Abstract
This Classic Article is a reprint of the original work by Marshall R. Urist, A Morphogenetic Matrix for Differentiation of Bone Tissue. An accompanying biographical sketch of Marshall R. Urist, MD is available at DOI 10.1007/s11999-009-1067-4; a second Classic Article is available at DOI 10.1007/s11999-009-1068-3; and a third Classic Article is available at DOI 10.1007/s11999-009-1069-2. The Classic Article is © 1970 by Springer and is reprinted with permission from Urist MR. A morphogenetic matrix for differentiation of bone tissue. Calc Tiss Res. 1970:4(Suppl);98–101.
The development of bone is multiphasic, proceeding concurrently from deposition of woven bone (histogenesis), to resorption and reformation of an ossicle of lamellar bone filled with bone marrow (morphogenesis). Recent experimental works on differentiation of post-fetal mesenchymal cells of muscle demonstrate the three requirements for bone morphogenesis. The first is the cell intrinsic or genetic blueprints, including competence, a state of unexpressed readiness to synthesize specialized cell products. The second, is an extrinsic or extracellular substratum for cell intercommunications and interactions. The third, is the accessory supply complex which includes all the metabolic, endocrine, nutritional and mineral requirements for building specialized cell products. The first and third requirements are now well defined in the physico-chemical terms in modern textbooks of cell biology. The second, the cell communication or extrinsic system is poorly undefined and usually open to doubt. This lecture will present some new evidence of the existence of local extrinsic requirements of post-fetal mesenchymal cells for bone morphogenesis.
Mesenchymal cells differentiate into bone in the interior of a block of bone matrix implanted in belly of a muscle within a period of 2 to 3 weeks. The reaction occurs almost invariably in mice, rats, guinea pigs and rabbits if the matrix is prepared by decalcification in 6/10 normal HCl at 2°C for not more than 3 or 4 days, and if denaturation and gelatinization of the bone collagen is minimal [1–14]. After rat bone matrix is decalcified, it can be preserved by lyophilization and stored in sterile vials, for at least one year with very little loss of its morphogenetic properties. Within 10 to 15 days after implantation of bone matrix, mesenchymal cells grow in from the surrounding muscle into every available old vascular channel, proliferate, fuse, and become multinucleated cells. Through the action of multinucleated giant cells and some mononucleated forms, the old matrix is resorbed and replaced by reticular cells which appear to be the product of fission of multinucleated cells and perivascular connective tissue cells of sprouting capillaries. These reticular cells can be classified as osteoprogenitor cells because they differentiate into osteoblasts and deposit bone on the walls of excavation chambers in the interior of the implant. In some locations deep in the implant, isolated from sprouting capillaries, mesenchymal cells proliferate, aggregate and differentiate directly into hyaline cartilage. Later the cartilage vascularizes, modulates and produces endochondral deposits of new bone. The earliest deposits consist of woven bone which are remodelled immediately after formation. The remodelling process occurs in two directions, centripetally to replace woven bone with hematopoietic bone marrow and centripetally to replace woven bone with lamellar bone. The process is an example of diverse means to a common end which is, as previously stated, not simply histogenesis but morphogenesis, a process of formation of a spherical ossicle consisting of a cortex and a central medulla filled with bone marrow.
The chemical components of bone matrix responsible for its morphogenetic properties appear to be intimately associated with the interfibrillar cross-links and weave pattern of collagen fibers found in all calcified tissues. Morphogenetic properties are displayed by intramuscular implants of decalcified matrix prepared from enamel, dentin, calcified cartilage, calcified placenta, urinary bladder epithelium. Lathyritic bone, although fully calcified, is poorly cross-linked and readily solubilized and does not possess morphogenetic properties following implantation in muscle. The morphogenetic process is relatively easy to quantitate, because the implanted matrix is ashless, and the yield of new bone is proportional to the quantity of ash following incineration at 300°C. In general, the yield of new bone is proportional to the mass of implanted matrix, but there is a plateau in the quantity of new bone which is determined by the number of mesenchymal cells available for migration and proliferation.
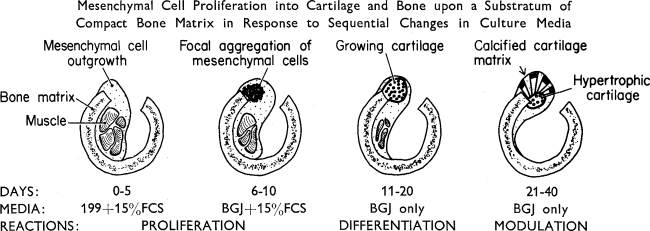
Fig. 1.
Diagramatic illustration of sequence of events, time relationships, and changes in culture media in differentiation of cartilage in response to a morphogenetic matrix in vitro.
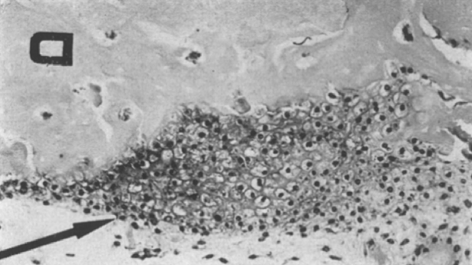
Fig. 2.
Photomicrograph showing new cartilage proliferating on the surface of 0.6 N HCl decalcified bone matrix in BGJ culture medium approximately 20 days after explantation. Hematoxylin eosin and azure II.
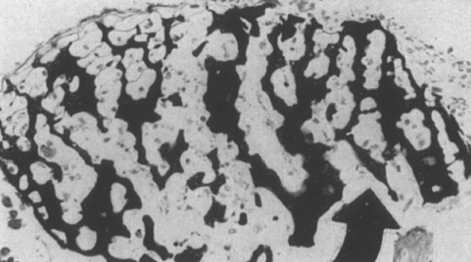
While the proliferation and differentiation of mesenchymal cells is also dependent upon the development of the vascular network for the transport of the accessory metabolic nutritional factors, endothelial cells and intravascular blood elements are not the source of the new cartilage or bone cells. Implants of morphogenetic matrix and minced muscle produce new cartilage and chondroosteoid even in the interior of millipore chambers (pore size, .45μ and a thickness of 125μ) which exclude capillaries. Recently, in collaboration with Nogami [12], we are able to explant small fragments of muscle in the medulla of segments of diaphyseal decalcified bone matrix, and observe differentiation of mesenchymal cells into cartilage in a chemically-defined tissue culture medium within a period of nine days. If the BGJ medium is supplemented with plasma, cartilage cells hypertrophy, modulate and produce endochondral bone. The intercellular matrix of cartilage calcifies and is resorbed in tissue culture without the development of capillary sprouts (Fig. 3). In the absence of the morphogenetic matrix in tissue culture, mesenchymal cells grow out onto the flask in a monolayer and differentiate into fibroblasts and produce only a network of collagen fibrils. Denatured bone matrix similarly produces only fibrous tissue. Thus, a morphogenetic matrix or inductive substratum appears to be an essential requirement of the system. Prior to the use of the above described preparations of bone morphogenetic matrix, tissue culture work on bone was limited to development of embryonic cartilage models, and surviving calvareal bone cells. No bone cell differentiation de novo in tissue culture seems to have been reported previously, presumably because a morphogenetic matrix was unavailable.
Fig. 3.
Photomicrograph showing hypertrophic cartilage developed and calcified in vitro 30 days after explantation of endomysial mesenchymal cells in a cylinder of bone matrix in BGJ culture medium. Hematoxylin eosin and von Kossa stain. Arrowhead indicates direction of ingrowth of mesenchyma.
Undemineralized bone matrix implanted in muscle fails to produce more than a scanty deposit of new bone and never in more than a few percent of trials. Surface-demineralized lyophilized implants also produce small deposits, but the yield is proportional to the mass of the demineralized fraction of the implanted matrix. Particles of demineralized bone matrix produce only a chronic inflammatory and massive giant cell reaction, but pellets of particulate bone mineral produce an encysted ossicle. Deamination or dinitrophenolation of the epsilon-amino groups, irradiation and other physical agents which produce denaturation of the bone collagen destroy the morphogenetic properties of the bone matrix.
Species differences which are presently difficult to explain, are an obstacle to the clinical use of morphogenetic matrix as a substitute for a bone graft. Dogs, monkeys, baboons, and human beings produce much lower yields of new bone than rodents in intramuscular implants of bone matrix; frogs and birds also produce only very small yields of new bone by presently known methods of decalcification of the morphogenetic cross-linked structure of the bone matrix. Dentin matrix, which is highly permeable to demineralizing solutions and more highly cross-linked than bone matrix, produces a high yield of new bone even in dogs. The relationship between the insoluble cross-linked structure, the calcification initiator, and morphogenetic properties of the implanted matrix seems to hold the key to the solution of the problem of osteogenesis as we see it now [11].
Differences in osteogenetic competence, a state of unexpressed readiness of mesenchymal cell population to differentiate into bone cells, indicates that there are no wholly undifferentiated cells in the body. Implants of bone matrix in thyroid, thymus, spleen, liver, and kidney reveal that the mesenchyma of these organs are osteogenetically incompetent. Implants of bone matrix into subcutaneous tissue, brain, spinal cord, i.v. disc, muscle, cartilage bone, bone marrow, tendon and peritoneum and many visceral organ connective tissue capsules display osteogenetic competence [10]. The cardinal question—which physico-chemical component or components of the matrix activate osteogenetic competence, and how the property is transmitted from one mesenchymal cell generation to another—is presently unanswerable. Whatever the morphogenetic property may be, its effects are so rapidly transferred from matrix to mesenchyma that Huggins and associate [3] report a 10-fold rise in tissue alkaline phosphatase activity, measured by accurate methods within 5 days after decalcified dentin is implanted subcutaneously in rats.
Footnotes
Richard A. Brand MD (✉) Clinical Orthopaedics and Related Research, 1600 Spruce Street, Philadelphia, PA 19103, USA e-mail: dick.brand@clinorthop.org
References
- 1.Buring, K., and M. R. Urist: Clin. Orthop. 54, 235—242 (1967). [PubMed]
- 2.Dubuc, F. L., and M. R. Urist: Clin. Orthop. 55, 217—223 (1967). [PubMed]
- 3.Huggins, C. B., and M. R. Urist: In preparation.
- 4.Strates, B. S., and M. R. Urist: Clin. Orthop. 66, 226—240 (1969). [PubMed]
- 5.Urist, M. R.: Science, 150, 893—899 (1965). [DOI] [PubMed]
- 6.Urist, M. R., et al.: Clin. Orthop. 53, 243—283 (1967). [PubMed]
- 7.Urist, M. R., and T. A. Dowell: Clin. Orthop. 61, 61—71 (1969). 4236465
- 8.Urist, M. R.: Mesenchymal Cell Reactions to inductive Substances for Bone Formation. In, Wound Healing. W. van Winkle, Jr., ed. New York: McGraw-Hill Book Co. 1969.
- 9.Urist, M. R., et al.: Clin. Orthop. 63, 210—221 (1969).
- 10.Urist, M. R., et al.: Clin. Orthop. 64, 194—220 (1969). [PubMed]
- 11.Urist, M. R., and P. L. Craven: Fed. Proceed., In preparation.
- 12.Urist, M. R., and H. Nogami: In preparation.
- 13.vande Putte, K. A., and M. R. Urist: Clin. Orthop. 43, 257—270 (1966).
- 14.Yeomans, J. D., and M. R. Urist: Arch. Oral Biol. 12, 999—1008 (1967). [DOI] [PubMed]