Abstract
The Bactec MGIT 960 system for testing susceptibility to second-line drugs was evaluated with 117 clinical strains in a multicenter study. The four drugs studied were levofloxacin, amikacin, capreomycin, and ethionamide. The critical concentration established for levofloxacin and amikacin was 1.5 μg/ml, that established for capreomycin was 3.0 μg/ml, and that established for ethionamide was 5.0 μg/ml. The overall level of agreement between the agar proportion method and the MGIT 960 system was 96.4%, and the levels of agreement for the individuals drugs were 99.1% for levofloxacin, 100% for amikacin, 97.4% for capreomycin, and 88.9% for ethionamide. The rate of reproducibility of the drug susceptibility testing results between the participating laboratories was 99.5%.
The increase in the incidence of multidrug-resistant tuberculosis (MDR TB) and the emergence of extensively drug-resistant tuberculosis present tremendous challenges to the global efforts to combat tuberculosis (1, 5, 16, 21). Rapid methods enabling accurate susceptibility testing of first-line and second-line drugs are critical for the early diagnosis of MDR TB and extensively drug-resistant tuberculosis and the initiation of effective regimens. Various drug susceptibility testing (DST) methods that use solid media, including the agar proportion method (AP) and other methods, have the drawback of prolonged turnaround times (TATs). The World Health Organization and the U.S. Centers for Disease Control and Prevention have recommended the use of liquid culture systems for the diagnosis of tuberculosis and DST to improve TATs (22, 25). The Bactec 460 (Becton Dickinson Diagnostic Systems, Sparks, MD), a radiometric liquid system, provided an excellent alternative for testing of the susceptibilities of Mycobacterium tuberculosis complex (MTBC) isolates to streptomycin, isoniazid, rifampin (rifampicin), and ethambutol (SIRE) and to pyrazinamide (PZA) with improved TATs. The MGIT 960 liquid, nonradiometric SIRE DST (Becton Dickinson Diagnostic Systems), whose performance is comparable to that of the Bactec 460 system, has been commercially available since April 2002 (4, 20, 23). The Microbial Diseases Laboratory (MDL) of the California Department of Public Health implemented SIRE DST with the MGIT 960 system in 2004. With confidence in the SIRE DST with the MGIT 960 system, a study that used the same platform to test the susceptibilities of MTBC isolates to four classes of second-line drugs, levofloxacin (LVX), amikacin (AMK), capreomycin (CAP), and ethionamide (ETH), was initiated in November 2004. The study was conducted at two laboratories: MDL and the TB Reference Laboratory of the Veteran Affairs Medical Center (VA) in West Haven, CT. Here we report the results of the multicenter study, in which the critical concentrations of the test drugs were established, the performance of the MGIT 960 system was compared to that of AP, and the interlaboratory reproducibility of the method was evaluated.
(Part of this work was presented at the 46th Interscience Conference on Antimicrobial Agents and Chemotherapy, 2006, San Francisco, CA.)
MATERIALS AND METHODS
Study design.
This study consisted of five phases: phase I, determination of the MIC of each drug for the susceptible control strain, Mycobacterium tuberculosis H37Rv (ATCC 27294); phase II, determination of the critical concentration of each drug; phase III, testing of clinical strains at the critical concentration of each drug determined in phase II; phase IV, study of interlaboratory reproducibility; and phase V, study of the reproducibility of the medium and reagents.
Strains.
A total of 117 clinical strains of MTBC, including 49 pansusceptible strains and 68 resistant strains whose drug susceptibility results were previously determined by AP, were tested. MDL contributed 89 strains (42 susceptible and 47 resistant strains), and VA contributed 28 strains (7 susceptible and 21 resistant strains). At MDL, the pansusceptible strains were randomly chosen from cultures in which MTBC was isolated between 2003 and 2006. As for the resistant strains, we included as many strains from our archived collections as we could find, excluding those found to be nonviable or contaminated. Strains from VA were selected from cultures in which MTBC was isolated between 2002 and 2003 to include as many resistant strains as possible, and susceptible strains from the same period were randomly chosen.
Antimicrobial agents.
AMK, CAP, and ETH were purchased from Sigma-Aldrich Corporation (St. Louis, MO); and LVX was provided by Johnson & Johnson Pharmaceutical Research & Development, L.L.C. (Spring House, PA). Each laboratory prepared drug solutions according to the protocol described below. The stock solutions of AMK (120 μg/ml), CAP (75 μg/ml), and LVX (120 μg/ml) were prepared in sterile water. All drug concentrations, including the concentrations in the stock solutions, the MICs, and the critical concentrations, are expressed as the final concentrations used in tests with the MGIT 960 system. These stock solutions were filtered through 0.22-μm-pore-size Millex-GS filter units (Millipore, Bedford, MA) and were stored at −20°C. The working solutions of AMK, CAP, and LVX were diluted from the stock solution, aliquoted, and frozen for future use. The stock solution of ETH (120 μg/ml) was prepared in ethylene glycol (Spectrum Quality Products, Inc., Gardena, CA) and was incubated at 37°C overnight. It was then filtered through 0.22 μm-pore-size Millex-GS filter units, aliquoted, and stored at −20°C. The working solution was made fresh from the stock solution in sterile water for each test run. (After this study was completed, some aliquots of the ETH stock solution were found to contain ETH precipitates. Those precipitates did not readily dissolve at room temperature. Storage of the ETH stock solutions at 2 to 8°C and periodic testing of the MIC of ETH for the control strain is recommended. Our experience indicated that the MIC of ETH for the H37Rv control strain remained unchanged over a 2-year period.)
Preinoculation preparation.
The LVX, AMK, CAP, and ETH drug panel consisted of five MGIT tubes: one tube for the growth control and four tubes for the drugs (one for each drug). Preinoculation preparation included addition of 0.8 ml SIRE supplement to each MGIT tube and addition of 0.1 ml drug working solution to each designated MGIT 960 system tube. No drug was added to the growth control tube. The SIRE supplement containing oleic acid, albumin, dextrose, and catalase (OADC) is one of the components of the SIRE drug kit (Becton Dickinson Diagnostic Systems). The Middlebrook OADC enrichment from BBL (Becton Dickinson Diagnostic Systems) is an alternative to the SIRE supplement. According to Becton Dickinson Diagnostic Systems (personal communication), the two products are identical.
Inoculum preparation.
Inocula were prepared from cultures of all 117 strains grown in Lowenstein Jensen (LJ) slants. The cultures were 2 to 5 weeks old. The manufacturer's protocol for the preparation of inocula from solid media for use in the SIRE DST was followed, with one exception: sterile normal saline instead of Middlebrook 7H9 broth or MGIT broth was used to prepare the cell suspensions and to adjust the turbidity of the suspension to a 0.5 McFarland standard. In addition, the procedure was further validated for the testing of positive MGIT tubes. A subset of 23 strains was subcultured to MGIT tubes and tested after growth was detected by the MGIT 960 system. The inoculum prepared from MGIT tubes was also standardized to a 0.5 McFarland standard. Briefly, the growth at the bottom of a positive MGIT tube was transferred to a sterile tube containing 2 ml sterile normal saline and the components were gently mixed. Clumps were allowed to settle. The supernatant containing the homogeneous cell suspension was transferred to another sterile tube, and its turbidity was adjusted to a 0.5 McFarland standard. After the cell suspension was standardized, it was diluted 1:5 with sterile normal saline for inoculation into drug-containing MGIT tubes. The 1:5 cell suspension was further diluted 100-fold with sterile normal saline for inoculation of the growth control tube. The volume of each inoculum was 0.5 ml.
Determination of the MIC of each drug for H37Rv.
On the basis of our experiences with the Bactec 460 system, three concentrations of each drug were chosen for testing. These were 0.25, 0.5, and 1.0 μg/ml for AMK, LVX, and ETH and 0.5, 1, and 1.5 μg/ml for CAP. Three experiments were performed at each laboratory, and the results obtained from the two laboratories were compared. This was designed to confirm that the drug concentrations prepared at each laboratory were accurate and that the test procedures were properly followed. This was a critical step in the establishment of a sound basis for a multicenter study.
Determination of critical concentration for each drug.
Determination of the critical concentration for each drug was done at MDL. A subset of 29 strains from the 117-strain pool, including 8 pansusceptible strains and 21 resistant strains with various drug susceptibility profiles (15 strains resistant to AMK and CAP, 13 resistant to ETH, and 10 resistant to LVX), were studied. An additional four quinolone-resistant strains with known gyrA mutations, obtained from B. Kreiswirth at the Public Health Research Institute Tuberculosis Center (Newark, NJ), were tested only for their susceptibilities to LVX. By testing both susceptible and resistant strains, this phase was designed to determine the critical concentration for each drug that could best distinguish the susceptible group from the resistant group. Three concentrations were tested for each drug. AMK and LVX were tested at 1, 1.5, and 2 μg/ml; CAP was tested at 2, 3, and 4 μg/ml; and ETH was tested at 3, 4, and 5 μg/ml.
Testing of additional clinical strains at the critical concentration of each drug.
After determination of the critical concentrations, an additional 88 clinical strains (41 susceptible and 47 resistant strains) were tested to further establish that the critical concentrations would correctly discriminate susceptible and resistant strains on a larger scale. MDL tested 60 strains, and VA tested 28 strains.
Study for reproducibility between laboratories.
A total of 48 strains from the study pool (28 strains submitted by VA to MDL and 20 strains submitted by MDL to VA) were tested at the critical concentrations at both laboratories. Of the 48 strains, 17 were pansusceptible strains and 31 were resistant strains with various drug susceptibility profiles. Two sets of 192 data points were compared to determine the reproducibility between the two laboratories.
Study of reagent lot-to-lot reproducibility.
A subset of six strains from the study pool (three susceptible strains and three resistant strains) were tested at the critical concentrations with three lots of MGIT medium and three lots of SIRE supplement in three different test runs at MDL. Cell suspensions were prepared fresh for each test run. Three sets of 24 data points were analyzed to determine the reagent reproducibility.
QC.
A strain of Mycobacterium tuberculosis, H37Rv (ATCC 27294), was used as a quality control (QC) strain and was tested with each batch of DST at the critical concentration of each drug. This QC strain is pansusceptible to the four drugs tested in the present study. If the QC strain did not yield the expected results, the test with that batch had to be repeated.
Reference methods and discrepancy resolution.
AP was the primary reference method for this study. All strains were previously tested by AP with AMK at 2 μg/ml (strains from VA were tested at 6 μg/ml), CAP at 10 μg/ml, ETH at 5 μg/ml, and OFX at 2 μg/ml. LVX is the l form of OFX. In addition to using the results obtained by AP with OFX as a reference, we also tested LVX at 2 μg/ml with the Bactec 460 system (19). For the resolution of discrepancies, DST was repeated at VA by AP and at MDL with the MGIT 960 and Bactec 460 systems. In tests with the Bactec 460 system, the test concentrations were 1 μg/ml for AMK, 1.25 μg/ml for CAP, 2.5 μg/ml for ETH, and 2 μg/ml for LVX.
RESULTS
Interpretation of results.
The MGIT 960 system supports the testing of various combinations of SIRE and PZA panels configured by the manufacturer, but second-line drug panels are not available. Testing of second-line drugs must be registered in the MGIT 960 system as one of the SIRE panels, and the user manually enters the drug identification on the printout of the results. The MGIT 960 system flags the completion of a DST when the growth unit (GU) of the growth control reaches 400 and reports S for susceptible or R for resistant, as well as a GU value for each drug-containing MGIT tube on the printout. An isolate is interpreted to be susceptible when the GU of a drug-containing MGIT tube is equal to or less than 100 or as resistant when the GU is greater than 100. If an isolate was interpreted to be resistant, a smear was made and stained to prove the presence of acid-fast bacilli (AFB) with morphology compatible with that of MTBC and the absence of contaminants.
MIC of each drug for H37Rv (ATCC 27294).
The results obtained at both participating laboratories demonstrated 100% reproducibility in the three runs performed at each laboratory. The MIC results for AMK, LVX, and ETH obtained at VA and MDL were the same (0.5 μg/ml for the three drugs), but the MIC of CAP was slightly lower at VA (1.0 μg/ml at VA and 1.5 μg/ml at MDL). To resolve this discrepancy, CAP was tested with an additional concentration of 1.25 μg/ml at MDL, and the MIC of CAP was determined to be 1.25 μg/ml three of three times. Thus, the difference in the MIC for CAP at MDL and VA was minimal and acceptable.
Critical concentration of each drug.
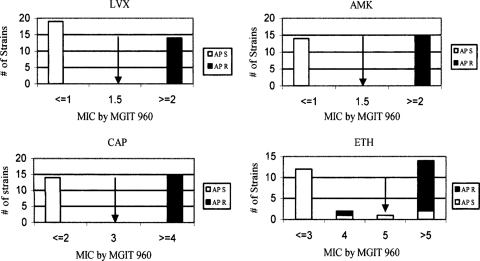
The critical concentration of each drug established by this study is shown in Fig. 1. To yield the best discrimination between susceptible and resistant strains, the critical concentrations were determined to be 1.5 μg/ml for AMK and LVX, 3.0 μg/ml for CAP, and 5.0 μg/ml for ETH. Determination of the critical concentrations for AMK, LVX, and CAP was straightforward, since we were able to decide on a concentration at which 100% of the resistant strains grew in the presence of the drug and 100% of the susceptible strains were inhibited. For ETH, the critical concentration was set at 5.0 μg/ml to yield the best discrimination between susceptible and resistant strains, yet 3 strains with discordant results were found among the 29 strains tested, which yielded a 90% (26/29) correlation between the results obtained with the MGIT 960 system and by AP. Twelve of 13 (92.3%) resistant strains yielded resistant results, and 14 of 16 (87.5%) susceptible strains yielded susceptible results. Among the three discrepancies, one strain, which tested resistant by AP but susceptible by MGIT 960, had a MIC of 4.0 μg/ml by MGIT 960, and two strains, which tested susceptible by AP but resistant by MGIT 960, had MICs greater than 5.0 μg/ml (the MIC for one strain was 8.0 μg/ml and the MIC for the other one was greater than 10 μg/ml) by MGIT 960.
FIG. 1.
MIC of each drug determined by use of the MGIT 960 system with strains that tested susceptible (S) or resistant (R) by AP.
Overall agreement.
The overall agreement between the results obtained with MGIT 960 and by AP was 96.4% (451/468), and a comparison of the results between the two methods after discrepancy resolution is shown in Table 1. For AMK, there was 100% agreement. For CAP and LVX, a total of four discrepancies were detected, but the results obtained with Bactec 460 were in concordance with those obtained with the MGIT 960 system. For ETH, there were 13 discrepancies. Two strains (designated group A) tested resistant by AP but susceptible by MGIT 960, and 11 strains (designated group B) tested susceptible by AP but resistant by MGIT 960. Both strains in group A demonstrated pinpoint colonies on the ETH-containing quadrant on Middlebrook 7H10 plates by AP. It indicated some degree of inhibition by the drug, although the test result was interpreted to be resistant. One of these two strains tested susceptible by Bactec 460; the other strain tested equivocal (in one test it was susceptible and in the other test it was resistant and had a low increase in the growth index). Ten of the 11 strains in group B tested resistant and 1 tested susceptible by Bactec 460. The overall rate of agreement was 88.9% (104/117) between AP and MGIT 960; however, the results for 11 of the 13 strains with discrepancies were in concordance between the Bactec 460 and MGIT 960 systems.
TABLE 1.
Comparison of results obtained by use of MGIT 960 and APa
| Drug | No. of strains with indicated results by AP/MGIT 960b |
Overall agreementc | |||
|---|---|---|---|---|---|
| Agreement |
Discrepancy |
||||
| R/R | S/S | R/S | S/R | ||
| LVX | 28 | 88 | 0 | 1d | 99.1 (116/117) |
| AMK | 37 | 80 | 0 | 0 | 100 (117/117) |
| CAP | 35 | 79 | 0 | 3d | 97.4 (114/117) |
| ETH | 43 | 61 | 2e | 11f | 88.9 (104/117)g |
A total of 117 strains were tested.
R, resistant; S, susceptible.
The data represent percent agreement (number of strains with the correct result/total number of strains tested).
Tested resistant with the Bactec 460 system.
One of two strains tested susceptible with the Bactec 460 system.
Ten of 11 strains tested resistant with the Bactec 460 system.
The results obtained with the MGIT 960 and Bactec 460 systems were concordant for 11 of 13 discrepancies.
Interlaboratory reproducibility.
A subset of 48 strains from the study pool was tested at both laboratories. The interlaboratory reproducibility study was analyzed on the basis of the results of first-shot testing at each laboratory. One discrepancy was found between the two sets of 192 test results, which yielded an overall reproducibility of 99.5% (191/192) (Table 2). No discrepancies were found for LVX, AMK, and ETH, which yielded 100% reproducibility for each of the three drugs. The only discrepancy occurred with CAP. The particular strain with the discrepancy tested susceptible at VA but resistant at MDL and had a GU of 177. Upon retesting at MDL, this strain tested susceptible and had a GU of 6, but substantial growth in the MGIT tube was observed, which indicated the presence of resistant populations.
TABLE 2.
Results of interlaboratory reproducibilitya
| Result at VA | No. of strains with indicated result for drug at MDLb |
|||||||
|---|---|---|---|---|---|---|---|---|
| LVX |
AMK |
CAP |
ETH |
|||||
| S | R | S | R | S | R | S | R | |
| S | 33 | 0 | 29 | 0 | 29 | 1 | 25 | 0 |
| R | 0 | 15 | 0 | 19 | 0 | 18 | 0 | 23 |
S, susceptible; R, resistant.
The overall agreement was 99.5% (191/192 strains); and the levels of agreement for the individuals drugs were 100% (48/48 strains) for LVX, 100% (48/48 strains) for AMK, 98% (47/48 strains) for CAP, and 100% (48/48 strains) for ETH.
Reproducibility of reagents.
Three lots of MGIT medium and three lots of SIRE supplement were tested with three susceptible strains and three resistant strains. A total of 72 data points were generated, and 100% reproducibility was realized. The duration for the completion of a DST in the MGIT 960 system is called “time in protocol” (TIP) by the manufacturer. The average TIPs for the three sets of tests were 8 days and 9.2 h, 8 days and 15.4 h, and 8 days and 8.3 h. The MGIT 960 system demonstrated excellent reproducibility with different lots of MGIT medium and growth supplement.
Inoculum source: growth from LJ slants versus that from MGIT medium.
Inocula were prepared from 23 seeded MGIT tubes (which included 8 pansusceptible strains and 15 resistant strains with various drug susceptibility profiles), and the results were compared with those prepared from the LJ slants. There was a 100% reproducibility in the results between the inocula prepared from MGIT tubes and LJ slants. The reproducibility was excellent, which may be due to the use of homogeneous cell suspensions and standardization of the inocula, regardless of the source of growth.
DISCUSSION
Use of the Bactec 460 system to test for susceptibility to the primary drugs SIRE and PZA has been cleared by the U.S. Food and Drug Administration (FDA). It has been standardized and widely used, and its performance has been considered a reference standard. Although use of the Bactec 460 system for DST of second-line drugs has been studied and used by some laboratories (15), FDA has not approved it for use with those drugs. Many laboratories still use AP to perform testing for susceptibility to second-line drugs. Therefore, we used AP as the primary reference method for validation of the DST with second-line drugs with the MGIT 960 system.
The basis for this study was, first, the establishment of comparable MICs of each drug for the control strain, H37Rv (ATCC 27294), at both laboratories. The MIC study, which demonstrated excellent interlaboratory agreement, provided a sound basis and confidence for the remainder of the study. Second, in the process of determining the critical concentration for each drug, we did not take the traditional twofold dilution approach, which was used in two previous studies (9, 18). Instead, we tested additional drug concentrations within twofold dilutions. This fine-tuning approach enabled us to select a drug concentration that could better discriminate susceptible and resistant strains.
The overall levels of agreement between the results obtained by AP and with MGIT 960 were excellent for AMK, CAP, and LVX, which were 100%, 97.4%, and 99.1%, respectively. However, the agreement for ETH was only 88.9%. This level of correlation between the results obtained by use of MGIT 960 and AP for ETH was also demonstrated in a study conducted by Martin et al. (12). The results obtained for ETH revealed a problematic aspect of the DST with ETH. In our opinion, to validate a new method, when the correlation between the new method and the reference method is greater than 95%, it provides a relatively high degree of confidence in the applicability of the new method. However, we were unable to find a critical concentration that could yield greater than 95% discrimination between susceptible strains and resistant strains when AP was used as the “gold standard” for DST with ETH. Lefford and Mitchison (10) conducted a study and found that the MIC distributions of ETH between probable susceptible strains (specimens obtained from patients before treatment) and probable resistant strains (specimens obtained after treatment with ETH) were not well separated. In the process of resolving the discrepancies for ETH, we tested the MICs for the 11 strains which tested resistant by MGIT 960 but susceptible by AP. We found that 7 of the 11 strains had MICs greater than 10 μg/ml, 3 strains had MICs of 10 μg/ml, and 1 strain had an MIC of 8 μg/ml. These MICs were much higher than the critical concentration (5 μg/ml) established in this study, and we inferred that the discrepancies were unlikely to be resolved by choosing a higher drug concentration as the critical concentration. To prove this, we retested all ETH-resistant strains at 6, 8, and 10 μg/ml, and we found that 6 of the 43 resistant strains became susceptible at 6 μg/ml and that 15 strains became susceptible at 10 μg/ml. Thus, none of the higher concentrations would generate a better correlation. Furthermore, we also used the Bactec 460 system to evaluate the strains with discrepancies, and we found that the results between the MGIT 960 and Bactec 460 systems were in concordance for 11 of 13 strains. The better correlation between the MGIT 960 and the Bactec 460 systems shown in our study was also demonstrated in studies conducted by Rodrigues et al. (17) and Rusch-Gerdes et al. (18). These results may indicate that the causes of the discrepancies for ETH were perhaps attributable more to methodology differences than to the selection of the critical concentration.
The overall reproducibility studied in phase IV was excellent. We found only one discrepant result with CAP. For the particular strain with that result, MDL not only could not reproduce the result from VA but also could not reproduce its own result when the strain was retested. Poor reproducibility may be expected when a strain has an MIC that is at or very close to the critical concentration (8, 24). As shown in this study, this strain initially tested resistant at MDL and had a GU of 177, but it was susceptible on retesting and had a GU of 6. The cutoff for resistance is a GU of 100. The first result was interpreted to be resistant, and the second result was interpreted to be susceptible. How to interpret such results presents a challenge. Although the majority of drug tests had GU values of 0 for susceptibility and 400 for resistance, 2.7% (13/468) of the tests in this study yielded GU values between 1 and 399. It may be advisable to designate a borderline category for the interpretation of results that fall in this range. We believe that it is more reliable to report a borderline result as “borderline” than “susceptible” or “resistant” by chance. However, establishment of the precise definition of “borderline” is beyond the scope of this study.
The MGIT 960 system DST report contains a TIP with two figures (days and hours) for each DST panel tested. The average TIP was 8 days and 6 h at MDL and 9 days and 8 h at VA. We were not aware of the TIP difference when the MIC study was conducted in phase I. Although it did not seem to affect the results, it would have been better if the TIP issue had been addressed at the beginning of the study. An ideal DST protocol would be one that can generate accurate results with the shortest TIP. This study used a 1:5 dilution of the cell suspension equivalent to a 0.5 McFarland standard as an inoculum. A future study is required to find the optimal cell concentration, which could shorten the average TIP yet still produce accurate results.
As a routine practice, only primary drugs are tested initially. When strains test resistant to rifampin or any two of the primary drugs, second-line drugs are then tested. When resistance to primary drugs is detected, the growth on LJ slants is usually adequate for the testing of second-line drugs. In this study, we used the growth from LJ slants as the main source for the inoculum preparation. With advances in molecular technologies, isoniazid and/or rifampin resistance can be detected by rapid methods, such as those that use molecular beacons, line probes, or microchips (2, 3, 6, 7, 11, 13). Once rifampin resistance or MDR TB is detected, testing for susceptibility to second-line drugs should be performed along with testing for susceptibility to first-line drugs as early as possible, and testing should not wait for growth from LJ slants. Therefore, we included a subset of 23 specimens for validation of this assay using inocula prepared from positive MGIT tubes. Our protocol prepares inocula from MGIT tubes by standardization of the growth to a 0.5 McFarland standard, as is done for LJ slants. DST can be performed from a primary MGIT tube and not subject to the manufacturer's time schedule, as stated in the package insert for SIRE DST. This has two advantages: the inoculum does not contain coarse clumps, which helps to produce more consistent results, and it does not require seeding of a MGIT tube and waiting for its growth for DST, thus improving the TAT and reducing the cost for medium.
This study presents a DST protocol that uses a homogeneous, standardized cell suspension to prepare the inoculum regardless of the source of growth: solid or liquid medium. The verification data were good, and the reproducibilities for interlaboratory test results, different lots of reagents, and different sources of inocula were excellent. This study and previous studies (9, 17, 18), regardless of the reference methods used, provided data that may be used to demonstrate that DST with the MGIT 960 system is a reliable method for the testing of second-line drugs.
Acknowledgments
We thank Becton Dickinson for providing the MGIT tubes, SIRE supplements, and Bactec 12B vials and Johnson & Johnson Pharmaceutical Research & Development, L.L.C., for providing LVX. We also thank Beverly Metchock at CDC for assistance with performing DST by AP for several strains with discrepancies.
Footnotes
Published ahead of print on 9 September 2009.
REFERENCES
- 1.Banerjee, R., G. F. Schecter, J. Flood, and T. C. Porco. 2008. Extensively drug-resistant tuberculosis: new strains, new challenges. Exp. Rev. Anti-Infect. Ther. 6:713-724. [DOI] [PubMed] [Google Scholar]
- 2.Bang, D., A. Bengard Andersen, and V. O. Thomsen. 2006. Rapid genotypic detection of rifampin- and isoniazid-resistant Mycobacterium tuberculosis directly in clinical specimens. J. Clin. Microbiol. 44:2605-2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnard, M., H. Albert, G. Coetzee, R. O'Brien, and M. E. Bosman. 2008. Rapid molecular screening for multidrug-resistant tuberculosis in a high-volume public health laboratory in South Africa. Am. J. Respir. Crit. Care Med. 177:787-792. [DOI] [PubMed] [Google Scholar]
- 4.Bemer, P., F. Palicova, S. Rusch-Gerdes, H. B. Drugeon, and G. E. Pfyffer. 2002. Multicenter evaluation of fully automated BACTEC Mycobacteria Growth Indicator Tube 960 system for susceptibility testing of Mycobacterium tuberculosis. J. Clin. Microbiol. 40:150-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. 2006. Emergence of Mycobacterium tuberculosis with extensive resistance to second-line drugs—worldwide, 2000-2004. MMWR Morb. Mortal. Wkly. Rep. 55:301-305. [PubMed] [Google Scholar]
- 6.Hillemann, D., S. Rusch-Gerdes, and E. Richter. 2007. Evaluation of the GenoType MTBDRplus assay for rifampin and isoniazid susceptibility testing of Mycobacterium tuberculosis strains and clinical specimens. J. Clin. Microbiol. 45:2635-2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johansen, I. S., B. Lundgren, A. Sosnovskaja, and V. O. Thomsen. 2003. Direct detection of multidrug-resistant Mycobacterium tuberculosis in clinical specimens in low- and high-incidence countries by line probe assay. J. Clin. Microbiol. 41:4454-4456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim, S. J. 2005. Drug-susceptibility testing in tuberculosis: methods and reliability of results. Eur. Respir. J. 25:564-569. [DOI] [PubMed] [Google Scholar]
- 9.Kruuner, A., M. D. Yates, and F. A. Drobniewski. 2006. Evaluation of MGIT 960-based antimicrobial testing and determination of critical concentrations of first- and second-line antimicrobial drugs with drug-resistant clinical strains of Mycobacterium tuberculosis. J. Clin. Microbiol. 44:811-818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lefford, M. J., and D. A. Mitchison. 1966. Comparison of methods for testing the sensitivity of Mycobacterium tuberculosis to ethionamide. Tubercle (London) 47:250-262. [DOI] [PubMed] [Google Scholar]
- 11.Lin, S. Y. G., W. Probert, M. Lo, and E. Desmond. 2004. Rapid detection of isoniazid and rifampin resistance mutations in Mycobacterium tuberculosis complex from cultures or smear-positive sputa by use of molecular beacons. J. Clin. Microbiol. 42:4204-4208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martin, A., A. von Groll, K. Fissette, J. C. Palomino, F. Varaine, and F. Portaels. 2008. Rapid detection of Mycobacterium tuberculosis resistance to second-line drugs by use of the manual Mycobacterium Growth Indicator Tube system. J. Clin. Microbiol. 46:3952-3956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mikhailovich, V., S. Lapa, D. Gryadunov, A. Sobolev, B. Strizhkov, N. Chernyh, O. Skotnikova, O. Irtuganova, A. Moroz, V. Litvinov, M. Vladimirskii, M. Perelman, L. Chernousova, V. Erokhin, A. Zasedatelev, and A. Mirzabekov. 2001. Identification of rifampin-resistant Mycobacterium tuberculosis strains by hybridization, PCR, and ligase detection reaction on oligonucleotide microchips. J. Clin. Microbiol. 39:2531-2540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reference deleted.
- 15.Pfyffer, G. E., D. A. Bonato, A. Ebrahimzadeh, W. Gross, J. Hotaling, J. Kornblum, A. Laszlo, G. Roberts, M. Salfinger, F. Wittwer, and S. Siddiqi. 1999. Multicenter laboratory validation of susceptibility testing of Mycobacterium tuberculosis against classical second-line and newer antimicrobial drugs by using the radiometric BACTEC 460 technique and the proportion method with solid media. J. Clin. Microbiol. 37:3179-3186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raviglione, M. C., and I. M. Smith. 2007. XDR tuberculosis—implications for global public health. N. Engl. J. Med. 356:656-659. [DOI] [PubMed] [Google Scholar]
- 17.Rodrigues, C., J. Jani, S. Shenai, P. Thakkar, S. Siddiqui, and A. Mehta. 2008. Drug susceptibility testing of Mycobacterium tuberculosis against second-line drugs using the Bactec MGIT 960 System. Int. J. Tuberc. Lung Dis. 12:1449-1455. [PubMed] [Google Scholar]
- 18.Rusch-Gerdes, S., G. E. Pfyffer, M. Casal, M. Chadwick, and S. Siddiqi. 2006. Multicenter laboratory validation of the BACTEC MGIT 960 technique for testing susceptibilities of Mycobacterium tuberculosis to classical second-line drugs and newer antimicrobials. J. Clin. Microbiol. 44:688-692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanders, C. A., R. R. Nieda, and E. P. Desmond. 2004. Validation of the use of Middlebrook 7H10 agar, BACTEC MGIT 960, and BACTEC 460 12B media for testing the susceptibility of Mycobacterium tuberculosis to levofloxacin. J. Clin. Microbiol. 42:5225-5228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scarparo, C., P. Ricordi, G. Ruggiero, and P. Piccoli. 2004. Evaluation of the fully automated BACTEC MGIT 960 system for testing susceptibility of Mycobacterium tuberculosis to pyrazinamide, streptomycin, isoniazid, rifampin, and ethambutol and comparison with the radiometric BACTEC 460TB method. J. Clin. Microbiol. 42:1109-1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shah, N. S., A. Wright, G. H. Bai, L. Barrera, F. Boulahbal, N. Martin-Casabona, F. Drobniewski, C. Gilpin, M. Havelkova, R. Lepe, R. Lumb, B. Metchock, F. Portaels, M. F. Rodrigues, S. Rusch-Gerdes, A. Van Deun, V. Vincent, K. Laserson, C. Wells, and J. P. Cegielski. 2007. Worldwide emergence of extensively drug-resistant tuberculosis. Emerg. Infect. Dis. 13:380-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tenover, F. C., J. T. Crawford, R. E. Huebner, L. J. Geiter, C. R. Horsburgh, Jr., and R. C. Good. 1993. The resurgence of tuberculosis: is your laboratory ready? J. Clin. Microbiol. 31:767-770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tortoli, E., M. Benedetti, A. Fontanelli, and M. T. Simonetti. 2002. Evaluation of automated BACTEC MGIT 960 system for testing susceptibility of Mycobacterium tuberculosis to four major antituberculous drugs: comparison with the radiometric BACTEC 460TB method and the agar plate method of proportion. J. Clin. Microbiol. 40:607-610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization. 2008. Policy guidance on drug-susceptibility testing (DST) of second-line antituberculosis drugs. WHO/HTM/TB/2008.392. WHO, Geneva, Switzerland. [PubMed]
- 25.World Health Organization. 2007. Use of liquid TB culture and drug susceptibility testing (DST) in low and medium income settings. Summary report of the expert group meeting on the use of liquid culture media. 26 March 2007. WHO, Geneva, Switzerland.