Abstract
Associations of men’s substance use problems–defined as meeting at least one criterion of dependence on each of a number of substances by the mid-20s–and their perpetration of intimate partner violence (IPV) were examined in an at-risk community sample of 150 men in long-term relationships from late adolescence to the late 20s. Men who had a problem with substances other than sedatives (especially cannabis and hallucinogens) committed more IPV than did men without such problems. Most of the men who had a problem with marijuana also had an alcohol problem, explaining why alcohol was found to have only an indirect association with IPV. The failure of previous alcohol-use studies to control for co-occurrence of alcohol and marijuana problems may explain the discrepancy with conclusions from past research that alcohol problems contribute directly to the perpetration of IPV.
Keywords: at-risk sample, substance abuse, intimate partner violence
Substance use frequently has been considered a contributing factor to intimate partner violence (IPV). A study of police visits to domestic violence scenes found that 92% of perpetrators had used alcohol or other drugs on the day of the incident (Brookoff, O’Brien, Cook, Thompson, & Williams, 1997). Furthermore, 40–60% of married or cohabitating patients entering substance-abuse treatment reported at least one episode of IPV in the prior year (reviewed in Fals-Stewart & Kennedy, 2005). The associations of problem use of specific substance with IPV, especially while accounting for polysubstance use, have still not been well established.
Associations of Specific Substances with IPV
It is generally believed that there is a direct contribution of alcohol problems to IPV (Thompson & Kingree, 2006). Mechanism by which substance use may contribute to perpetration of violence include disinhibition associated with intoxication as well as expectations (e.g., Arseneault, Moffitt, Caspi, Taylor, & Silva, 2000; Gelles & Cavanaugh, 2005). In addition, intoxication provides a more socially acceptable reason for violence than admission of aggression when judgment is unaffected by substances (Lennings, Copeland, & Howard, 2003).
Findings regarding the connection of marijuana use and violence have been mixed, with some studies supporting a positive or negative association (e.g., Boles & Miotto, 2003; Friedman, Terras, & Glassman, 2003) and others failing to find a link between the two (Lennings et al., 2003). Amphetamines have mood-altering effects, including irritability, aggression, and paranoid and psychotic states, which can be particularly severe depending on dosage and chronicity of use (see review by Boles & Miotto). Two studies based on related samples of methamphetamine users reported that paranoia and violence, most often in family and acquaintance relationships, were associated with use (Sommers & Baskin, 2006; Sommers, Baskin, & Baskin-Sommers, 2006).
Previously, cocaine use had been found consistently to be associated with violence, including IPV. Boles and Miotto’s (2003) review found similar mood-altering effects and violent states for casual and chronic cocaine users as for amphetamine users. Little research has been done on the contributions of problems with sedatives and hallucinogens to IPV, making examination of the associations of these problems to IPV particularly important.
Role of Antisocial Behavior in Substance Use and IPV
In addition to direct effects of substance use problems on domestic violence, substance use and IPV may also be associated because of individual and contextual factors that underlie both problems. Risk in the family of origin, including factors such as parental transitions (e.g., divorce, repartnering) and poor parenting behavior (e.g., poor parental monitoring), is involved in the etiology of conduct problems or antisocial behavior in childhood and adolescence, and such behavior is a common developmental pathway to numerous problem outcomes (Capaldi & Shortt, 2003). Antisocial behavior predicts both IPV (Capaldi & Clark, 1998) and substance use problems (e.g., Dishion, Capaldi, & Yoerger, 1999), as well as involvement in environments (e.g., associations with antisocial peers) that support both problem behaviors (e.g., Capaldi, Dishion, Stoolmiller, & Yoerger, 2001). Thus, to test the independent role of substance use in engagement in IPV, antisocial behavior should be controlled. However, most studies on this topic do not control for the role of antisocial behavior. There is some evidence that the associations between substance use problems (including alcohol) and IPV may persist when antisocial behavior is controlled (Fals-Stewart, Leonard, & Birchler, 2005). Moreover, if different substances vary in their associations with antisocial behavior, the pattern of the associations of drug problems with IPV could be different after antisocial behavior is held constant.
Substance Dependence versus Substance Problems
The most accepted way to identify a substance-abuse problem, even among community (i.e., nonclinical) samples, is to use a diagnostic clinical interview to determine whether the individual meets the DSM-IV (American Psychiatric Association, 2000) criteria for substance use dependency for each substance class. The DSM-IV requires that three of seven dependence symptoms be observed to warrant a diagnosis of dependency for a particular substance. Unfortunately, with community samples, applying such stringent criteria often results in too few participants classified as having a problem with many substances to allow for examinations of the association of some substance problems with IPV, and this was the case even for the current at-risk sample with relatively high levels of substance use. For example, all but 10 of our participants did not have even a single symptom for dependence on sedatives. However, examining these associations in community samples is of critical importance to understanding the likely role of substance use in IPV.
It is not clear that use of the DSM-IV dependency diagnosis is, in fact, the best approach to studying the association of IPV and substance use problems. Psychometric analyses by Feingold and Rounsaville (1995a, 1995b) have shown that dependence is best conceptualized as a continuous, rather than a dichotomous, outcome and that the DSM-IV dichotomization of dependence symptoms is arbitrary. Their findings were consistent with a wide body of literature on the dependence syndrome construct that provided the theoretical foundation for their work. Therefore, for both practical and methodological reasons, participants in this study were assigned to the problem category if they met a single criterion for dependency for a particular drug. Subsequent analyses examined whether there were associations between number of dependence symptoms and IPV as a function of substance type for those having at least one symptom of dependence for each targeted substance. A difficulty in comparing men who do and do not have a problem with a specific substance is that men who have a problem with one substance also are more likely to have problems with other substances (e.g., Jackson, Sher, & Schulenberg, 2005), thereby confounding the effects of different drugs on IPV. A partial solution to this problem is to supplement analyses based on individual drugs with those using groupings that incorporate problems with multiple substances.
Present Study
The present study contributes to the field by overcoming significant limitations of prior research on the associations between substance use problems and IPV; namely, failures to account for the co-occurrence of use of multiple substance types (i.e., polydrug use) and the well-established associations that antisocial behavior has both with substance use and IPV. In particular, this is the first study to look at the linkage between lifetime drug-problem symptoms at ages 25–26 years and IPV across ages 19–28 years (approximately). A wide range of legal and illicit substances were considered, affording comparisons of the effects of different substances in the same sample. Moreover, this is one of the few studies to employ a community sample. Although positive associations alone cannot prove a causal link between drug problems and IPV (particularly when drug use is not measured prior to IPV commission), the absence of such associations would indicate a lack of a causal effect.
Aspects of IPV examined in this study included aggression (both physical and psychological) displayed by the man toward his partner and the injuries she received as a result of his physical aggression (see Capaldi & Crosby, 1997). Capaldi and Owen (2001) have emphasized that understanding of IPV will be increased by considering violent acts and their impacts (e.g., injuries) separately.
The data were obtained from the Couples Study associated with the Oregon Youth Study (OYS; Capaldi & Clark, 1998), which has followed at-risk men and their current romantic partners every 2 to 4 years from the late teens to the late twenties (Capaldi & Owen, 2001; Kim & Capaldi, 2004). Past research on men in the Couples Study sample has shown that about only about 20% of them committed physical IPV over the previous year, but the mean number of psychological IPV incidences was between two and three (Capaldi & Crosby, 1997).
Although the Couples Study is a longitudinal study, the current research focuses on the between-participants rather than within-participants associations of drug problems with IPV. However, IPV data are averaged over time to afford a more stable measure of the behavior across early adulthood than would be obtained by use of a measure obtained at only one time, as in the case of typical nonlongitudinal studies.
The present study examines the association between IPV and at least one dependency symptom at ages 25–26 years for eight substance classes examined separately: nicotine, alcohol, cannabis, amphetamines, hallucinogens, cocaine, opiates, and sedatives. Differences on IPV among men grouped by substance categories are also examined. Finally, antisocial behavior is controlled in supplemental analyses to determine if significant covariation between substance problems and IPV remains after antisocial behavior is held constant.
Method
Participants
The OYS sampled 206 boys from two cohorts of fourth graders at risk for delinquency who were recruited over 2 consecutive years from schools with a higher incidence of delinquency in the neighborhood of a medium-sized city in the Pacific Northwest. The Couples Study began when the boys reached late adolescence and were participating in Wave 9 of OYS data collection. Each adolescent who had a current romantic female partner was asked to have the partner participate with him in a battery of OYS questionnaire and behavioral assessments created expressly for the Couples Study (in addition to OYS measures administered exclusively to the men). The men who did not participate with a partner in OYS Year 9 (mainly because they did not have a partner at the time) were invited to do so the following year, and those who had not participated with a partner in either Year 9 or Year 10 were asked to bring in a partner for OYS Year 11. Thus, the first time point of the Couples Study (T1) consisted of paired sets of data gathered from a male OYS participant and a female romantic partner in 1 of the 3 years in which he contributed to the annual OYS assessments, and men who did not participate with a partner in any of these three OYS waves were considered “missing” from T1 of the Couples Study.
Time 2 (T2) of the Couples Study began in OYS Year 12 when all OYS men were again requested to participate with current romantic partners. Men who did not participate with a partner in this year had opportunities to bring in a partner to either of the following two OYS annual assessments, and the data from a man and his partner in this next 3-year window constituted T2 of the Couples Study. The same approach was use to collect the data for Time 3, Time 4, and Time 5 (T5), but couples were assessed biannually in these later assessments.
A subsample of 150 of the 206 OYS men who had at least one long-term relationship (defined as those who participated with the same woman in at least 2 of the 5 assessments) was used in the analyses. Because 28 of these men had participated 2 or 3 times with each of 2 women, separate assessments were made of their levels of IPV with each of their 2 partners, and the results were averaged for each OYS man to ensure independence of observations.
Procedure
Assessments used interviews, questionnaires of self- and partner reports of IPV, and also a videotaped problem-solving discussion task to assess psychological aggression manifested in dyadic interaction. (For further description of the discussion task, see Capaldi, Shortt, & Crosby, 2003 and Kim & Capaldi, 2004.)
Measurements
Drug problems
Drug-problem status was first determined by the men’s responses to a psychiatric interview, Version 2.0 of the Composite International Diagnostic Interview (CIDI; World Health Organization, 1997), administered to them at Wave 3, when men were ages 25–26 years. For each of a wide range of substances (including nicotine, cannabis, cocaine, opiates, hallucinogens, sedatives, and amphetamines), the men were evaluated using the criteria for each of the seven drug dependence symptoms that contribute to a lifetime-based diagnosis of substance dependency by DSM-IV for that substance. These responses were used to classify the men’s substance-problem status in the following three ways.
A participant was coded as having a problem with a particular substance if he ever met any of the seven dependence criteria for that drug by Wave 4.
Four dichotomous drug-problem variables were derived from the preceding categorizations as follows: (a) no substance problem versus any substance problem, including only nicotine problems; (b) no psychoactive substance problem (i.e., subsuming nicotine dependence) versus psychoactive substance problem; (c) no illicit substance problem (including dependencies limited to nicotine and alcohol) versus illicit substance problem (dependency on cannabis or hard drugs); and (d) no hard-drug problem (including dependencies limited to nicotine, alcohol, and cannabis) versus hard-drug problem (dependency on at least one of any other substance).
The dichotomous drug-problem variables were used to sort the men into one of four mutually exclusive and exhaustive drug-dependency groups reflecting ascending levels of substance-problem severity on the basis of the nature of the psychoactive (i.e., nicotine excluded) substance abused: (a) no problems, (b) alcohol problem, (c) cannabis problem (with or without an alcohol problem), or (d) hard-drug problem (with or without problems with alcohol and/or cannabis). Within each group, men were dichotomized by the presence or absence of a nicotine problem.
Antisocial behavior
Antisocial behavior was measured by three indicators:
Number of arrests. Lifetime arrest records as of T5 of the Couples Study were available and coded for whether or not they were the result of IPV, with number of IPV arrests subtracted from the total number of arrests, M = 5.2, SD = 7.5. Because outliers on this measure were observed (i.e., a few men had an atypically large number of arrests), the numbers of non-IPV arrests were converted to z scores, and z values greater than 3.0 were set equal to 3.0.
Interviewer ratings. Interviewers made three ratings of men’s antisocial behaviors (e.g., “He seemed antisocial, delinquent”) at each assessment, which were summed to yield an interviewer rating score. The interviewer ratings were then averaged across the time points to form a cross-time measure of interviewer rating of antisocial behavior. Alphas for this scale, successfully used in prior research, were previously reported to be .66 (Kim & Capaldi, 2004).
Lifetime diagnosis for antisocial personality disorder. A lifetime diagnosis of antisocial personality disorder (no = 0, yes = 1) was assessed from the DIS-IV (Washington University, 1998) when the men were ages 25–26 years, and it was found that 17% of the men met the criterion for diagnosis.
Intimate partner violence
IPV was measured by six variables assessing physical aggression, psychological aggression, and injuries through self-reports, partner reports, interviewer ratings, and behavioral assessments.
APQ-Physical Aggression. Reported physical aggression was assessed with the Adjustment with Partner Questionnaire (APQ; Kessler, 1990). The men rated their physical aggression toward the partner with whom they were participating at that wave (alphas = .69–.70; Kim & Capaldi, 2004), and their partner concurrently rated the men’s physical aggression toward them (alphas = .78–.83; Kim & Capaldi). Because the self- and partner reports (each based on two items, “When disagree, how often do you push, grab, shove, throw something at partner, slap, or hit?”) were highly correlated, r = .53, they were combined to yield the time-varying APQ-Physical Aggression measure used in multilevel analyses. These scores were then averaged over time.
APQ-Psychological Aggression. Reported psychological aggression was assessed at each wave. The men rated their psychological aggression toward the partner with whom they were participating at the wave (alphas = .78–.80; Kim & Capaldi, 2004), and their partner concurrently rated the men’s psychological aggression toward them (alphas = .87–.89; Kim & Capaldi). Because the self- and partner reports (each based on two items, e.g., “When disagree, how often do you insult or swear, sulk or refuse to talk, stomp out of the room, threaten to hit?”) were highly correlated, r = .52, they were combined to yield the time-varying APQ-Psychological Aggression measure used in multilevel analyses. The scores were averaged over times.
Observed-Psychological Aggression. A coded score of psychological aggression was obtained via observation of the men's behavior toward their partners during a problem-solving discussion task. These video recordings were quantified with a Family Peer and Process Code that examined rate per minute of negative interpersonal, verbal attack, and coercive behavior. For further description of the observational methodology, see Kim and Capaldi (2004). Kappa coefficients computed as reliability indicators for intercoder agreement were .73–.76 (Capaldi et al., 2003). The scores were then averaged over times.
Coder Ratings-Psychological Aggression. The observational coders for the interaction task also provided their own ratings of the men's psychological aggression on the basis of their subjective observations of his behavior toward his partner. Alphas based on an 11-item version were .73–.74 (Kim & Capaldi, 2004). The scores on a seven-point version of the scale were averaged over times.
Injuries. As described in Capaldi and Owen (2001), responses to questions posed to men’s partners in interviews in the Couples Study Waves 2 through 5 were used to derive three measures of injuries reportedly received by each OYS man’s partners: (a) number of times hurt or injured, (b) number of injuries on worst occasion, and (c) severity of worst injury. Because the last two of these measures were almost perfectly associated, r = .97, only the first two items were used in the current analyses. The injuries score was obtained by taking the mean of the z scores of the two measures and calculating the z score of the composite. Right-tail outliers were eliminated by setting z scores greater than 3.00 equal to 3.00. The injuries scores were then averaged over time.
Emergency Room Visits. At each wave, the man’s participating partner was asked, “Have you had to go to a doctor or emergency room because of anything that your partner did”? A score of “1” was assigned for the outcome if any of the man’s partners at any time responded affirmatively. Otherwise, a code of “0” was recorded for the outcome for the man. Relatively few men (8%) had a partner report that their IPV necessitated an emergency room visit.
Data Analyses
A principal components analysis with oblique (promax) rotation was used to confirm the expectation that the IPV measures would form two or more factors that would be distinct from global antisocial behavior. An eigenvalue greater than 1.00 was the criterion that determined the number of factors to be extracted, and the correlations among these factors were examined.
The effects of each of eight substance dependencies (nicotine, alcohol, cannabis, cocaine, opiates, sedatives, amphetamines, and hallucinogens) and four dichotomous drug-problem groupings (none, psychoactive, illicit, and hard drugs) on the promax-derived IPV factor scores were examined using a series of 2 (Drug Status) × 2 (IPV Type) mixed analysis of variance (with IPV Type as the repeated-measures factor and Drug Status as the between-participants factor). The analyses were then replicated with antisocial behavior added to the model as a covariate in analyses of covariance (ANCOVAs).
A 2 (Nicotine Problem: no versus yes) × 4 (Substance Severity Category: none, alcohol, cannabis, and hard drugs) between-participants ANOVA next assessed whether (a) severity of type of psychoactive substance problem affected IPV (controlling for nicotine), (b) nicotine affected IPV (controlling for other substances), and (c) effects of nicotine varied with psychoactive substance group (via the Psychoactive × Nicotine interaction). Next, the linear and quadratic trend of the means as a function of substance severity group (i.e., no problem < alcohol < cannabis < hard-drug, with differences between groups treated as equal) were examined. These analyses were then repeated in an ANCOVA that added antisocial behavior as a covariate. Finally, the association between severity of dependence on a particular substance and IPV was examined by correlating the number of dependence symptoms for a given substance and IPV within the subsample of men identified as having had a problem with the respective substance.
Results
Descriptive Statistics for Men
Table 1 reports the main descriptive statistics for age, relationship length, marital status, and ethnicity for the men who participated at each assessment wave. In addition, 17% of the men met criteria for diagnosis of antisocial personality disorder, their mean number of arrests (excluding arrests for domestic violence) was 5.2, and 8% of the men had a partner who reported that his IPV caused her to seek care at an emergency room.
Table 1.
Descriptive Statistics for Men at Each Assessment Wave
| Wave Number | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| N | 48 | 104 | 122 | 133 | 111 |
| Age (in years) | |||||
| Mean (SD) | 19 (.8) | 21 (.9) | 24 (.6) | 26 (.6) | 28 (.5) |
| Ethnicity (% non-White) | 8 | 14 | 13 | 10 | 9 |
| Relationship Length (in weeks) | |||||
| Mean | 54 | 106 | 169 | 208 | 288 |
| Standard Deviation | 45 | 77 | 118 | 143 | 147 |
| Relationship Status | |||||
| % Dating | 60 | 32 | 22 | 14 | 8 |
| % Cohabitation | 31 | 43 | 36 | 36 | 29 |
| % Married | 8 | 25 | 42 | 50 | 63 |
Measurement Model and Data Reduction
The principal components analysis of the nine IPV and antisocial behavior lifetime measures yielded a three-factor solution that explained 70% of the variance. As shown by the loadings in Table 2, the promax-rotated components were readily interpretable as IPV-Aggression (defined by questionnaire and behavioral measures of both physical and psychological aggression), IPV-Injuries (defined by the two measures of injuries), and Antisocial Behavior (defined by all three antisocial behavior measures) factors. The highest interfactor correlation was between the IPV-Aggression and Antisocial Behavior factors, r = .41. These factor scores were used in further analyses.
Table 2.
Structure Matrix from Principal Components Analysis of Measures of Intimate Partner Violence (IPV) and Antisocial Behavior (N = 150)
| Components | |||
|---|---|---|---|
| Measures | IPV Aggression |
IPV Injuries |
Antisocial Behavior |
| IPV-Agression | |||
| APQ-Physical | .72 | .52 | .17 |
| APQ-Psychological | .76 | .45 | .40 |
| Observed Psychological | .85 | .04 | .32 |
| Coder Rating Psychological | .85 | .10 | .48 |
| IPV-Injuries | |||
| Injuries Score | .38 | .89 | .18 |
| Emergency Room Visits | .06 | .83 | .22 |
| Antisocial Behavior | |||
| Arrests | .27 | .20 | .88 |
| Interviewer Rating | .47 | .29 | .83 |
| Diagnosis | .45 | .08 | .58 |
Note. Mean scores indicate that the measure was obtained at each time (except for injuries, which were not measured in Time 1), and the score was the arithmetic average of the repeated measures. APQ = Adjustment with Partner Questionnaire.
Association of Antisocial Behavior and Drug Problems
As predicted, the association of antisocial behavior and drug use was relatively consistent across the four different categories of drug problems, rs = .23–.29. For specific drugs, the association was highest for nicotine, r = .33, and the lowest for alcohol, sedatives, hallucinogens, and cocaine, rs = .16–.19. The associations of antisocial behavior with opiates, amphetamines, and cannabis were slightly higher, rs = .23–.27.
Association of Substance Dependence and IPV
The questions of whether (a) men with a substance use problem were higher in IPV than other men and (b) whether drug problems had comparable effects on each of the two types of IPV (aggression and injuries) were examined first. A separate analysis was conducted for each substance and substance grouping.
Shown in Table 3 are the F ratios from the ANOVA and ANCOVA analyses.1 In Panel I (top of the table) the results for individual substances are reported, and the findings for substance categories are reported in Panel II (bottom of the table). The zero-order effects of drug problems on IPV in the ANOVAs are reported in the columns on the left, and the effects found by the ANCOVAs in which antisocial behavior was controlled using the Antisocial Behavior factor score as the covariate are reported along with the effects of the covariate in the last two columns. The tabled F values for Drug are for the main effects of Drug Status from the mixed ANOVAs and ANCOVAs, which compared the means of men with and without drug problems on the average of the two IPV factor scores (repeated measures). The F values for the Drug × IPV interaction provide a test of whether drug problems had different effects on the Aggression than on the Injuries IPV scores.
Table 3.
ANOVA and ANCOVA Analyses of Intimate Partner Violence Means as a Function of Different Substance Problems and Categories, with Antisocial Behavior as the ANCOVA Covariate
| Panel I | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ANOVAs | ANCOVAs | |||||||||
| Size | Drug | Drug × IPV Type | Drug | ASB | ||||||
| nNP | nP | F | η2 | F | η2 | F | η2 | F | η2 | |
| Substances | ||||||||||
| Nicotine | 60 | 90 | 11.54*** | .07 | 1.64 | .01 | 4.01* | .03 | 16.70*** | .10 |
| Alcohol | 54 | 96 | 8.37** | .04 | .23 | .00 | 3.52 | .02 | 22.88*** | .13 |
| Cannabis | 87 | 63 | 23.09*** | .14 | .52 | .00 | 15.41*** | .09 | 17.15*** | .10 |
| Cocaine | 132 | 18 | 4.12* | .03 | 2.09 | .01 | 1.71 | .01 | 24.16*** | .13 |
| Opiates | 141 | 9 | 3.72 | .02 | .08 | .00 | .87 | .01 | 21.54*** | .13 |
| Sedatives | 140 | 10 | .41 | .00 | .35 | .00 | .02 | .00 | 24.30*** | .14 |
| Amphetamines | 129 | 21 | 8.59** | .06 | .60 | .00 | 3.27 | .02 | 18.96*** | .11 |
| Hallucinogens | 122 | 28 | 14.15*** | .09 | .11 | .00 | 10.11** | .06 | 20.55*** | .12 |
| Panel II | ||||||||||
| ANOVAs | ANCOVAs | |||||||||
| Size | Drug | Drug χ IPV Type | Drug | ASB | ||||||
| nNP | nP | F | η2 | F | η2 | F | η2 | F | η2 | |
| Categories | ||||||||||
| Any | 30 | 120 | 10.89*** | .07 | .41 | .00 | 4.68* | .03 | 18.08*** | .11 |
| Psychoactive | 43 | 107 | 9.65** | .06 | .00 | .00 | 4.83* | .04 | 19.54*** | .12 |
| Illicit | 80 | 70 | 27.69*** | .16 | .82 | .01 | 17.37*** | .11 | 14.78*** | .09 |
| Hard Drug | 108 | 42 | 25.37*** | .15 | .01 | .00 | 16.93*** | .10 | 16.51*** | .10 |
Note. nNP = n no drug problem, nP = n drug problem.
Findings from the ANOVAs (Table 3) indicate that drug problems were predictive of IPV for all individual substances, other than for opiates and sedatives (Panel I), and for all groupings or categories (Panel II).2 Because opiates and sedatives were the substances in which the smallest numbers of men (ns = 9–10) had problems, lower statistical power in those analyses resulting from a more extreme split in the dichotomous predictor might have yielded Type II errors for the effects of these drugs on IPV. This was almost certainly the case with opiates, as the F value for that effect barely missed significance, p = .056. However, the effect for sedatives was essentially zero, suggesting that even a larger sample would have been unlikely to have yielded a significant difference. The interactions between IPV Type (Aggression versus Injuries) and Drug Problem (Absent versus Present) were all nonsignificant.
Effect sizes in the form of η2 are shown in Table 3. Because the F ratios have 1 df for the numerator, each effect size is equal to r2 (Rosenthal & Rosnow, 1984), which is the point-biserial correlation between the average of the two IPV factor scores and the dichotomous drug-problem outcome. (These values are algebraically equivalent to Cohen’s d, the difference between the means of the two groups divided by the pooled within-group standard deviation, which is generally used to express magnitude of effect between two groups.)
The substances yielding the largest effects on IPV were cannabis (η2 = .14) and hallucinogens (η2 = .09). When Antisocial Behavior was included as a covariate (having η2s = .09–.14) in ANCOVA models, effect sizes for associations of drug problems dropped markedly. Indeed, the only exception was for sedatives, where the effect size was zero whether or not Antisocial Behavior was controlled. Because the effect sizes were dramatically reduced by holding Antisocial Behavior constant, the statistical power to detect partial effects was also reduced. Thus, nicotine, cannabis, and hallucinogens were the only substances to have significant effects on IPV once Antisocial Behavior was controlled, because these substances had the largest zero-order effects on IPV. Also, because the analyses of substance groupings yielded larger zero-order effects than those of individual substances, the effect of all substance groupings on IPV remained significant after Antisocial Behavior was controlled.
The correlation between the zero-order η2 s and paired antisocial behavior controlled partialled η2s across all substance and categories was .98 (n = 12). Thus, controlling for Antisocial Behavior reduced effect sizes proportionately across substances.
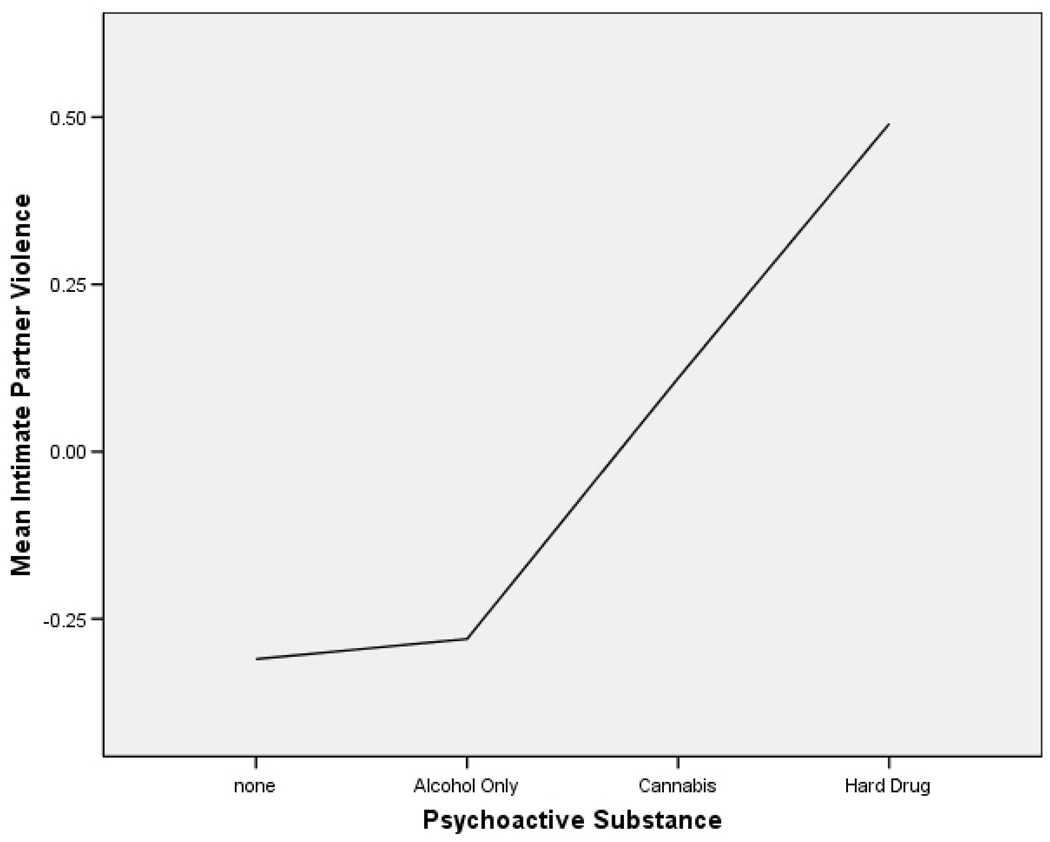
The 2 (Nicotine: Problem versus No Problem) × 4 (Psychoactive Substance Grouping) ANOVA that used the average of the two IPV factor scores as the dependent measure found only a significant main effect of psychoactive substances, F(3, 142) = 7.11, p < .001, η2 = .13. As shown in Figure 1, averaged over the nicotine factor, there was a monotonic increase in IPV (marginal) means as a function of psychoactive substance category severity: −.31 for no substance problem (n = 43), −.28 for alcohol-only problem (n = 37), .11 for cannabis problem (n = 28), and .49 for hard-drug problem (n = 42). The linear contrast of increases in IPV as a function of psychoactive drug severity was highly significant, p < .001, but the quadratic trend was also significant, p < .05. The significant curvilinearity was because of the fact that there was essentially no mean difference (.03) between men who had no psychoactive substance problem and those whose only problem involved alcohol. By contrast, the IPV mean for the marijuana group was much higher (by about .40) than for either of the other two groups, and there was an IPV increase of about the same magnitude from the marijuana group to the hard-drug group. In the ANCOVA that held Antisocial Behavior constant, the substance category effect remained statistically significant, F(3, 141) = 5.08, p < .01, η2 = .10. The adjusted means for the four categories, in the same order, were −.20, −.26, .06, and .46, evidencing the same pattern found for the unadjusted means (but with a reduced range). Once again the linear contrast was highly significant, p < .001, although the quadratic trend only approached significance, p = .08.
Figure 1.
Intimate partner violence means as a function of psychoactive substance-use category.
Association of Severity of Dependence and IPV
Next, correlations were computed to determine whether there was an association between IPV (mean of the two factor scores) and severity of dependence based on the number of dependence symptoms. For men with an alcohol problem (n = 96), there was a significant association between number of alcohol dependence symptoms and IPV (mean of two IPV factor scores), r = .22, p < .05. Therefore, individuals who met the DSM-IV criteria for alcohol dependence (three or more symptoms) committed more IPV than men classified as having an alcohol problem because they had one or two dependence symptoms. However, that correlation was nonsignificant, r = .08, after controlling for the presence of problems with cannabis and other hard drugs. This indicated that among men with an alcohol problem, those with a greater number of alcohol dependence symptoms were more likely than those with fewer symptoms to be polysubstance abusers, and that it was the co-occurring problems with marijuana and hard drugs, rather than a more severe problem with alcohol, that were responsible for the higher incidence of IPV.
The number of dependence symptoms for the target drug and IPV was not significant in the subsamples of men with problems with nicotine, r = .12, or any illicit drug with a subsample that was large enough to warrant a calculation of a correlation coefficient (cannabis, r = −.14, n = 63; cocaine, r = −.01, n = 18; hallucinogens, r = −.05, n = 28; amphetamines, r = −.27, n = 21). Surprisingly, the nonsignificant correlations were all in the negative direction.
Discussion
The association between IPV and at least one symptom of substance dependence was examined for each of eight substance classes in an approximately 9-year study of at-risk men, aged 17–19 years at the onset, who were in long-term relationships with women who participated with them in the assessments at regular intervals. The IPV scores examined involved men’s perpetration of IPV averaged over the study period. Findings confirmed the hypothesis that substance dependence was associated with IPV, and that antisocial behavior at least partially accounted for the associations. Only a dependence on sedatives was found to be completely unrelated to IPV. In addition, substance dependencies were found to be equally predictive of each of the two factorially validated IPV factors (Aggression and Injuries).
Somewhat surprisingly, marijuana and hallucinogen dependencies (rather than alcohol dependence) emerged as the strongest predictors of IPV in analyses, grouping the men by presence or absence of problems with individual substances. Marijuana intoxication generally decreases aggression and hostility (Boles & Miotto, 2003). However, studies that examine patterned use reveal positive associations with violence. For example, in a birth cohort study by Arseneault et al. (2000), marijuana dependence was strongly associated with violence after controlling for significant effects of alcohol and other dependence. Notably, associations between violence and alcohol dependence were best explained by substance use prior to committing violence, whereas relations with marijuana dependence were better explained by a history of juvenile conduct problems. In the present study, antisocial behavior did not explain the association between marijuana use and IPV. Yet, it remains possible that marijuana users differ from nonusers on other personality factors that increase their risk for committing IPV. For example, individuals with problems controlling angry and violent impulses may use marijuana to relax and reduce aggressive outbursts, a “self-medication” hypothesis that has received recent support (Arendt et al., 2007). It was unexpected that hallucinogens were more strongly associated with IPV than was any other hard drug (and the only hard drug to remain significantly associated with IPV after Antisocial Behavior was held constant), given that little previous research has examined the linkage between hallucinogens and IPV.
In analyses of polysubstance problems, all four dichotomous drug grouping analyses found dependency to be associated with IPV. The two strongest effects on IPV were found in comparisons between (a) men who had a problem with an illicit substance (i.e., marijuana or a hard drug) with those who did not and (b) men who had a hard-drug problem (a substance other than nicotine, alcohol, and marijuana) with those who did not. Indeed, the effect sizes associated with these two comparisons exceeded those observed for any individual substance.
Although there were associations of both nicotine and alcohol with IPV, they were no longer significant when problems with illicit drugs (cannabis, hard drugs) were controlled. There was no difference in IPV level between men whose only psychoactive problem was with alcohol and men without any psychoactive substance problem. However, men with a cannabis problem had much higher levels of IPV than the men with only an alcohol (or no) problem (see Figure 1). Because the majority (86%) of men with cannabis (but no hard-drug) problem were also alcohol dependent, the comparisons between the alcohol group and marijuana group was essentially a comparison between men who had problems with both alcohol and cannabis (though not necessarily at the same time) versus those who had a problem with alcohol alone. Finally, men who had a hard-drug problem were higher in IPV than men whose only illicit substance problem involved marijuana. These data indicate that previous findings linking alcohol problems to violence may be because of the concurrent use of alcohol by the marijuana users who commit more IPV. Thus, our work is not inconsistent with past research because we also found associations between alcohol problems and IPV before controls were introduced. Because past work did not control for the correlation between marijuana and alcohol use, our study is the first to assess the indirect effect of alcohol problems on IPV (controlling for marijuana problems). The lack of such an association indicates that more needs to be conducted to test if this finding is robust.
As was expected, because of the association of antisocial behavior with both IPV and substance use, antisocial behavior explained part of the association between IPV and drug problems. When antisocial behavior was entered as a covariate in the analyses, two consistent findings emerged. First, when substance use problems and antisocial behavior were considered simultaneously, the latter had much stronger effects on IPV than the former. Second, the reductions in the effect sizes for different substances after controlling for antisocial behavior were almost perfectly proportionate to the zero-order effects of the same substances. As a result, the only substances that yielded significant differences in IPV after controlling for antisocial behavior were marijuana and hallucinogens, which had the largest univariate associations. However, all four of the dichotomous dependence groupings were significantly associated with IPV, with the largest effects again seen for those groupings that compared men who had problems with illicit and hard substances (which were again larger than the effects for any single substance problem). The earlier finding from multiple-group analysis–that hard-drug abusers had higher IPV than marijuana abusers, who in turn had higher IPV than the alcohol only abusers and nonabusers (with no differences in IPV among the latter two groups)--held after antisocial behavior was controlled.
Limitations and Conclusions
A key limitation to the present research was that data on substance-dependence symptoms was assessed at a single time point and for lifetime rather than current dependency. Most important, substance-abuse assessment was conducted toward the end of the study. Thus, it was not possible to do a prospective study or to model variations in IPV as a function of variations in substance dependency symptoms. In addition, the study involved a predominantly White sample and male IPV perpetration, thus tests of generalizability to other populations should be made. However, the current findings have important implications for the efficacy of substance treatment for reducing risk to a partner for IPV. Treating marijuana and hard-drug use may be more consequential than treating alcohol use. Moreover, a further implication of these findings is that the goal of treatment should be abstinence for the illicit substances most predictive of IPV, rather than merely a reduction in the use of such substances. However, further research is needed to determine whether the most productive targets for intervention should be personality factors associated with drug use (e.g., anger and poor self-regulation; Arendt et al., 2007) or drug use itself. Overall, findings suggest that the role of alcohol problems in IPV perpetration may not be as strong as has previously been considered, because of the role of antisocial behavior and to polysubstance use. Future research is needed to examine whether changes in IPV over time can be explained by concomitant changes in substance-abuse problems over the same period.
Acknowledgements
Support for the Couples Study (Grant HD 46364) was provided by Cognitive, Social and Affective Development, National Institute of Child Health and Human Development (NICHD), and by the Division of Epidemiology, Services and Prevention Branch, National Institute on Drug Abuse (NIDA). Additional support was provided by Grant MH 37940 from the Antisocial and Other Personality Disorders Program, National Institute of Mental Health, and by Grant DA 051485 from the Division of Epidemiology, Services and Prevention Branch, NIDA, and Cognitive, Social, and Affective Development, NICHD. We thank Jane Wilson and the assessment team for data collection and Sally Schwader for editorial assistance.
Footnotes
An anonymous reviewer suggested that the number of men’s participating partners in the analysis (one versus two) might have affected the results. Accordingly, we ran a 2 (Drug Problem) × 2 (No. of Partners) × 2 (IPV Type) ANOVA for each of the four drug categories. Because no predictions were made, we used Bonferroni corrections by testing significance at p < .0125. No significant interactions were found that involved the number of partners’ factor.
We also conducted Hierarchical Linear Modeling (HLM) analyses using measures of both aggression and injuries factors derived from a subset of time-varying measures and treating age as a grand-centered variable (both with and without antisocial behavior as a covariate). As would be expected (because both types of analyses examined the same hypotheses about associations between dependency and mean IPV scores), the correlations of substance dependency with IPV intercepts mirrored the findings on the effects of drug classification on IPV from the ANOVAs/ANCOVAs. However, the number of significant associations between substance dependency and IPV slopes were about the same as would be expected due solely to chance.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders DSM-IV-TR. 4th ed. Text Revision. Washington, DC: Author: 2000. [Google Scholar]
- Arendt M, Rosenberg R, Fjordback L, Brandholdt J, Foldager L, Sher L, Munk-Jorgensen P. Testing the self-medication hypothesis of depression and aggression in cannabis-dependent subjects. Psychological Medicine. 2007;37:935–945. doi: 10.1017/S0033291706009688. [DOI] [PubMed] [Google Scholar]
- Arseneault L, Moffitt TE, Caspi A, Taylor PJ, Silva PA. Mental disorders and violence in a total birth cohort. Archives of General Psychiatry. 2000;57:979–986. doi: 10.1001/archpsyc.57.10.979. [DOI] [PubMed] [Google Scholar]
- Boles SM, Miotto K. Substance abuse and violence: A review of the literature. Aggression and Violent Behavior. 2003;8:155–174. [Google Scholar]
- Brookoff D, O’Brien KK, Cook CS, Thompson TD, Williams C. Characteristics of participants in domestic violence: Assessment at the scene of domestic assault. Journal of the American Medical Association. 1997;277:1369–1376. [PubMed] [Google Scholar]
- Capaldi DM, Clark S. Prospective family predictors of aggression toward female partners for at-risk young men. Developmental Psychology. 1998;34:1175–1188. doi: 10.1037//0012-1649.34.6.1175. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Crosby L. Observed and reported psychological and physical aggression in young, at-risk couples. Social Development. 1997;6:184–206. [Google Scholar]
- Capaldi DM, Dishion TJ, Stoolmiller M, Yoerger K. Aggression toward female partners by at-risk young men: The contribution of male adolescent friendships. Developmental Psychology. 2001;37:61–73. [PubMed] [Google Scholar]
- Capaldi DM, Owen LD. Physical aggression in a community sample of at-risk young couples: Gender comparisons for high frequency, injury, and fear. Journal of Family Psychology. 2001;15:425–440. doi: 10.1037//0893-3200.15.3.425. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Shortt JW. Understanding conduct problems in adolescence from a lifespan perspective. In: Adams GR, Berzonsky MD, editors. Blackwell handbook of adolescence. Oxford, UK: Blackwell Publishing Ltd.; 2003. pp. 470–493. [Google Scholar]
- Capaldi DM, Shortt JW, Crosby L. Physical and psychological aggression in at-risk young couples: Stability and change in young adulthood. Merrill-Palmer Quarterly. 2003;49:1–27. [Google Scholar]
- Dishion TJ, Capaldi DM, Yoerger K. Middle childhood antecedents to progression in male adolescent substance use: An ecological analysis of risk and protection. Journal of Adolescent Research. 1999;14:175–206. [Google Scholar]
- Fals-Stewart W, Kennedy C. Addressing intimate partner violence in substance-abuse treatment. Journal of Substance Abuse Treatment. 2005;29:5–17. doi: 10.1016/j.jsat.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Leonard KE, Birchler GR. The occurrence of male-to-female intimate partner violence on day’s of men’s drinking: The moderating effects of antisocial personality disorder. Journal of Consulting and Clinical Psychology. 2005;73:239–248. doi: 10.1037/0022-006X.73.2.239. [DOI] [PubMed] [Google Scholar]
- Feingold A, Rounsaville B. Construct validity of the abuse-dependence distinction as measured by DSM-IV criteria for different psychoactive substances. Drug and Alcohol Dependence. 1995a;39:99–109. doi: 10.1016/0376-8716(95)01142-l. [DOI] [PubMed] [Google Scholar]
- Feingold A, Rounsaville B. Construct validity of the dependence syndrome as measured by DSM-IV for different psychoactive substances. Addiction. 1995b;90:1661–1669. doi: 10.1046/j.1360-0443.1995.901216618.x. [DOI] [PubMed] [Google Scholar]
- Friedman AS, Terras A, Glassman K. The differential disinhibition effect of marijuana use on violent behavior: A comparison of this effect on a conventional, nondelinquent group versus a delinquent or deviant group. Journal of Addictive Diseases. 2003;22:63–78. doi: 10.1300/J069v22n03_06. [DOI] [PubMed] [Google Scholar]
- Gelles RJ, Cavanaugh MM. Association is not causation: Alcohol and other drugs do not cause violence. In: Loseke DR, Gelles RJ, Cavanaugh MM, editors. Current controversies on family violence. Thousand Oaks, CA: Sage; 2005. pp. 175–189. [Google Scholar]
- Jackson KM, Sher KJ, Schulenberg JE. Conjoint developmental trajectories of young adulthood alcohol and tobacco use. Journal of Abnormal Psychology. 2005;114:612–626. doi: 10.1037/0021-843X.114.4.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC. The national comorbidity survey. DIS Newsletter. 1990;7(12):1–2. [Google Scholar]
- Kim HK, Capaldi DM. The association of antisocial behavior and depressive symptoms between partners and risk for aggression in romantic relationships. Journal of Family Psychology. 2004;18:82–96. doi: 10.1037/0893-3200.18.1.82. [DOI] [PubMed] [Google Scholar]
- Lennings CJ, Copeland J, Howard J. Substance use patterns of young offenders and violent crime. Aggressive Behavior. 2003;29:414–422. [Google Scholar]
- Rosenthal R, Rosnow RL. Essentials of behavioral research: Methods and data analysis. New York: McGraw-Hill; 1984. [Google Scholar]
- Sommers I, Baskin D. Methamphetamine use and violence. Journal of Drug Issues. 2006:77–96. [Google Scholar]
- Sommers I, Baskin D, Baskin-Sommers A. Methamphetamine use among young adults: Health and social consequences. Addictive Behaviors. 2006;31:1469–1476. doi: 10.1016/j.addbeh.2005.10.004. [DOI] [PubMed] [Google Scholar]
- Thompson MP, Kingree JB. The roles of victim and perpetrator alcohol use in intimate partner violence outcomes. Journal of Interpersonal Violence. 2006;21:163–177. doi: 10.1177/0886260505282283. [DOI] [PubMed] [Google Scholar]
- Washington University. Diagnostic interview schedule. 4th ed. St. Louis, MO: Author; 1998. [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview (CIDI) Core version 2. 1. Geneva, Switzerland: Author; 1997. [Google Scholar]