. 370:1644-1652. [DOI] [PubMed] [Google Scholar]
- 84.Halstead, S. B. 2006. Dengue in the Americas and Southeast Asia: do they differ? Rev. Panam. Salud Publica 20:407-415. [DOI] [PubMed] [Google Scholar]
- 85.Halstead, S. B. 1970. Observations related to pathogensis of dengue hemorrhagic fever. VI. Hypotheses and discussion. Yale J. Biol. Med. 42:350-362. [PMC free article] [PubMed] [Google Scholar]
- 86.Halstead, S. B., S. Nimmannitya, and S. N. Cohen. 1970. Observations related to pathogenesis of dengue hemorrhagic fever. IV. Relation of disease severity to antibody response and virus recovered. Yale J. Biol. Med. 42:311-328. [PMC free article] [PubMed] [Google Scholar]
- 87.Harris, E., E. Videa, L. Perez, E. Sandoval, Y. Tellez, M. L. Perez, R. Cuadra, J. Rocha, W. Idiaquez, R. E. Alonso, M. A. Delgado, L. A. Campo, F. Acevedo, A. Gonzalez, J. J. Amador, and A. Balmaseda. 2000. Clinical, epidemiologic, and virologic features of dengue in the 1998 epidemic in Nicaragua. Am. J. Trop. Med. Hyg. 63:5-11. [DOI] [PubMed] [Google Scholar]
- 88.Hayden, F. G., R. Fritz, M. C. Lobo, W. Alvord, W. Strober, and S. E. Straus. 1998. Local and systemic cytokine responses during experimental human influenza A virus infection. Relation to symptom formation and host defense. J. Clin. Investig. 101:643-649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Heller, M. V., M. C. Saavedra, R. Falcoff, J. I. Maiztegui, and F. C. Molinas. 1992. Increased tumor necrosis factor-alpha levels in Argentine hemorrhagic fever. J. Infect. Dis. 166:1203-1204. [DOI] [PubMed] [Google Scholar]
- 90.Hjelm, F., F. Carlsson, A. Getahun, and B. Heyman. 2006. Antibody-mediated regulation of the immune response. Scand. J. Immunol. 64:177-184. [DOI] [PubMed] [Google Scholar]
- 91.Ho, L. J., M. F. Shaio, D. M. Chang, C. L. Liao, and J. H. Lai. 2004. Infection of human dendritic cells by dengue virus activates and primes T cells towards Th0-like phenotype producing both Th1 and Th2 cytokines. Immunol. Investig. 33:423-437. [DOI] [PubMed] [Google Scholar]
- 92.Ho, L. J., J. J. Wang, M. F. Shaio, C. L. Kao, D. M. Chang, S. W. Han, and J. H. Lai. 2001. Infection of human dendritic cells by dengue virus causes cell maturation and cytokine production. J. Immunol. 166:1499-1506. [DOI] [PubMed] [Google Scholar]
- 93.Hober, D., W. Chehadeh, A. Bouzidi, and P. Wattre. 2001. Antibody-dependent enhancement of coxsackievirus B4 infectivity of human peripheral blood mononuclear cells results in increased interferon-alpha synthesis. J. Infect. Dis. 184:1098-1108. [DOI] [PubMed] [Google Scholar]
- 94.Huang, Y. H., B. I. Chang, H. Y. Lei, H. S. Liu, C. C. Liu, H. L. Wu, and T. M. Yeh. 1997. Antibodies against dengue virus E protein peptide bind to human plasminogen and inhibit plasmin activity. Clin. Exp. Immunol. 110:35-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Huang, Y. H., H. Y. Lei, H. S. Liu, Y. S. Lin, C. C. Liu, and T. M. Yeh. 2000. Dengue virus infects human endothelial cells and induces IL-6 and IL-8 production. Am. J. Trop. Med. Hyg. 63:71-75. [DOI] [PubMed] [Google Scholar]
- 96.Huerre, M. R., N. T. Lan, P. Marianneau, N. B. Hue, H. Khun, N. T. Hung, N. T. Khen, M. T. Drouet, V. T. Huong, D. Q. Ha, Y. Buisson, and V. Deubel. 2001. Liver histopathology and biological correlates in five cases of fatal dengue fever in Vietnamese children. Virchows Arch. 438:107-115. [DOI] [PubMed] [Google Scholar]
- 97.Huerta-Zepeda, A., C. Cabello-Gutierrez, J. Cime-Castillo, V. Monroy-Martinez, M. E. Manjarrez-Zavala, M. Gutierrez-Rodriguez, R. Izaguirre, and B. H. Ruiz-Ordaz. 2008. Crosstalk between coagulation and inflammation during dengue virus infection. Thromb. Haemost. 99:936-943. [DOI] [PubMed] [Google Scholar]
- 98.Iankov, I. D., M. Pandey, M. Harvey, G. E. Griesmann, M. J. Federspiel, and S. J. Russell. 2006. Immunoglobulin G antibody-mediated enhancement of measles virus infection can bypass the protective antiviral immune response. J. Virol. 80:8530-8540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Imrie, A., J. Meeks, A. Gurary, M. Sukhbataar, P. Kitsutani, P. Effler, and Z. Zhao. 2007. Differential functional avidity of dengue virus-specific T-cell clones for variant peptides representing heterologous and previously encountered serotypes. J. Virol. 81:10081-10091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jassal, R., N. Jenkins, J. Charlwood, P. Camilleri, R. Jefferis, and J. Lund. 2001. Sialylation of human IgG-Fc carbohydrate by transfected rat alpha2,6-sialyltransferase. Biochem. Biophys. Res. Commun. 286:243-249. [DOI] [PubMed] [Google Scholar]
- 101.Jessie, K., M. Y. Fong, S. Devi, S. K. Lam, and K. T. Wong. 2004. Localization of dengue virus in naturally infected human tissues, by immunohistochemistry and in situ hybridization. J. Infect. Dis. 189:1411-1418. [DOI] [PubMed] [Google Scholar]
- 102.Reference deleted.
- 103.Juffrie, M., G. M. Meer, C. E. Hack, K. Haasnoot, Sutaryo, A. J. Veerman, and L. G. Thijs. 2001. Inflammatory mediators in dengue virus infection in children: interleukin-6 and its relation to C-reactive protein and secretory phospholipase A2. Am. J. Trop. Med. Hyg. 65:70-75. [DOI] [PubMed] [Google Scholar]
- 104.Kangwanpong, D., N. Bhamarapravati, and H. L. Lucia. 1995. Diagnosing dengue virus infection in archived autopsy tissues by means of the in situ PCR method: a case report. Clin. Diagn. Virol. 3:165-172. [DOI] [PubMed] [Google Scholar]
- 105.Kaplanski, G., B. Granel, T. Vaz, and J. M. Durand. 1998. Jarisch-Herxheimer reaction complicating the treatment of chronic Q. fever endocarditis: elevated TNFalpha and IL-6 serum levels. J. Infect. 37:83-84. [DOI] [PubMed] [Google Scholar]
- 106.Killen, H., and M. A. O'Sullivan. 1993. Detection of dengue virus by in situ hybridization. J. Virol. Methods 41:135-146. [DOI] [PubMed] [Google Scholar]
- 107.Kim, S. K., M. Cornberg, X. Z. Wang, H. D. Chen, L. K. Selin, and R. M. Welsh. 2005. Private specificities of CD8 T cell responses control patterns of heterologous immunity. J. Exp. Med. 201:523-533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kima, P. E., S. L. Constant, L. Hannum, M. Colmenares, K. S. Lee, A. M. Haberman, M. J. Shlomchik, and D. McMahon-Pratt. 2000. Internalization of Leishmania mexicana complex amastigotes via the Fc receptor is required to sustain infection in murine cutaneous leishmaniasis. J. Exp. Med. 191:1063-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kittigul, L., P. Pitakarnjanakul, D. Sujirarat, and K. Siripanichgon. 2007. The differences of clinical manifestations and laboratory findings in children and adults with dengue virus infection. J. Clin. Virol. 39:76-81. [DOI] [PubMed] [Google Scholar]
- 110.Klenerman, P., and R. M. Zinkernagel. 1998. Original antigenic sin impairs cytotoxic T lymphocyte responses to viruses bearing variant epitopes. Nature 394:482-485. [DOI] [PubMed] [Google Scholar]
- 111.Kliks, S. C., S. Nimmanitya, A. Nisalak, and D. S. Burke. 1988. Evidence that maternal dengue antibodies are important in the development of dengue hemorrhagic fever in infants. Am. J. Trop. Med. Hyg. 38:411-419. [DOI] [PubMed] [Google Scholar]
- 112.Kliks, S. C., A. Nisalak, W. E. Brandt, L. Wahl, and D. S. Burke. 1989. Antibody-dependent enhancement of dengue virus growth in human monocytes as a risk factor for dengue hemorrhagic fever. Am. J. Trop. Med. Hyg. 40:444-451. [DOI] [PubMed] [Google Scholar]
- 113.Koraka, P., S. Benton, G. van Amerongen, K. J. Stittelaar, and A. D. Osterhaus. 2007. Characterization of humoral and cellular immune responses in cynomolgus macaques upon primary and subsequent heterologous infections with dengue viruses. Microbes Infect. 9:940-946. [DOI] [PubMed] [Google Scholar]
- 114.Koraka, P., S. Benton, G. van Amerongen, K. J. Stittelaar, and A. D. Osterhaus. 2007. Efficacy of a live attenuated tetravalent candidate dengue vaccine in naive and previously infected cynomolgus macaques. Vaccine 25:5409-5416. [DOI] [PubMed] [Google Scholar]
- 115.Koraka, P., B. Murgue, X. Deparis, E. C. Van Gorp, T. E. Setiati, A. D. Osterhaus, and J. Groen. 2004. Elevation of soluble VCAM-1 plasma levels in children with acute dengue virus infection of varying severity. J. Med. Virol. 72:445-450. [DOI] [PubMed] [Google Scholar]
- 116.Koraka, P., C. Suharti, T. E. Setiati, A. T. Mairuhu, E. Van Gorp, C. E. Hack, M. Juffrie, J. Sutaryo, G. M. Van Der Meer, J. Groen, and A. D. Osterhaus. 2001. Kinetics of dengue virus-specific serum immunoglobulin classes and subclasses correlate with clinical outcome of infection. J. Clin. Microbiol. 39:4332-4338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kou, Z., M. Quinn, H. Chen, W. W. Rodrigo, R. C. Rose, J. J. Schlesinger, and X. Jin. 2008. Monocytes, but not T or B cells, are the principal target cells for dengue virus (DV) infection among human peripheral blood mononuclear cells. J. Med. Virol. 80:134-146. [DOI] [PubMed] [Google Scholar]
- 118.Kouri, G. P., M. G. Guzman, and J. R. Bravo. 1987. Why dengue haemorrhagic fever in Cuba? 2. An integral analysis. Trans. R. Soc. Trop. Med. Hyg. 81:821-823. [DOI] [PubMed] [Google Scholar]
- 119.Kouri, G. P., M. G. Guzman, J. R. Bravo, and C. Triana. 1989. Dengue haemorrhagic fever/dengue shock syndrome: lessons from the Cuban epidemic, 1981. Bull. W. H. O. 67:375-380. [PMC free article] [PubMed] [Google Scholar]
- 120.Krishnamurti, C., and B. Alving. 1989. Effect of dengue virus on procoagulant and fibrinolytic activities of monocytes. Rev. Infect. Dis. 11 Suppl. 4:S843-S846. [DOI] [PubMed] [Google Scholar]
- 121.Krishnamurti, C., S. Kalayanarooj, M. A. Cutting, R. A. Peat, S. W. Rothwell, T. J. Reid, S. Green, A. Nisalak, T. P. Endy, D. W. Vaughn, S. Nimmannitya, and B. L. Innis. 2001. Mechanisms of hemorrhage in dengue without circulatory collapse. Am. J. Trop. Med. Hyg. 65:840-847. [DOI] [PubMed] [Google Scholar]
- 122.Kurosu, T., P. Chaichana, M. Yamate, S. Anantapreecha, and K. Ikuta. 2007. Secreted complement regulatory protein clusterin interacts with dengue virus nonstructural protein 1. Biochem. Biophys. Res. Commun. 362:1051-1056. [DOI] [PubMed] [Google Scholar]
- 123.Kwan, W. H., A. M. Helt, C. Maranon, J. B. Barbaroux, A. Hosmalin, E. Harris, W. H. Fridman, and C. G. Mueller. 2005. Dendritic cell precursors are permissive to dengue virus and human immunodeficiency virus infection. J. Virol. 79:7291-7299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kyle, J. L., P. R. Beatty, and E. Harris. 2007. Dengue virus infects macrophages and dendritic cells in a mouse model of infection. J. Infect. Dis. 195:1808-1817. [DOI] [PubMed] [Google Scholar]
- 125.LaFleur, C., J. Granados, G. Vargas-Alarcon, J. Ruiz-Morales, C. Villarreal-Garza, L. Higuera, G. Hernandez-Pacheco, T. Cutino-Moguel, H. Rangel, R. Figueroa, M. Acosta, E. Lazcano, and C. Ramos. 2002. HLA-DR antigen frequencies in Mexican patients with dengue virus infection: HLA-DR4 as a possible genetic resistance factor for dengue hemorrhagic fever. Hum. Immunol. 63:1039-1044. [DOI] [PubMed] [Google Scholar]
- 126.Lancet. 1997. Dengue in the Americas—time to talk. Lancet 350:455. [PubMed] [Google Scholar]
- 127.Larroche, C., and L. Mouthon. 2004. Pathogenesis of hemophagocytic syndrome (HPS). Autoimmun. Rev. 3:69-75. [DOI] [PubMed] [Google Scholar]
- 128.Laur, F., B. Murgue, X. Deparis, C. Roche, O. Cassar, and E. Chungue. 1998. Plasma levels of tumour necrosis factor alpha and transforming growth factor beta-1 in children with dengue 2 virus infection in French Polynesia. Trans. R. Soc. Trop. Med. Hyg. 92:654-656. [DOI] [PubMed] [Google Scholar]
- 129.Lee, N., C. K. Wong, P. K. Chan, S. W. Lun, G. Lui, B. Wong, D. S. Hui, C. W. Lam, C. S. Cockram, K. W. Choi, A. C. Yeung, J. W. Tang, and J. J. Sung. 2007. Hypercytokinemia and hyperactivation of phospho-p38 mitogen-activated protein kinase in severe human influenza A virus infection. Clin. Infect. Dis. 45:723-731. [DOI] [PubMed] [Google Scholar]
- 130.Lee, Y. R., M. T. Liu, H. Y. Lei, C. C. Liu, J. M. Wu, Y. C. Tung, Y. S. Lin, T. M. Yeh, S. H. Chen, and H. S. Liu. 2006. MCP-1, a highly expressed chemokine in dengue haemorrhagic fever/dengue shock syndrome patients, may cause permeability change, possibly through reduced tight junctions of vascular endothelium cells. J. Gen. Virol. 87:3623-3630. [DOI] [PubMed] [Google Scholar]
- 131.Leitmeyer, K. C., D. W. Vaughn, D. M. Watts, R. Salas, I. Villalobos, C. de, C. Ramos, and R. Rico-Hesse. 1999. Dengue virus structural differences that correlate with pathogenesis. J. Virol. 73:4738-4747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Libraty, D. H., T. P. Endy, H. S. Houng, S. Green, S. Kalayanarooj, S. Suntayakorn, W. Chansiriwongs, D. W. Vaughn, A. Nisalak, F. A. Ennis, and A. L. Rothman. 2002. Differing influences of virus burden and immune activation on disease severity in secondary dengue-3 virus infections. J. Infect. Dis. 185:1213-1221. [DOI] [PubMed] [Google Scholar]
- 133.Libraty, D. H., S. Pichyangkul, C. Ajariyakhajorn, T. P. Endy, and F. A. Ennis. 2001. Human dendritic cells are activated by dengue virus infection: enhancement by gamma interferon and implications for disease pathogenesis. J. Virol. 75:3501-3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Libraty, D. H., P. R. Young, D. Pickering, T. P. Endy, S. Kalayanarooj, S. Green, D. W. Vaughn, A. Nisalak, F. A. Ennis, and A. L. Rothman. 2002. High circulating levels of the dengue virus nonstructural protein NS1 early in dengue illness correlate with the development of dengue hemorrhagic fever. J. Infect. Dis. 186:1165-1168. [DOI] [PubMed] [Google Scholar]
- 135.Lidbury, B. A., and S. Mahalingam. 2000. Specific ablation of antiviral gene expression in macrophages by antibody-dependent enhancement of Ross River virus infection. J. Virol. 74:8376-8381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Limon-Flores, A. Y., M. Perez-Tapia, I. Estrada-Garcia, G. Vaughan, A. Escobar-Gutierrez, J. Calderon-Amador, S. E. Herrera-Rodriguez, A. Brizuela-Garcia, M. Heras-Chavarria, A. Flores-Langarica, L. Cedillo-Barron, and L. Flores-Romo. 2005. Dengue virus inoculation to human skin explants: an effective approach to assess in situ the early infection and the effects on cutaneous dendritic cells. Int. J. Exp. Pathol. 86:323-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Limonta, D., V. Capo, G. Torres, A. B. Perez, and M. G. Guzman. 2007. Apoptosis in tissues from fatal dengue shock syndrome. J. Clin. Virol. 40:50-54. [DOI] [PubMed] [Google Scholar]
- 138.Lin, C. F., S. C. Chiu, Y. L. Hsiao, S. W. Wan, H. Y. Lei, A. L. Shiau, H. S. Liu, T. M. Yeh, S. H. Chen, C. C. Liu, and Y. S. Lin. 2005. Expression of cytokine, chemokine, and adhesion molecules during endothelial cell activation induced by antibodies against dengue virus nonstructural protein 1. J. Immunol. 174:395-403. [DOI] [PubMed] [Google Scholar]
- 139.Lin, C. F., H. Y. Lei, C. C. Liu, H. S. Liu, T. M. Yeh, S. T. Wang, T. I. Yang, F. C. Sheu, C. F. Kuo, and Y. S. Lin. 2001. Generation of IgM anti-platelet autoantibody in dengue patients. J. Med. Virol. 63:143-149. [PubMed] [Google Scholar]
- 140.Lin, C. F., H. Y. Lei, A. L. Shiau, C. C. Liu, H. S. Liu, T. M. Yeh, S. H. Chen, and Y. S. Lin. 2003. Antibodies from dengue patient sera cross-react with endothelial cells and induce damage. J. Med. Virol. 69:82-90. [DOI] [PubMed] [Google Scholar]
- 141.Lin, C. F., H. Y. Lei, A. L. Shiau, H. S. Liu, T. M. Yeh, S. H. Chen, C. C. Liu, S. C. Chiu, and Y. S. Lin. 2002. Endothelial cell apoptosis induced by antibodies against dengue virus nonstructural protein 1 via production of nitric oxide. J. Immunol. 169:657-664. [DOI] [PubMed] [Google Scholar]
- 142.Lin, C. F., S. W. Wan, M. C. Chen, S. C. Lin, C. C. Cheng, S. C. Chiu, Y. L. Hsiao, H. Y. Lei, H. S. Liu, T. M. Yeh, and Y. S. Lin. 2008. Liver injury caused by antibodies against dengue virus nonstructural protein 1 in a murine model. Lab. Investig. 88:1079-1089. [DOI] [PubMed] [Google Scholar]
- 143.Loke, H., D. Bethell, C. X. Phuong, N. Day, N. White, J. Farrar, and A. Hill. 2002. Susceptibility to dengue hemorrhagic fever in Vietnam: evidence of an association with variation in the vitamin d receptor and Fc gamma receptor IIa genes. Am. J. Trop. Med. Hyg. 67:102-106. [DOI] [PubMed] [Google Scholar]
- 144.Loke, H., D. B. Bethell, C. X. Phuong, M. Dung, J. Schneider, N. J. White, N. P. Day, J. Farrar, and A. V. Hill. 2001. Strong HLA class I-restricted T cell responses in dengue hemorrhagic fever: a double-edged sword? J. Infect. Dis. 184:1369-1373. [DOI] [PubMed] [Google Scholar]
- 145.Luplertlop, N., D. Misse, D. Bray, V. Deleuze, J. P. Gonzalez, V. Leardkamolkarn, H. Yssel, and F. Veas. 2006. Dengue-virus-infected dendritic cells trigger vascular leakage through metalloproteinase overproduction. EMBO Rep. 7:1176-1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ma, H., and J. A. Kapp. 2000. Antigenic epitopes regulate the phenotype of CD8+ CTL primed by exogenous antigens. J. Immunol. 164:5698-5703. [DOI] [PubMed] [Google Scholar]
- 147.Ma, H., and J. A. Kapp. 2001. Peptide affinity for MHC influences the phenotype of CD8(+) T cells primed in vivo. Cell. Immunol. 214:89-96. [DOI] [PubMed] [Google Scholar]
- 148.Mabalirajan, U., T. Kadhiravan, S. K. Sharma, A. Banga, and B. Ghosh. 2005. Th(2) immune response in patients with dengue during defervescence: preliminary evidence. Am. J. Trop. Med. Hyg. 72:783-785. [PubMed] [Google Scholar]
- 149.Reference deleted.
- 150.Mahalingam, S., and B. A. Lidbury. 2003. Antibody-dependent enhancement of infection: bacteria do it too. Trends Immunol. 24:465-467. [DOI] [PubMed] [Google Scholar]
- 151.Mahalingam, S., and B. A. Lidbury. 2002. Suppression of lipopolysaccharide-induced antiviral transcription factor (STAT-1 and NF-kappa B) complexes by antibody-dependent enhancement of macrophage infection by Ross River virus. Proc. Natl. Acad. Sci. USA 99:13819-13824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Mairuhu, A. T., M. R. Mac Gillavry, T. E. Setiati, A. Soemantri, H. ten Cate, D. P. Brandjes, and E. C. van Gorp. 2003. Is clinical outcome of dengue-virus infections influenced by coagulation and fibrinolysis? A critical review of the evidence. Lancet Infect. Dis. 3:33-41. [DOI] [PubMed] [Google Scholar]
- 153.Mairuhu, A. T., T. E. Setiati, P. Koraka, C. E. Hack, A. Leyte, S. M. Faradz, C. H. ten, D. P. Brandjes, A. D. Osterhaus, P. H. Reitsma, and E. C. van Gorp. 2005. Increased PAI-1 plasma levels and risk of death from dengue: no association with the 4G/5G promoter polymorphism. Thromb. J. 3:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Mangada, M. M., T. P. Endy, A. Nisalak, S. Chunsuttiwat, D. W. Vaughn, D. H. Libraty, S. Green, F. A. Ennis, and A. L. Rothman. 2002. Dengue-specific T cell responses in peripheral blood mononuclear cells obtained prior to secondary dengue virus infections in Thai schoolchildren. J. Infect. Dis. 185:1697-1703. [DOI] [PubMed] [Google Scholar]
- 155.Marchette, N. J., and S. B. Halstead. 1973. Survival of dengue virus in post mortem samples of tissues from experimentally infected rhesus monkeys. Am. J. Trop. Med. Hyg. 22:242-243. [DOI] [PubMed] [Google Scholar]
- 156.Marchette, N. J., S. B. Halstead, W. A. Falkler, Jr., A. Stenhouse, and D. Nash. 1973. Studies on the pathogenesis of dengue infection in monkeys. 3. Sequential distribution of virus in primary and heterologous infections. J. Infect. Dis. 128:23-30. [DOI] [PubMed] [Google Scholar]
- 157.Marchette, N. J., S. B. Halstead, D. R. Nash, and A. C. Stenhouse. 1972. Recovery of dengue viruses from tissues of experimentally infected rhesus monkeys. Appl. Microbiol. 24:328-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Markiewski, M. M., B. Nilsson, K. N. Ekdahl, T. E. Mollnes, and J. D. Lambris. 2007. Complement and coagulation: strangers or partners in crime? Trends Immunol. 28:184-192. [DOI] [PubMed] [Google Scholar]
- 159.Markoff, L. J., B. L. Innis, R. Houghten, and L. S. Henchal. 1991. Development of cross-reactive antibodies to plasminogen during the immune response to dengue virus infection. J. Infect. Dis. 164:294-301. [DOI] [PubMed] [Google Scholar]
- 160.Marta, R. F., V. S. Montero, C. E. Hack, A. Sturk, J. I. Maiztegui, and F. C. Molinas. 1999. Proinflammatory cytokines and elastase-alpha-1-antitrypsin in Argentine hemorrhagic fever. Am. J. Trop. Med. Hyg. 60:85-89. [DOI] [PubMed] [Google Scholar]
- 161.Mathew, A., I. Kurane, S. Green, D. W. Vaughn, S. Kalayanarooj, S. Suntayakorn, F. A. Ennis, and A. L. Rothman. 1999. Impaired T cell proliferation in acute dengue infection. J. Immunol. 162:5609-5615. [PubMed] [Google Scholar]
- 162.Medin, C. L., K. A. Fitzgerald, and A. L. Rothman. 2005. Dengue virus nonstructural protein NS5 induces interleukin-8 transcription and secretion. J. Virol. 79:11053-11061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Mehlhop, E., C. Ansarah-Sobrinho, S. Johnson, M. Engle, D. H. Fremont, T. C. Pierson, and M. S. Diamond. 2007. Complement protein C1q inhibits antibody-dependent enhancement of flavivirus infection in an IgG subclass-specific manner. Cell Host Microbes 2:417-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Miagostovich, M. P., R. G. Ramos, A. F. Nicol, R. M. Nogueira, T. Cuzzi-Maya, A. V. Oliveira, R. S. Marchevsky, R. P. Mesquita, and H. G. Schatzmayr. 1997. Retrospective study on dengue fatal cases. Clin. Neuropathol. 16:204-208. [PubMed] [Google Scholar]
- 165.Mongkolsapaya, J., W. Dejnirattisai, X. N. Xu, S. Vasanawathana, N. Tangthawornchaikul, A. Chairunsri, S. Sawasdivorn, T. Duangchinda, T. Dong, S. Rowland-Jones, P. T. Yenchitsomanus, A. McMichael, P. Malasit, and G. Screaton. 2003. Original antigenic sin and apoptosis in the pathogenesis of dengue hemorrhagic fever. Nat. Med. 9:921-927. [DOI] [PubMed] [Google Scholar]
- 166.Mongkolsapaya, J., T. Duangchinda, W. Dejnirattisai, S. Vasanawathana, P. Avirutnan, A. Jairungsri, N. Khemnu, N. Tangthawornchaikul, P. Chotiyarnwong, K. Sae-Jang, M. Koch, Y. Jones, A. McMichael, X. Xu, P. Malasit, and G. Screaton. 2006. T cell responses in dengue hemorrhagic fever: are cross-reactive T cells suboptimal? J. Immunol. 176:3821-3829. [DOI] [PubMed] [Google Scholar]
- 167.Morel, J. C., C. C. Park, J. M. Woods, and A. E. Koch. 2001. A novel role for interleukin-18 in adhesion molecule induction through NF kappa B and phosphatidylinositol (PI) 3-kinase-dependent signal transduction pathways. J. Biol. Chem. 276:37069-37075. [DOI] [PubMed] [Google Scholar]
- 168.Murgue, B., O. Cassar, and X. Deparis. 2001. Plasma concentrations of sVCAM-1 and severity of dengue infections. J. Med. Virol. 65:97-104. [PubMed] [Google Scholar]
- 169.Mustafa, A. S., E. A. Elbishbishi, R. Agarwal, and U. C. Chaturvedi. 2001. Elevated levels of interleukin-13 and IL-18 in patients with dengue hemorrhagic fever. FEMS Immunol. Med. Microbiol. 30:229-233. [DOI] [PubMed] [Google Scholar]
- 170.Nachman, R. L., and S. Rafii. 2008. Platelets, petechiae, and preservation of the vascular wall. N. Engl. J. Med. 359:1261-1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Nakao, S., C. J. Lai, and N. S. Young. 1989. Dengue virus, a flavivirus, propagates in human bone marrow progenitors and hematopoietic cell lines. Blood 74:1235-1240. [PubMed] [Google Scholar]
- 172.Nguyen, T. H., H. Y. Lei, T. L. Nguyen, Y. S. Lin, K. J. Huang, B. L. Le, C. F. Lin, T. M. Yeh, Q. H. Do, T. Q. Vu, L. C. Chen, J. H. Huang, T. M. Lam, C. C. Liu, and S. B. Halstead. 2004. Dengue hemorrhagic fever in infants: a study of clinical and cytokine profiles. J. Infect. Dis. 189:221-232. [DOI] [PubMed] [Google Scholar]
- 173.Nisalak, A., S. B. Halstead, P. Singharaj, S. Udomsakdi, S. W. Nye, and K. Vinijchaikul. 1970. Observations related to pathogenesis of dengue hemorrhagic fever. 3. Virologic studies of fatal disease. Yale J. Biol. Med. 42:293-310. [PMC free article] [PubMed] [Google Scholar]
- 174.Nishioka, K. 1974. Serum complement level in dengue hemorrhagic fever. Allerg. Immunol. (Leipz) 21:385-392. [PubMed] [Google Scholar]
- 175.Nkhoma, E. T., C. Poole, V. Vannappagari, S. A. Hall, and E. Beutler. 2009. The global prevalence of glucose-6-phosphate dehydrogenase deficiency: a systematic review and meta-analysis. Blood Cells Mol. Dis. 42:267-278. [DOI] [PubMed] [Google Scholar]
- 176.Ogawa, Y., and J. A. Grant. 2007. Mediators of anaphylaxis. Immunol. Allergy Clin. N. Am. 27:249-260, vii. [DOI] [PubMed] [Google Scholar]
- 177.Oishi, K., S. Inoue, M. T. Cinco, E. M. Dimaano, M. T. Alera, J. A. Alfon, F. Abanes, D. J. Cruz, R. R. Matias, H. Matsuura, F. Hasebe, S. Tanimura, A. Kumatori, K. Morita, F. F. Natividad, and T. Nagatake. 2003. Correlation between increased platelet-associated IgG and thrombocytopenia in secondary dengue virus infections. J. Med. Virol. 71:259-264. [DOI] [PubMed] [Google Scholar]
- 178.Ong, A., M. Sandar, M. I. Chen, and L. Y. Sin. 2007. Fatal dengue hemorrhagic fever in adults during a dengue epidemic in Singapore. Int. J. Infect. Dis. 11:263-267. [DOI] [PubMed] [Google Scholar]
- 179.Reference deleted.
- 180.Padigel, U. M., and J. P. Farrell. 2005. Control of infection with Leishmania major in susceptible BALB/c mice lacking the common gamma-chain for FcR is associated with reduced production of IL-10 and TGF-beta by parasitized cells. J. Immunol. 174:6340-6345. [DOI] [PubMed] [Google Scholar]
- 181.Paes, M. V., A. T. Pinhao, D. F. Barreto, S. M. Costa, M. P. Oliveira, A. C. Nogueira, C. M. Takiya, J. C. Farias-Filho, H. G. Schatzmayr, A. M. Alves, and O. M. Barth. 2005. Liver injury and viremia in mice infected with dengue-2 virus. Virology 338:236-246. [DOI] [PubMed] [Google Scholar]
- 182.Palmer, D. R., P. Sun, C. Celluzzi, J. Bisbing, S. Pang, W. Sun, M. A. Marovich, and T. Burgess. 2005. Differential effects of dengue virus on infected and bystander dendritic cells. J. Virol. 79:2432-2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Perez, A. B., G. Garcia, B. Sierra, M. Alvarez, S. Vazquez, M. V. Cabrera, R. Rodriguez, D. Rosario, E. Martinez, T. Denny, and M. G. Guzman. 2004. IL-10 levels in dengue patients: some findings from the exceptional epidemiological conditions in Cuba. J. Med. Virol. 73:230-234. [DOI] [PubMed] [Google Scholar]
- 184.Peyrefitte, C. N., B. Pastorino, G. E. Grau, J. Lou, H. Tolou, and P. Couissinier-Paris. 2006. Dengue virus infection of human microvascular endothelial cells from different vascular beds promotes both common and specific functional changes. J. Med. Virol. 78:229-242. [DOI] [PubMed] [Google Scholar]
- 185.Picard, C., J. L. Casanova, and L. Abel. 2006. Mendelian traits that confer predisposition or resistance to specific infections in humans. Curr. Opin. Immunol. 18:383-390. [DOI] [PubMed] [Google Scholar]
- 186.Pinheiro, F. P., and S. J. Corber. 1997. Global situation of dengue and dengue haemorrhagic fever, and its emergence in the Americas. World Health Stat. Q. 50:161-169. [PubMed] [Google Scholar]
- 187.Polizel, J. R., D. Bueno, J. E. Visentainer, A. M. Sell, S. D. Borelli, L. T. Tsuneto, M. M. Dalalio, M. T. Coimbra, and R. A. Moliterno. 2004. Association of human leukocyte antigen DQ1 and dengue fever in a white Southern Brazilian population. Mem. Inst. Oswaldo Cruz 99:559-562. [DOI] [PubMed] [Google Scholar]
- 188.Pongsumpun, P., S. Yoksan, and I. M. Tan. 2002. A comparison of the age distributions in the dengue hemorrhagic fever epidemics in Santiago de Cuba (1997) and Thailand (1998). Southeast Asian J. Trop. Med. Public Health 33:255-258. [PubMed] [Google Scholar]
- 189.Ponnuraj, E. M., J. Springer, A. R. Hayward, H. Wilson, and E. A. Simoes. 2003. Antibody-dependent enhancement, a possible mechanism in augmented pulmonary disease of respiratory syncytial virus in the Bonnet monkey model. J. Infect. Dis. 187:1257-1263. [DOI] [PubMed] [Google Scholar]
- 190.Quaresma, J. A., V. L. Barros, C. Pagliari, E. R. Fernandes, H. F. Andrade, Jr., P. F. Vasconcelos, and M. I. Duarte. 2007. Hepatocyte lesions and cellular immune response in yellow fever infection. Trans. R. Soc. Trop. Med. Hyg. 101:161-168. [DOI] [PubMed] [Google Scholar]
- 191.Quaresma, J. A., V. L. Barros, C. Pagliari, E. R. Fernandes, F. Guedes, C. F. Takakura, H. F. Andrade, Jr., P. F. Vasconcelos, and M. I. Duarte. 2006. Revisiting the liver in human yellow fever: virus-induced apoptosis in hepatocytes associated with TGF-beta, TNF-alpha and NK cells activity. Virology. 345:22-30. [DOI] [PubMed] [Google Scholar]
- 192.Raghupathy, R., U. C. Chaturvedi, H. Al-Sayer, E. A. Elbishbishi, R. Agarwal, R. Nagar, S. Kapoor, A. Misra, A. Mathur, H. Nusrat, F. Azizieh, M. A. Khan, and A. S. Mustafa. 1998. Elevated levels of IL-8 in dengue hemorrhagic fever. J. Med. Virol. 56:280-285. [DOI] [PubMed] [Google Scholar]
- 193.Ravelli, A. 2002. Macrophage activation syndrome. Curr. Opin. Rheumatol. 14:548-552. [DOI] [PubMed] [Google Scholar]
- 194.Restrepo, B. N., D. M. Isaza, C. L. Salazar, R. Ramirez, M. Ospina, and L. G. Alvarez. 2008. Serum levels of interleukin-6, tumor necrosis factor-alpha and interferon-gamma in infants with and without dengue. Rev. Soc. Bras. Med. Trop. 41:6-10. [DOI] [PubMed] [Google Scholar]
- 195.Rico-Hesse, R. 1990. Molecular evolution and distribution of dengue viruses type 1 and 2 in nature. Virology 174:479-493. [DOI] [PubMed] [Google Scholar]
- 196.Rico-Hesse, R., L. M. Harrison, A. Nisalak, D. W. Vaughn, S. Kalayanarooj, S. Green, A. L. Rothman, and F. A. Ennis. 1998. Molecular evolution of dengue type 2 virus in Thailand. Am. J. Trop. Med. Hyg. 58:96-101. [DOI] [PubMed] [Google Scholar]
- 197.Rico-Hesse, R., L. M. Harrison, R. A. Salas, D. Tovar, A. Nisalak, C. Ramos, J. Boshell, M. T. de Mesa, R. M. Nogueira, and A. T. da Rosa. 1997. Origins of dengue type 2 viruses associated with increased pathogenicity in the Americas. Virology 230:244-251. [DOI] [PubMed] [Google Scholar]
- 198.Rodriguez-Roche, R., M. Alvarez, T. Gritsun, S. Halstead, G. Kouri, E. A. Gould, and M. G. Guzman. 2005. Virus evolution during a severe dengue epidemic in Cuba, 1997. Virology 334:154-159. [DOI] [PubMed] [Google Scholar]
- 199.Rosen, L., M. T. Drouet, and V. Deubel. 1999. Detection of dengue virus RNA by reverse transcription-polymerase chain reaction in the liver and lymphoid organs but not in the brain in fatal human infection. Am. J. Trop. Med. Hyg. 61:720-724. [DOI] [PubMed] [Google Scholar]
- 200.Rosenberg, R. D. 2001. Vascular-bed-specific hemostasis and hypercoagulable states: clinical utility of activation peptide assays in predicting thrombotic events in different clinical populations. Thromb. Haemost. 86:41-50. [PubMed] [Google Scholar]
- 201.Rosenberg, R. D., and W. C. Aird. 1999. Vascular-bed-specific hemostasis and hypercoagulable states. N. Engl. J. Med. 340:1555-1564. [DOI] [PubMed] [Google Scholar]
- 202.Rothwell, S. W., R. Putnak, and V. F. La Russa. 1996. Dengue-2 virus infection of human bone marrow: characterization of dengue-2 antigen-positive stromal cells. Am. J. Trop. Med. Hyg. 54:503-510. [DOI] [PubMed] [Google Scholar]
- 203.Sahaphong, S., S. Riengrojpitak, N. Bhamarapravati, and T. Chirachariyavej. 1980. Electron microscopic study of the vascular endothelial cell in dengue hemorrhagic fever. Southeast Asian J. Trop. Med. Public Health 11:194-204. [PubMed] [Google Scholar]
- 204.Saito, M., K. Oishi, S. Inoue, E. M. Dimaano, M. T. Alera, A. M. Robles, B. D. Estrella, Jr., A. Kumatori, K. Moji, M. T. Alonzo, C. C. Buerano, R. R. Matias, K. Morita, F. F. Natividad, and T. Nagatake. 2004. Association of increased platelet-associated immunoglobulins with thrombocytopenia and the severity of disease in secondary dengue virus infections. Clin. Exp. Immunol. 138:299-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Sakuntabhai, A., C. Turbpaiboon, I. Casademont, A. Chuansumrit, T. Lowhnoo, A. Kajaste-Rudnitski, S. M. Kalayanarooj, K. Tangnararatchakit, N. Tangthawornchaikul, S. Vasanawathana, W. Chaiyaratana, P. T. Yenchitsomanus, P. Suriyaphol, P. Avirutnan, K. Chokephaibulkit, F. Matsuda, S. Yoksan, Y. Jacob, G. M. Lathrop, P. Malasit, P. Despres, and C. Julier. 2005. A variant in the CD209 promoter is associated with severity of dengue disease. Nat. Genet. 37:507-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Sanchez, I. J., and B. H. Ruiz. 1996. A single nucleotide change in the E protein gene of dengue virus 2 Mexican strain affects neurovirulence in mice. J. Gen. Virol. 77:2541-2545. [DOI] [PubMed] [Google Scholar]
- 207.Sangkawibha, N., S. Rojanasuphot, S. Ahandrik, S. Viriyapongse, S. Jatanasen, V. Salitul, B. Phanthumachinda, and S. B. Halstead. 1984. Risk factors in dengue shock syndrome: a prospective epidemiologic study in Rayong, Thailand. I. The 1980 outbreak. Am. J. Epidemiol. 120:653-669. [DOI] [PubMed] [Google Scholar]
- 208.Sariol, C. A., J. L. Pelegrino, A. Martinez, E. Arteaga, G. Kouri, and M. G. Guzman. 1999. Detection and genetic relationship of dengue virus sequences in seventeen-year-old paraffin-embedded samples from Cuba. Am. J. Trop. Med. Hyg. 61:994-1000. [DOI] [PubMed] [Google Scholar]
- 209.Selin, L. K., M. A. Brehm, Y. N. Naumov, M. Cornberg, S. K. Kim, S. C. Clute, and R. M. Welsh. 2006. Memory of mice and men: CD8+ T-cell cross-reactivity and heterologous immunity. Immunol. Rev. 211:164-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Selin, L. K., M. Cornberg, M. A. Brehm, S. K. Kim, C. Calcagno, D. Ghersi, R. Puzone, F. Celada, and R. M. Welsh. 2004. CD8 memory T cells: cross-reactivity and heterologous immunity. Semin. Immunol. 16:335-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Selin, L. K., S. M. Varga, I. C. Wong, and R. M. Welsh. 1998. Protective heterologous antiviral immunity and enhanced immunopathogenesis mediated by memory T cell populations. J. Exp. Med. 188:1705-1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Seneviratne, S. L., G. N. Malavige, and H. J. de Silva. 2006. Pathogenesis of liver involvement during dengue viral infections. Trans. R. Soc. Trop. Med. Hyg. 100:608-614. [DOI] [PubMed] [Google Scholar]
- 213.Setiati, T. E., A. T. Mairuhu, P. Koraka, M. Supriatna, M. R. Mac Gillavry, D. P. Brandjes, A. D. Osterhaus, J. W. van der Meer, E. C. van Gorp, and A. Soemantri. 2007. Dengue disease severity in Indonesian children: an evaluation of the World Health Organization classification system. BMC Infect. Dis. 7:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Shaio, M. F., F. Y. Chang, and S. C. Hou. 1992. Complement pathway activity in serum from patients with classical dengue fever. Trans. R. Soc. Trop. Med. Hyg. 86:672-675. [DOI] [PubMed] [Google Scholar]
- 215.Sharma, J. N., A. Al-Omran, and S. S. Parvathy. 2007. Role of nitric oxide in inflammatory diseases. Inflammopharmacology 15:252-259. [DOI] [PubMed] [Google Scholar]
- 216.Shen, B. Q., D. Y. Lee, K. M. Cortopassi, L. A. Damico, and T. F. Zioncheck. 2001. Vascular endothelial growth factor KDR receptor signaling potentiates tumor necrosis factor-induced tissue factor expression in endothelial cells. J. Biol. Chem. 276:5281-5286. [DOI] [PubMed] [Google Scholar]
- 217.Shresta, S., K. L. Sharar, D. M. Prigozhin, P. R. Beatty, and E. Harris. 2006. Murine model for dengue virus-induced lethal disease with increased vascular permeability. J. Virol. 80:10208-10217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Shu, P. Y., L. K. Chen, S. F. Chang, Y. Y. Yueh, L. Chow, L. J. Chien, C. Chin, T. H. Lin, and J. H. Huang. 2000. Dengue NS1-specific antibody responses: isotype distribution and serotyping in patients with dengue fever and dengue hemorrhagic fever. J. Med. Virol. 62:224-232. [DOI] [PubMed] [Google Scholar]
- 219.Reference deleted.
- 220.Reference deleted.
- 221.Simmons, C. P., T. N. Chau, T. T. Thuy, N. M. Tuan, D. M. Hoang, N. T. Thien, B. Lien le, N. T. Quy, N. T. Hieu, T. T. Hien, C. McElnea, P. Young, S. Whitehead, N. T. Hung, and J. Farrar. 2007. Maternal antibody and viral factors in the pathogenesis of dengue virus in infants. J. Infect. Dis. 196:416-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Snyder, J. T., M. A. Alexander-Miller, J. A. Berzofskyl, and I. M. Belyakov. 2003. Molecular mechanisms and biological significance of CTL avidity. Curr. HIV Res. 1:287-294. [DOI] [PubMed] [Google Scholar]
- 223.Sosothikul, D., P. Seksarn, S. Pongsewalak, U. Thisyakorn, and J. Lusher. 2007. Activation of endothelial cells, coagulation and fibrinolysis in children with dengue virus infection. Thromb. Haemost. 97:627-634. [PubMed] [Google Scholar]
- 224.Soundravally, R., and S. L. Hoti. 2007. Immunopathogenesis of dengue hemorrhagic fever and shock syndrome: role of TAP and HPA gene polymorphism. Hum. Immunol. 68:973-979. [DOI] [PubMed] [Google Scholar]
- 225.Soundravally, R., and S. L. Hoti. 2008. Polymorphisms of the TAP 1 and 2 gene may influence clinical outcome of primary dengue viral infection. Scand. J. Immunol. 67:618-625. [DOI] [PubMed] [Google Scholar]
- 226.Reference deleted.
- 227.Sreedharan, A., S. Bowyer, C. A. Wallace, M. J. Robertson, K. Schmidt, A. E. Woolfrey, and R. P. Nelson, Jr. 2006. Macrophage activation syndrome and other systemic inflammatory conditions after BMT. Bone Marrow Transplant. 37:629-634. [DOI] [PubMed] [Google Scholar]
- 228.Srichaikul, T., and S. Nimmannitya. 2000. Haematology in dengue and dengue haemorrhagic fever. Baillieres Best Pract. Res. Clin. Haematol. 13:261-276. [DOI] [PubMed] [Google Scholar]
- 229.Srikiatkhachorn, A., C. Ajariyakhajorn, T. P. Endy, S. Kalayanarooj, D. H. Libraty, S. Green, F. A. Ennis, and A. L. Rothman. 2007. Virus-induced decline in soluble vascular endothelial growth receptor 2 is associated with plasma leakage in dengue hemorrhagic fever. J. Virol. 81:1592-1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Srikiatkhachorn, A., A. Krautrachue, W. Ratanaprakarn, L. Wongtapradit, N. Nithipanya, S. Kalayanarooj, A. Nisalak, S. J. Thomas, R. V. Gibbons, M. P. Mammen, Jr., D. H. Libraty, F. A. Ennis, A. L. Rothman, and S. Green. 2007. Natural history of plasma leakage in dengue hemorrhagic fever: a serial ultrasonographic study. Pediatr. Infect. Dis. J. 26:283-290. (Discussion, 26:291-292.) [DOI] [PubMed] [Google Scholar]
- 231.Stamatovic, S. M., R. F. Keep, S. L. Kunkel, and A. V. Andjelkovic. 2003. Potential role of MCP-1 in endothelial cell tight junction ‘opening’: signaling via Rho and Rho kinase. J. Cell Sci. 116:4615-4628. [DOI] [PubMed] [Google Scholar]
- 232.Stephens, H. A., R. Klaythong, M. Sirikong, D. W. Vaughn, S. Green, S. Kalayanarooj, T. P. Endy, D. H. Libraty, A. Nisalak, B. L. Innis, A. L. Rothman, F. A. Ennis, and D. Chandanayingyong. 2002. HLA-A and -B allele associations with secondary dengue virus infections correlate with disease severity and the infecting viral serotype in ethnic Thais. Tissue Antigens 60:309-318. [DOI] [PubMed] [Google Scholar]
- 233.Strait, R., S. C. Morrist, and F. D. Finkelman. 2004. Cytokine enhancement of anaphylaxis. Novartis Found Symp 257:80-91. (Discussion, 257:91-100, 276-285.) [PubMed] [Google Scholar]
- 234.Streatfield, R., G. Bielby, and D. Sinclair. 1993. A primary dengue 2 epidemic with spontaneous haemorrhagic manifestations. Lancet 342:560-561. [DOI] [PubMed] [Google Scholar]
- 235.Subbramanian, R. A., J. Xu, E. Toma, R. Morisset, E. A. Cohen, J. Menezes, and A. Ahmad. 2002. Comparison of human immunodeficiency virus (HIV)-specific infection-enhancing and -inhibiting antibodies in AIDS patients. J. Clin. Microbiol. 40:2141-2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Suharti, C., E. C. van Gorp, T. E. Setiati, W. M. Dolmans, R. J. Djokomoeljanto, C. E. Hack, C. H. ten, and J. W. van der Meer. 2002. The role of cytokines in activation of coagulation and fibrinolysis in dengue shock syndrome. Thromb. Haemost. 87:42-46. [PubMed] [Google Scholar]
- 237.Sun, D. S., C. C. King, H. S. Huang, Y. L. Shih, C. C. Lee, W. J. Tsai, C. C. Yu, and H. H. Chang. 2007. Antiplatelet autoantibodies elicited by dengue virus non-structural protein 1 cause thrombocytopenia and mortality in mice. J. Thromb. Haemost. 5:2291-2299. [DOI] [PubMed] [Google Scholar]
- 238.Takada, A., H. Feldmann, T. G. Ksiazek, and Y. Kawaoka. 2003. Antibody-dependent enhancement of Ebola virus infection. J. Virol. 77:7539-7544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Takhampunya, R., R. Padmanabhan, and S. Ubol. 2006. Antiviral action of nitric oxide on dengue virus type 2 replication. J. Gen. Virol. 87:3003-3011. [DOI] [PubMed] [Google Scholar]
- 240.Tamura, M., R. G. Webster, and F. A. Ennis. 1994. Subtype cross-reactive, infection-enhancing antibody responses to influenza A viruses. J. Virol. 68:3499-3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.ter Meulen, J., M. Sakho, K. Koulemou, N. Magassouba, A. Bah, W. Preiser, S. Daffis, C. Klewitz, H. G. Bae, M. Niedrig, H. Zeller, M. Heinzel-Gutenbrunner, L. Koivogui, and A. Kaufmann. 2004. Activation of the cytokine network and unfavorable outcome in patients with yellow fever. J. Infect. Dis. 190:1821-1827. [DOI] [PubMed] [Google Scholar]
- 242.Thein, S., J. Aaskov, T. T. Myint, T. N. Shwe, T. T. Saw, and A. Zaw. 1993. Changes in levels of anti-dengue virus IgG subclasses in patients with disease of varying severity. J. Med. Virol. 40:102-106. [DOI] [PubMed] [Google Scholar]
- 243.Thiel, S., P. D. Frederiksen, and J. C. Jensenius. 2006. Clinical manifestations of mannan-binding lectin deficiency. Mol. Immunol. 43:86-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Thomas, B. N., and L. U. Buxbaum. 2008. FcgammaRIII mediates immunoglobulin G-induced interleukin-10 and is required for chronic Leishmania mexicana lesions. Infect. Immun. 76:623-631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Thomas, L., O. Verlaeten, A. Cabie, S. Kaidomar, V. Moravie, J. Martial, F. Najioullah, Y. Plumelle, C. Fonteau, P. Dussart, and R. Cesaire. 2008. Influence of the dengue serotype, previous dengue infection, and plasma viral load on clinical presentation and outcome during a dengue-2 and dengue-4 co-epidemic. Am. J. Trop. Med. Hyg. 78:990-998. [PubMed] [Google Scholar]
- 246.Thulkar, S., S. Sharma, D. N. Srivastava, S. K. Sharma, M. Berry, and R. M. Pandey. 2000. Sonographic findings in grade III dengue hemorrhagic fever in adults. J. Clin. Ultrasound. 28:34-37. [DOI] [PubMed] [Google Scholar]
- 247.To, K. F., P. K. Chan, K. F. Chan, W. K. Lee, W. Y. Lam, K. F. Wong, N. L. Tang, D. N. Tsang, R. Y. Sung, T. A. Buckley, J. S. Tam, and A. F. Cheng. 2001. Pathology of fatal human infection associated with avian influenza A H5N1 virus. J. Med. Virol. 63:242-246. [DOI] [PubMed] [Google Scholar]
- 248.Ubol, S., T. Chareonsirisuthigul, J. Kasisith, and C. Klungthong. 2008. Clinical isolates of dengue virus with distinctive susceptibility to nitric oxide radical induce differential gene responses in THP-1 cells. Virology 376:290-296. [DOI] [PubMed] [Google Scholar]
- 249.Ubol, S., P. Masrinoul, J. Chaijaruwanich, S. Kalayanarooj, T. Charoensirisuthikul, and J. Kasisith. 2008. Differences in global gene expression in peripheral blood mononuclear cells indicate a significant role of the innate responses in progression of dengue fever but not dengue hemorrhagic fever. J. Infect. Dis. 197:1459-1467. [DOI] [PubMed] [Google Scholar]
- 250.Urbani, S., B. Amadei, P. Fisicaro, M. Pilli, G. Missale, A. Bertoletti, and C. Ferrari. 2005. Heterologous T cell immunity in severe hepatitis C virus infection. J. Exp. Med. 201:675-680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Vaughn, D. W., S. Green, S. Kalayanarooj, B. L. Innis, S. Nimmannitya, S. Suntayakorn, T. P. Endy, B. Raengsakulrach, A. L. Rothman, F. A. Ennis, and A. Nisalak. 2000. Dengue viremia titer, antibody response pattern, and virus serotype correlate with disease severity. J. Infect. Dis. 181:2-9. [DOI] [PubMed] [Google Scholar]
- 252.Venkata Sai, P. M., B. Dev, and R. Krishnan. 2005. Role of ultrasound in dengue fever. Br. J. Radiol 78:416-418. [DOI] [PubMed] [Google Scholar]
- 253.Villinger, F., P. E. Rollin, S. S. Brar, N. F. Chikkala, J. Winter, J. B. Sundstrom, S. R. Zaki, R. Swanepoel, A. A. Ansari, and C. J. Peters. 1999. Markedly elevated levels of interferon (IFN)-gamma, IFN-alpha, interleukin (IL)-2, IL-10, and tumor necrosis factor-alpha associated with fatal Ebola virus infection. J. Infect. Dis. 179(Suppl. 1):S188-S191. [DOI] [PubMed] [Google Scholar]
- 254.Wahid, S. F., S. Sanusi, M. M. Zawawi, and R. A. Ali. 2000. A comparison of the pattern of liver involvement in dengue hemorrhagic fever with classic dengue fever. Southeast Asian J. Trop. Med. Public Health 31:259-263. [PubMed] [Google Scholar]
- 255.Wallace, M. J., D. W. Smith, A. K. Broom, J. S. Mackenzie, R. A. Hall, G. R. Shellam, and P. C. McMinn. 2003. Antibody-dependent enhancement of Murray Valley encephalitis virus virulence in mice. J. Gen. Virol. 84:1723-1728. [DOI] [PubMed] [Google Scholar]
- 256.Wang, C. C., C. C. Wu, J. W. Liu, A. S. Lin, S. F. Liu, Y. H. Chung, M. C. Su, I. K. Lee, and M. C. Lin. 2007. Chest radiographic presentation in patients with dengue hemorrhagic fever. Am. J. Trop. Med. Hyg. 77:291-296. [PubMed] [Google Scholar]
- 257.Wang, L., and S. M. Dudek. 2009. Regulation of vascular permeability by sphingosine 1-phosphate. Microvasc. Res. 77:39-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Wang, W. K., D. Y. Chao, C. L. Kao, H. C. Wu, Y. C. Liu, C. M. Li, S. C. Lin, S. T. Ho, J. H. Huang, and C. C. King. 2003. High levels of plasma dengue viral load during defervescence in patients with dengue hemorrhagic fever: implications for pathogenesis. Virology 305:330-338. [DOI] [PubMed] [Google Scholar]
- 259.Wang, W. K., H. L. Chen, C. F. Yang, S. C. Hsieh, C. C. Juan, S. M. Chang, C. C. Yu, L. H. Lin, J. H. Huang, and C. C. King. 2006. Slower rates of clearance of viral load and virus-containing immune complexes in patients with dengue hemorrhagic fever. Clin. Infect. Dis. 43:1023-1030. [DOI] [PubMed] [Google Scholar]
- 260.Wedemeyer, H., E. Mizukoshi, A. R. Davis, J. R. Bennink, and B. Rehermann. 2001. Cross-reactivity between hepatitis C virus and Influenza A virus determinant-specific cytotoxic T cells. J. Virol. 75:11392-11400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Wichmann, O., J. Gascon, M. Schunk, S. Puente, H. Siikamaki, I. Gjorup, R. Lopez-Velez, J. Clerinx, G. Peyerl-Hoffmann, A. Sundoy, B. Genton, P. Kern, G. Calleri, M. de Gorgolas, N. Muhlberger, T. Jelinek, and the European Network on Surveillance of Imported Infectious Diseases. 2007. Severe dengue virus infection in travelers: risk factors and laboratory indicators. J. Infect. Dis. 195:1089-1096. [DOI] [PubMed] [Google Scholar]
- 262.Wills, B. A., E. E. Oragui, A. C. Stephens, O. A. Daramola, N. M. Dung, H. T. Loan, N. V. Chau, M. Chambers, K. Stepniewska, J. J. Farrar, and M. Levin. 2002. Coagulation abnormalities in dengue hemorrhagic fever: serial investigations in 167 Vietnamese children with dengue shock syndrome. Clin. Infect. Dis. 35:277-285. [DOI] [PubMed] [Google Scholar]
- 262a.World Health Organization. 1997. Dengue haemorrhagic fever: diagnosis, treatment, prevention and control, 2nd ed. WHO, Geneva, Switzerland.
- 263.Wu, S. J., G. Grouard-Vogel, W. Sun, J. R. Mascola, E. Brachtel, R. Putvatana, M. K. Louder, L. Filgueira, M. A. Marovich, H. K. Wong, A. Blauvelt, G. S. Murphy, M. L. Robb, B. L. Innes, D. L. Birx, C. G. Hayes, and S. S. Frankel. 2000. Human skin Langerhans cells are targets of dengue virus infection. Nat. Med. 6:816-820. [DOI] [PubMed] [Google Scholar]
- 264.Wu, Y. H., C. P. Tseng, M. L. Cheng, H. Y. Ho, S. R. Shih, and D. T. Chiu. 2008. Glucose-6-phosphate dehydrogenase deficiency enhances human coronavirus 229E infection. J. Infect. Dis. 197:812-816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Yamada, M., S. Kim, K. Egashira, M. Takeya, T. Ikeda, O. Mimura, and H. Iwao. 2003. Molecular mechanism and role of endothelial monocyte chemoattractant protein-1 induction by vascular endothelial growth factor. Arterioscler. Thromb. Vasc. Biol. 23:1996-2001. [DOI] [PubMed] [Google Scholar]
- 266.Yamanaka, A., S. Kosugi, and E. Konishi. 2008. Infection-enhancing and -neutralizing activities of mouse monoclonal antibodies against dengue type 2 and 4 viruses are controlled by complement levels. J. Virol. 82:927-937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Yauch, L. E., and S. Shresta. 2008. Mouse models of dengue virus infection and disease. Antivir. Res. 80:87-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Yuen, K. Y., P. K. Chan, M. Peiris, D. N. Tsang, T. L. Que, K. F. Shortridge, P. T. Cheung, W. K. To, E. T. Ho, R. Sung, and A. F. Cheng. 1998. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet 351:467-471. [DOI] [PubMed] [Google Scholar]
- 269.Zampieri, C. A., N. J. Sullivan, and G. J. Nabel. 2007. Immunopathology of highly virulent pathogens: insights from Ebola virus. Nat. Immunol. 8:1159-1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Zivna, I., S. Green, D. W. Vaughn, S. Kalayanarooj, H. A. Stephens, D. Chandanayingyong, A. Nisalak, F. A. Ennis, and A. L. Rothman. 2002. T cell responses to an HLA-B*07-restricted epitope on the dengue NS3 protein correlate with disease severity. J. Immunol. 168:5959-5965. [DOI] [PubMed] [Google Scholar]