Abstract
During limb lengthening over an intramedullary nail, decisions regarding external fixator removal and weightbearing depend on the amount of callus seen at the lengthening area on radiographs. However, this method is subjective and objective evaluation of the amount of callus likely would minimize nail or interlocking screw breakage and refracture after fixator removal. We asked how many cortices with full corticalization of the newly formed bone at the lengthening area are needed to allow fixator removal and full weightbearing and how to radiographically determine the stage of corticalization. We retrospectively reviewed 17 patients (34 lengthenings) who underwent bilateral tibial lengthenings over an intramedullary nail. The average gain in length was 7.2 ± 3.4 cm. We determined the pixel value ratio (ratio of pixel value of regenerate versus the mean pixel value of adjacent bone) of the lengthened area on radiographs. There were no nail or screw breakage and refracture. Partial weightbearing with crutches was permitted when the pixel value ratio was 1 in two cortices and full weightbearing without crutches was permitted when the pixel value ratio was 1 in three cortices. The pixel value ratio on radiographs can be an objective parameter for callus measurement and may provide guidelines for the timing of external fixator removal. We cannot determine from our limited data the minimum pixel value in how many cortices would suggest safe removal, but we can say our criteria were not associated with subsequent refracture.
Introduction
Distraction osteogenesis with an external fixator has become the standard method in the management of limb lengthening procedures [1, 4, 5, 18]. However, this method is typically time-consuming and inconvenient or even uncomfortable for the patient, with complications such as pin tract infections and stiffness of the knee [19]. The technique of lengthening over an intramedullary nail reduces the external fixation time and seemingly provides better comfort for patients [20].
During limb lengthening over an intramedullary nail, surgeons must make decisions regarding the distraction rate, fixator removal, and weightbearing. These decisions currently involve qualitative assessment of the callus seen on serial radiographs [28]. Radiographic analysis of the callus feature type is useful for recording, summarizing, and monitoring the healing process [2].
Some studies suggest making the decision [21, 22] to increase weightbearing according to the number of matured cortices at the periphery of the newly formed bone seen on the radiographs: recommending patients remain partial weightbearing with two crutches until the newly formed bone has two mature cortices; full weightbearing without crutches was recommended when two intact cortices are seen on the radiographs, but this assessment is subjective and ill-defined. Previous studies report an increased screw or nail breakage rate of 10% [11] to 33% [13] when the tibia was lengthened with an interlocking nail; these complications require additional surgeries and would best be avoided. Traditional radiographic techniques allow qualitative assessment of new bone formation, but that has never been properly quantified [6, 17]. Quantitative methods include quantitative computed tomography (CT) [23, 24], quantitative technetium scintigraphy [17], and dual-energy xray absorptiometry (DEXA) [7, 8]. These methods measure callus mineralization, which correlates with the callus stiffness [16], but these investigations are expensive and the patient must undergo additional imaging [4]. A technique using pixel value on digital radiographs [10, 25] was shown to be an economical method for measuring the serial changes in callus mineralization in different cortices of the callus to ascertain the callus stiffness to provide objective parameters for decision making.
We therefore asked whether the pixel value ratio (ratio of pixel value of regenerate versus the mean pixel value of adjacent bone) on radiographs could be used as an objective parameter of corticalization and provide guidelines for fixator removal and full weightbearing.
Materials and Methods
We retrospectively reviewed 17 patients who underwent bilateral tibial lengthenings over an intramedullary nail to increase height between 2004 and 2006. All patients had a height less than the third percentile for age and gender, with no history of medical illness, bone infection, tumors, fracture, or soft tissue compromise. The average age of the patients at the time of surgery was 22.9 years (range, 18–35 years). Thirteen patients were male and four were female. We excluded two patients who had an intramedullary infection after bilateral tibial lengthening. Before being selected as a candidate for lengthening, we explained the nature of the procedure, duration of treatment, and complications or risks related to surgery to the patients. All patients were highly motivated and fully informed about the procedure and possible complications. The minimum duration of followup was 2 years (average, 2.8 years; range, 2–4.5 years). No patients were lost to followup.
All patients were operated on by a senior author (HRS). Our technique was similar to that described by Herzenberg et al. [20], and AO tibial interlocking nails and Ilizarov external fixators were used. Three rings were used for distraction. Two proximal wires and one proximal half-pin were inserted and fixed at the proximal ring. Two distal wires and one distal half-pin were inserted and fixed at the distal ring. The middle ring had no half-pin and wire.
Patients underwent supervised daily physiotherapy including active and passive range of motion of the knee and ankle beginning 2 days after surgery. Physiotherapy was performed twice per day for 2 hours during 2 weeks of admission and 1 hour per day after discharge until the end of the distraction phase. Daily walking at least 4 hours with partial weightbearing with two crutches was allowed during the distraction phase. Distraction was started 7 days postoperatively at a rate of 0.25 mm four times a day until the desired length was achieved. The average gain in length was 7.2 ± 3.4 cm.
We adjusted the rate of distraction with or without compression and distraction during the distraction period according to one of three types of callus pathways seen radiographically using the classification of Li et al. [15]: homogeneous, heterogeneous, or lucent (Figs. 1 and 2). In the homogenous pathway, distraction rates were 1 mm per day when the callus had a cylindrical shape and 1.5 mm or 2 mm per day when the callus showed a fusiform shape to avoid premature consolidation. In the heterogeneous pathway, we adjusted the rate of distraction, starting at 0.5 mm per day for 2 weeks and then gradually increasing to 1 mm per day when new bone formation was seen on the radiographs. In the lucent pathway, we gave gradual compression until disappearance of the radiolucent gap. After 1 week, we began the distraction at 0.5 mm per day until the segment attained the adequate amount of lengthening compared with the opposite segment, and we delayed fixator removal because pixel value ratios did not reach 1 in two cortices until 40 weeks.
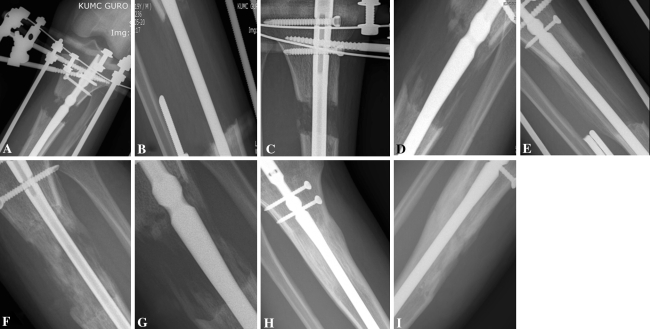
Fig. 1A–I.
The radiographs show (A) Type 1, a sparse low-density callus; (B) Type 2, an homogeneous low-density callus; (C) Type 3, an heterogeneous low-density callus; (D) Type 4, a lucent low-density callus; (E) Type 6, an homogeneous intermediate-density callus; (F) Type 7, an heterogeneous intermediate-density callus; (G) Type 8, a lucent intermediate-density callus; (H) Type 9, an homogeneous normal-density callus; and (I) Type 10, an heterogeneous normal-density callus.
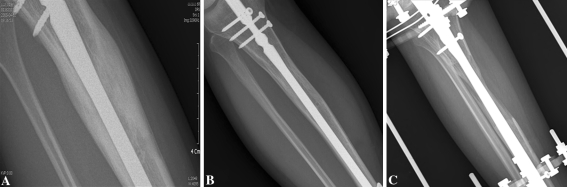
Fig. 2A–C.
The radiographs show (A) homogeneous (B) heterogeneous, and (C) lucent patterns of callus.
Three of us (KPV, QF, HRS) evaluated all patients clinically and radiographically every week during the distraction phase and every 4 weeks during the consolidation phase. During visits, patients were examined for any signs of pin tract infection, and range of motion of adjoining joints was assessed. After the desired limb length was achieved, we inserted distal locking screws and the external fixator was removed before or after the pixel value ratio was 1 in two cortices. The patients were permitted partial weightbearing with crutches when the pixel value ratio reached 1 in two cortices and full weightbearing without crutches when the pixel value ratio reached 1 in three cortices.
All radiographs were taken using StarPACS PiView Star 5.0.6.0 software (INFINITT Co, Ltd, Seoul, Korea) with xray beams parallel to the Ilizarov ring nearest the distraction site to minimize the chance of metal at the site of interest [29]. All radiographs were analyzed retrospectively by three observers (KPV, QF, HRS). Interobserver variability for each pair of observers was determined using the kappa value. The values for the pairs of observers were 0.54, 0.54, and 0.42 for classifying the pathway.
We measured the pixel value on digital radiographs using the region of interest programmer of StarPACS PiView Star 5.0.6.0 software (INFINITT Co) (Fig. 3). The pixel value was calculated on anteroposterior and lateral views. The areas of the regenerate proximal and distal bony fragments were divided into anterior, posterior, medial, and lateral areas, which were between the outer margins of the nail and cortices. The pixel value ratio of the regenerate then was calculated using the following formula: pixel value ratio = [(pixel value of the proximal segment + pixel value of the distal segment)/2]/pixel value of the regenerate. The stage of corticalization was decided by pixel value ratio. A pixel value ratio of 1 indicated corticalization of the regenerate in the lengthening area was comparable to that of the adjacent bone. Less than 1 meant lesser maturation of the regenerate. Three surgeons (KPV, QF, HRS) measured the pixel value ratio to test interobserver and intraobserver variability. Each surgeon reviewed the radiographs twice within a 3-week interval. Intraobserver and interobserver variability for the pixel values ratios were determined using Pearson correlation coefficients. The correlations for intraobserver measures were 0.91, 0.90, and 0.88; the mean Pearson correlation coefficient was 0.90. The correlations for interobserver measures for each pair of observers ranged from 0.80 to 0.92 during the first and second readings.
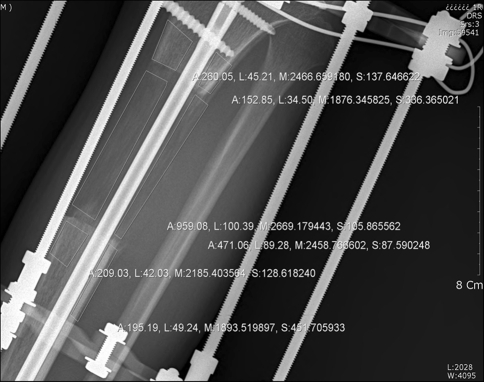
Fig. 3.
The pixel values measured on a digital radiograph are shown. The different cortices of callus and the proximal and distal segments of bone were measured using the free region of interest programmer of StarPACS PiView Star 5.0.6.0 software (INFINITT Co).
Results
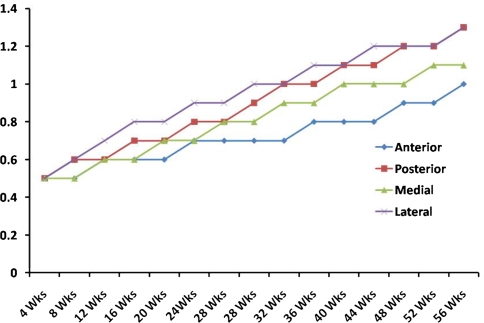
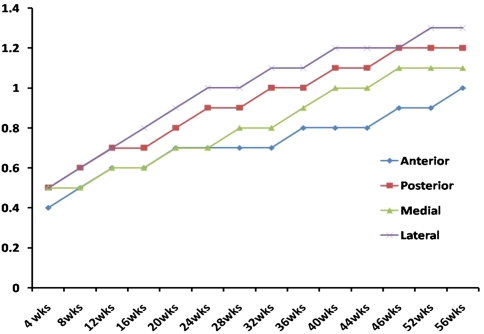
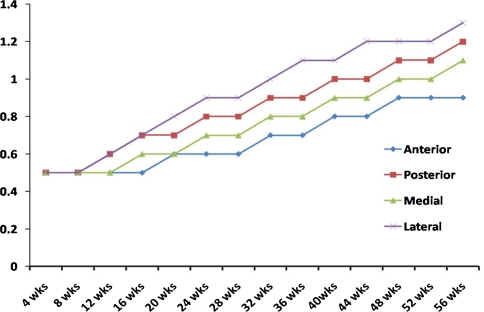
The pixel value ratio increased progressively during the period of consolidation, more so in lateral and posterior cortices and less so in anterior and medial cortices. A pixel value ratio of 1 (mineral density of the callus is the same as that of the bone in the proximal and distal segments) was reached by 28 weeks in lateral cortices, by 32 weeks in posterior cortices, by 44 weeks in medial cortices, and after 56 weeks in anterior cortices (Fig. 4). The homogeneous and heterogeneous callus pathways showed a pixel value ratio of 1 in two cortices by 32 weeks and in three cortices by 40 weeks (Fig. 5). However, it was delayed in the lucent callus pathway, with a pixel value ratio of 1 in two cortices by 40 weeks and in three cortices by 48 weeks (Fig. 6).
Fig. 4.
A graph shows the pixel value ratio in different cortices of the callus during different periods of healing. The pixel value ratio is less in anterior and medial cortices and more in posterior and lateral cortices.
Fig. 5.
A graph shows a pixel value ratio of 1 in two cortices by 32 weeks and in three cortices by 40 weeks in different cortices of the callus in the homogeneous and heterogeneous callus groups during different periods of healing.
Fig. 6.
A graph shows a pixel value ratio of 1 in two cortices by 40 weeks and in three cortices by 48 weeks in different cortices of the callus in the lucent callus group during different periods of healing.
There were no complications such as regenerate refracture or screw breakage in patients who began partial weightbearing with crutches when the pixel value ratio was 1 in two cortices and full weightbearing without crutches when the pixel value ratio was 1 in three cortices.
Discussion
During limb lengthening over an intramedullary nail, decisions regarding external fixator removal and weightbearing depend on the amount of callus at the lengthening area seen on radiographs. However, this method is subjective and objective evaluation of callus amount is necessary to prevent nail or interlocking screw breakage and refracture after fixator removal. We asked whether the pixel value ratio on radiographs could be used as an objective parameter of corticalization and provide guidelines for fixator removal and full weightbearing.
We note several limitations. First, a disadvantage of our technique is that measurement of pixel value is affected by the presence of metal in the vicinity of the point of interest. To avoid this problem, we followed the guidelines proposed by Young et al. [29]. We aligned the xray beam parallel to the plane of the ring nearest the distraction site. Second, we measured the callus stiffness indirectly by measuring the pixel value ratio of the regenerate. Because of indirect measurement, we cannot determine from our limited data the minimum pixel value in how many cortices would suggest safe removal, and our study had inadequate power to discern safety between the three types of callus pathways. Lauterburg et al. [14] assessed bony stability by direct measurement of the compressive stability of the regenerate using a force transducer with a strain gauge. However, additional study is required to evaluate the correlation between pixel value of the callus and real callus stiffness using a force transducer.
After lengthening, the decisions regarding timing of external fixator removal and full weightbearing are important to avoid complications such as nail or screw breakage and refracture. Paley [19] suggested partial weightbearing with two crutches until the callus bridging was visible at two cortices and full weightbearing without crutches when there were two intact cortices seen on radiographs after femoral lengthening over an intramedullary nail. He reported one nail and one screw breakage in two of 32 femoral segments. Kristiansen and Steen [13] reported fatigue fracture of the nail or screws in three of nine tibial segments after tibial lengthening over a nail. They allowed full weightbearing 2 weeks after fixator removal. Kocaoglu et al. [11] reported one screw bending and one screw breakage in 35 femoral segments after lengthening over a nail. They allowed toe-touch walking with two crutches after removal of the fixator and increased the amount of weightbearing depending on the quality of the callus. Full weightbearing was allowed after regeneration of at least three cortices at the lengthening area was seen on the radiographs. In these studies, the definition of corticalization was unclear and subjective. The width or shape or density of cortical bone seen on radiographs may be different between patients. The cortex with narrower width and normal density cortex may have the same strength as that with wider width and low or intermediate density. Without an objective measurement method, intraobserver or interobserver error may be high in subjective measurements using radiographs. Measurement of mineralization of the cortex with DEXA or CT can be an objective method because quantitative assessment is possible. However, these methods are expensive and inconvenient.
Recently, the picture archiving communication system (PACS) has become popular and measurement of pixel value ratio can be an objective method for evaluation of mineralization of the cortex at the lengthening area seen on radiographs because it is quantitative assessment. In a previous study [10], good correlation was observed between bone mineral density measured with DEXA and pixel value ratio, with a Pearson’s coefficient of correlation of 0.79. This result suggested the pixel value ratio on standard radiographs might represent mineralization of the callus and could be used instead of DEXA. The proportional relationship among the mineral content, radiographic presentation, and mechanical features of bone has been reported in other studies [3, 9, 27].
We found anterior and medial cortices showed a lower pixel value ratio compared with the posterior and lateral sides. This is the result of less soft tissue coverage and injury to the periosteum during corticotomy and bone healing requiring the presence of periosteum and soft tissue coverage [12]. To set objective guidelines for weightbearing, we retrospectively analyzed all cases of limb lengthening over intramedullary nail performed at our institute. We found the cases with bone regenerate fracture [26] had a pixel value ratio less than 0.8, and we observed no instance of regenerate fracture in patients in whom the pixel value ratio was 1 or greater in a minimum of two cortices of callus at the time of weightbearing. We applied this criterion prospectively and observed no regenerate fracture or screw breakage in patients who began full weightbearing with two crutches when the pixel value ratio was 1 in two cortices and full weightbearing without crutches when the pixel value ratio was 1 in three cortices. The homogeneous and heterogeneous callus groups had a pixel value ratio of 1 in two cortices by 32 weeks and in three cortices by 40 weeks. However, it was delayed in the lucent callus group (pixel value ratio of 1 in two cortices by 40 weeks and in three cortices by 48 weeks), in which case we delayed full weightbearing to prevent stress on the screws and their breakage [13].
Most authors consider it is reasonable to remove a lengthening fixator without a nail when three cortices are formed; there are few refractures even though the assessment of the cortices is not entirely objective or reproducible. In lengthening over a nail, two cortices with a pixel value ratio of 1 at the lengthening area may not produce callus or metal breakage during full weightbearing because the nail can support weight with the same strength as an intact cortical bone. However, this presumption should be confirmed by additional studies. Our data suggest three corticalizations with a pixel value ratio of 1 could allow full weightbearing after fixator removal without complications, and a pixel value ratio can be used as an objective guideline to define corticalization. However, we emphasize ours is a pilot study with a small number of cases with a specific loading regime.
Footnotes
This study was supported by a grant from the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare and Family Affairs, Republic of Korea (A080588).
Each author certifies that his or her institute has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This study was performed at Korea University School of Medicine.
References
- 1.Aquerreta JD, Forriol F, Canadell J. Complications of bone lengthening. Int Orthop. 1994;18:299–303. [DOI] [PubMed]
- 2.Catagni M. Imaging techniques: the radiographic classification of bone regenerate during distraction. In: Maiocchi AB, Aronson J, eds. Operative Principles of Ilizarov. London, UK: Williams & Wilkins; 1991;5:53–57.
- 3.Chakkalakal DA, Lippiello L, Wilson RF, Shindell R, Connolly JF. Mineral and matrix contributions to rigidity in fracture healing. J Biomech. 1990;23:425–434. [DOI] [PubMed]
- 4.De Backer AI, Mortele KJ, De Keulenaer BL. Picture archiving and communication system: Part one: filmless radiology and distance radiology. JBR-BTR. 2004;87:234–241. [PubMed]
- 5.De Bastiani G, Aldegheri R, Renzi-Brivio L, Trivella G. Limb lengthening by callus distraction (callotasis). J Pediatr Orthop. 1987;7:129–134. [DOI] [PubMed]
- 6.Donnan LT, Saleh M, Rigby AS, McAndrew A. Radiographic assessment of bone formation in tibia during distraction histiogenesis. J Pediatr Orthop. 2002;22:645–651. [DOI] [PubMed]
- 7.Eyres KS, Bell MJ, Kanis JA. New bone formation during leg lengthening: evaluated by dual energy x-ray absorptiometry. J Bone Joint Surg Br. 1993;75:96–106. [DOI] [PubMed]
- 8.Eyres KS, Bell MJ, Kanis JA. Methods of assessing new bone formation during limb lengthening: ultrasonography, dual energy x-ray absorptiometry and radiography compared. J Bone Joint Surg Br. 1993;75:358–364. [DOI] [PubMed]
- 9.Fischgrund J, Paley D, Suter C. Variables affecting time to bone healing during limb lengthening. Clin Orthop Relat Res. 1994;301:31–37. [PubMed]
- 10.Hazra S, Song HR, Biswal S, Lee SH, Lee SH, Jang KM, Modi HN. Quantitative assessment of mineralization in distraction osteogenesis. Skeletal Radiol. 2008;37:843–847. [DOI] [PubMed]
- 11.Kocaoglu M, Eralp L, Kilicoglu O, Burc H, Cakmak M. Complications encountered during lengthening over an intramedullary nail. J Bone Joint Surg Am. 2004;86:2406–2411. [DOI] [PubMed]
- 12.Kojimoto H, Yasui N, Goto T, Matsuda S, Shimomura Y. Bone lengthening in rabbits by callus distraction: the role of periosteum and endosteum. J Bone Joint Surg Br. 1988;70:543–549. [DOI] [PubMed]
- 13.Kristiansen LP, Steen H. Lengthening of the tibia over an intramedullary nail, using the Ilizarov external fixator: major complications and slow consolidation in 9 lengthenings. Acta Orthop Scand. 1999;70:271–274. [DOI] [PubMed]
- 14.Lauterburg MT, Exner GU, Jacob HA. Forces involved in lower limb lengthening: an in vivo biomechanical study. J Orthop Res. 2006;24:1815–1822. [DOI] [PubMed]
- 15.Li R, Saleh M, Yang L, Coulton L. Radiographic classification of osteogenesis during bone distraction. J Orthop Res. 2006;24:339–347. [DOI] [PubMed]
- 16.Maffulli N, Cheng JC, Sher A, Ng BK, Ng E. Bone mineralization at the callotasis site after completion of lengthening. Bone. 1999;25:333–338. [DOI] [PubMed]
- 17.Minematsu K, Tsuchiya H, Taki J, Tomita K. Blood flow measurement during distraction osteogenesis. Clin Orthop Relat Res. 1998;347:229–235. [DOI] [PubMed]
- 18.Paley D. Current techniques of limb lengthening. J Pediatr Orthop. 1988;8:73–92. [DOI] [PubMed]
- 19.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed]
- 20.Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail: a matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464–1480. [DOI] [PubMed]
- 21.Park HW, Yang KH, Lee KS, Joo SY, Kwak YH, Kim HW. Tibial lengthening over an intramedullary nail with use of the Ilizarov external fixator for idiopathic short stature. J Bone Joint Surg Am. 2008;90:1970–1978. [DOI] [PubMed]
- 22.Powell ES, Lawford PV, Duckworth T, Black MM. Is callus calcium content an indicator of the mechanical strength of healing fractures? An experimental study in rat metatarsals. J Biomed Eng. 1989;11:277–281. [DOI] [PubMed]
- 23.Romanowski CA, Underwood AC, Sprigg A. Reduction of radiation doses in leg lengthening procedures by means of audit and computed tomography scanogram techniques. Br J Radiol. 1994;67:1103–1107. [DOI] [PubMed]
- 24.Salmas MG, Nikiforidis G, Sakellaropoulos G, Kosti P, Lambiris E. Estimation of artifacts induced by the Ilizarov device in quantitative computed tomographic analysis of tibiae. Injury. 1998;29:711–716. [DOI] [PubMed]
- 25.Shim JS, Chung KH, Ahn JM. Value of measuring bone density serial changes on a picture archiving and communication system (PACS) monitor in distraction osteogenesis. Orthopedics. 2002;25:1269–1272. [DOI] [PubMed]
- 26.Song HR, Oh CW, Mattoo R, Park BC, Kim SJ, Park IH, Jeon IH, Ihn CH. Femoral lengthening over an intramedullary nail using the external fixator: risk of infection and knee problems in 22 patients with a follow-up of 2 years or more. Acta Orthop. 2005;76:245–252. [DOI] [PubMed]
- 27.Tselentakis G, Owen PJ, Richardson JB, Kuiper JH, Haddaway MJ, Dwyer JS, Evans GA. Fracture stiffness in callotasis determined by dual-energy x-ray absorptiometry scanning. J Pediatr Orthop B. 2001;10:248–254. [DOI] [PubMed]
- 28.Vade A, Eissenstat R. Radiographic features of bone lengthening procedures. Radiology. 1990;174:531–537. [DOI] [PubMed]
- 29.Young JW, Kovelman H, Resnik CS, Paley D. Radiologic assessment of bones after Ilizarov procedures. Radiology. 1990;177:89–93. [DOI] [PubMed]