Abstract
Recombinant Sindbis viruses were engineered to express alternative forms of the protective antigen (PA) of Bacillus anthracis. The recombinant viruses induced PA-specific immunoglobulin G and neutralizing antibodies in Swiss Webster mice. Vaccination with the recombinant viruses induced immunity that offered some protection from a lethal Ames strain spore challenge and synergized the protective effects of ciprofloxacin.
Bacillus anthracis is a gram-positive, spore-forming bacterium that is the causative agent of anthrax. The intentional dissemination of anthrax spores through the United States mail in 2001 heightened concerns about the use of anthrax as a bioweapon (3) and stimulated efforts to develop improved vaccines and therapeutic agents to effectively prevent and treat anthrax disease (7, 14). Protection against anthrax disease correlates with the induction of neutralizing antibodies to protective antigen (PA) (8, 9). PA mediates cell binding through specific interactions with one of two known host cellular receptors (2, 16) and facilitates toxin translocation across the plasma membrane (6, 12).
PA domain 4 (PAd4) contains neutralizing epitopes, and experimental vaccines based on PAd4 have offered protection against lethal anthrax disease (4). Here, we describe the construction of two PAd4-expressing Sindbis viruses and their evaluation as anthrax vaccines. The first virus, designated E2S1-26S/PA, expressed PAd4 from a duplicated 26S promoter. The second virus, designated E2S1-PA/2A, expressed PAd4 fused to the 2A protease of foot-and-mouth disease virus. In this virus, the PAd4/2A coding sequences were placed in frame between those of the capsid and E3. During replication, the PAd4/2A fusion protein is expressed as a component of the viral structural polyprotein and then resolved by autoproteolytic cleavage mediated by capsid protein (upstream) and 2A (downstream). Each virus expressed a PAd4-containing protein which was of the predicted size and reacted with a PA-specific polyclonal rabbit antiserum in Western immunoblot assays (data not shown).
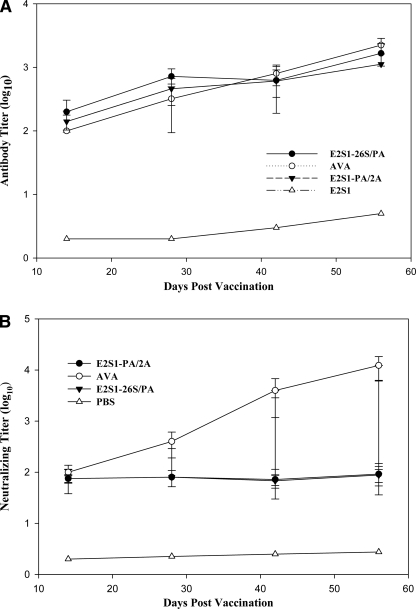
The parental virus (E2S1) and each recombinant virus were administered to adult Swiss Webster mice via intramuscular (i.m.) injection of 107 PFU. Mice were boosted similarly at days 14, 28, and 42. As a positive control, a group of mice was vaccinated and boosted similarly with 20 μl of anthrax vaccine adsorbed (AVA), a dose previously shown to protect mice against a lethal Sterne strain spore challenge (15, 19). Serum samples were collected prior to vaccination and 14 days following each injection. Serum was assayed for PA-specific antibodies by enzyme-linked immunosorbent assay (14). PA-specific antibodies were absent from all prevaccine sera (data not shown). Mice vaccinated with AVA or either recombinant virus produced similar levels of PA-specific immunoglobulin G (IgG) following the initial vaccination and subsequent boosts (Fig. 1A). The levels of neutralizing antibody differed markedly between the groups. Although mice vaccinated with AVA or a recombinant virus produced similar neutralizing antibody titers following the primary vaccination, only AVA-vaccinated mice displayed increased titers following booster injections (Fig. 1B). This result could be due to the fact that AVA-vaccinated mice were exposed to a far greater level of PA antigen than mice vaccinated with the recombinant viruses. The quantity of AVA administered to the mice in this study, scaled on a mass-to-weight ratio, was approximately 60 times the normal human dose. This dosage was used because AVA is not protective for mice when administered at quantities scaled to a single human dose (11), and it was previously determined to be the minimal amount necessary to ensure complete or nearly complete survival following exposure to 10 times the 50% lethal dose (10 LD50) of Ames strain spores (J. M. Thomas and J. W. Peterson, unpublished data). Alternatively, the inability of the virus-based vaccines to boost levels of neutralizing antibody may be due to neutralization of the vaccine by virus-specific antibodies produced following the primary vaccination. The limited ability of the recombinant viruses to induce neutralizing antibodies was unexpected, since another PAd4-based vaccine induced high levels of neutralizing titers in A/J mice (11). However, the immunogenic properties of PA vary markedly in different mouse strains, and Swiss Webster mice are known to respond poorly to PAd4 and to produce low levels of PAd4-specific neutralizing antibodies compared to the levels seen in other mouse strains (1). Swiss Webster mice were used in this project because they are highly sensitive to lethal toxin (LT) and, therefore, represent the most stringent mouse model for evaluating anthrax vaccine efficacy (5, 13). It is unlikely that the fusion of PAd4 to the 2A protein altered neutralizing epitopes on PAd4, because 2A did not measurably affect the antigenicity of other proteins (17, 18) and the titers of neutralizing antibodies elicited by E2S1-26S/PAd4 were not higher than those induced by E2S1-PAd4/2A.
FIG. 1.
(A) Swiss Webster mice infected with recombinant virus produce PA-specific IgG. Adult female mice (n = 10) were injected i.m. with 107 PFU of either E2S1-26S/PA or E2S1-PA/2A four times over a 56-day period. Additional groups were dosed concurrently with AVA and E2S1. Serum was collected at regular intervals and assayed for PA-specific IgG by enzyme-linked immunosorbent assay. (B) Infection of mice with recombinant virus elicits LT-neutralizing antibodies. Adult Swiss Webster mice (n = 10) were injected i.m. with 107 PFU of either E2S1-26S/PA or E2S1-PA/2A four times over a 56-day period. Additional groups were concurrently dosed with AVA. Serum was collected at regular intervals and assayed using an anthrax LT neutralization assay. Error bars show standard deviations.
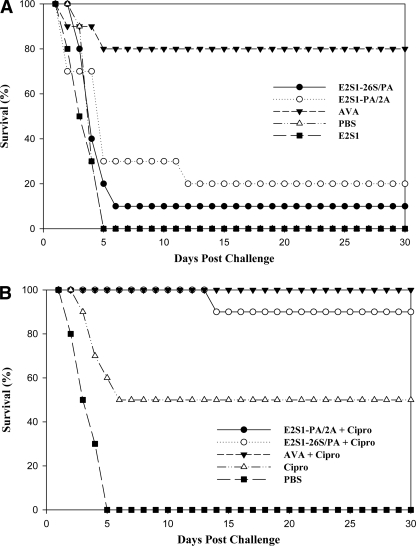
To assess vaccine efficacy, each group of mice was challenged intranasally (i.n.) with 10 LD50 of Ames anthrax spores and monitored for 30 days (14). Control groups included mice infected with the parental virus and mice injected with phosphate-buffered saline (PBS). Additional groups of mice were vaccinated with AVA or with a recombinant virus and challenged similarly. These mice received 30 mg/kg of body weight/day of ciprofloxacin for a period of 7 days postchallenge. These groups of mice were included in the challenge study based on a report that acquired immunity to anthrax could enhance the protective effects of ciprofloxacin, the antibiotic most commonly used to treat anthrax disease (14). Mice that received PBS or E2S1 were not protected from virulent spore challenge, and all succumbed to infection by day 5 (Fig. 2A). Survival among AVA-vaccinated mice was 80%, while 20% of mice vaccinated with E2S1-PA/2A and 10% of animals vaccinated with E2S1-26S/PA survived the spore challenge (Fig. 2A). For these groups of mice, the level of protection generally correlated with the level of neutralizing antibody, as vaccination with AVA provided significantly greater protection than either recombinant virus (P < 0.05, Fisher's exact test). Although AVA vaccination offered significantly better protection than vaccination with either recombinant virus, all three vaccines were capable of enhancing the protective effects of ciprofloxacin. The survival rate among PBS-treated control mice receiving ciprofloxacin was 50%. Survival improved to 100% when ciprofloxacin was administered to AVA- or E2S1-PA/2A-vaccinated mice and to 90% when it was administered to mice vaccinated with E2S1-26S/PA (Fig. 2B).
FIG. 2.
(A) Mice immunized with recombinant virus are protected from virulent spore challenge. Vaccinated animals were challenged by i.n. administration of 10 LD50 of Ames spores and monitored for survival. (B) Vaccination with AVA and PAd4-expressing Sindbis viruses enhances the protective effects of ciprofloxacin (Cipro). Vaccinated animals were challenged by i.n. administration of 10 LD50 of Ames spores and monitored for survival. Ciprofloxacin (30 mg/kg twice a day) was administered daily from day 1 to day 7.
Anthrax vaccines based on recombinant alphaviruses have been described previously. A vaccine based on PA-expressing Venezuelan equine encephalitis virus (VEEV) replicons was shown to offer better protection than the recombinant Sindbis viruses used in this study (10). However, there are several significant differences between these two studies. First, the study based on VEEV replicons only showed protection of A/J and C57BL/6 mice instead of the highly susceptible Swiss Webster mouse. In addition, mice in the VEEV replicon study were challenged by the subcutaneous route, and challenges were performed using the Sterne strain of B. anthracis. That strain lacks the plasmid that encodes the anti-phagocytic capsule, which functions as the major determinant of anthrax virulence. In contrast, this study used the highly sensitive Swiss Webster mouse. These mice were challenged by i.n. administration of highly virulent, capsule-producing Ames spores. Therefore, we feel that our system was more stringent and more closely models a real-world scenario in which a vaccine would need to protect against aerosolized spores from a toxin- and capsule-producing strain of B. anthracis.
Despite the low level of protection provided by the Sindbis virus-based vaccines, each markedly enhanced the protective effects of ciprofloxacin. The basis for enhanced survival of mice exposed to AVA/PAd4 and ciprofloxacin was not addressed directly in this study. However, the enhanced protection may be due to the ability of ciprofloxacin to maintain initial levels of bacterial growth below a threshold where the modest levels of neutralizing antibody maintain effectiveness. In the absence of ciprofloxacin treatment, bacterial growth may overwhelm the limited immunity induced by the vaccines, leading to the rapid death of infected animals. This study demonstrates that an anthrax vaccine that induces humoral immunity but fails to afford a high level of protection by itself can still provide benefit by markedly enhancing the effectiveness of the antibiotic most commonly used to treat anthrax disease.
Acknowledgments
This work was supported by a grant from the National Institute of Allergy and Infectious Disease (1N01AI30065).
Footnotes
Published ahead of print on 16 September 2009.
REFERENCES
- 1.Abboud, N., and A. Casadevall. 2008. Immunogenicity of Bacillus anthracis protective antigen domains and efficacy of elicited antibody responses depend on host genetic background. Clin. Vaccine Immunol. 15:1115-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bradley, K. A., J. Mogridge, M. Mourez, R. J. Collier, and J. A. Young. 2001. Identification of the cellular receptor for anthrax toxin. Nature 414:225-229. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control. 2001. Update: investigation of bioterrorism-related anthrax and interim guidelines for exposure management and antimicrobial therapy, October 2001. Morb. Mortal. Wkly. Rep. 50:909-919. [PubMed] [Google Scholar]
- 4.Flick-Smith, H. C., N. J. Walker, P. Gibson, H. Bullifent, S. Hayward, J. Miller, R. W. Titball, and E. D. Williamson. 2002. A recombinant carboxy-terminal domain of the protective antigen of Bacillus anthracis protects mice against anthrax infection. Infect. Immun. 70:1653-1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friedlander, A. M., R. Bhatnagar, S. H. Leppla, L. Johnson, and Y. Singh. 1993. Characterization of macrophage sensitivity and resistance to anthrax lethal toxin. Infect. Immun. 61:245-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gordon, V. M., S. H. Leppla, and E. L. Hewlett. 1988. Inhibitors of receptor-mediated endocytosis block the entry of Bacillus anthracis adenylate cyclase toxin but not that of Bordetella pertussis adenylate cyclase toxin. Infect. Immun. 56:1066-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heine, H. S., J. Bassett, L. Miller, A. Bassett, B. E. Ivins, D. Lehoux, F. F. Arhin, T. R. Parr, Jr., and G. Moeck. 2008. Efficacy of oritavancin in a murine model of Bacillus anthracis spore inhalation anthrax. Antimicrob. Agents Chemother. 52:3350-3357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hewetson, J. F., S. F. Little, B. E. Ivins, W. M. Johnson, P. R. Pittman, J. E. Brown, S. L. Norris, and C. J. Nielsen. 2008. An in vivo passive protection assay for the evaluation of immunity in AVA-vaccinated individuals. Vaccine 26:4262-4266. [DOI] [PubMed] [Google Scholar]
- 9.Klinman, D. M., H. Xie, and B. E. Ivins. 2006. CpG oligonucleotides improve the protective immune response induced by the licensed anthrax vaccine. Ann. N. Y. Acad. Sci. 1082:137-150. [DOI] [PubMed] [Google Scholar]
- 10.Lee, J. S., A. G. Hadjipanayis, and S. L. Welkos. 2003. Venezuelan equine encephalitis virus-vectored vaccines protect mice against anthrax spore challenge. Infect. Immun. 71:1491-1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McConnell, M. J., P. C. Hanna, and M. J. Imperiale. 2006. Cytokine response and survival of mice immunized with an adenovirus expressing Bacillus anthracis protective antigen domain 4. Infect. Immun. 74:1009-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Milne, J. C., and R. J. Collier. 1993. pH-dependent permeabilization of the plasma membrane of mammalian cells by anthrax protective antigen. Mol. Microbiol. 10:647-653. [DOI] [PubMed] [Google Scholar]
- 13.Muehlbauer, S. M., T. H. Evering, G. Bonuccelli, R. C. Squires, A. W. Ashton, S. A. Porcelli, M. P. Lisanti, and J. Brojatsch. 2007. Anthrax lethal toxin kills macrophages in a strain-specific manner by apoptosis or caspase-1-mediated necrosis. Cell Cycle 6:758-766. [DOI] [PubMed] [Google Scholar]
- 14.Peterson, J. W., J. E. Comer, D. M. Noffsinger, A. Wenglikowski, K. G. Walberg, B. M. Chatuev, A. K. Chopra, L. R. Stanberry, A. S. Kang, W. W. Scholz, and J. Sircar. 2006. Human monoclonal anti-protective antigen antibody completely protects rabbits and is synergistic with ciprofloxacin in protecting mice and guinea pigs against inhalation anthrax. Infect. Immun. 74:1016-1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pitt, M. L., S. Little, B. E. Ivins, P. Fellows, J. Boles, J. Barth, J. Hewetson, and A. M. Friedlander. 1999. In vitro correlate of immunity in an animal model of inhalational anthrax. J. Appl. Microbiol. 87:304. [DOI] [PubMed] [Google Scholar]
- 16.Scobie, H. M., G. J. Rainey, K. A. Bradley, and J. A. Young. 2003. Human capillary morphogenesis protein 2 functions as an anthrax toxin receptor. Proc. Natl. Acad. Sci. USA 100:5170-5174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas, J. M., W. B. Klimstra, K. D. Ryman, and H. W. Heidner. 2003. Sindbis virus vectors designed to express a foreign protein as a cleavable component of the viral structural polyprotein. J. Virol. 77:5598-5606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang, S., Q. Yao, J. Tao, Y. Qiao, and Z. Zhang. 2007. Co-ordinate expression of glycine betaine synthesis genes linked by the FMDV 2A region in a single open reading frame in Pichia pastoris. Appl. Microbiol. Biotechnol. 77:891-899. [DOI] [PubMed] [Google Scholar]
- 19.Xie, H., I. Gursel, B. E. Ivins, M. Singh, D. T. O'Hagan, J. B. Ulmer, and D. M. Klinman. 2005. CpG oligodeoxynucleotides adsorbed onto polylactide-co-glycolide microparticles improve the immunogenicity and protective activity of the licensed anthrax vaccine. Infect. Immun. 73:828-833. [DOI] [PMC free article] [PubMed] [Google Scholar]