Abstract
It was found previously that induction of innate immunity, particularly chemokines, is an important mechanism of rabies virus (RABV) attenuation. To evaluate the effect of overexpression of chemokines on RABV infection, chemokines macrophage inflammatory protein 1α (MIP-1α), RANTES, and IP-10 were individually cloned into the genome of attenuated RABV strain HEP-Flury. These recombinant RABVs were characterized in vitro for growth properties and expression of chemokines. It was found that all the recombinant viruses grew as well as the parent virus, and each of the viruses expressed the intended chemokine in a dose-dependent manner. When these viruses were evaluated for pathogenicity in the mouse model, it was found that overexpression of MIP-1α further decreased RABV pathogenicity by inducing a transient innate immune response. In contrast, overexpression of RANTES or IP-10 increased RABV pathogenicity by causing neurological diseases, which is due to persistent and high-level expression of chemokines, excessive infiltration and accumulation of inflammatory cells in the central nervous system, and severe enhancement of blood-brain barrier permeability. These studies indicate that overexpression of chemokines, although important in controlling virus infection, may not always be beneficial to the host.
Rabies virus (RABV) is a negative-strand RNA virus belonging to the Rhabidoviridae family, genus Lyssavirus, which causes rabies (fatal encephalomyelitis) in many species of mammals (5). More than 55,000 humans die of rabies each year worldwide (26). Once clinical signs develop, rabies is always fatal (12, 53). Despite the lethality of rabies, only mild inflammation and little neuronal destruction were observed in the central nervous system (CNS) of rabies patients (31, 32). Adaptation of wild-type (wt) RABV in laboratory animals and/or cell culture leads to attenuation in phenotype, and laboratory-adapted RABVs have been used for vaccine development (1, 10). To delineate the mechanism(s) of RABV attenuation, previous studies compared the host responses to infection with either laboratory-attenuated or wt RABV (52). It was found that laboratory-attenuated RABV induced extensive inflammation, apoptosis, and neuronal degeneration, as well as induction of expression of innate immune genes in the CNS; however, wt RABV caused little or no neuronal damage and avoided the activation of expression of innate molecule genes. Other investigators also reported the induction of innate immunity in mice or neuronal cells infected with laboratory-attenuated viruses (20, 33, 37). The mostly upregulated genes in the innate immune responses after infection with attenuated RABV include genes encoding for inflammatory chemokines and type I interferon (IFN) as well as IFN-related proteins (20, 33, 378). Further studies have shown that the expression of chemokines (mRNA and proteins), particularly macrophage inflammatory protein 1α (MIP-1α; CCL3), RANTES (CCL5), and IP-10 (CXCL10), correlates with the infiltration of inflammatory cells and enhancement of blood-brain barrier (BBB) permeability (23).
Chemokines are a group of small (∼8- to 14-kDa), basic, structurally related molecules that can attract inflammatory cells along concentration gradients and enhance leukocyte-endothelial cell interactions (55). The tertiary structure of chemokines is highly conserved; they contain at least four cysteine residues that form two disulfide bonds (50). Chemokines have been divided into major subfamilies on the basis of the arrangement of the two N-terminal cysteine residues, CC and CXC. CC chemokines act primarily upon monocytes, whereas CXC family members are specific for neutrophils and lymphocytes (14). Chemokines regulate cell trafficking of various types of leukocytes through interactions with G-protein-coupled receptors with seven transmembrane regions (55). Most chemokine receptors are stimulated by more than one chemokine, and one ligand can bind to more than one receptor (50). This combination of redundancy and promiscuity might act as a safety factor to ensure adequate host defenses (15, 30). Chemokines have direct antiviral activities and/or recruit inflammatory cells to the site of infection to kill virus or virus-infected cells (30, 34). However, due to their ability to direct migration of inflammatory cells, overexpression of chemokines may have detrimental effects, especially in the process of autoimmune inflammation. In an experimental autoimmune encephalomyelitis model, IP-10, monocyte chemoattractant protein 1 (MCP-1), and MIP-1α were strongly upregulated (14). Administration of anti-IP-10 antibody decreased disease incidence and severity and the infiltration of mononuclear cells into the CNS (11).
In the present study, the roles of chemokines in RABV infection were further investigated by cloning and expressing MIP-1α, RANTES, and IP-10 in the genome of the RABV HEP-Flury strain. It was found that overexpression of MIP-1α decreased the pathogenicity by inducing transient expression of chemokines and infiltration of inflammatory cells into the CNS. In contrast, recombinant RABV expressing RANTES and IP-10 induced persistent and high-level expression of chemokines and extensive infiltration of inflammatory cells into the CNS, causing neurological diseases and death.
MATERIALS AND METHODS
Cells, viruses, antibodies, and animals.
Mouse neuroblastoma cells (NA) were maintained in RPMI 1640 medium (Mediatech, Herndon, VA) supplemented with 10% fetal bovine serum (Gibco, Grand Island, NY). BSR cells, a cloned cell line derived from BHK-21 cells, were maintained in Dulbecco's modified Eagle's medium (Mediatech) containing 10% fetal bovine serum. Recombinant RABV strains were propagated in BSR cells. CVS-11 was propagated in mouse neuroblastoma cells. CVS-24 was propagated in suckling mouse brains as described previously (54). Fluorescein isothiocyanate (FITC)-conjugated antibody against the RABV N protein was purchased from FujiRab (Melvin, PA). Anti-RABV nucleoprotein (N) monoclonal antibody 802-2 was obtained from Charles Rupprecht, Centers for Disease Control and Prevention. Antibodies used for flow cytometric analysis, such as CD3 (17A2), Ly6G (RB6-8C5), CD45 (30-F11), and CD11b (M1/70), were purchased from BD Pharmingen (San Jose, CA). Anti-CD3 polyclonal antibody was purchased from Abcam (England). Biotinylated secondary antibodies were purchased from Vector Laboratories (Burlingame, CA). Female BALB/c mice at the age of 6 to 8 weeks were purchased from Harlan and housed in temperature- and light-controlled quarters in the Animal Facility, College of Veterinary Medicine, University of Georgia. All animal experiments were carried out as approved by the Institutional Animal Care and Use Committee.
Construction of recombinant RABV clones.
Mouse MIP-1α, RANTES, and IP-10 cDNAs were amplified from RNA extracted from RABV-infected mouse brain using the SuperScript III One-Step reverse transcription (RT)-PCR system with Platinum Taq DNA polymerase (Invitrogen-Life Technology). The primer sets used for PCR were designed by Primer3 (http://primer3.sourceforge.net/) (Table 1). The PCR products were digested with BsiWI and NheI (New England Biolabs, Berverly, MA) and then ligated into RABV vector pHEP-3.0 (18) that had been previously digested with BsiWI and NheI. The resulting plasmids had each of the chemokine genes cloned between RABV glycoprotein (G) and the polymerase (L) genes and were designated pHEP-MIP1α, pHEP-RANTES, and pHEP-IP10, respectively (Fig. 1).
TABLE 1.
Primers used for amplification of chemokines
| Chemokine | Sequence |
|
|---|---|---|
| Forward primer (5′-3′) | Reverse primer (3′-5′) | |
| MIP-1α | CTGCTCCGTACGATGAAGGTCTCCACCACT | CCTCCAGCTAGCTCAGGCATTCAGTTCCAG |
| RANTES | GCCGCGCGTACGATGAAGATCTCTGCAGCT | AAACCCGCTAGCCTAGCTCATCTCCAAATA |
| IP-10 | CCCATCCGTACGATGAACCCAAGTGCTGCC | GCTTCAGCTAGCTTAAGGAGCCCTTTTAGA |
FIG. 1.
Construction and characterization of recombinant RABVs expressing different chemokins. (A) Construction of full-length recombinant RABVs. Chemokine genes MIP-1α, RANTES, and IP-10 were individually inserted between BsiWI and NheI sites of the pHEP-3.0 vector. (B) Growth curves of the recombinant and parental rabies viruses in NA cells. NA cells were infected with different recombinant RABVs at a multiplicity of infection (MOI) of 0.01. At days 1, 2, 3, 4, and 5 p.i., culture supernatants were recovered and virus titers were determined in NA cells. (C) Chemokine production in NA cells by recombinant viruses. NA cells were infected with different recombinant RABVs at MOIs of 0.001, 0.01, 0.1 and 1. After 24 h of incubation at 34°C, the culture supernatants were recovered and the concentration of the indicated chemokine was determined by ELISA.
Rescue of recombinant RABV.
Recombinant RABVs were rescued as described previously (18). Briefly, BSR cells were transfected with 2.0 μg of full infectious clone, 0.5 μg of pH-N, 0.25 μg of pH-P, 0.1 μg of pH-L, and 0.15 μg of pH-G using SuperFect transfection reagent (Qiagen, Valencia, CA) according to the manufacturer's protocol. After incubation for 4 days, the culture medium was removed and fresh medium added to the cells. After incubation for another 3 days, the culture medium was transferred into NA cells and examined for the presence of rescued virus by using FITC-conjugated antibody against the RABV N protein.
Virus titration.
Viruses were titrated by direct fluorescent antibody assay in NA cells. NA cells in 96-well plates were inoculated with serial 10-fold dilutions of virus and incubated at 34°C for 2 days. The culture supernatant was removed and the cells were fixed with 80% ice-cold acetone for 30 min. The cells were then stained with FITC-conjugated anti-RABV N antibodies. Antigen-positive foci were counted under a fluorescence microscope (Zeiss, Germany), and viral titers were calculated as fluorescent focus units (FFU) per milliliter. All titrations were carried out in quadruplicate.
ELISA and multiplex ELISA.
Brains were homogenized in a ninefold volume of phosphate-buffered saline (PBS) containing 0.1% NP-40 and Complete protease inhibitor (Roche Applied Science, Indianapolis, IN). The homogenates were centrifuged at 11,000 × g for 30 min to remove debris, and the supernatants were taken out carefully and aliquoted into microtubes at 0.5 ml/tube. The supernatant was subjected to an enzyme-linked immunosorbent assay (ELISA) to quantify the amount of MIP-1α, RANTES, and IP-10 individually in cell culture supernatants or mouse brain suspensions by using the murine MIP-1α, RANTES, and IP-10 ELISA kit (R&D Systems, Minneapolis, MN) according to the manufacturer's protocol. A multiplex ELISA kit (Quansys Biosciences, Logan, UT) was used to quantify a panel of 16 cytokines (interleukin-1α [IL-1α], IL-1β, IL-2, IL-3, IL-4, IL-5, IL-6, IL-10, IL-12p70, IL-17, MCP-1, IFN-γ, tumor necrosis factor alpha [TNF-α], MIP-1α, granulocyte-macrophage colony-stimulating factor, and RANTES) in brain extracts according to the manufacturer's protocol.
Quantitative real-time RT-PCR.
To determine viral load, real-time RT-PCR was performed on the RNA samples using G gene-specific primers (5′-CCATCTGGATGCCTGAGAAT-3′ and 5′-GGCACCATTTGGTCTCATCT-3′) in an Mx3000P apparatus (Stratagene, La Jolla, CA). With a 100-ng sample RNA or no-template control, PCR was performed in two steps; only one primer was used for cDNA synthesis at 50°C for 30 min, and both primers were used in PCR amplification. Each reaction was carried out in duplicate. The reverse transcriptase and DNA polymerase were from a One-Step Brilliant II SYBR green QRT-PCR master mix kit (Stratagene). For absolute quantitation, a standard curve was generated from serial diluted RABV G RNAs of known copy numbers, and the copy numbers of samples were normalized to 1 μg of total RNA. The RNA standard was prepared from pH-G by using a reverse transcription system (Promega) according to the manufacturer's protocol.
Histopathology and immunohistochemistry.
For histopathology and immunohistochemistry, animals were anesthetized with ketamine-xylazine and perfused by intracardiac injection of PBS followed by 10% neutral buffered formalin as described previously (23). Brain tissues were removed and embedded with paraffin. Histopathology was performed by staining the paraffin-embedded sections with hematoxylin and eosin. For immunohistochemistry, paraffin-embedded brain sections were heated at 70°C for 10 min and then dipped in CitriSolv (Fisher Scientific) three times for 5 min and dried until chalky white. Slides were incubated with proteinase K (20 μg/ml) in 10 mM Tris-HCl (pH 7.4 to 8.0) for 15 min at 37°C and rinsed three times with PBS. The primary antibodies and then secondary antibodies were used for immunological reactions. Finally, diaminobenzidine was used as a substrate for color development.
Leukocyte isolation from the CNS.
Mouse brains infected with different recombinant viruses were harvested on days 3, 6, and 9 postinfection (p.i.) and digested with 2 μg/μl collagenase D (Worthington Biochemical Corporation, Lakewood, NJ), 1 μg/μl DNase I (Sigma-Aldrich) in Hanks balanced salt solution (with Ca2+ and Mg2+) for 1 h to disperse the tissue into single-cell suspension. Viable cells were separated by discontinuous Percoll gradient (70/30%) centrifugation for 25 min (650 ×g at room temperature, without brake). After being washed once with Hanks balanced salt solution (without Ca2+ or Mg2+; Invitrogen) and counted, cells were stained for CD3 (17A2), Ly6G (RB6-8C5), CD45 (30-F11), and CD11b (M1/70) with directly conjugated antibodies (BD Pharmingen) for 30 min at 4°C and then fixed with 1% paraformaldehyde. Data collection and analysis were performed with a BD LSR-II flow cytometer and BD FACSDiva software (BD Pharmingen).
Measurement of BBB permeability.
BBB permeability was assessed using a modification of a previously described technique (35, 49) with the following markers: sodium fluorescein (NaF; 100 μl of 100 mg/ml, intravenous [i.v.]); fluorescein-dextran (FITC-dextran) of molecular mass 10,000 Da (FITC-dextran-10,000; 200 μl of 100 mg/ml; i.v.); fluorescein-dextran (FITC-dextran) of molecular mass 150,000 Da (FITC-dextran-150,000; 200 μl of 37.5 mg/ml, i.v.). Mice received these markers intravenously under anesthesia. After 10-min circulation for NaF and FITC-dextran-10,000 and 4-h circulation for FITC-dextran-150,000, peripheral blood was collected. Serum (50 μl) was recovered and mixed with an equal volume of 15% trichloroacetic acid (TCA). After centrifugation for 10 min at 10,000 × g, the supernatant was recovered and made up to 150 μl by adding 30 μl 5 M NaOH and 7.5% TCA. The brain was perfused with PBS injected through the left ventricle to flush out intravascular fluorescein. Then the brain tissues were homogenized in cold 7.5% TCA and centrifuged for 10 min at 10,000 × g to remove insoluble precipitates. After addition of 30 μl 5 M NaOH to 120 μl supernatant, the fluorescence was determined using a BioTek spectrophotometer (Bio-Tek Instruments) with excitation at 485 nm and emission at 530 nm. Markers taken up into tissue are expressed as the micrograms of fluorescence in cerebrum per mg of brain tissue divided by the micrograms of fluorescence per μl of serum to normalize uptake values of the dye for blood levels of the dye at the time of tissue collection (49).
Statistical analyses.
All experiments were repeated at least three times. Statistical significance of the differences between different treatment groups was analyzed with SigmaStat software (Systat Software Inc., San Jose, California). One-way analysis of variance with the Holm-Sidak method was used to analyze clinical score, body weight, chemokine/cytokine concentration, and immune cell infiltration into the CNS.
RESULTS
In vitro characterization of recombinant RABVs.
Our previous studies indicated that induction of chemokines, particularly MIP-1α, RANTES, and IP-10, is important for RABV attenuation (23, 52). To further investigate the roles of chemokines in RABV infection, the genes encoding murine MIP-1α, RANTES, and IP-10 were amplified from virus-infected mouse brain and cloned into rHEP (18) between the G and the L genes (Fig. 1A). Recombinant viruses were rescued in BSR cells as described previously (18), and these viruses are designated as HEP-MIP1α, HEP-RANTES, and HEP-IP10, respectively. To characterize these viruses in vitro, the growth kinetics of these viruses were examined in NA cells. As shown in Fig. 1B, no significant difference in growth kinetics was observed between each of the recombinant viruses and the parental virus, indicating that viral growth was not affected by the insertion of chemokines. The ability of the recombinant RABV to produce chemokines was determined by measuring chemokine production in virus-infected cells. As shown in Fig. 1C, production of the intended chemokine was detected in NA cells infected with each recombinant RABV in a dose-dependent manner. No chemokine was detected in NA cells infected with parent virus rHEP.
Pathogenicity of recombinant RABVs in mice.
To determine the effect of chemokine expression on RABV infection, BALB/c mice (10 per group) at 6 to 8 weeks of age were infected with 105 FFU of recombinant viruses by the intracerebral (i.c.) route. Infected mice were monitored twice daily for 2 weeks. Body weight was measured, and the development of diseases and death was recorded. The animals were scored for clinical signs as follows: 0, normal mouse; 1, disorder movement; 2, ruffled fur; 3, trembling and shaking; 4, paralysis; 5, dead.
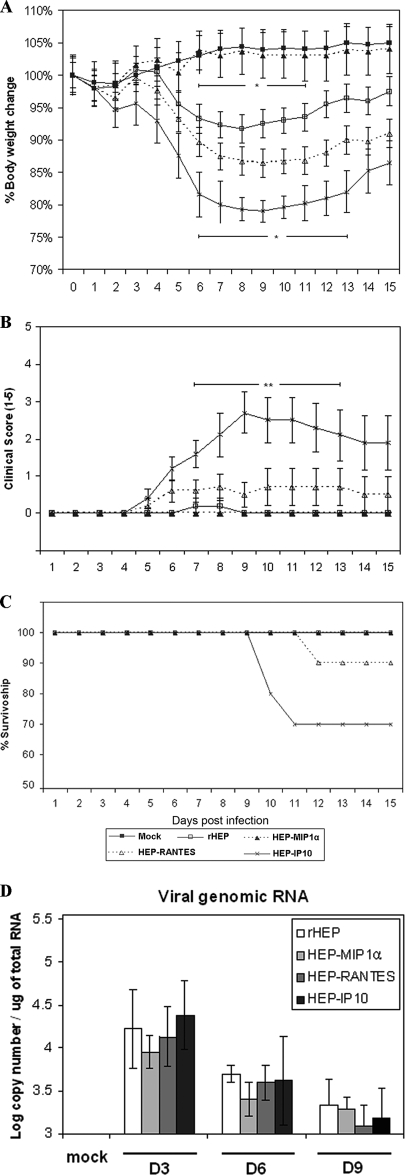
As shown in Fig. 2A, mice infected with HEP-MIP1α were similar to sham-infected mice during the observation period. Neither obvious weight loss nor clinical signs were observed in these two groups of mice. Mice infected with parent virus rHEP lost about 7% of their body weight compared with sham-infected mice (P ≤ 0.05), and one mouse developed mild symptoms including rough fur and slow movement at days 6 to 9 p.i. and then recovered. Mice infected with HEP-RANTES lost about 14% of their body weight and 30% of the mice developed severe symptoms such as rough fur and emaciation, but no paralysis. One mouse in this group died at day 12 p.i. (Fig. 2C). Mice infected with HEP-IP10 lost about 21% of their body weight. Seventy percent of the mice in this group developed severe symptoms, and 30% of the mice succumbed to infection at day 10 or 11 p.i. (Fig. 2C). The observed symptoms in HEP-IP10-infected mice occurred significantly more frequently (P ≤ 0.01) than in mice infected with the parental virus (Fig. 2B). Mice infected with HEP-IP10 lost more body weight (P ≤ 0.05) than those infected with the parent virus (Fig. 2A). These results indicate that recombinant RABV expressing MIP-1α is more attenuated while viruses expressing RANTES or IP-10 enhanced RABV pathogenicity compared to the parental virus.
FIG. 2.
Effects of overexpression of chemokines on virus pathogenicity and virus replication. Body weight (A), clinical score (B), survivorship (C), and viral genomic RNA (D) were monitored in BALB/c mice (n = 10) after i.c. infection with 105 FFU of different recombinant RABV or medium (sham infection) as described in Materials and Methods. Data were obtained from 10 mice (three mice for genomic RNA) in each group and are given as mean values ± standard errors. Asterisks indicate significant differences between the indicated experimental groups: *, P < 0.05; **, P < 0.01; ***, P < 0.001.
To determine if the effects of chemokines on pathogenicity are associated with virus replication, the virus titers, viral antigen, and viral genomic RNA in the mouse brain were determined at days 3, 6, and 9 p.i. Consistent with the previous study (47), virus titer was not detected in the brains of mice infected with any of the viruses during the period (data not shown). By immunohistochemical analysis, viral antigen (N) was only sporadically detected in the region of hippocampus at only day 3 p.i. in mice infected with each of the viruses, but not in sham-infected mice (data not shown). Quantification of viral genomic RNA by real-time PCR revealed that the copy number of viral genomic RNA in mouse brains was highest at day 3 p.i. Although the lowest copy number of viral genomic RNA was detected in mice infected with HEP-MIP-1α among all the groups, particularly at days 3 and 6 p.i., there is no significant difference for the quantity of the genomic RNA among mice infected with the parent or the recombinant viruses (Fig. 2D). The data indicate that the rate of viral replication is low, and overexpression of chemokines has no apparent effect on viral replication in adult mice. Thus, the rate of replication is not a determinant for the pathogenicity of different recombinant viruses expressing different chemokines.
Expression of chemokines and cytokines in mouse brain after infection with recombinant RABVs.
To investigate the mechanism of HEP-MIP1α attenuation relative to rHEP and of exacerbated disease associated with HEP-RANTES and HEP-IP10 viruses, the expression of these chemokines was determined by ELISA. A multiplex ELISA was also performed to measure the expression of other inflammatory chemokines and cytokines. As shown in Fig. 3, all the recombinant viruses induced the expression of the intended chemokine to high levels at day 3 p.i. except HEP-IP10, which induced high-level IP-10 expression at day 6 p.i. Interestingly, expression of one chemokine led to the expression of other chemokines. Virus expressing MIP-1α induced only a transient high level of MIP-1α at day 3 p.i. (P ≤ 0.01), and its expression declined quickly by days 6 and 9 p.i. Expression of MIP-1α did induce the expression of other chemokines compared to sham-infected mice. However, the level of expression was mostly the lowest among the mice infected with all the recombinant viruses. In contrast, viruses expressing RANTES or IP-10 not only induced high and persistent expression of the respective chemokines but also induced high expression of other chemokines. HEP-RANTES induced significantly higher expression of RANTES at day 3 (P ≤ 0.01) and 6 p.i. (P ≤ 0.05) than the parent virus, and the level persisted with a slight reduction by day 9 p.i. This virus also induced a higher level of IP-10 expression (P ≤ 0.001) at day 6 p.i. than the parent virus and HEP-MIP1α. HEP-IP10 induced a significantly higher level of IP-10 expression at day 6 p.i. than the parent virus and HEP-MIP1α (P ≤ 0.001). The IP-10 expression was slightly reduced by day 9 p.i. in HEP-IP-10-infected mice, but still significantly higher than in mice infected with other viruses (P ≤ 0.05). In addition, HEP-IP10 induced higher expression of other chemokines and cytokines as well. It induced the highest expression of MIP-1α at day 6 and RANTES at day 9 p.i. It also induced the highest expression of MCP-1, TNF-α, and IL-6 at days 6 and 9 p.i. The parent virus rHEP induced the highest expression of RANTES at day 6 p.i. and only low expression of all other chemokines or cytokines. Overall, parent rHEP and HEP-MIP1α induced low-level expression of chemokines and cytokines while HEP-RANTES, particularly HEP-IP10, induced high expression of not only the intended chemokine but also other chemokines and cytokines. Expression of IP-10, MCP-1, and TNF-α at high levels correlates well with the development of diseases in the animals.
FIG. 3.
Concentration of chemokines and cytokines in mouse brains after infection with recombinant RABVs. BALB/c mice were infected i.c. with 105 FFU different recombinant RABVs. At days 3, 6, and 9 p.i., brains were harvested and homogenized. After centrifugation, the suspension was used to measure the concentration of indicated chemokines and cytokines by using multiplex ELISA kits. Experiments were performed with three mice for each time point and condition. Asterisks indicate significant differences between experimental groups: *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Induction of inflammation in mouse brain by recombinant RABVs.
Chemokines and cytokines produced in large quantities may cause the huge influx of inflammatory cells into the brains (50). To investigate if expression of chemokines and cytokines induces inflammation in the CNS of mice infected with each of the recombinant RABVs, histopathology was performed to analyze the inflammatory cells present in brain tissue. Less infiltration of inflammatory cells was observed in the brain of mice infected with HEP-MIP1α than that in rHEP-infected mouse brain at days 3, 6, and 9 p.i. At day 6 p.i., HEP-RANTES and HEP-IP10 induced much more inflammatory infiltration than rHEP. By day 9 p.i., infiltration of inflammatory cells decreased in rHEP-infected mice, while infiltration of inflammatory cells continued to persist or increase at day 9 p.i. in HEP-RANTES- and HEP-IP10-infected mice. No inflammatory cells were seen in brains of sham-infected mice (Fig. 4A). To quantify the infiltration of inflammatory cells, immunohistochemical analysis revealed that slightly fewer CD3-positive cells were detected in the HEP-MIP1α-infected mouse brains than in those infected with rHEP at days 3, 6, and 9 p.i., while significantly more CD3-positive cells were detected in the brains of mice infected with HEP-RANTES and HEP-IP10 at 6 and 9 day p.i. (P ≤ 0.001). By day 9 p.i., the number of CD3-positive cells decreased in mice infected with rHEP but continued to increase in mice infected with HEP-RANTES and HEP-IP10 (Fig. 4B and C).
FIG. 4.
Inflammatory responses induced by recombinant RABVs. BALB/c mice were infected i.c. with 105 FFU different recombinant RABVs, and brains were harvested after extensive perfusion at days 3, 6, or 9 p.i. (A) Pathological changes were observed in paraffin sections after hematoxylin and eosin staining. (B) Quantification of CD3-positive T lymphocytes in the hippocampus sections was performed with anti-CD3 antibody. (C) CD3-positive cell numbers were quantified and are expressed as mean values ± standard errors obtained from three mice at each time point. Asterisks indicate significant differences between the indicated experimental groups: *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Differentiation of inflammatory cells infiltrated into or activated in mouse brain after infection with recombinant RABVs.
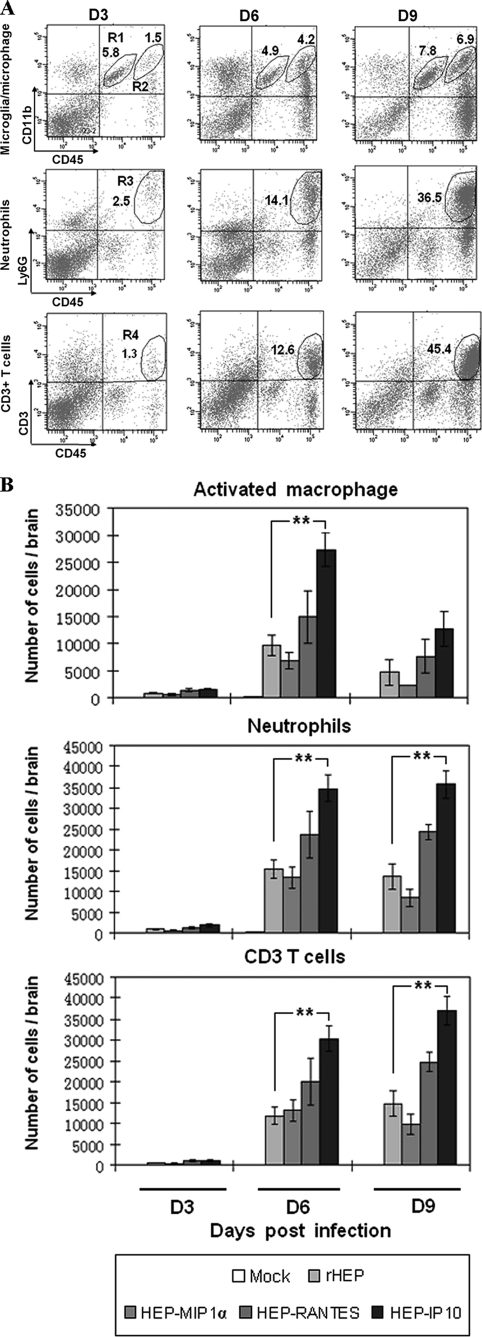
To differentiate the inflammatory cells infiltrated into or activated in the CNS after infection with different RABVs, leukocytes were recovered from mouse brains and analyzed by flow cytometry. The populations of activated microglia/microphage, neutrophils, and T cells were differentiated using cell surface markers CD11b, Ly6G, and CD3, respectively (Fig. 5A). CD45 was used as a maker for all the inflammatory cells. At day 3 p.i., the cells of each type were found to be less than 3 × 103/brain (Fig. 5A), and no significant difference was detected among these groups of mice infected with each recombinant virus. By day 6 p.i., inflammatory cells increased quickly to more than 104/brain (Fig. 5A). HEP-MIP1a induced equal or less while HEP-RANTES induced more infiltration of all the cell types compared with the parent virus. However, no significant differences were observed. On the other hand, HEP-IP10 induced significantly more infiltration of activated microglia/macrophages (P = 0.0042), neutrophils (P = 0.0056), and CD3+ T cells (P = 0.0041) compared with the parent virus. By day 9 p.i., the number of CD11bhi/CD45hi activated microglia/macrophages decreased in all groups (Fig. 5B), whereas the number of neutrophils and CD3+ T cells remained the same or continued to increase in HEP-RANTES- and especially in HEP-IP10-infected mouse brains. Taken together, the histopathological and flow cytometric analyses suggested that the increased neutrophils and CD3+ T cells trafficking to and accumulating in the mouse brain correlate with the pathogenicity of HEP-RANTES and HEP-IP10.
FIG. 5.
Differentiation of inflammatory cells that infiltrated into the CNS by using flow cytometric analysis. BALB/c mice were infected i.c. with 105 FFU of different recombinant RABVs, and brains were harvested after extensive perfusion at days 3, 6, and 9 p.i. CNS leukocytes were isolated by Percoll centrifugation and analyzed by flow cytometry with the indicated antibodies. (A) Representative flow cytometric plots of inflammatory cell infiltration in the mouse brain at days 3, 6, and 9 p.i. with HEP-IP10. Resting microglia (CD45int, CD11bint) appear in region 1 (R1), and activated microglia/macrophages (CD45hi, CD11bhi) appear in R2. CD45hi Ly6Ghi cells that appear in R3 were defined as neutrophils. CD3+ T cells appear in R4. (B) The absolute numbers of specific inflammatory cells in brains were calculated (three mice per group for each time point). Asterisks indicate significant differences between the indicated experimental groups: *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Enhancement of BBB permeability after infection with recombinant RABV.
To investigate if infection with each of the recombinant viruses induces changes in BBB permeability, the leakage of sodium fluorescein from the circulation into CNS tissues was measured in the cerebrum, cerebellum, and spinal cord. No significant change in BBB permeability was observed in the cerebellum or the spinal cord (data not shown). BBB permeability was significantly enhanced in the cerebrum of mice infected with all the viruses by 6 days p.i compared to sham-infected mouse brain. BBB permeability in mice infected with HEP-RANTES or HEP-IP10 was significantly higher than that of rHEP- or HEP-MIP1α-infected mice. By day 9 p.i., BBB permeability in mice infected with HEP-IP10 was significantly higher than that in rHEP-infected mice (P ≤ 0.01) or HEP-RANTES-infected mice (P ≤ 0.05) (Fig. 6A). These data indicate that infection with all the viruses enhanced BBB permeability at day 6 p.i. compared to sham infection. Furthermore, HEP-IP10 induced significantly higher and more persistent BBB permeability than parent virus or HEP-MIP1α.
FIG. 6.
Determination of changes in BBB permeability and chemokine levels in the brain versus serum. BALB/c mice were infected i.c. with 105 FFU of recombinant RABVs. At days 3, 6, and 9 p.i., BBB permeability was determined by uptake of NaF (A). The extent of BBB permeability to different-sized markers was compared at day 6 p.i. (B). The concentrations of chemokines in both serum and brains were assayed by ELISA (C). Each set of data has at least triplicates. Data are given as mean values ± standard errors. Asterisks indicate significant differences between the indicated experimental groups: *, P < 0.05; **, P < 0.01; ***, P < 0.001.
To investigate if overexpression of different chemokines can induce BBB changes so that large molecules can easily enter the CNS, different-sized markers such as NaF (376 Da), FITC-dextran-10,000 (10 kDa), and FITC-dextran-150,000 (150 kDa) were used to measure changes of BBB permeability at day 6 p.i. As shown in Fig. 6B, molecules of 150 kDa or larger did not infiltrate into the cerebrum for any mice in any of the groups. Only HEP-IP10 induced significantly higher permeability to a 10-kDa marker (P ≤ 0.001) than other viruses. This indicates that overexpression of chemokines MIP-1α or RANTES can induce enhancement of BBB permeability to allow small molecules (NaF, 376 Da) to enter into the CNS, while overexpression of IP-10 can significantly enhance the permeability to allow not only small but also large molecules (10 kDa) across the BBB.
To investigate if the enhancement of BBB permeability is associated with chemokine expression in the brain or in the serum, the concentrations of chemokines (MIP-1α, RANTES, and IP-10) were determined at day 6 p.i. As shown in Fig. 6C, the concentrations of chemokines (MIP-1α, RANTES, and IP-10) in the brain were much higher than that in the serum. Overall, infection with different viruses by the i.c. route did not significantly affect the chemokine concentration in the serum. In the mouse brain, HEP-RANTES induced a significantly higher production of RANTES and IP-10, while HEP-IP10 induced a significantly higher production of IP-10. Only the IP-10 level correlated well with the enhancement of BBB permeability.
DISCUSSION
The RABV genome has been used to express antigens from other viruses (7, 28, 45), host proteins (7, 29, 38), or an extra copy of the RABV G gene (8). Expression of these proteins in the RABV genome invariably results in virus attenuation in the mouse model. For example, expression of host proteins, such as cytochrome c, TNF-α, or IL-2, has led to attenuated pathogenicity (7, 29, 38). In the present study, chemokines MIP-1α, RANTES, and IP-10 were cloned into the genome of the RABV HEP-Flurry strain. It was found that although expression of MIP-1α further reduced RABV pathogenicity, expression of RANTES, or IP-10 enhanced RABV pathogenicity in the mouse model. It has been reported previously that expression of host immune proteins, notably IL-4, resulted in enhanced pathogenicity in other viral expression systems. It is believed that expression of IL-4 may downregulate immune responses, thus exacerbating diseases. Ectromelia virus expressing IL-4 developed symptoms of acute mousepox with high mortality by suppressing cytolytic responses of NK and cytotoxic T lymphocytes (CTL) and the expression of IFN-γ by the latter (19). The clearance of recombinant vaccinia virus expressing IL-4 was delayed compared with control recombinant vaccinia virus because the expression of IL-4 suppresses antiviral CTL responses and production of nitric oxide (44). Expression of IL-4 by recombinant respiratory syncytial virus resulted in an accelerated pulmonary inflammatory responses, yet the CTL response was deficient in the production of IFN-γ and was nonfunctional for in vitro cell killing (4).
The rationale to clone chemokines into the RABV genome was to further investigate the role of chemokines in RABV infection, because our previous studies showed that expression of chemokines, particularly MIP-1α, RANTES, and IP-10, correlates with infiltration of inflammatory cells into the CNS, enhancement of BBB permeability, and attenuation of RABV (23). Inflammatory cells and other immune effectors attracted by chemokines enter the CNS and help clear RABV-infected cells, thus attenuating RABV pathogenicity. Yet, infection with the recombinant RABV expressing these chemokines resulted in a very different outcome. One possibility is that expression of these chemokines affects virus replication. To this end, virus titers, viral antigen, and viral genomic RNA were measured in the mouse brain at various time points after infection. No virus was detected, and viral antigen was detected only sparsely in mice infected with each of the viruses. Quantitative RT-PCR revealed no significant difference in the copy numbers of viral genomic RNA. Thus, expression of chemokines did not change the rate of RABV replication in the context of HEP-Flurry strain and thus could not account for the difference of pathogenicity induced by these recombinant RABVs.
Chemokines are redundant and multifunctional. Expression of one chemokine in the brain could induce the expression of other chemokines or cytokines and thus would have profound effects in recruiting different subsets of inflammatory cells into the CNS (30). To determine if expression of a particular chemokine in the RABV genome leads to the expression of other chemokines and infiltration of a particular set(s) of inflammatory cells, the expression of chemokine/cytokine was monitored using a multiplex ELISA, and inflammatory cells infiltrating into the CNS were differentiated by flow cytometry. Each of the recombinant viruses expressed high levels of the intended chemokine at day 3 or 6 p.i. However the level of MIP-1α in mice infected with HEP-MIP1α subsided quickly. In addition, only low to moderate levels of other chemokines are induced in these mice. Likewise, only low and transient infiltration of inflammatory cells at day 6 p.i., and by day 9 p.i. infiltration of inflammatory cells returned to the level found in sham-infected animals. In contrast, HEP-RANTES and particularly HEP-IP10 not only induced high and persistent expression of the intended chemokines but also induced high expression of other chemokines. High and persistent infiltration of inflammatory cells, particularly neutrophils and T cells, was also observed in the CNS, which can produce neurotoxins, free radicals, and proinflammatory cytokines, causing CNS destruction (13).
Overall our studies indicate that transient expression of chemokines may help attenuation, while the high and persistent expression of these chemokines, particularly IP-10, may be responsible for the enhanced pathogenicity. It is known that MIP-1α is a monocyte chemokine and may activate resident microglia within the brain (27, 39). Microglia are constantly moving and analyzing the CNS and are able to recognize and swallow foreign antigens and act as antigen-presenting cells (39). It is conceivable that the high level of MIP-1α expression in the earlier stage of infection results in activation of residential microglia and inhibition of virus replication. As a consequence, less virus replication leads to less expression of other chemokines/cytokines and less infiltration of inflammatory cells. Indeed, the least amount of viral genomic RNA was detected in mice infected with recombinant RABV expressing MIP-1α among all the infected groups. Likewise, the expression levels of chemokines/cytokines are the lowest in this group of mice, except for the high level of MIP-1α expression at day 3 p.i. Consequently, the least infiltration of inflammatory cells into the CNS was observed in this group of mice when compared with the groups of mice infected with other RABVs. In contrast, the expression of RANTES or IP-10 attracted large numbers of neutrophils and T cells into the CNS (6, 43, 48), which resulted in the induction of a high level of IFN-γ and TNF-α expression (14), leading to severe diseases and deaths.
It seems that the results from this present study contradict our previous findings, particularly with regard to IP-10 expression. In our previous study, expression of IP-10 correlated with RABV attenuation (23, 52). In those studies, attenuated RABV strain B2C was used. In the present study, overexpression of IP-10 induced immune-mediated diseases. This could be related to the stage of disease or the amount and the duration of chemokine expression. Earlier and transient expression of chemokines including IP-10 is important in clearing RABV from the CNS; however, high and persistent expression may cause excessive damage. A high level of IP-10 expression was detected at the stages of diseases when animals were infected with B2C at high doses, and extensive inflammation and apoptosis were found in these animals (42, 52). Thus, the findings in the present study are not contradictory to our previous studies; rather, they support our previous hypothesis that laboratory-attenuated RABV induces neurological diseases by immune-mediated pathogenesis (52). Beneficial and detrimental effects of chemokine expression, particularly IP-10, have also been reported in other viral infections. For example, expression of IP-10 in CNS following infection with mouse hepatitis virus (MHV) (25), lymphocytic choriomeningitis virus (3), and Theiler's virus (16) is important in initiating and maintaining protective Th1 immune responses. Overexpression of IP-10 from the MHV genome promoted protection from coronavirus-induced neurological and liver diseases (51). Neutralization or genetic deficiency of CXCL10 in mice leads to increased viral burden and delayed virus clearance upon infection with West Nile virus (22) or MHV (6). However, persistent expression of IP-10 following MHV infection may be detrimental to the host by recruiting excessive CD4+ T cells into the CNS. CD4+ T cells release additional chemokines, such as RANTES, which enhances the infiltration of macrophages and increase the severity of demyelination (24, 25). The precise role of chemokines, particularly IP-10, in RABV protection and pathogenicity is not currently known and will be addressed by controlling (with small interfering RNA) or ablating (knocking out) the expression of each chemokine.
Recently it has been reported that enhancement of BBB permeability is one of the important mechanisms for RABV attenuation (35, 40, 41). Pathogenic strains of RABV, such as SHBRV, are deficient in BBB opening and prevent immune effectors from entering the CNS. On the other hand, attenuated RABV induces enhancement of BBB permeability, thus allowing small molecules (presumably immune effectors) to enter the CNS (9). In our study, we found that all the recombinant RABVs enhanced the BBB permeability; however, HEP-RANTES and HEP-IP10 induced more extensive and prolonged enhancement of BBB permeability than HEP-MIP1α or rHEP. Furthermore, HEP-IP10 induced BBB permeability to the extent that allowed large molecules (10 kDa) to enter the CNS. Although the consequence is not entirely clear, this may have allowed more inflammatory cells or other toxic substances to enter into the CNS, resulting in severe diseases and deaths. In other virus models of CNS autoimmunity and virus-induced neuroinflammation, such as experimental autoimmune encephalomyelitis (21), multiple sclerosis (46), lymphocytic choriomeningitis virus infection (2), and Borna disease (17), CNS inflammation was generally associated with increased BBB permeability and CNS damage and disease. CNS inflammation can be prevented by decreasing or inhibiting BBB permeability (17, 21, 36). Thus, precaution should be taken if strategies to enhance BBB permeability are to be developed to treat clinical rabies or other CNS diseases.
Acknowledgments
This work was supported partially by Public Health Service grant AI-051560 from the National Institute of Allergy and Infectious Diseases (Z.F.F.) and by a grant from The Natural Science Foundation of China (30928020 to Z.F.F. and H.C.).
We thank Charles Rupprecht from the Centers for Disease Control and Prevention for supplying monoclonal antibody 802-2. We also thank Yongjun Wen and Hualei Wang for help with some of the animal experiments.
Footnotes
Published ahead of print on 9 September 2009.
REFERENCES
- 1.Abelseth, M. K. 1964. An attenuated rabies vaccine for domestic animals produced in tissue culture. Can. Vet. J. 5:279-286. [PMC free article] [PubMed] [Google Scholar]
- 2.Andersen, I. H., O. Marker, and A. R. Thomsen. 1991. Breakdown of blood-brain barrier function in the murine lymphocytic choriomeningitis virus infection mediated by virus-specific CD8+ T cells. J. Neuroimmunol. 31:155-163. [DOI] [PubMed] [Google Scholar]
- 3.Asensio, V. C., and I. L. Campbell. 1997. Chemokine gene expression in the brains of mice with lymphocytic choriomeningitis. J. Virol. 71:7832-7840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bukreyev, A., I. M. Belyakov, G. A. Prince, K. C. Yim, K. K. Harris, J. A. Berzofsky, and P. L. Collins. 2005. Expression of interleukin-4 by recombinant respiratory syncytial virus is associated with accelerated inflammation and a nonfunctional cytotoxic T-lymphocyte response following primary infection but not following challenge with wild-type virus. J. Virol. 79:9515-9526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dietzschold, B., C. E. Rupprecht, Z. F. Fu, and H. Koproski. 1996. Rhabdoviruses, p. 1137-1159. In D. M. Knipe, P. M. Howley, et al. (ed.), Field's virology, 3rd ed. Raven Press, Philadelphia, PA.
- 6.Dufour, J. H., M. Dziejman, M. T. Liu, J. H. Leung, T. E. Lane, and A. D. Luster. 2002. IFN-gamma-inducible protein 10 (IP-10; CXCL10)-deficient mice reveal a role for IP-10 in effector T cell generation and trafficking. J. Immunol. 168:3195-3204. [DOI] [PubMed] [Google Scholar]
- 7.Faber, M., M. Bette, M. A. Preuss, R. Pulmanausahakul, J. Rehnelt, M. J. Schnell, B. Dietzschold, and E. Weihe. 2005. Overexpression of tumor necrosis factor alpha by a recombinant rabies virus attenuates replication in neurons and prevents lethal infection in mice. J. Virol. 79:15405-15416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Faber, M., R. Pulmanausahakul, S. S. Hodawadekar, S. Spitsin, J. P. McGettigan, M. J. Schnell, and B. Dietzschold. 2002. Overexpression of the rabies virus glycoprotein results in enhancement of apoptosis and antiviral immune response. J. Virol. 76:3374-3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fabis, M. J., T. W. Phares, R. B. Kean, H. Koprowski, and D. C. Hooper. 2008. Blood-brain barrier changes and cell invasion differ between therapeutic immune clearance of neurotrophic virus and CNS autoimmunity. Proc. Natl. Acad. Sci. USA 105:15511-15516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fenje, P. 1960. Propagation of rabies virus in cultures of hamster kidney cells. Can. J. Microbiol. 6:479-484. [DOI] [PubMed] [Google Scholar]
- 11.Fife, B. T., K. J. Kennedy, M. C. Paniagua, N. W. Lukacs, S. L. Kunkel, A. D. Luster, and W. J. Karpus. 2001. CXCL10 (IFN-gamma-inducible protein-10) control of encephalitogenic CD4+ T cell accumulation in the central nervous system during experimental autoimmune encephalomyelitis. J. Immunol. 166:7617-7624. [DOI] [PubMed] [Google Scholar]
- 12.Fu, Z. F. 1997. Rabies and rabies research: past, present and future. Vaccine 15(Suppl.):S20-S24. [DOI] [PubMed] [Google Scholar]
- 13.Fu, Z. F., E. Weihe, Y. M. Zheng, M. K. Schafer, H. Sheng, S. Corisdeo, F. J. Rauscher III, H. Koprowski, and B. Dietzschold. 1993. Differential effects of rabies and borna disease viruses on immediate-early- and late-response gene expression in brain tissues. J. Virol. 67:6674-6681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glabinski, A. R., M. Tani, S. Aras, M. H. Stoler, V. K. Tuohy, and R. M. Ransohoff. 1995. Regulation and function of central nervous system chemokines. Int. J. Dev. Neurosci. 13:153-165. [DOI] [PubMed] [Google Scholar]
- 15.Glass, W. G., H. F. Rosenberg, and P. M. Murphy. 2003. Chemokine regulation of inflammation during acute viral infection. Curr. Opin. Allergy Clin. Immunol. 3:467-473. [DOI] [PubMed] [Google Scholar]
- 16.Hoffman, L. M., B. T. Fife, W. S. Begolka, S. D. Miller, and W. J. Karpus. 1999. Central nervous system chemokine expression during Theiler's virus-induced demyelinating disease. J. Neurovirol. 5:635-642. [DOI] [PubMed] [Google Scholar]
- 17.Hooper, D. C., R. B. Kean, G. S. Scott, S. V. Spitsin, T. Mikheeva, K. Morimoto, M. Bette, A. M. Rohrenbeck, B. Dietzschold, and E. Weihe. 2001. The central nervous system inflammatory response to neurotropic virus infection is peroxynitrite dependent. J. Immunol. 167:3470-3477. [DOI] [PubMed] [Google Scholar]
- 18.Inoue, K., Y. Shoji, I. Kurane, T. Iijima, T. Sakai, and K. Morimoto. 2003. An improved method for recovering rabies virus from cloned cDNA. J. Virol. Methods 107:229-236. [DOI] [PubMed] [Google Scholar]
- 19.Jackson, R. J., A. J. Ramsay, C. D. Christensen, S. Beaton, D. F. Hall, and I. A. Ramshaw. 2001. Expression of mouse interleukin-4 by a recombinant ectromelia virus suppresses cytolytic lymphocyte responses and overcomes genetic resistance to mousepox. J. Virol. 75:1205-1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson, N., C. S. McKimmie, K. L. Mansfield, P. R. Wakeley, S. M. Brookes, J. K. Fazakerley, and A. R. Fooks. 2006. Lyssavirus infection activates interferon gene expression in the brain. J. Gen. Virol. 87:2663-2667. [DOI] [PubMed] [Google Scholar]
- 21.Kean, R. B., S. V. Spitsin, T. Mikheeva, G. S. Scott, and D. C. Hooper. 2000. The peroxynitrite scavenger uric acid prevents inflammatory cell invasion into the central nervous system in experimental allergic encephalomyelitis through maintenance of blood-central nervous system barrier integrity. J. Immunol. 165:6511-6518. [DOI] [PubMed] [Google Scholar]
- 22.Klein, R. S., E. Lin, B. Zhang, A. D. Luster, J. Tollett, M. A. Samuel, M. Engle, and M. S. Diamond. 2005. Neuronal CXCL10 directs CD8+ T-cell recruitment and control of West Nile virus encephalitis. J. Virol. 79:11457-11466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuang, Y., S. N. Lackay, L. Zhao, and Z. F. Fu. 2009. Role of chemokines in the enhancement of BBB permeability and inflammatory infiltration after rabies virus infection. Virus Res. 144:18-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lane, T. E., M. T. Liu, B. P. Chen, V. C. Asensio, R. M. Samawi, A. D. Paoletti, I. L. Campbell, S. L. Kunkel, H. S. Fox, and M. J. Buchmeier. 2000. A central role for CD4+ T cells and RANTES in virus-induced central nervous system inflammation and demyelination. J. Virol. 74:1415-1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu, M. T., B. P. Chen, P. Oertel, M. J. Buchmeier, D. Armstrong, T. A. Hamilton, and T. E. Lane. 2000. The T cell chemoattractant IFN-inducible protein 10 is essential in host defense against viral-induced neurologic disease. J. Immunol. 165:2327-2330. [DOI] [PubMed] [Google Scholar]
- 26.Martinez, L. 2000. Global infectious disease surveillance. Int. J. Infect. Dis. 4:222-228. [DOI] [PubMed] [Google Scholar]
- 27.Maurer, M., and E. von Stebut. 2004. Macrophage inflammatory protein-1. Int. J. Biochem. Cell Biol. 36:1882-1886. [DOI] [PubMed] [Google Scholar]
- 28.McGettigan, J. P., H. D. Foley, I. M. Belyakov, J. A. Berzofsky, R. J. Pomerantz, and M. J. Schnell. 2001. Rabies virus-based vectors expressing human immunodeficiency virus type 1 (HIV-1) envelope protein induce a strong, cross-reactive cytotoxic T-lymphocyte response against envelope proteins from different HIV-1 isolates. J. Virol. 75:4430-4434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McGettigan, J. P., M. L. Koser, P. M. McKenna, M. E. Smith, J. M. Marvin, L. C. Eisenlohr, B. Dietzschold, and M. J. Schnell. 2006. Enhanced humoral HIV-1-specific immune responses generated from recombinant rhabdoviral-based vaccine vectors co-expressing HIV-1 proteins and IL-2. Virology 344:363-377. [DOI] [PubMed] [Google Scholar]
- 30.Melchjorsen, J., L. N. Sorensen, and S. R. Paludan. 2003. Expression and function of chemokines during viral infections: from molecular mechanisms to in vivo function. J. Leukoc. Biol. 74:331-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miyamoto, K., and S. Matsumoto. 1967. Comparative studies between pathogenesis of street and fixed rabies infection. J. Exp. Med. 125:447-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murphy, F. A. 1977. Rabies pathogenesis. Arch. Virol. 54:279-297. [DOI] [PubMed] [Google Scholar]
- 33.Nakamichi, K., S. Inoue, T. Takasaki, K. Morimoto, and I. Kurane. 2004. Rabies virus stimulates nitric oxide production and CXC chemokine ligand 10 expression in macrophages through activation of extracellular signal-regulated kinases 1 and 2. J. Virol. 78:9376-9388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nakayama, T., J. Shirane, K. Hieshima, M. Shibano, M. Watanabe, Z. Jin, D. Nagakubo, T. Saito, Y. Shimomura, and O. Yoshie. 2006. Novel antiviral activity of chemokines. Virology 350:484-492. [DOI] [PubMed] [Google Scholar]
- 35.Phares, T. W., M. J. Fabis, C. M. Brimer, R. B. Kean, and D. C. Hooper. 2007. A peroxynitrite-dependent pathway is responsible for blood-brain barrier permeability changes during a central nervous system inflammatory response: TNF-alpha is neither necessary nor sufficient. J. Immunol. 178:7334-7343. [DOI] [PubMed] [Google Scholar]
- 36.Phares, T. W., R. B. Kean, T. Mikheeva, and D. C. Hooper. 2006. Regional differences in blood-brain barrier permeability changes and inflammation in the apathogenic clearance of virus from the central nervous system. J. Immunol. 176:7666-7675. [DOI] [PubMed] [Google Scholar]
- 37.Prehaud, C., F. Megret, M. Lafage, and M. Lafon. 2005. Virus infection switches TLR-3-positive human neurons to become strong producers of beta interferon. J. Virol. 79:12893-128904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pulmanausahakul, R., M. Faber, K. Morimoto, S. Spitsin, E. Weihe, D. C. Hooper, M. J. Schnell, and B. Dietzschold. 2001. Overexpression of cytochrome C by a recombinant rabies virus attenuates pathogenicity and enhances antiviral immunity. J. Virol. 75:10800-10807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rock, R. B., G. Gekker, S. Hu, W. S. Sheng, M. Cheeran, J. R. Lokensgard, and P. K. Peterson. 2004. Role of microglia in central nervous system infections. Clin. Microbiol. Rev. 17:942-964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roy, A., and D. C. Hooper. 2007. Lethal silver-haired bat rabies virus infection can be prevented by opening the blood-brain barrier. J. Virol. 81:7993-7998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roy, A., T. W. Phares, H. Koprowski, and D. C. Hooper. 2007. Failure to open the blood-brain barrier and deliver immune effectors to central nervous system tissues leads to the lethal outcome of silver-haired bat rabies virus infection. J. Virol. 81:1110-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sarmento, L., X. Q. Li, E. Howerth, A. C. Jackson, and Z. F. Fu. 2005. Glycoprotein-mediated induction of apoptosis limits the spread of attenuated rabies viruses in the central nervous system of mice. J. Neurovirol. 11:571-581. [DOI] [PubMed] [Google Scholar]
- 43.Schall, T. J., K. Bacon, K. J. Toy, and D. V. Goeddel. 1990. Selective attraction of monocytes and T lymphocytes of the memory phenotype by cytokine RANTES. Nature 347:669-671. [DOI] [PubMed] [Google Scholar]
- 44.Sharma, D. P., A. J. Ramsay, D. J. Maguire, M. S. Rolph, and I. A. Ramshaw. 1996. Interleukin-4 mediates down regulation of antiviral cytokine expression and cytotoxic T-lymphocyte responses and exacerbates vaccinia virus infection in vivo. J. Virol. 70:7103-7107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Siler, C. A., J. P. McGettigan, B. Dietzschold, S. K. Herrine, J. Dubuisson, R. J. Pomerantz, and M. J. Schnell. 2002. Live and killed rhabdovirus-based vectors as potential hepatitis C vaccines. Virology 292:24-34. [DOI] [PubMed] [Google Scholar]
- 46.Silver, N. C., C. D. Good, M. P. Sormani, D. G. MacManus, A. J. Thompson, M. Filippi, and D. H. Miller. 2001. A modified protocol to improve the detection of enhancing brain and spinal cord lesions in multiple sclerosis. J. Neurol. 248:215-224. [DOI] [PubMed] [Google Scholar]
- 47.Takayama-Ito, M., K. Inoue, Y. Shoji, S. Inoue, T. Iijima, T. Sakai, I. Kurane, and K. Morimoto. 2006. A highly attenuated rabies virus HEP-Flury strain reverts to virulent by single amino acid substitution to arginine at position 333 in glycoprotein. Virus Res. 119:208-215. [DOI] [PubMed] [Google Scholar]
- 48.Taub, D. D., A. R. Lloyd, K. Conlon, J. M. Wang, J. R. Ortaldo, A. Harada, K. Matsushima, D. J. Kelvin, and J. J. Oppenheim. 1993. Recombinant human interferon-inducible protein 10 is a chemoattractant for human monocytes and T lymphocytes and promotes T cell adhesion to endothelial cells. J. Exp. Med. 177:1809-1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Trout, J. J., H. Koenig, A. D. Goldstone, and C. Y. Lu. 1986. Blood-brain barrier breakdown by cold injury. Polyamine signals mediate acute stimulation of endocytosis, vesicular transport, and microvillus formation in rat cerebral capillaries. Lab. Investig. 55:622-631. [PubMed] [Google Scholar]
- 50.Ubogu, E. E., M. B. Cossoy, and R. M. Ransohoff. 2006. The expression and function of chemokines involved in CNS inflammation. Trends Pharmacol. Sci. 27:48-55. [DOI] [PubMed] [Google Scholar]
- 51.Walsh, K. B., M. B. Lodoen, R. A. Edwards, L. L. Lanier, and T. E. Lane. 2008. Evidence for differential roles for NKG2D receptor signaling in innate host defense against coronavirus-induced neurological and liver disease. J. Virol. 82:3021-3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang, Z. W., L. Sarmento, Y. Wang, X. Q. Li, V. Dhingra, T. Tseggai, B. Jiang, and Z. F. Fu. 2005. Attenuated rabies virus activates, while pathogenic rabies virus evades, the host innate immune responses in the central nervous system. J. Virol. 79:12554-12565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.World Health Organization. 1992. WHO Expert Committee on Rabies (Eighth Report). Technical Report Series 824. World Health Organization, Geneva, Switzerland. [PubMed]
- 54.Yan, X., M. Prosniak, M. T. Curtis, M. L. Weiss, M. Faber, B. Dietzschold, and Z. F. Fu. 2001. Silver-haired bat rabies virus variant does not induce apoptosis in the brain of experimentally infected mice. J. Neurovirol. 7:518-527. [DOI] [PubMed] [Google Scholar]
- 55.Zlotnik, A., and O. Yoshie. 2000. Chemokines: a new classification system and their role in immunity. Immunity 12:121-127. [DOI] [PubMed] [Google Scholar]