Abstract
Purpose
The study's objective was to compare the quality of life (QoL) of patients with endometrial cancer undergoing surgical staging via laparoscopy versus laparotomy.
Patients and Methods
The first 802 eligible patients (laparoscopy, n = 535; laparotomy, n = 267) participated in the QoL study in a Gynecologic Oncology Group (GOG) randomized trial of laparoscopy versus laparotomy (GOG 2222). Patients completed QoL assessments at baseline; at 1, 3, and 6 weeks; and at 6 months postsurgery.
Results
In an intent-to-treat analysis, laparoscopy patients reported significantly higher Functional Assessment of Cancer Therapy–General (FACT-G) scores (P = .001), better physical functioning (P = .006), better body image (BI; P < .001), less pain (P < .001) and its interference with QoL (P < .001), and an earlier resumption of normal activities (P = .003) and return to work (P = .04) over the 6-week postsurgery period, as compared with laparotomy patients. However, the differences in BI and return to work between groups were modest, and the adjusted FACT-G scores did not meet the minimally important difference (MID) between the two surgical arms over 6 weeks. By 6 months, except for better BI in laparoscopy patients (P < .001), the difference in QoL between the two surgical techniques was not statistically significant.
Conclusion
Although the FACT-G did not show a MID between the two surgical groups, and only modest differences in return to work and BI were found between the two groups, statistically significantly better QoL across many parameters in the laparoscopy arm at 6 weeks provides modest support for the QoL advantage of using laparoscopy to stage patients with early endometrial cancer.
INTRODUCTION
In the early 1990s, the Gynecologic Oncology Group (GOG) began evaluating minimally invasive surgical approaches to staging women with endometrial cancer. In comparing laparoscopy with laparotomy, surgical complications, perioperative morbidity, length of hospital stay, the incidence of subcutaneous metastases, and patients' quality of life (QoL) were evaluated. Potential benefits of laparoscopic surgery include a reduction in wound complications and adhesion formation and decreased hospital stay when compared with laparotomy.1–8 Potential complications associated with laparoscopy include visceral and vascular injuries owing to trocar insertion, trocar site recurrences, hernias, and bowel and urinary tract injury.1
There is little information concerning the QoL outcomes associated with laparoscopy compared with laparotomy in patients with endometrial cancer. A retrospective study of 30 patients with endometrial cancer demonstrated a reduction in time to return to work (2.4 v 5.3 weeks) when comparing laparoscopy with laparotomy.7 In their study of 84 patients with endometrial cancer, Zullo et al9 found that QoL (physical and emotional functioning) 1 month postoperatively was significantly better in the laparoscopic versus the laparotomy group (P < .05). By 6 months, no significant QoL differences were identified between the two groups.
Differences in QoL among patients treated with laparoscopy have been studied in other patient populations. In a large randomized trial of patients with colon cancer, only pain medication required during hospitalization and global QoL at 2 weeks favored the laparoscopy group compared with the open colectomy arm.10 There were no QoL differences between the two groups 2 months after surgery. Braga et al11 found a significantly better QoL in patients with colon cancer undergoing laparoscopy compared with those undergoing open colectomy at 12 months, whereas at 24 months, the only remaining significant advantage in the laparoscopic group was social functioning.
The lack of outcome information pertaining to patients with endometrial cancer undergoing laparoscopy versus laparotomy prompted the GOG to conduct a randomized clinical trial (GOG 2222) to compare the two procedures in terms of the proportion of serious complications (initial primary end point) and recurrence-free interval (subsequent primary end point), staging information, complications, operative time, hospital stay, recurrence pattern, and QoL.12 The study was designed to test whether laparoscopy would result in a significant improvement in patient's QoL as a result of less pain, earlier return to work and normal activities, better body image, and, as a consequence, less psychological distress compared with those undergoing laparotomy.
PATIENTS AND METHODS
This study was approved by the institutional review boards of all participating GOG institutions, and patients provided written informed consent. All patients participating in the QoL component of this study were accrued to the GOG clinical trial; had no clinical evidence of metastatic disease; had adequate bone marrow, renal, and hepatic function; had a GOG performance status of 0 to 3 (0, normal activity, to 3, symptomatic and in bed > 50% of time); and spoke English, French-Canadian, or Spanish. To maximize information about laparoscopy, a 2 to 1 randomization scheme was chosen, as there was less known about clinical and QoL outcomes in patients undergoing laparoscopy. Patients' QoL was assessed before surgery; at 1, 3, and 6 weeks; and at 6 months postsurgery. At baseline, patients were provided with four copies of all postsurgery assessment forms and stamped, self-addressed envelopes for use in returning completed questionnaires to the clinician/data manager. Questionnaires were reviewed for completeness. Patients having difficulty in reading the questionnaires were interviewed by the clinician/data manager either in person or by telephone. Reminder calls were placed to patients by data managers a few days before the expected return date of the questionnaires. Questionnaires not received in a week's time were followed up with a second reminder call.
QoL Measures
The Functional Assessment of Cancer Therapy Scale–General (FACT-G; version 3.0)13 consists of five subscales: physical, social, emotional, and functional well-being and relationship with one's doctor. The FACT-G total score is based on 27 items that include only the physical, social, emotional, and functional well-being subscales, with scores ranging from 0 to 108. Higher scores indicate a better QoL.
Additional Treatment Related Symptoms (AP) consists of six items related to surgical side effects such as fever, constipation, diarrhea, shortness of breath, the ability to eat, and problems urinating. Higher scores indicate worse symptoms. The total AP scores range from 0 to 24.
The Physical Functioning Subscale of the Medical Outcome Study–Short Form (MOS-SF36; PF) is a 10-item scale with items designed to assess activities of daily living.14 The item scores are summated and are then transformed to a scale of 0 to 100. Higher scores indicate better physical functioning.
Resumption of Normal Activities is a single item rated on a 0% to 100% scale designed to assess the extent that the patient was able to resume all of their normal activities.
Two items from the Brief Pain Inventory (BPI)15 were selected to assess pain severity at its least and worst in the previous 7 days. Seven items measure pain's interference with different domains of QoL. The pain severity total scores range from 0 to 20 and 0 to 70 for pain's interference with QoL, with higher scores indicating worse pain or more interference of pain on QoL.
Fear of Recurrence is a five-item scale measuring patients' beliefs about recurrence of their cancer.16 The total score ranges from 0 to 20, with higher scores indicating a greater fear of recurrence.
Body Image (BI), a seven-item scale created for all follow-up assessments and developed by the authors, assesses patients' concerns about their physical appearance as a consequence of having surgery and its relationship to other areas in their life. Higher scores indicate a better body image. The total score ranges from 0 to 28. The Cronbach α coefficient of 0.67 for the seven-item scale at 6 months indicated marginal internal consistency.17
Return to Work is a single item that asks patients who were employed the date on which they returned to work after their operation.
Statistical Methods
The data were analyzed as an intent-to-treat analysis, although 21% of patients in the QoL study who were randomly assigned to laparoscopy converted to laparotomy. Because of the multiplicity of QoL outcome measures and potential correlations among the scales, each QoL scale was tested at a significance level of .01 (.05/5) to control for the overall type I error at .05. As the overall measure of QoL was the FACT-G, it was considered the primary QoL outcome. A required sample size of 600 eligible patients was estimated based on the original primary clinical end point: the proportion of serious complications. This provided 96% statistical power to detect the minimally important difference (MID) of 5 points on the FACT-G at a significance level of .01. The difference of 5 points on FACT-G is comparable to a one-unit change of the GOG performance score and is considered an MID.18 To allow for approximately 20% patient attrition and noncompliance, 800 patients were accrued to the QoL study. In April 2001, the study group increased the sample size to include recurrence-free survival as a primary study end point. Because the original QoL sample size provided sufficient statistical power, it was decided to terminate enrollment for the QoL study in April 2001.
The comparison of the postsurgery QoL scores between the two randomized arms was focused on the 1, 3, and 6-week postsurgical assessments. A linear mixed model was fitted for each QoL scale score, adjusted for corresponding baseline assessment scores, time effect, patients' age, weight (in kilograms) at study entry, and marital status (married v not married). The interaction between treatment and time was first examined for the similarity of treatment effects at 1, 3, and 6 weeks postsurgery, with the significance level for an interaction set at .05. If the interaction effect was significant, then treatment effects at each postsurgical assessment were tested at the significance level of .01 by comparing least-square means between the two arms. Otherwise, the mixed model was refitted without the interaction, and treatment effects were tested as an overall effect over the postsurgical assessments. The 6-month evaluation was considered exploratory and was examined only if there was a significant difference between surgical groups in a particular QoL score within 6 weeks postsurgery. The general linear model was used to explore whether the difference persisted at 6 months, adjusting for corresponding baseline scores, patients' age, weight at baseline, and marital status. Each scale was tested at a significance level of .05 for this purpose.
The treatment effect on the completion rates of QoL assessments across time were examined using the Generalized Estimating Equations method with an unstructured working correlation matrix.
RESULTS
Between April 1, 1996, and April 1, 2001, the first 808 patients (laparoscopy, n = 539; laparotomy, n = 269) of the 2,616 patients from the clinical trial were enrolled onto the QoL component of GOG 2222. Six patients (laparoscopy, n = 4; laparotomy, n = 2) were deemed unassessable because of refusal of treatment. The QoL results presented here are based on the remaining assessable 802 patients with endometrial cancer (laparoscopy, n = 535; laparotomy, n = 267).
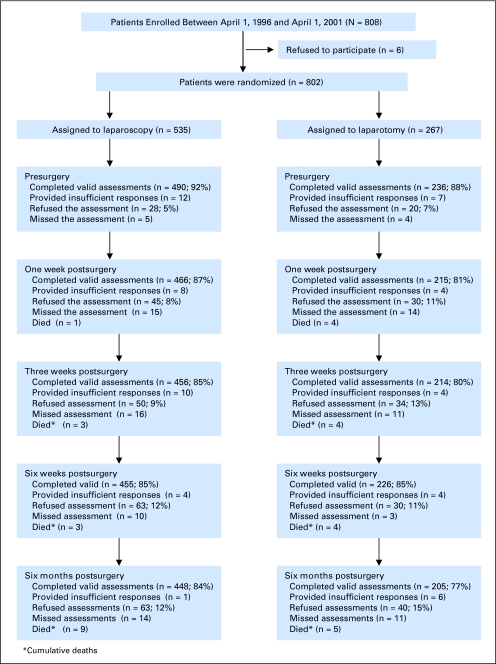
Ninety-two percent of laparoscopy patients and 88% of laparotomy patients provided valid baseline QoL assessments. Completion rates were slightly but significantly higher in the laparoscopy group at 1 week (87% v 81%; P = .02) and 6 months (84% v 77%; P = .02) postsurgery (Fig 1, CONSORT diagram). Reasons for noncompliance included patient refusal (laparoscopy, 9%; laparotomy, 12%), incomplete questionnaires (1.5%), illness (1%), death (0.5%), and other (2%).
Fig 1.
Quality of life assessment compliance CONSORT diagram.
To test for sample bias, the sample of participants in the QoL study (n = 802) was compared with those who were randomly assigned and received treatment after April 1, 2001 (n = 1,789), but were not offered participation in the QoL study. The only sociodemographic difference between groups was that more non-Hispanic patients were enrolled before April 1, 2001, as compared with those accrued after that date (96.8% v 83.9%; χ2 test P < .001). However, 204 patients did not report their ethnicity.
Patient characteristics are presented in Table 1. The patients' mean age was 63.6 years, the majority were white, and approximately half were married. There were no significant differences between the two randomly assigned groups with respect to age, weight, race, Hispanic ethnicity, and marital status.
Table 1.
Patient Characteristics
| Characteristic | Laparoscopy (n = 535) |
Laparotomy (n = 267) |
||
|---|---|---|---|---|
| No. | % | No. | % | |
| Age, years | ||||
| Mean | 64.1 | 62.5 | ||
| Standard deviation | 11.2 | 11.8 | ||
| ≤ 39 | 13 | 2.4 | 8 | 3.0 |
| 40-49 | 40 | 7.5 | 28 | 10.5 |
| 50-59 | 142 | 26.5 | 69 | 25.8 |
| 60-69 | 161 | 30.1 | 91 | 34.1 |
| 70-79 | 147 | 27.5 | 50 | 18.7 |
| ≥80 | 32 | 6.0 | 21 | 7.9 |
| Weight, kg | ||||
| Mean | 75.9 | 77.0 | ||
| Standard deviation | 19.9 | 21.2 | ||
| Race | ||||
| White | 473 | 88.4 | 227 | 85.0 |
| Asian | 21 | 3.9 | 11 | 4.1 |
| Black | 22 | 4.1 | 12 | 4.5 |
| Other/not specified | 19 | 3.6 | 17 | 6.4 |
| Ethnicity | ||||
| Hispanic | 16 | 3.0 | 8 | 3.4 |
| Non-Hispanic | 519 | 97.0 | 257 | 96.3 |
| Not specified | 0 | 0.0 | 1 | 0.4 |
| Marital status | ||||
| Married | 286 | 53.5 | 147 | 55.1 |
| Widowed | 110 | 20.6 | 32 | 12.0 |
| Separated/divorced | 55 | 10.3 | 32 | 12.0 |
| Single | 37 | 6.9 | 22 | 8.2 |
| Unknown | 47 | 8.8 | 34 | 12.7 |
QoL of Patients With Endometrial Cancer Assigned to Laparoscopy Versus Laparotomy
Before surgery, there were no significant differences in any QoL measures except for the MOS Physical Functioning Scale, in which patients assigned to laparoscopy had a score that was 6.8 points higher in physical functioning (95% CI, 2.3 to 11.3; P = .003) than those assigned to laparotomy (Table 2).
Table 2.
QoL Scores for Each Assessment Between Patients Assigned to Laparoscopy Versus Laparotomy
| QoL Measure and Assessment Point | Assigned to Laparoscopy (n = 535) |
Assigned to Laparotomy (n = 267) |
P† | ||||
|---|---|---|---|---|---|---|---|
| No.* | Mean | SD | No.* | Mean | SD | ||
| FACT-G‡ | |||||||
| Presurgery | 476 | 87.0 | 12.8 | 229 | 85.7 | 14.5 | .26 |
| 1 week postsurgery | 455 | 77.1 | 14.6 | 212 | 72.3 | 15.3 | .004 |
| 3 weeks postsurgery | 447 | 83.9 | 14.5 | 213 | 80.1 | 14.6 | .025 |
| 6 weeks postsurgery | 446 | 89.6 | 14.1 | 223 | 85.4 | 15.3 | .006 |
| 6 months postsurgery | 434 | 91.9 | 14.0 | 203 | 90.7 | 14.5 | .64 |
| Additional treatment-related problems§ | |||||||
| Presurgery | 465 | 2.6 | 2.4 | 223 | 2.5 | 2.5 | .73 |
| 1 week postsurgery | 446 | 3.8 | 2.9 | 202 | 4.6 | 3.3 | .003 |
| 3 weeks postsurgery | 442 | 3.0 | 2.7 | 206 | 3.0 | 2.5 | .75 |
| 6 weeks postsurgery | 437 | 2.5 | 2.5 | 214 | 2.8 | 2.7 | .08 |
| 6 months postsurgery | 428 | 2.3 | 2.4 | 194 | 2.2 | 2.6 | .84 |
| Physical functioning‡ | |||||||
| Presurgery | 468 | 75.9 | 27.8 | 228 | 69.2 | 30.1 | .004 |
| 1 week postsurgery | 449 | 24.8 | 19.5 | 202 | 17.6 | 17.0 | .006 |
| 3 weeks postsurgery | 443 | 46.7 | 24.5 | 205 | 36.2 | 20.8 | < .001 |
| 6 weeks postsurgery | 441 | 66.5 | 26.6 | 217 | 55.9 | 25.5 | < .001 |
| 6 months postsurgery | 438 | 76.2 | 26.1 | 198 | 72.3 | 27.2 | .44 |
| Pain severity§ | |||||||
| Presurgery | 452 | 2.8 | 4.2 | 220 | 3.3 | 4.5 | .15 |
| 1 week postsurgery | 451 | 7.0 | 4.7 | 204 | 8.4 | 4.8 | .004 |
| 3 weeks postsurgery | 439 | 4.1 | 4.1 | 205 | 5.0 | 4.0 | .013 |
| 6 weeks postsurgery | 434 | 2.4 | 3.5 | 214 | 2.9 | 3.7 | .201 |
| 6 months postsurgery | 432 | 1.4 | 3.0 | 195 | 1.4 | 2.8 | .85 |
| Pain interference with QoL§ | |||||||
| Presurgery | 468 | 7.7 | 13.4 | 228 | 9.6 | 15.6 | .10 |
| 1 week postsurgery | 451 | 26.8 | 18.8 | 204 | 31.5 | 18.5 | .011 |
| 3 weeks postsurgery | 444 | 16.3 | 16.8 | 205 | 20.0 | 17.8 | .06 |
| 6 weeks postsurgery | 436 | 8.9 | 13.5 | 217 | 12.7 | 16.4 | .021 |
| 6 months postsurgery | 432 | 5.3 | 10.7 | 194 | 5.8 | 11.8 | .40 |
| Body image‡ | |||||||
| Presurgery | 468 | 10.5 | 3.5 | 223 | 10.1 | 3.2 | .10 |
| 1 week postsurgery | 439 | 20.1 | 4.5 | 203 | 17.7 | 4.9 | < .001 |
| 3 weeks postsurgery | 429 | 21.2 | 4.4 | 204 | 18.8 | 4.7 | < .001 |
| 6 weeks postsurgery | 434 | 21.8 | 4.4 | 215 | 19.5 | 4.7 | < .001 |
| 6 months postsurgery | 424 | 22.2 | 4.2 | 192 | 20.8 | 4.6 | < .001 |
| Fear of recurrence§ | |||||||
| 1 week postsurgery | 434 | 4.7 | 3.9 | 203 | 5.3 | 4.1 | .06 |
| 3 weeks postsurgery | 427 | 4.1 | 3.8 | 203 | 4.7 | 3.9 | .14 |
| 6 weeks postsurgery | 430 | 3.9 | 3.6 | 214 | 4.1 | 3.9 | .40 |
| 6 months postsurgery | 421 | 4.0 | 3.6 | 192 | 3.9 | 3.7 | .79 |
| Resumption of normal activities (%)‡ | |||||||
| 1 week postsurgery | 392 | 22.3 | 21.5 | 184 | 19.3 | 23.3 | .20 |
| 3 weeks postsurgery | 374 | 43.2 | 25.9 | 185 | 36.0 | 25.6 | .002 |
| 6 weeks postsurgery | 377 | 67.3 | 27.9 | 186 | 56.6 | 27.9 | < .001 |
| 6 months postsurgery | 378 | 82.6 | 23.9 | 175 | 81.3 | 23.4 | .50 |
Abbreviations: QoL, quality of life; SD, standard deviation; FACT-G, Functional Assessment of Cancer Therapy–General.
No. of valid assessments.
Two-sided t test for presurgery comparison. Postsurgery comparisons (within 6 weeks) were tested by fitting linear mixed model adjusting for baseline scores, time effect, age, weight, and marital status, and taking into account of the assumed covariance structure. The 6-month follow-up comparison was tested by fitting the general linear model adjusting for baseline scores, age, weight, and marital status.
Higher scores indicate better quality of life.
Higher scores indicate worse quality of life.
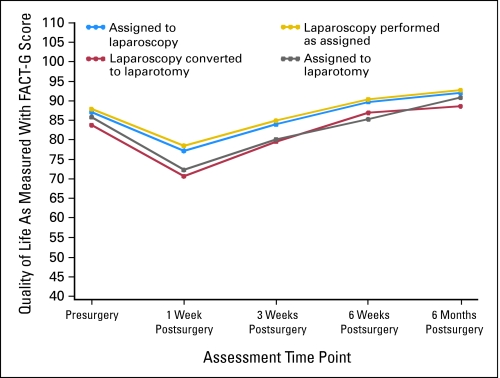
Within 6 weeks postsurgery, patients assigned to laparoscopy reported better QoL on all scales other than Fear of Recurrence as compared with those assigned to laparotomy (Table 2). The observed treatment differences between laparotomy and laparoscopy did not vary from 1 to 6 weeks for the FACT-G, PF, Pain Interference with QoL, and BI. After adjustment (baseline scores, assessment time, age, weight, marital status), patients assigned to laparoscopy reported an average of 3.0 points higher in FACT-G scores (99% CI, 0.63 to 5.3; P = .001), 6.0 points higher in PF scores (99% CI, 2.6 to 9.5; P < .001), 2 points higher in BI (99% CI, 1.2 to 2.9; P < .001), and 3.0 points lower in Pain Interference with QoL (99% CI, 0.26 to 5.8; P = .005) than those assigned to laparotomy during the 6 weeks postsurgery period. The difference in averaged adjusted FACT-G scores between the two surgical arms did not reach the MID of 5 points over the 6 weeks postsurgery period (Fig 2). However, 52% of laparotomy patients (104 of 200) compared with 43% of laparoscopy patients (181 of 421) had a worsening of their FACT-G scores at 5 points or greater (MID) at 3 weeks, and 37.3% of laparotomy patients (78 of 209) had a worsening of their FACT-G scores at 5 points or greater at 6 weeks compared with 25% of laparoscopy patients (107 of 424).
Fig 2.
Quality of life as measured with Functional Assessment of Cancer Therapy–General (FACT-G) scores.
The observed treatment differences in AP, Pain Severity, and Resumption of Normal Activities varied over the 6-week postsurgical period. Patients randomly assigned to laparoscopy reported significantly lower AP scores (0.8 points lower; 99% CI, 0.1 to 1.5; P = .003) and lower Pain Severity scores (1.4 points lower; 99% CI, 0.4 to 2.4; P < .001) than those randomly assigned to laparotomy at 1 week, but not at 3 and 6 weeks. In addition, patients randomly assigned to laparoscopy reported that more daily activities were resumed after surgery compared with those randomly assigned to laparotomy at 3 weeks (6.9% higher in the laparoscopy group; 99% CI, 1.1% to 12.7%; P = .002) and 6 weeks (9.8% higher in the laparoscopy group; 99% CI, 3.6% to 16.2%; P < .001), but not at 1 week. Of 273 patients reporting the time to return to work, the median time to return to work was 42 days for the laparoscopy group compared with 45 days in the laparotomy group, a small but significant difference (Wilcoxon rank sum test, P = .04).
At 6 months postsurgery, all reported differences in QoL scales between the two arms were not statistically significant, except for BI, which was 1.32 points higher (95% CI, 0.61 to 2.04; P < .001) in the laparoscopy compared with the laparotomy arm.
Although there were significant differences in physical functioning at baseline, this did not affect the overall results, as the analyses were adjusted for baseline levels. Given this approach to statistical analyses and the fact that there were no other statistically significant baseline differences between the two groups in the other QoL variables, it is unlikely that the differences in physical functioning at baseline would have affected other QoL findings.
DISCUSSION
The purpose of the study was to test whether there would be an improved QoL as a result of laparoscopy being less invasive than laparotomy in staging women with endometrial cancer. Patients treated with laparoscopy were found to have similar rates of intraoperative complications and ability to identify metastatic disease, a shorter length of hospitalization, and significantly fewer moderate to severe (Common Toxicity Criteria for Adverse Events grade 2) postoperative complications than those treated with laparotomy.1 In addition, patients undergoing laparoscopy were found to have a superior overall QoL during the 6-week postoperative period, with fewer physical symptoms, less pain and pain-related interference with functioning, better physical functioning and emotional state, earlier resumption of normal activities, earlier return to work, and better BI as compared with those undergoing laparotomy.
However, adjusted scores of the FACT-G did not reach the predefined MID between the surgical arms19 and differences between surgical arms in return to work and BI were modest. Yet approximately 10% (9% at 3 weeks and 12% at 6 weeks) more patients in the laparotomy arm experienced a decline in FACT-G scores beyond the MID than patients in the laparoscopy arm. In other words, for every 10 patients offered laparoscopy, one patient would be spared the short-term decline in QoL. The converging QoL between the two groups at 6 months may reflect the slower, but eventually equal recovery experienced by laparotomy patients in all areas other than BI, which persisted at 6 months.
Some of our findings are consistent with studies comparing laparoscopy to laparotomy.7,9–11 Zullo et al9 found that physical and emotional functioning was significantly better in the laparoscopy group versus the laparotomy group at 1 month postsurgery. A significantly earlier return to work in the laparoscopy compared with the laparotomy group was also found by Spirtos et al,7 with a bigger difference in the length of time to return to work than our results showed. Both Zullo et al9 and our results showed no QoL differences between the two groups by 6 months. Yet Brega et al11 found in patients with colon cancer that the significantly better QoL in the laparoscopy group compared with the open colectomy group at 12 months resolved at 24 months, a longer time to resolve differences than was found in our study. However, Weeks et al10 found that only pain medication and global QoL in patients with colon cancer was significantly better in the laparoscopy compared with the open colectomy group at 2 weeks. These differences resolved by 2 months.
Perhaps the reason for our modest but statistically significant QoL differences between the surgical groups and that the FACT-G did not reach a MID between groups can be explained by similar clinical outcomes, including intraoperative complications and identification of metastatic disease, and minor differences in length of hospitalization (4 v 3 days for laparotomy and laparoscopy, respectively) found in the clinical trial.1 These findings might have outweighed the significantly fewer postoperative complications in the laparoscopy than the laparotomy group (14% v, 21%, respectively; P < .0011) found in the clinical trial, in its impact on QoL, as these differences between surgical groups were not large. Additionally, 21% of patients who participated in the QoL study who were randomly assigned to laparoscopy were converted to laparotomy. QoL differences between the laparoscopy and laparotomy arms might have been greater if there had not been such a large proportion of laparoscopy patients who converted to laparotomy. It should be noted that the FACT-G scores of laparoscopy patients who converted to laparotomy approached the findings of those randomly assigned to laparotomy (Fig 2). Last, the modest differences found in return to work might be accounted for by employers' sickness leave plans that allowed for a specified time for patients to be out sick.
Long-term QoL findings could be affected if a difference is found in survival when comparing the two treatment arms. We also intended to measure the effect of the two surgical techniques on sexual functioning. However, only 45% (n = 362) answered questions on sexual functioning at baseline, decreasing to 38% (n = 307) at 6 months. This was partly due to the number of patients without sexual partners, in addition to those who refused to answer the sexual functioning questions.
In conclusion, although the FACT-G did not reach the MID between surgical groups, and there were only modest statistically significant improvements in QoL in laparoscopy compared with laparotomy patients in return to work and BI, the significant improvement in all QoL variables except for Fear of Recurrence in patients undergoing laparoscopy provides some support for a QoL advantage in the use of laparoscopy over laparotomy.
Appendix
The following GOG institutions participated in the quality of life component of GOG 2222 (LAP-2): Abington Memorial Hospital, Walter Reed Army Medical Center, University of Minnesota Medical School, University of Mississippi Medical Center, University of Pennsylvania Cancer Center, University of California at San Diego, University of Iowa Hospitals and Clinics, University of Texas Southwestern Medical Center at Dallas, Indiana University School of Medicine, University of California Medical Center at Irvine, Tufts-New England Medical Center, Rush-Presbyterian-St Luke's Medical Center, University of New Mexico, The Cleveland Clinic Foundation, State University of New York at Stony Brook, Washington University School of Medicine, Memorial Sloan-Kettering Cancer Center, Columbus Cancer Council, The University of Texas M. D. Anderson Cancer Center, University of Massachusetts Medical School, Women's Cancer Center, University of Oklahoma, Tacoma General Hospital, Tampa Bay Cancer Consortium, Gynecologic Oncology Network, Fletcher Allen Health Care, University of Wisconsin Hospital, Women and Infants Hospital, and Community Clinical Oncology Program.
Footnotes
Supported by National Cancer Institute grants to the Gynecologic Oncology Group (GOG) Administrative Office (Grant No. CA 27469) and the GOG Statistical and Data Center (Grant No. CA 37517). J.L.W. was supported by GOG.
Presented in part at the Society of Gynecologic Oncology 37th Annual Meeting on Women's Cancer, March 22-26, 2006, Palm Springs, CA.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Alice B. Kornblith, David Cella
Provision of study materials or patients: Nick M. Spirtos
Data analysis and interpretation: Helen Q. Huang, David Cella
Manuscript writing: Alice B. Kornblith, Helen Q. Huang, Joan L. Walker, Nick M. Spirtos, David Cella
Final approval of manuscript: Alice B. Kornblith, Helen Q. Huang, Joan L. Walker, Jacob Rotmensch, David Cella
REFERENCES
- 1.Walker JL, Piedmonte MR, Spirtos NM, et al. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group study LAP2. J Clin Oncol. 2009;27:5331–5336. doi: 10.1200/JCO.2009.22.3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scribner DR, Jr, Mannel RS, Walker JL, et al. Cost analysis of laparoscopy versus laparotomy for early endometrial cancer. Gynecol Oncol. 1999;75:460–463. doi: 10.1006/gyno.1999.5606. [DOI] [PubMed] [Google Scholar]
- 3.Boike GM, Miller CE, Spirtos NM, et al. Incisional bowel herniations after operative laparoscopy: A series of nineteen cases and review of the literature. Am J Obstet Gynecol. 1995;172:1726–1733. doi: 10.1016/0002-9378(95)91404-8. [DOI] [PubMed] [Google Scholar]
- 4.Childers JM, Brzechffa PR, Hatch KD, et al. Laparoscopically assisted surgical staging (LASS) of endometrial cancer. Gynecol Oncol. 1993;51:33–38. doi: 10.1006/gyno.1993.1242. [DOI] [PubMed] [Google Scholar]
- 5.Eltabbakh GH, Shamonki MI, Moody JM, et al. Laparoscopy as the primary modality for the treatment of women with endometrial carcinoma. Cancer. 2001;91:378–387. doi: 10.1002/1097-0142(20010115)91:2<378::aid-cncr1012>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 6.Fowler JM. The role of laparoscopic staging in the management of patients with early endometrial cancer. Gynecol Oncol. 1999;73:1–3. doi: 10.1006/gyno.1999.5385. [DOI] [PubMed] [Google Scholar]
- 7.Spirtos NM, Schlaerth JB, Gross GM, et al. Cost and quality-of-life analyses of surgery for early endometrial cancer: Laparotomy versus laparoscopy. Am J Obstet Gynecol. 1996;174:1795–1799. doi: 10.1016/s0002-9378(96)70212-0. [DOI] [PubMed] [Google Scholar]
- 8.Homesley HD, Boike C, Spiegel GW. Feasibility of laparoscopic management of presumed stage I endometrial carcinoma and assessment of accuracy of myoinvasion estimates by frozen section: A Gynecologic Oncology Group Study. Int J Gynecol Cancer. 2004;14:341–347. doi: 10.1111/j.1048-891x.2004.014219.x. [DOI] [PubMed] [Google Scholar]
- 9.Zullo F, Palomba S, Russo T, et al. A prospective randomized comparison between laparoscopic and laparotomic approaches in women with early stage endometrial cancer: A focus on the quality of life. Am J Obstet Gynecol. 2005;193:1344–1352. doi: 10.1016/j.ajog.2005.02.131. [DOI] [PubMed] [Google Scholar]
- 10.Weeks JC, Nelson H, Gelber S, et al. Clinical Outcomes of Surgical Therapy (COST) Study Group: Short-term quality of life outcomes following laparoscopic-assisted colectomy vs. open colectomy for colon cancer—A randomized trial. JAMA. 2002;287:321–328. doi: 10.1001/jama.287.3.321. [DOI] [PubMed] [Google Scholar]
- 11.Braga M, Frasson M, Vignali A, et al. Laparoscopic vs. open colectomy in cancer patients: Long-term complications, quality of life and survival. Dis Colon Rectum. 2005;48:2217–2223. doi: 10.1007/s10350-005-0185-7. [DOI] [PubMed] [Google Scholar]
- 12.Walker JL, Mannel RS. The role of laparoscopy in the management of endometrial cancer. In: Coukos G, Rubin SC, editors. Cancer of the Uterus. New York, NY: Marcel Dekker; 2005. pp. 275–304. [Google Scholar]
- 13.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy Scale: Development and validation of the general measure. J Clin Oncol. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 14.Stewart AL, Ware JE., Jr . Measuring Functioning and Well-Being. Durham, NC: Duke University Press; 1992. [Google Scholar]
- 15.Daut RL, Cleeland CS, Flanery RC. Development of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain. 1983;17:197–210. doi: 10.1016/0304-3959(83)90143-4. [DOI] [PubMed] [Google Scholar]
- 16.Greenberg DB, Kornblith AB, Herndon JE, et al. Quality of life of adult leukemia survivors treated on clinical trials of the Cancer and Leukemia Group B from 1971-1988: Predictors for later psychological distress. Cancer. 1997;80:1936–1944. doi: 10.1002/(sici)1097-0142(19971115)80:10<1936::aid-cncr10>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 17.Nunnally JC, Bernstein IH. Psychometric Theory. ed 3. New York, NY: McGraw-Hill; 1994. [Google Scholar]
- 18.Yost KJ, Eton DT. Combining distribution and anchor-based approaches to determine minimally important differences: The FACIT experience. Eval Health Prof. 2005;28:172–191. doi: 10.1177/0163278705275340. [DOI] [PubMed] [Google Scholar]
- 19.Brucker PS, Yost K, Cashy J, et al. General population and cancer patient norms for the Functional Assessment of Cancer Therapy General (FACT-G) Eval Health Prof. 2005;28:192–211. doi: 10.1177/0163278705275341. [DOI] [PubMed] [Google Scholar]