Abstract
Background:
Reactive telephone helplines for smoking cessation (where all calls to counselors are smoker initiated) are increasingly used in the United States. However, limited data from randomized controlled trials are available on their effectiveness. The study objective was to evaluate the real-world effectiveness of reactive telephone counseling for smoking cessation using a randomized controlled trial study design.
Methods:
The study was implemented during a period from 2003 to 2006 to evaluate a reactive telephone helpline run by the American Lung Association chapter of Illinois-Iowa. The 990 new callers, all adult current smokers who called the helpline, were randomized on their first call into one of the two following groups: a control group that received only mailed self-help literature (n = 496); and a study group that received supplemental live reactive telephone counseling (n = 494). Telephone follow-up was completed at 1, 3, 6, and 12 months after study enrollment by interviewers blinded to group assignment. Seven-day point prevalence rates of self-reported abstinence at follow-up evaluations were compared between the two groups using an intent-to-treat design.
Results:
The two groups did not differ significantly in baseline demographics and smoking-related behavior. The abstinence rates (ranging between 0.09 and 0.15) were not significantly different between the two groups at 1-, 3-, 6-, and 12-month follow-up evaluations. Post hoc subgroup analysis showed that black callers had lower abstinence rates at the 3- and 12-month follow-up evaluations as compared with white callers.
Conclusion:
Supplemental live, reactive telephone counseling does not provide greater success in smoking cessation than self-help educational materials alone.
Twenty percent of all adult Americans currently report smoking cigarettes, a preventable behavior associated with tremendous personal and societal costs.1 Between 1997 and 2001, smoking caused approximately 438,000 premature deaths annually and approximately $167 billion in annual health-care costs in the United States.2 Reducing tobacco use is a key component of Healthy People 2010, the national action plan for improving the health of all Americans during the first decade of the 21st century.3
Telephone counseling against smoking has become increasingly popular in the United States and worldwide, and may play a major role in addressing this significant public health problem. The following two primary forms of telephone counseling are currently used: “proactive counseling,” in which calls to smokers are initiated by a counselor according to a prearranged schedule; and “reactive counseling,” in which all calls to counselors are smoker initiated. If trained human counselors (as opposed to automated messages) provide the latter service, it is called live reactive counseling. Although several randomized controlled trials4–9 have found proactive telephone counseling to be efficacious, studies10,11 of reactive telephone counseling have been criticized for lack of randomization and adequate controls. Therefore, the US Department of Health and Human Services clinical practice guidelines10,11 for treating tobacco use and dependence called for additional research on the effectiveness of reactive telephone helplines.
The objective of this randomized controlled study was to evaluate the real-world effectiveness of combined live reactive telephone counseling and self-help educational materials against smoking. We hypothesized that the combination of live reactive telephone counseling and self-help educational materials would provide greater success in smoking cessation than self-help educational materials alone.
Materials and Methods
Design Overview
A randomized controlled trial was implemented comprising 990 new callers, all adult current smokers, who called a reactive telephone helpline run by the American Lung Association chapter of Illinois-Iowa during the period January 2003 to December 2005. Eligible subjects were randomized on their first call (prior to offering counseling) into one of the following two groups: a control group that received only self-help literature by mail; and a study group that received supplemental live reactive telephone counseling. The inclusion and exclusion criteria and the randomization process for the study are provided in the online supplement. Verbal informed consent was obtained from all eligible subjects. The protocol was approved by the local institutional review board (Springfield Committee for Research in Human Subjects; Springfield, IL).
Interventions
Self-Help Educational Material:
This educational material, called “Freedom from Smoking,”12 was specially developed by the American Lung Association and contained information about smoking cessation methods.
Live Telephone Counseling:
All counselors were experienced professionals who were similarly trained and used a standardized state-of-the-art counseling protocol to develop an individualized plan for quitting for each caller. The protocol was based on a compilation of experience of helpline team professionals with input from other successful helplines and conformed to the 2004 state-of-the-art guidelines by the US Centers for Disease Control and Prevention.13 The underlying behavioral basis for this protocol was the transtheoretical model as applied to smoking cessation,14–17 supplemented by the principles of social cognitive theory,18 patient-centered counseling strategy,19–21 and recommendations by clinical experts.13 Additional details about the protocol are provided in the online supplement. Due to the reactive nature of the helpline, the callers themselves determined the pattern of counseling. The counselors encouraged but did not regulate use of the helpline by smokers, staying true to the current real-world character of reactive telephone helplines. As a result, callers in the study group received a variable amount of counseling but always at least one counseling session.
Data Collection and Follow-up
Information about demographics and smoking habits was obtained from all eligible subjects during the first call. Standardized instruments were used to evaluate smoking behavior,17,22–24 as detailed in the online supplement. Questionnaires to determine self-efficacy and the Prochaska transtheoretical model of behavior change had a κ value of 0.7222 and a Cronbach α coefficient value of > 0.80,23 respectively. Follow-up information about smoking behavior was collected, via telephone calls, at 1, 3, 6, and 12 months after the date of enrollment. The interviewer assessing outcomes was blinded to the initial randomized assignment status at the time of the follow-up interview.
Steps To Minimize Subject Attrition
These steps included making multiple attempts (up to 25) to reach subjects by telephone, encouraging subjects to give the telephone numbers of two additional contacts, mailing $5 checks to subjects after each follow-up interview, using Internet directories to track changed telephone numbers, and mailing prestamped postcards requesting contact information to those subjects who could not be traced by telephone.
Outcomes
Self-reported 7-day point prevalence abstinence rates were calculated at the 1-, 3-, 6- and 12-month follow-up evaluations. This outcome measure is sensitive to quitting initiated at any point prior to assessment and has the highest concurrent validity of all abstinence measures.25 Abstinence was defined as “not a single puff” for the designated period of 7 days minimum and no use of other tobacco products.25,26 Those subjects whom the researchers were unable to contact were designated as never having made any quit attempt during the period of loss to follow-up. This approach is consistent with the usual practice in intent-to-treat trials of smoking cessation interventions.25
Statistical Analysis
Statistical analysis was based on an intent-to-treat approach using a statistical software package (SPSS, version 16.0; SPSS Inc; Chicago, IL). A two-sample t test was used for continuous univariate analyses, Pearson χ2 statistic was used for categorical univariate analyses, and logistic regression was used for multivariable analyses. Covariates included the baseline number of cigarettes smoked daily, baseline educational status, baseline confidence level in quitting, and the use of pharmacologic aids (at the 6- and 12-month evaluations). Additional post hoc subgroup analyses restricted to blacks and whites were performed.
Power Analysis
This study was designed to have a minimum of 80% power to evaluate a minimum effect size at the 12-month follow-up of 8% between the two strategies (20% vs 12%, respectively) with a two-tailed α level of 0.05. Before starting the study, the sample size of 990 subjects was calculated to assume up to 50% attrition, as had been previously reported in the literature.4,7,27,28
Additional details about the methods used in the study are presented in the online supplement. The sponsor of the study was not involved in the study design, conduct, and reporting.
Results
Subject Characteristics
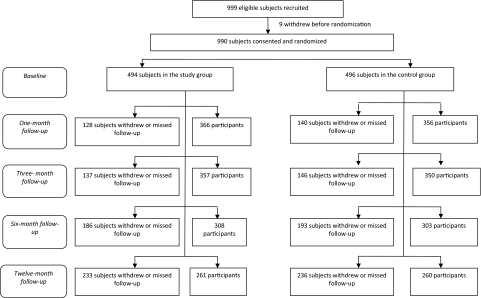
Of the 999 eligible subjects who were screened, 990 subjects were randomized into one of the following two groups: a control group that received only self-help literature by mail (n = 496); and a study group that received supplemental live reactive telephone counseling (n = 494). Seven hundred twenty-two subjects (72.9%), 707 subjects (71.4%), 611 subjects (61.7%), and 521 subjects (52.6%), respectively, completed follow-up at 1, 3, 6, and 12 months (Fig 1).
Figure 1.
Schematic flow diagram of recruitment, randomization, and follow-up in the study (using the Consolidated Standards of Reporting Trials [or CONSORT] standards). Note: At the 1-month follow-up, 722 subjects participated, 44 participants withdrew, and 224 subjects missed follow-up. At the 3-month follow-up, 707 subjects participated, 55 participants withdrew, and 228 subjects missed follow-up. At the 6-month follow-up, 611 subjects participated, 74 participants withdrew, and 305 subjects missed follow-up. At the 12-month follow up, 521 subjects participated, 95 participants withdrew, and 374 subjects missed follow-up.
The study and control groups did not differ significantly with respect to baseline demographic and smoking-related characteristics (Tables 1, 2). These results indicate the success of our randomization strategy. A robust female participation (n = 619, 62.5%) and black participation (n = 337; 34.0%) [Table 1] was noted, which supports the validity of our study. Only 53.5% of the study group and 56.0% of the control group subjects at the baseline evaluation were at least somewhat confident of quitting smoking (Table 2), reflecting the poor overall motivational status of the helpline callers.
Table 1.
Selected Demographic Characteristics of the Study and Control Groups at Baseline Evaluation
| Study Characteristics | Study Group | Control Group | p Value |
|---|---|---|---|
| Mean age, yr | 42.84 ± 13.46 | 42.48 ± 13.29 | 0.68 |
| (n = 492) | (n = 496) | ||
| Weight, lb | 172.34 ± 44.66 | 175.94 ± 49.66 | 0.23 |
| (n = 488) | (n = 491) | ||
| Sex, % | (n = 494) | (n = 496) | 0.52 |
| Male | 38.5 | 36.5 | |
| Female | 61.5 | 63.5 | |
| Race | (n = 492) | (n = 495) | 0.46 |
| White | 308 (62.6) | 295 (59.6) | |
| Black | 164 (33.3) | 173 (34.9) | |
| Others | 20 (4.1) | 27 (5.5) | |
| Education completed | (n = 493) | (n = 493) | 0.53 |
| Up to high school/GED | 278 (56.4) | 261 (52.9) | |
| Some college | 157 (31.8) | 172 (34.9) | |
| 4-yr college degree or greater | 58 (11.8) | 60 (12.2) | |
| Employment status | (n = 493) | (n = 496) | 0.56 |
| Working (full or part time) | 275 (55.8) | 272 (54.8) | |
| Student (full or part time) | 17 (3.4) | 12 (2.4) | |
| Unemployed | 201 (40.8) | 212 (42.7) | |
| Annual household income | (n = 445) | (n = 462) | 0.54 |
| < $35,000 | 305 (68.5) | 301 (65.2) | |
| $35,000–$49,999 | 53 (11.9) | 63 (13.6) | |
| ≥ $50,000 | 87 (19.6) | 98 (21.2) | |
| Place of residence | (n = 493) | (n = 495) | 0.72 |
| Urban | 271 (55.0) | 272 (54.9) | |
| Rural | 116 (23.5) | 108 (21.8) | |
| Semi-urban | 106 (21.5) | 115 (23.2) |
Values are given as the mean ± SD or No. (%), unless otherwise indicated. GED = General Education Development credential in the United States (equivalent to a high school diploma). There were 494 subjects assigned to the study group and 496 to the control group. The varying n values for each item reflect missing data.
Table 2.
Selected Smoking-Related Characteristics of the Study and Control Groups at Baseline Evaluation
| Study Characteristics | Study Group | Control Group | p Value |
|---|---|---|---|
| Cigarettes smoked daily, No. | 23.19 ± 12.58 | 22.01 ± 12.61 | 0.14 |
| (n = 494) | (n = 496) | ||
| Time to first cigarette after awakening | (n = 494) | (n = 496) | 0.16 |
| < 5 min | 256 (51.8) | 242 (48.8) | |
| 6–30 min | 165 (33.4) | 156 (31.5) | |
| 31–60 min | 44 (8.9) | 52 (10.5) | |
| > 60 min | 29 (5.9) | 46 (9.3) | |
| Transtheoretical behavioral stage of change | (n = 493) | (n = 495) | 0.29 |
| Precontemplation | 0 (0.0) | 2 (0.4) | |
| Contemplation | 242 (49.1) | 231 (46.7) | |
| Preparation | 251 (50.9) | 262 (52.9) | |
| Self-efficacy score on quitting smoking | 35.44 ± 6.47 | 35.26 ± 6.10 | 0.65 |
| (n = 492) | (n = 496) | ||
| Self-reported confidence level in quitting | (n = 494) | (n = 496) | 0.91 |
| Very confident | 68 (13.8) | 77 (15.5) | |
| Confident | 73 (14.8) | 77 (15.5) | |
| Somewhat confident | 123 (24.9) | 124 (25.0) | |
| Not confident | 196 (39.7) | 186 (37.5) | |
| Do not know | 251 (6.9) | 32 (6.5) |
Values are given as the mean ± SD or No. (%), unless otherwise indicated. A higher mean score revealed a lower self-efficacy level. There were 494 subjects assigned to the study group and 496 to the control group. The varying n values for each item reflects missing data.
Effectiveness of Live Reactive Telephone Counseling
Univariate analyses showed no significant differences in self-reported abstinence between the study and control groups at the 1-month (0.10 vs 0.09, respectively), 3-month (0.14 vs 0.13, respectively), 6-month (0.15 vs 0.15, respectively), and 12-month (0.14 vs 0.15, respectively) follow-up evaluations, as analyzed by intent-to-treat design (Tables 3, 4). Similar results were obtained by not using intent-to-treat design (Tables 3, 4) and using multivariable analyses after adjusting for covariates (Table 4).
Table 3.
Comparison of 7-Day Point Prevalence Rates for Abstinence From Smoking Between Study and Control Groups
| Follow-up Evaluation | Study Group | Control Group | p Value* |
|---|---|---|---|
| Intent-to-treat design | |||
| 1 mo | 0.10 (50/494) | 0.09 (45/496) | 0.58 |
| 3 mo | 0.14 (67/494) | 0.13 (64/496) | 0.76 |
| 6 mo | 0.15 (75/494) | 0.15 (76/496) | 0.95 |
| 12 mo | 0.14 (70/494) | 0.15 (73/496) | 0.67 |
| Not using intent-to-treat design | |||
| 1 mo | 0.14 (50/366) | 0.13 (45/356) | 0.69 |
| 3 mo | 0.19 (67/357) | 0.18 (64/350) | 0.87 |
| 6 mo | 0.24 (75/308) | 0.25 (76/303) | 0.83 |
| 12 mo | 0.27 (70/262) | 0.28 (73/259) | 0.71 |
Values are given as 7-day point prevalence rate (subjects abstaining from smoking for at least 7 days/total population in each study arm), unless otherwise indicated. The No. of subjects abstaining from smoking for at least 7 days varies in the “not using intent-to-treat” analysis because of attrition.
*The χ2 test was used for these analyses.
Table 4.
Univariate and Multivariable Analyses Comparing 7-Day Point Prevalence of Abstinence From Smoking Between Study and Control Groups
| Follow-up Evaluation* | Unadjusted |
Adjusted |
||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | N | OR (95% CI) | p Value | N | |
| Using intent-to-treat design | ||||||
| 1 mo | 1.13 (0.74–1.72) | 0.58 | 95/990 | 1.16 (0.76–1.77) | 0.50 | 95/986 |
| 3 mo | 1.06 (0.73–1.53) | 0.76 | 131/990 | 1.13 (0.78–1.64) | 0.53 | 129/986 |
| 6 mo | 0.99 (0.70–1.40) | 0.95 | 151/990 | 0.99 (0.68–1.42) | 0.95 | 150/986 |
| 12 mo | 0.93 (0.65–1.32) | 0.67 | 143/990 | 0.90 (0.62–1.31) | 0.59 | 141/986 |
| Not using intent-to-treat design | ||||||
| 1 mo | 1.09 (0.71–1.69) | 0.69 | 95/722 | 1.13 (0.73–1.74) | 0.59 | 95/719 |
| 3 mo | 1.03 (0.71–1.51) | 0.87 | 131/707 | 1.10 (0.75–1.63) | 0.61 | 129/703 |
| 6 mo | 0.96 (0.67–1.39) | 0.83 | 151/611 | 1.00 (0.68–1.46) | 0.99 | 150/608 |
| 12 mo | 0.90 (0.62–1.33) | 0.71 | 143/521 | 0.93 (0.63–1.38) | 0.71 | 141/518 |
Values are given as No. of subjects abstaining from smoking for at least 7 days/total population in each study arm, unless otherwise indicated. The total population in each study arm varies between adjusted and unadjusted analysis because of missing covariate values. OR = odds ratio.
*For 1- and 3-month follow-up, data were adjusted in multivariable logistic regression analysis for baseline number of cigarettes smoked daily, baseline educational status, and baseline confidence level in quitting. For 6- and 12-month follow-up, data were additionally adjusted for pharmacologic aids used.
Use of pharmaceutical aids for smoking cessation did not differ significantly between the study and control groups before calling the helpline (ever used aids, 0.52 vs 0.50, respectively; p = 0.48), and at the 6-month follow-up evaluation (0.25 vs 0.23, respectively; p = 0.58) and the 12-month follow-up evaluation (0.21 vs 0.18, respectively; p = 0.14) [online supplement Table 1]. Further, a pilot study analyzing salivary cotinine levels (using methods detailed in the online supplement) biochemically validated the self-reported abstinence in five of eight control subjects (63%) and seven of eight study group subjects (88%) in a small convenience sample; these proportions did not differ significantly between the groups (p = 0.57).
Subgroup Analysis of Black and White Callers
Post hoc subgroup analyses revealed no significant differences in abstinence rates between the study and control groups when the analyses were restricted to either blacks only or to whites only (data not shown; p ≥ 0.52 for interactions between race and randomization assignment on abstinence at each evaluation). However, a univariate analysis of pooled data revealed that black callers had lower abstinence rates than white callers at the 3-month follow-up evaluation (0.10 vs 0.15, respectively; p = 0.02) and the 12-month follow-up evaluation (0.12 vs 0.17, respectively; p = 0.04) [Table 5]. In addition, a significantly lower proportion of blacks used pharmaceutical aids compared with white callers prior to calling the helpline (ever use aids, 0.35 vs 0.60, respectively; p < 0.01), and at the 6-month follow-up evaluation (0.20 vs 0.27, respectively; p = 0.01), and 12-month follow-up evaluation (0.12 vs 0.24, respectively; p < 0.01) [online supplement Table 2].
Table 5.
Post Hoc Subgroup Analysis Comparing 7-Day Point Prevalence Rates for Abstinence From Smoking Between Black and White Callers
| Follow-up Evaluation | Blacks | Whites | p Value* |
|---|---|---|---|
| Intent-to-treat design† | |||
| 1 mo | 0.08 (26/337) | 0.11 (64/603) | 0.15 |
| 3 mo | 0.10 (33/337) | 0.15 (64/603) | 0.02 |
| 6 mo | 0.14 (46/337) | 0.16 (98/603) | 0.29 |
| 12 mo | 0.12 (40/337) | 0.17 (101/603) | 0.04 |
| Not using intent-to-treat design | |||
| 1 mo | 0.10 (26/248) | 0.14 (64/442) | 0.14 |
| 3 mo | 0.14 (33/236) | 0.21 (92/438) | 0.03 |
| 6 mo | 0.23 (46/201) | 0.26 (98/380) | 0.44 |
| 12 mo | 0.22 (40/177) | 0.31(101/325) | 0.04 |
Values are given as the 7-day point prevalence rate (No. of subjects abstaining from smoking for at least 7 days/total population in each group of callers). The total population in each group of callers varies in the “not using intent-to-treat” analysis because of attrition. Data from the two study arms were pooled for race-specific analysis. The interaction between race and randomization assignment on the point prevalence abstinence (using race as a binary variable) was not significant at each evaluation (p = 0.82 at 1 month; p = 0.12 at 3 months; p = 0.32 at 6 months; p = 0.15 at 12 months).
*The χ2 test was used for these analyses.
†Intent-to-treat analysis excluded 50 participants; 47 belonged to racial groups that were neither black nor white, and 3 had missing data.
Study Attrition
This study had a relatively high 12-month attrition rate of 47.4% due to voluntary withdrawals and missed follow-up appointments (Fig 1), which were partly influenced by the mass migration caused by Hurricane Katrina along the Gulf coast in 2005. However, the attrition was comparable to other large studies in this field of research4,7,27,28 and was not different between the study and control groups (online supplement Table 3). Baseline variables related to smoking were not significantly different between those who completed the study at 12 months as compared with those who did not (online supplement Table 4).
Discussion
This randomized controlled trial demonstrates that the combination of live reactive telephone counseling and self-help educational material does not provide greater success in smoking cessation than self-help educational materials alone. The abstinence rates in this study (range, 0.09 to 0.15) were comparable to those described in the literature for other self-help approaches in quitting smoking (0.14; 95% CI, 0.13 to 0.16).29 In addition, we noted that black callers had significantly lower 7-day point prevalence abstinence rates at 3- and 12-month follow- up evaluations, compared with white callers in the study. Studies30 of other smoking cessation interventions have also reported similar racial differences.
It is recommended that health providers prescribe behavioral counseling and pharmacologic assistance to all smokers attempting to quit.31 However, health providers are challenged to provide effective behavioral treatment due to time and fiscal constraints in their real-world practice. Further, few smokers are willing to attend traditional behavioral therapy clinics repeatedly.32,33 These issues have led to increased acceptance of telephone counseling to aid in smoking cessation. Although several randomized controlled trials4–9 have found proactive telephone counseling to be efficacious, studies10,11 of reactive telephone counseling have been criticized for lack of randomization and adequate controls.
Three distinct approaches have been used in the past to evaluate the effectiveness of reactive telephone helplines. First, prospective studies34,35 have demonstrated point prevalence abstinence of 22 to 24% at the 1-year follow-up of callers who received reactive counseling. Second, randomized or quasi-randomized controlled trials have been performed in which the intervention included access to a reactive helpline. Two of these studies4,36 found a beneficial effect of reactive telephone counseling in producing abstinence, whereas the third study37 found telephone counseling to be less effective than mailed self-help educational material in preventing relapse. Third, randomized controlled trials in which recruitment to the helpline was reactive but subsequent counseling was proactive have been performed. This study design merges reactive and proactive approaches and has been sometimes called “callback” counseling. Several such studies6–8,27,38–40 have demonstrated higher abstinence rates in the callback group, compared to control groups receiving self-help material. However, this study design has been criticized as more of an evaluation of proactive rather than reactive telephone counseling. Our study is unique in that it used both a randomized controlled study design and a reactive approach to recruitment and intervention, thereby staying true to the real-world character of reactive telephone helplines.
Our findings indicate that supplemental live reactive telephone counseling in its current form may be ineffective or inadequate. We primarily attribute the inability of the study to detect significant differences between the two groups to the weak nature of the intervention itself, which depended on the callers' motivational status. This conclusion is supported by our previous analysis41 of 286 subjects in the study group showing an infrequent use of the reactive telephone helpline (mean [± SD], 3.3 ± 4.6 calls per subject per year; median, 1.8 calls per subject per year [interquartile range, 1.0 to 3.3 calls per subject per year]; difference, 35.5 calls per subject per year [range, 1.0 to 36.5 calls per subject per year]). Similarly, low use of reactive helplines for smoking cessation at a community level has been described in the literature.4,34,36,42,43 We therefore support giving consideration to incorporation of some type of callback counseling instead as a method for future study. For example, callers to a reactive helpline could be asked whether a counselor could call them back at mutually agreeable prescheduled times for additional counseling, thus building in both follow-up and accountability. Furthermore, because black callers had lower abstinence rates at follow-up as compared to white callers, we suggest that helplines target specific interventions toward helping black (and other underrepresented minority) population groups to quit smoking, including but not limited to encouraging use of pharmaceutical aids.
Our study has several limitations. First, the high attrition rates reported in this and other similar studies27,28 are likely related to the poor overall motivational status of participants, a real-world problem in both studying this issue and delivering assistance. However, attrition rates between the two study groups (online supplement Table 3) and smoking-related characteristics between those who completed the study at 12 months and those who did not, were not significantly different (online supplement Table 4). This minimizes the likelihood of selection bias explaining our results. Second, differential information bias could arise if subjects in the study group reported abstinence falsely to directly or indirectly please the telephone counselor. However, our small biochemical validation study suggested that this bias was likely not significant. Third, participation bias may arise from increased motivation to quit smoking simply because of increased telephone contact with researchers and a small stipend offered for each follow-up call. However, this bias is likely nondifferential because it applies equally to both groups. Fourth, our study compared supplemental reactive telephone counseling with self-help educational materials alone to assess current practices at the specific helpline being modeled. However, the effect in the absence of self-help educational materials or in combination with other types of self-help interventions cannot be determined from this study. Finally, the helpline studied did not provide 24-h live reactive telephone counseling 7 days a week. However, these limitations do not detract from the significance of our study because we are not aware of any reactive telephone helplines that currently provide live counseling 24 h per day, 7 days per week.
The strengths of this study arise from the high public health significance of the problem, a relatively large sample size, the intent-to-treat analysis design, repeat assessments of multiple outcome measures over a 12-month period, strong female and black participation, blinding to group assignment of the interviewer assessing outcomes, and, most importantly, a randomized controlled design that did not fundamentally alter the reactive nature of the intervention being studied. Finally, this study was conducted under real-world conditions, making application of the findings generalizable and fairly straightforward.
This randomized controlled trial demonstrates that supplemental live reactive telephone counseling does not provide greater success in smoking cessation than self-help educational materials alone. These findings suggest that reactive telephone counseling in its current form may be ineffective or inadequate, possibly due to its infrequent use because of the poor motivational status of the callers. Consideration should be given to implementation of callback counseling, which has been previously demonstrated to be efficacious.
Acknowledgments
Author contributions: Drs. Sood and Verhulst contributed to the conception and design, data analysis and interpretation, drafting of the manuscript, statistical analysis, the obtaining of funding, and supervision. Ms. Andoh contributed to data analysis and interpretation, and statistical analysis. Ms. Ganesh and Ms. Edson were involved with data acquisition; critical revision of the manuscript for important intellectual content; and administrative technical, or material support. Dr. Hopkins-Price contributed to the conception and design, data analysis and interpretation, the obtaining of funding, and supervision. All authors contributed to data acquisition; critical revision of the manuscript for important intellectual content; and administrative, technical, or material support.
Financial/nonfinancial disclosures: The authors have reported to the ACCP that no significant conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Footnotes
Funding/Support: This study was supported by American Lung Association grant CG-870-N. Dr. Sood was also supported by the University of New Mexico Clinical Translational Science Center Scholar Award and Department of Health and Human Services/National Institutes of Health/National Center for Research Resources/General Clinical Research Center grant No. 5M01 RR00997.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal.org/site/misc/reprints.xhtml).
For editorial comment see page 1199
References
- 1.Centers for Disease Control and Prevention. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. Behavioral risk factor surveillance system survey data. [Google Scholar]
- 2.Fellows JL, Trosclair A, Adams EK, et al. Annual smoking-attributable mortality, years of potential life lost, and economic costs: United States, 1995–1999. MMWR Morb Mortal Wkly Rep. 2002;51:300–303. [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services. Washington, DC: US Department of Health and Human Services; 2000. Healthy people 2010 [Conference edition, in two volumes] [Google Scholar]
- 4.Ossip-Klein DJ, Giovino GA, Megahed N, et al. Effects of a smoker's hotline: results of a 10-county self-help trial. J Consult Clin Psychol. 1991;59:325–332. doi: 10.1037//0022-006x.59.2.325. [DOI] [PubMed] [Google Scholar]
- 5.Zhu SH, Anderson CM, Johnson CE, et al. A centralised telephone service for tobacco cessation: the California experience. Tob Control. 2000;9(suppl):II48–II55. doi: 10.1136/tc.9.suppl_2.ii48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu SH, Anderson CM, Tedeschi G, et al. Evidence of real-world effectiveness of a telephone quitline for smokers. N Engl J Med. 2002;347:1106–1109. doi: 10.1056/NEJMsa020660. [DOI] [PubMed] [Google Scholar]
- 7.Zhu SH, Tedeschi G, Anderson CM, et al. Telephone counseling as adjuvant treatment for nicotine replacement therapy in a “real-world” setting. Prev Med. 2000;31:357–363. doi: 10.1006/pmed.2000.0720. [DOI] [PubMed] [Google Scholar]
- 8.Zhu SH, Stretch V, Balabanis M, et al. Telephone counseling for smoking cessation: effects of single-session and multiple-session interventions. J Consult Clin Psychol. 1996;64:202–211. doi: 10.1037//0022-006x.64.1.202. [DOI] [PubMed] [Google Scholar]
- 9.Zhu SH, Anderson CM. Bridging the clinical and public health approaches to smoking cessation: California Smokers' Helpline. In: Jammer MS, Stokols D, editors. Promoting human wellness: new frontiers for research, practice and policy. Berkeley, CA: University of California Press; 2000. [Google Scholar]
- 10.Fiore MC, Bailey WC, Cohen JJ, et al. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2000. Treating tobacco use and dependence: clinical practice guideline. [Google Scholar]
- 11.Fiore MC, Jaen CR, Baker TB. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2008. May, Treating tobacco use and dependence: 2008 update; clinical practice guideline. [Google Scholar]
- 12.American Lung Association. Quitting for life: 2000 edition. South Deerfield, MA: Channing L. Bete; 1998. [Google Scholar]
- 13.Centers for Disease Control and Prevention. Final edition. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. Telephone quitlines: a resource for development, implementation, and evaluation. [Google Scholar]
- 14.Prochaska JO, DiClemente CC. Toward a comprehensive model of change. In: Miller WR, Heather N, editors. Treating addictive behaviors. New York, NY: Plenum Press; 1986. [Google Scholar]
- 15.Prochaska JO, DiClemente CC, Velicer WF, et al. Predicting change in smoking status for self-changers. Addict Behav. 1985;10:395–406. doi: 10.1016/0306-4603(85)90036-x. [DOI] [PubMed] [Google Scholar]
- 16.DiClemente CC, Prochaska JO, Fairhurst SK, et al. The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. J Consult Clin Psychol. 1991;59:295–304. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- 17.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 18.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 19.Ockene JK, Quirk ME, Goldberg RJ, et al. A residents' training program for the development of smoking intervention skills. Arch Intern Med. 1988;148:1039–1045. [PubMed] [Google Scholar]
- 20.Ockene JK. Physician-delivered interventions for smoking cessation: strategies for increasing effectiveness. Prev Med. 1987;16:723–737. doi: 10.1016/0091-7435(87)90054-5. [DOI] [PubMed] [Google Scholar]
- 21.Ockene JK, Kristeller J, Goldberg R, et al. Increasing the efficacy of physician-delivered smoking interventions: a randomized clinical trial. J Gen Intern Med. 1991;6:1–8. doi: 10.1007/BF02599381. [DOI] [PubMed] [Google Scholar]
- 22.Donovan RJ, Jones S, Holman CD, et al. Assessing the reliability of a stage of change scale. Health Educ Res. 1998;13:285–291. doi: 10.1093/her/13.2.285. [DOI] [PubMed] [Google Scholar]
- 23.Velicer WF, Diclemente CC, Rossi JS, et al. Relapse situations and self-efficacy: an integrative model. Addict Behav. 1990;15:271–283. doi: 10.1016/0306-4603(90)90070-e. [DOI] [PubMed] [Google Scholar]
- 24.Abrams DB, Herzog TA, Emmons KM, et al. Stages of change versus addiction: a replication and extension. Nicotine Tob Res. 2000;2:223–229. doi: 10.1080/14622200050147484. [DOI] [PubMed] [Google Scholar]
- 25.Hughes JR, Keely JP, Niaura RS, et al. Measures of abstinence in clinical trials: issues and recommendations. Nicotine Tob Res. 2003;5:13–25. [PubMed] [Google Scholar]
- 26.Velicer WF, Prochaska JO, Rossi JS, et al. Assessing outcome in smoking cessation studies. Psychol Bull. 1992;111:23–41. doi: 10.1037/0033-2909.111.1.23. [DOI] [PubMed] [Google Scholar]
- 27.Rabius V, McAlister AL, Geiger A, et al. Telephone counseling increases cessation rates among young adult smokers. Health Psychol. 2004;23:539–541. doi: 10.1037/0278-6133.23.5.539. [DOI] [PubMed] [Google Scholar]
- 28.Lipkus IM, McBride CM, Pollak KI, et al. A randomized trial comparing the effects of self-help materials and proactive telephone counseling on teen smoking cessation. Health Psychol. 2004;23:397–406. doi: 10.1037/0278-6133.23.4.397. [DOI] [PubMed] [Google Scholar]
- 29.Fiore MC, Bailey WC, Cohen JJ. Rockville, MD: US Department of Health and Human Services; 2000. Treating tobacco use and dependence: clinical practice guideline. [Google Scholar]
- 30.US Department of Health and Human Services. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking; 1998. Tobacco use among US racial/ethnic minority groups: African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics; a report of the Surgeon General. [Google Scholar]
- 31.Fiore MC, Bailey WC, Cohen SJ, et al. Rockville, MD: Agency for Health Care Policy and Research; 1996. Smoking cessation: clinical practice guideline No. 18. [Google Scholar]
- 32.Owen N, Davies MJ. Smokers' preferences for assistance with cessation. Prev Med. 1990;19:424–431. doi: 10.1016/0091-7435(90)90040-q. [DOI] [PubMed] [Google Scholar]
- 33.Lichtenstein E, Hollis JF. Patient referral to a smoking cessation program: who follows through. J Fam Pract. 1992;34:739–744. [PubMed] [Google Scholar]
- 34.Platt S, Tannahill A, Watson J, et al. Effectiveness of antismoking telephone helpline: follow up survey. BMJ. 1997;314:1371–1375. doi: 10.1136/bmj.314.7091.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Owen L. Impact of a telephone helpline for smokers who called during a mass media campaign. Tob Control. 2000;9:148–154. doi: 10.1136/tc.9.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McFall SL, Michener A, Rubin D, et al. The effects and use of maintenance newsletters in a smoking cessation intervention. Addict Behav. 1993;18:151–158. doi: 10.1016/0306-4603(93)90045-b. [DOI] [PubMed] [Google Scholar]
- 37.Brandon TH, Collins BN, Juliano LM, et al. Preventing relapse among former smokers: a comparison of minimal interventions through telephone and mail. J Consult Clin Psychol. 2000;68:103–113. doi: 10.1037//0022-006x.68.1.103. [DOI] [PubMed] [Google Scholar]
- 38.Smith PM, Cameron R, McDonald PW, et al. Telephone counseling for population-based smoking cessation. Am J Health Behav. 2004;28:231–241. doi: 10.5993/ajhb.28.3.4. [DOI] [PubMed] [Google Scholar]
- 39.Macleod ZR, Charles MA, Arnaldi VC, et al. Telephone counselling as an adjunct to nicotine patches in smoking cessation: a randomised controlled trial. Med J Aust. 2003;179:349–352. doi: 10.5694/j.1326-5377.2003.tb05590.x. [DOI] [PubMed] [Google Scholar]
- 40.Borland R, Segan CJ, Livingston PM, et al. The effectiveness of callback counseling for smoking cessation: a randomized trial. Addiction. 2001;96:881–889. doi: 10.1046/j.1360-0443.2001.9668819.x. [DOI] [PubMed] [Google Scholar]
- 41.Ganesh M, Verhulst S, Edson B, et al. Pattern of use of reactive telephone counseling by smokers [abstract] Proc Am Thorac Soc. 2006;3:A92. [Google Scholar]
- 42.Ossip-Klein DJ, McIntosh S. Quitlines in North America: evidence base and applications. Am J Med Sci. 2003;326:201–205. doi: 10.1097/00000441-200310000-00010. [DOI] [PubMed] [Google Scholar]
- 43.Glasgow RE, Lando H, Hollis J, et al. A stop-smoking telephone help line that nobody called. Am J Public Health. 1993;83:252–253. doi: 10.2105/ajph.83.2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]