Abstract
Objective
Clinical and radiological results of posterior dynamic stabilization using interspinous U (ISU, Coflex™, Paradigm Spine Inc.®, NY, USA) were analyzed in comparison with posterior lumbar interbody fusion (PLIF) in degenerative lumbar spinal stenosis (LSS).
Methods
A retrospective study was conducted for a consecutive series of 61 patients with degenerative LSS between May 2003 and December 2005. We included only the patients completed minimum 24 months follow up evaluation. Among them, 30 patients were treated with implantation of ISU after decompressive laminectomy (Group ISU) and 31 patients were treated with wide decompressive laminectomy and posterior lumbar interbody fusion (PLIF; Group PLIF). We evaluated visual analogue scale (VAS) and Oswestry Disability Index (ODI) for clinical outcomes (VAS, ODI), disc height ratio disc height (DH), disc height/vertebral body length ×100), static vertebral slip (VS) and depth of maximal radiolucent gap between ISU and spinous process) in preoperative, immediate postoperative and last follow up.
Results
The mean age of group ISU (66.2 ± 6.7 years) was 6.2 years older than the mean age of group PLIF (60.4 ± 8.1 years; p = 0.003 ). In both groups, clinical measures improved significantly than preoperative values (p < 0.001). Operation time and blood loss was significantly shorter and lower in group ISU than group PLIF (p < 0.001). In group ISU, the DH increased transiently in immediate postoperative period (15.7 ± 4.5% → 18.6 ± 5.9%), however decreased significantly in last follow up (13.8 ± 6.6%, p = 0.027). Vertebral slip (VS) of spondylolisthesis in group ISU increased during postoperative follow-up (2.3 ± 3.3 → 8.7 ± 6.2, p = 0.040). Meanwhile, the postoperatively improved DH and VS was maintained in group PLIF in last follow up.
Conclusion
According to our result, implantation of ISU after decompressive laminectomy in degenerative LSS is less invasive and provides similar clinical outcome in comparison with the instrumented fusion. However, the device has only transient effect on the postoperative restoration of disc height and reduction of slip in spondylolisthesis. Therefore, in the biomechanical standpoint, it is hard to expect that use of Interspinous U in decompressive laminectomy for degenerative LSS had long term beneficial effect.
Keywords: Degenerative spinal stenosis, Lumbar, Dynamic stabilization, Interspinous U, Coflex™, Posterior lumbar interbody fusion
INTRODUCTION
The decompressive laminectomy with or without fusion was mainstay of surgical management for lumbar stenosis15). Instrumented fusion in spine was advocated for anticipated postoperative instability after wide decompression, unstable spondylolisthesis and degenerative scoliosis7,19). However, fusion poses various problems such as higher morbidity, mortality for geriatric patients and transfusion requirement, fusion mass fracture, pseudarthrosis and adjacent segment disease5,13).
To overcome shortcomings associated with fusion, concept of dynamic stabilization was introduced. A number of devices has been developed and those may be divided into two categories, pedicle screw based systems and interspinous spacers including interspinous U (ISU; Coflex™)8,20,21). Short term clinical outcome of ISU was promising and initial indications of ISU was broad including mild segmental instability and degenerative disc disease3). However, recently interspinous spacer including ISU showed higher complication rate in spondylolisthesis, thus its use as a substitute of instrumented fusion for unstable lumbar spinal stenosis (LSS) was not advocated10,17,22,25).
Because LSS without instability could be treated successfully with decompressive laminectomy without fusion, the role and indications of interspinous spacers in this clinical condition is still questionable15).
In addition, mechanism of interspinous spacers in LSS is hypothesized to decompress stenotic spine by increasing forminal height11,16). However, no long term effect of ISU in restoration of disc and foraminal height has been proved2,25). As there is no report longer than two years for ISU, the longer term clinical and radiological role and problems of the device are still remained unknown8,9,25). The aim of this study was to evaluate minimum two-year follow up result of ISU in degenerative spinal stenosis in comparison to posterior lumbar interbody fusion (PLIF).
MATERIALS AND METHODS
Inclusion and exclusion criteria
Between July 2003 and December 2005, a consecutive series of 61 patients with degenerative LSS patients treated with ISU (Group ISU : 30 patients, 17 males and 13 females) and treated with posterior lumbar interbody fusion (Group PLIF : 31 patients, 12 males and 19 females) were included for study. All patients complained of low back pain, radiating pain and neurogenic claudication. Inclusion criteria were symptomatic, medically intractable degenerative LSS with or without degenerative spondylolisthesis grade I and completed follow up minimum two years postoperatively. Patients should have had a persistent symptom with analgesics, physiotherapy or caudal epidural block. Patients with prior surgical treatment, trauma, infection, any other spinal disease such as ankylosing spondylitis and pathologic fracture, degenerative spondylolisthesis greater than grade II, isthmic spondylolisthesis and cauda equina syndrome were excluded. The patients implanted ISU in adjunct with instrumented fusion were also excluded.
Operative technique
Patients were operated in prone position, flexed on the Wilson frame (OSI, Union, CA, USA) under general anesthesia. Midline incision was used over the level of spinal stenosis and periosteal dissection of paraspinal muscle was performed. For the ISU group, adequate decompression was achieved by bilateral partial hemilaminectomy and removing ligamentum flavum and confirming lateral margins of the thecal sac and freely movable exiting roots after foraminotomy under an operative microscope. Then, interspinous ligament was excised and the optimal size of ISU implant was measured with trial inserter. Thereafter, Coflex™ implant was inserted between two spinous processes and tightened wings with clamp.
Meanwhile, in the group PLIF, total laminectomy and parital or total facetectomy was performed for decompression. After thorough discectomy and preparation of end plate, interbody fusion cages filled with bone graft were inserted to the disc space and fixated the segment with pedicle screw system. The patients were allowed to ambulate freely from the next day after operation and kept lumbar orthosis for 3 months postoperatively.
Clinical outcome measures
Patients were asked to complete Oswestry Disability Index (ODI) and visual analogue scale (VAS) of low back pain and leg pain before surgery and at final follow up. Clinical questionnaire was inquired and collected by telephone interview.
Radiological outcome measures
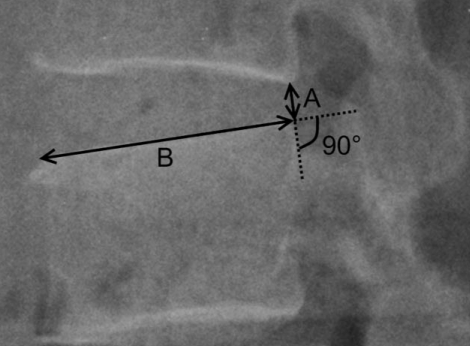
For radiologic analysis, 28 patients in group ISU and 29 patients in group PLIF were included and their preoperative, postoperative, and last follow up radiographs were evaluated. Disc height ratio (DH) was defined as posterior disc height/antero-posterior length of superior endplate of lower vertebra × 100 (%) (Fig. 1). DHs in preoperative, immediate postoperative and last follow up standing lateral radiograph in neutral position were measured. We measured posterior disc height as a distance from posterior inferior corner of upper vertebral body to superior end plate of lower vertebra perpendicularly. This is a modified method from previous reports in order to evaluate DH accurately in spondylolisthesis25,26). Anterior disc height was not measured because effect of ISU was considered to be related to posterior disc height.
Fig. 1.
Disc height ratio is calculated by disc height (length of line connecting posterior end of inferior endplate of superior vertebrae and inferior endplate perpendicularly) (A)/length of superior endplate of inferior vertebrae (B).
Anterior slippage of spondylolisthesis was calculated with percentage of vertebral slip (VS) [(distance between posterior margins of two adjacent vertebral bodies/anteroposterior length of superior endplate of lower vertebra × 100(%)]6).
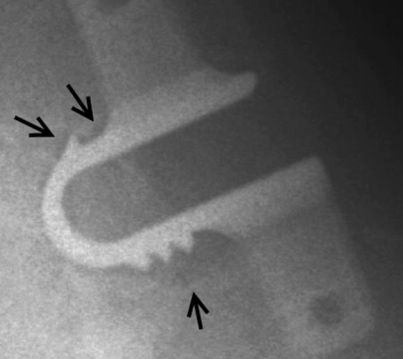
Radiolucent gap between spinous process and ISU was measured to identify any loosening or bone erosion of the device. In last follow up, longest depth of bone erosion around ISU was measured (Fig. 2).
Fig. 2.
Marked bone erosion around interspinous U, especially around spikes in a patient followed 50 months, can be seen (arrows).
Statistical analysis
We used student's t-test or Mann-Whitney U test for comparison of mean value between two groups and paired t-test or Wilcoxon signed rank test for comparison within the groups. To analyze correlations between variables, Pearson's correlation test and Spearman's rank correlation test were used. p value less than 0.05 was considered statistically significant. Standard deviations were calculated and mentioned for mean values. Error bars in graphs covers 95% confidence intervals. SPSS software (version 12.0, SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
RESULTS
Demographics and baseline variables
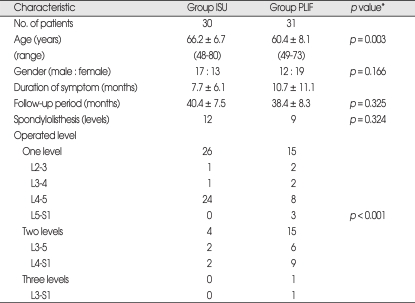
The mean age of group ISU was significantly older than group PLIF (66.2 ± 6.7 vs. 60.4 ± 8.1, p = 0.003, student's t-test) (Table 1) There was no statistically significant difference in frequency of gender between two groups (p = 0.166, Student's t test). There were no statistically significant difference between two groups in sex, duration of symptom, and follow up period. Degenerative spondylolisthesis (grade I) was associated with 12 levels of group ISU and 9 levels of group PLIF.
Table 1.
Demographic data
*Student-t test
In group ISU, 26 patients (87%) were operated in single level, four in two levels, and most frequent segment was L4-5 (24/30, 80%). In contrast, there were each 15 patients for single and two levels, one in three levels, and no predilection for operated segment in group PLIF. The difference in the number of operated levels between two groups was significant (p < 0.001, Student's t-test) (Table 1).
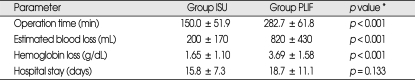
Perioperative data
Operation time was about half in group ISU (150.0 ± 51.9 minutes) than in group PLIF (282.7 ± 61.8 minutes, p < 0.001, Student's t-test) (Table 2). Estimated blood loss was much less in group ISU than group PLIF (197 ± 170 mL vs. 816 ± 430 mL, p < 0.001, Student's t-test). Because, the estimated blood loss may be inaccurate, perioperative hemoglobin loss (lowest hemoglobin during postoperative one week - last preoperative hemoglobin) was also calculated. The mean perioperative decrease of hemoglobin was smaller in group ISU (1.65 ± 1.10 g/dL) than group PLIF (3.69 ± 1.58 g/dL) (p < 0.001, Student's t-test). Only one patient in group ISU was transfused with two units of red blood cell. In the meantime 14 patients (45%) in group PLIF was transfused intraoperatively and mean transfusion amount for group PLIF was 0.98 unit of red blood cell per patient. The average postoperative length of stay in the hospital was 15.8 ± 7.3 days in group ISU and 18.7 ± 11.1 days in group PLIF. The difference was not significant (p = 0.133) (Table 2).
Table 2.
Perioperative data
*Student's t test. ISU : interspinous U, PLIF : posterior lumbar interbody fusion
Clinical outcome
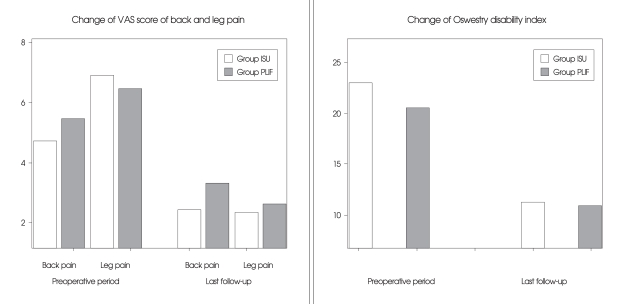
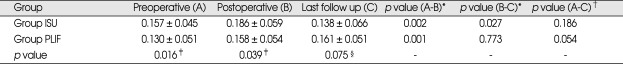
The mean follow up duration was 40.4 (27-51) months in group ISU and 38.4 (28-54) months in group PLIF. Both groups showed significant clinical improvement in the VAS scores for leg pain and back pain and ODI scores (Fig. 3, Table 3). There was no significant difference in clinical measures between two groups except that preoperative VAS score of back pain in group ISU (4.7 ± 2.0) was lower than group PLIF (5.5 ± 2.6) (p = 0.036, Student's t-test) (Table 3).
Fig. 3.
Both visual analogue scale (VAS) scores of back and leg pains and Oswestry disability index decreased significantly in last follow up (p < 0.001).
Table 3.
Visual analogue scale (VAS) pain scores and Oswestry Disability Index (ODI) scores (mean ± SD)
*Paired t-test, †Student's t-test, ‡Statistically significant
There was no significant difference between group ISU with spondylolisthesis (12 patients) and group ISU without spondylolisthesis (18 patients) in all clinical measures represented by VAS and ODI (p > 0.1, Mann-Whitney U test). There was also no significant difference between group PLIF with spondylolisthesis (n = 9) or without spondylolisthesis (n = 22) in clinical outcomes (p > 0.1, Mann-Whitney U test).
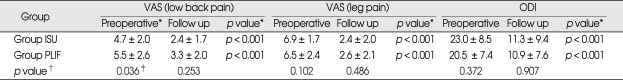
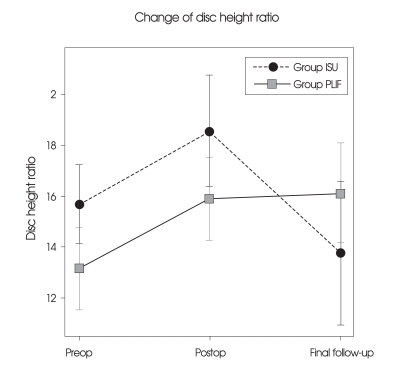
Radiologic changes of disk-height ratio
Preoperative DH was greater in group ISU (15.7 ± 4.5%) than group PLIF (13.0 ± 5.1%) (p = 0.016, Student's t-test) (Table 4, Fig. 4). Postoperative DH was increased significantly postoperatvely in both groups (18.6 ± 5.9% in group ISU p = 0.002, paired t-test, 15.8 ± 5.4% in group PLIF, p = 0.001, paired t-test). DH was still lower in group PLIF than group ISU (p = 0.039, Student's t-test). In last follow up, restored DH of group ISU was lost (13.8 ± 6.6%, p = 0.027, Wilcoxon signed rank test) in comparison with postoperative DH. However, PLIF group did not show any significant change of postoperative DH during follow up period (16.1% ± 5.1, p = 0.773, Wilcoxon signed rank test).
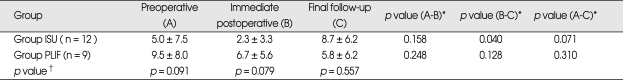
Table 4.
Changes in disc height percentage (%, mean ± SD)
*Paired t-test, †Wilcoxon signed rank test, ‡Student t-test, §Mann-Whitney U test. ISU : interspinous U, PLIF : posterior lumbar interbody fusion
Fig. 4.
Preoperative disk height ratio is lower in group posterior lumbar interbody fusion (PLIF) (p = 0.016). Disk height ratio initially improves in both groups (p = 0.002 in group interspinous U (ISU, Coflex™, Paradigm Spine Inc.®, NY, USA) p = 0.001 in group PLIF). However, it decreases significantly in Group ISU in minimum at 2 year follow up in comparison to immediate postoperative value (p = 0.027). There was no statistically significant difference between preoperative and minimum 24 months follow up disk height ratio in Group ISU (p = 0.186). Error bar covers 95% confidence interval.
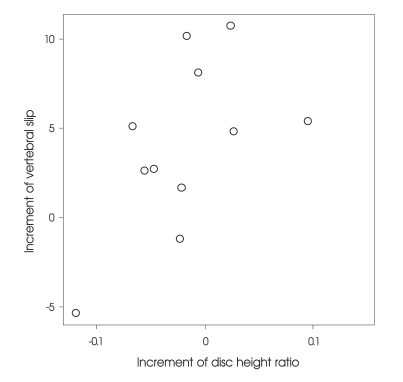
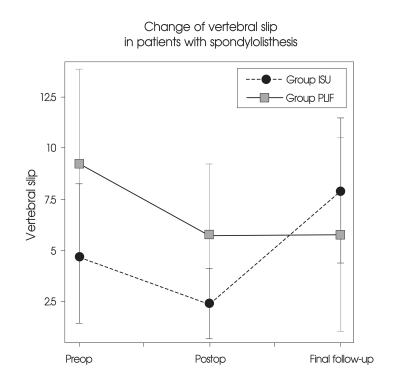
Change of vertebral slip in patients with spondylolisthesis
Degenerative spondylolisthesis grade I was associated in 12 levels of group ISU and 9 levels of group PLIF. Mean preoperative VS was lower in group ISU (5.0 ± 7.5%) than in group PLIF (9.5 ± 8.0%), however there was no significant difference (p > 0.1, Mann-Whitney U test). In postoperative period, VS was reduced in both groups and tend to be lower in group ISU (2.3 ± 3.3%, 6.7 ± 5.6% respectively, p = 0.079, Mann-Whitney U test). However, there was no statistical significance in reduction (p = 0.158 in group ISU, p = 0.248 in group PLIF, Wilcoxon signed rank test). In final follow up VS of group ISU increased significantly (8.7 ± 6.2%, p = 0.040, Wilcoxon signed rank test). In group PLIF there was no significant change in VS in final follow up (5.8 ± 6.2%, p = 0.128, Wilcoxon signed rank test). At final follow up, there was no difference between two groups (p = 0.557, Mann-Whitney U test).
Among the radiological outcome, increment of DH was correlated with increment of VS in group ISU (p = 0.040, Spearman's rank correlation coefficient = 0.599) (Fig. 6).
Fig. 6.
Increment of Disc height ratio was correlated with increment of vertebral slip in group interspinous U (ISU, Coflex™, Paradigm Spine Inc.®, NY, USA) (p = 0.040, Spearman's rank correlation coefficient = 0.599).
Device failures and complications
There was one patient with a fractured ISU. One patient in group ISU was reoperated due to compression of operation site by bony materials between the nerve root and the ISU.
Two patients in group PLIF were reoperated, because of infection and screw malposition.
Radiolucent gaps between ISUs and spinous processes were found in 57% of group ISU patients followed radiologically over 24 months. Mean maximum depth of gaps was 1.8 ± 1.5 mm in our series. Radiolucent gaps were especially prominent around spikes of ISU (Fig. 2). There was no gap around pedicle screw in radiologically evaluated patients in group PLIF.
DISCUSSION
Development of interspinous devices
The concept of "dynamic stabilization" or "soft stabilization" has been introduced to overcome problems related with spinal fusion. Theoretically, dynamic stabilization system may alter favorably the movement and load transmission of a spinal motion segment, without the intention of fusion of the segment by restriction of motion in the direction or plane that produces pain, or painful motion, but otherwise allowing a full range of motion4). Since the 1950s when a metal "plug" was implanted between two spinous processes by Dr. Fred L. Knowles, numerous interspinous devices have been designed and introduced for various types of lumbar spinal diseases3). In the biomechanical standpoint, all the interspinous devices exert their role by distracting the spinous processes and blocking extension9). As a consequence, they were able to increase foraminal and spinal canal dimensions and reduce intradiscal pressure at the implanted level and off-load the facet joints in vitro and in vivo studies11,18,24,27). Although it is quite certain that interspinous devices have a great advantage of "minimal invasiveness", their enthusiastic applications of various lumbar spinal disorders such as degenerative spinal stenosis, discogenic back pain, facet joint syndrome, herniated disc diseases, and instability are seem to be resulted partly from the overestimation of biomechanical function as well as ease of the implantation. However, it has been still remained unanswered how much and which type of the interspinous devices can fulfill the ideal goal of dynamic stabilization. Therefore, individual interspinous devices should be evaluated to prove their efficacy according to each applicable disease entity.
Characteristics and surgical indications of interspinous U
ISU, originally developed in France, is one of a dynamic interspinous devices having axially compressible U-shaped piece of metal3). As the mechanism of action inherited by all the interspinous devices including ISU is distracting two spinous processes and preventing extension, degenerative LSS with neurogenic intermittent claudication is one of their best indications. However, unlike X-stop, there are only a few international literatures dealing with ISU in LSS and no long-term outcome has been documented1,2,12,14,25). Our study is of value because the patients had mean follow up period over 3 years postoperatively and surgical indication was limited to LSS.
ISU was used in our study for patients with mild segmental instability based on one year experience of ISU in degenerative LSS with segmental instability which showed favorable result17). In fact, we also conceptualized the ISU may provide more stabilizing effect on the operated segment and prevent or delay the occurrence of secondary instability or recurrent stenosis than decompressive laminectomy without instrumentation in LSS. The merits of ISU in aspect of less invasiveness and ease of implantation made more frequent use in elderly patients. We also expected that the spinal stability provided by ISU would be less solid than PLIF. Therefore, majority of patients in the group ISU were implanted at single level without significant instability inherent or related to multi-level decompression (Table 1).
Because of short or rudimentary spinous process of S1, ISU was precluded at L5-S1 and no case was implanted at L5-S1 in our series. Thus, most frequent segment treated by ISU was L4-5, the most common location of spinal stenosis.
In the meantime, PLIF was considered more appropriate when patients had well tolerable general condition, multi-level diseases, or spinal segments including L5-S1, or surgical decompression would result in secondary instability.
The demographic difference of our study reflected well these considerations in selecting surgical methods between the two groups. (Table 1, 4). Our study should be interpreted carefully because of this selection bias.
Clinical results of interspinous U
As mentioned previously, there are few clinical reports dealing with ISU3). Bono et al.3) quoted unpublished data of Dr J. Samani's series with various diagnosis (106 patients) that 74% good or excellent outcome and 10% revision rate. Follow-up duration of our study was longer than previous reports and also showed significant reduction in VAS low back and leg pain scores and ODI scores postoperatively in both groups (Table 3, Fig. 3)9). Although preoperative VAS low back pain score was significantly higher in group PLIF, it should be interpreted as selection bias. In addition, group ISU had less operation time, blood loss, and hospital stay than group PLIF (Table 2). X-stop showed mean operation time was 54 ± 18 minutes and mean blood loss 46 mL and was less invasive than ISU27). However, it should be considered that in X-stop series the decompressive laminectomy was not usually performed unlike ISU.
Therefore, it is suggested that minimum 2-year clinical outcome of ISU in LSS with or without degenerative spondylolisthesis grade I is less invasive but comparable with rigid fixation from our result.
Radiological results : disc height, vertebral slip, and bone erosion
The fundamental function of interspinous devices is distraction of two adjacent vertebra, thus ameliorating foraminal stenosis and intradiscal pressure. Four different interspinous implants-Coflex, Wallis, DIAM and X-stop were studied in terms of three dimensional flexibility and the intradiscal pressure in vitro and no significant biomechanical difference among the implants23).
The previous study of ISU showed significant increase of posterior disc height one year postoperatively9). On the contrary, restored disc height was lost in last follow up radiograph in group ISU of our series (Table 4, Fig. 4). In the subpopulation with spondylolisthesis, postoperative vertebral slip was partly reduced in both groups however, VS of group ISU was merely not maintained but more progressed than preoperative state during follow up period (Table 5, Fig. 5). This progression of spondylolisthesis might be related to directional and quantitative change of load caused by increased posterior disc height, because degree of aggravation of spondylolisthesis is correlated with increment of disc height (Fig. 6).
Table 5.
Mean change of vertebral slip in patients with spondylolisthesis in any period (%, mean ± SD)
*Wilcoxon signed rank test, †Mann-Whitney U test. ISU : interspinous U, PLIF : posterior lumbar interbody fusion
Fig. 5.
Vertebral slip (VS) in a subgroup of patients with spondylolisthesis increased significantly in Group interspinous U (ISU, Coflex™, Paradigm Spine Inc.®, NY, USA) in final follow up in comparison to both preoperative period (p = 0.038) and postoperative period (p = 0.071). VS in group interbody fusion (PLIF) was not increased and there was no statistically significant difference between group ISU and group PLIF during all period. Error bar covers 95% confidence interval.
The other probable cause of this result is bone erosion. Fifty-seven percent of ISU group showed bone erosion at the spinous process - ISU interface in our series (Fig. 2). In a previous report with mean 22 months follow up poor clinical outcome was speculated to be related with bone-implant interface failure13). Because minimally invasive merits of interspinous devices make propensity toward their use in the elderly, long term bone erosion should be considered especially in severe osteoporotic patients.
Our result raises an important criticism on the biomechanical function of ISU. In contrast, a number of literatures have mentioned favorable result of interspinous devices both biomechanically and clinically23,27). However, the majority of them are in vitro cadaveric study or short-term outcome. In one year experience of X-stop in LSS, maximal clinical improved by 3 months and then gradually declined18). X-stop in LSS with degenerative spondylolisthesis showed high failure rate (7/12 patients)22). They concluded that the degenerative spondylolisthesis in patients with LSS may be considered as a contraindication for the X-stop.
According to our result, it is suggested that biomechanical function of ISU as a interspinous distracting device may not be as durable as expected and this phenomenon may result in late clinical deterioration.
Limitations of the study
A firm conclusion about the clinical efficacy of ISU is difficult to be made from this study due to several reasons. The sample size is not large and study design is a retrospective review without randomization. Thus, selection biases between two groups exist. Finally, this study does not include segmental motion analysis. Therefore, our data do not support any comparative efficacy of the decompressive laminectomy plus implantation of ISU over PLIF. However, to best of our knowledge, no literature dealing with ISU in LSS has longer term result than this study.
CONCLUSION
Implantation of ISU after decompressive laminectomy in degenerative LSS was less invasive and showed clinical effectiveness comparable to PLIF. Even though it provided restoration of disc height and reduction of vertebral slip postoperatively, these were not maintained during follow up period.
Therefore, in the biomechanical standpoint, the efficacy of interspinous U, as an adjunct of decompressive laminectomy in degenerative LSS, may be sustained for merely several months of postoperative period and it is hard to expect that it has long term beneficial effect. Clinical application of interspinous devices including interspinous U based on short term clinical results should be reconsidered.
References
- 1.Adelt D, Samani J, Kim W, Eif M, Lowery GL, Chomiak RJ. Coflex interspinous stabilization : Clinical and Radiographic results from an international multicenter retrospective study. Paradigm Spine Journal. 2007;1:1–4. [Google Scholar]
- 2.Bae YS, Ha Y, Ahn PG, Lee DY, Yi S, Kim KN, et al. Interspinous implantation for degnerative lumbar spine : clinical and radiologic outcome at 3-yr follow up. Korean J Spine. 2008;5:130–135. [Google Scholar]
- 3.Bono CM, Vaccaro AR. Interspinous process devices in the lumbar spine. J Spinal Disord Tech. 2007;20:255–261. doi: 10.1097/BSD.0b013e3180331352. [DOI] [PubMed] [Google Scholar]
- 4.Christie SD, Song JK, Fessler RG. Dynamic interspinous process technology. Spine (Phila Pa 1976) 2005;30:S73–S78. doi: 10.1097/01.brs.0000174532.58468.6c. [DOI] [PubMed] [Google Scholar]
- 5.Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992;74:536–543. [PubMed] [Google Scholar]
- 6.Friberg O. Functional radiography of the lumbar spine. Ann Med. 1989;21:341–346. doi: 10.3109/07853898909149218. [DOI] [PubMed] [Google Scholar]
- 7.Hur JW, Kim SH, Lee JW, Lee HK. Clinical analysis of postoperative outcome in elderly patients with lumbar spinal stenosis. J Korean Neurosurg Soc. 2007;41:157–160. [Google Scholar]
- 8.Kaech DL. Spinal Restabilization Procedures. Amsterdam: Elsvier; 2002. The interspinous-U : A new restabilization device for the lumbar spine; pp. 355–362. [Google Scholar]
- 9.Kong DS, Kim ES, Eoh W. One-year outcome evaluation after interspinous implantation for degenerative spinal stenosis with segmental instability. J Korean Med Sci. 2007;22:330–335. doi: 10.3346/jkms.2007.22.2.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim HJ, Roh SW, Jeon SR, Rhim SC. Early experience with interspinous U in the management of the degenerative lumbar disease. Korean J Spine. 2004;1:456–462. [Google Scholar]
- 11.Lindsey DP, Swanson KE, Fuchs P, Hsu KY, Zucherman JF, Yerby SA. The effects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. Spine (Phila Pa 1976) 2003;28:2192–2197. doi: 10.1097/01.BRS.0000084877.88192.8E. [DOI] [PubMed] [Google Scholar]
- 12.Park CK, Kim DH, Kim MK, Ryu KS. World Spine IV. Istanbul: World Spine Society; 2007. Effects of "Interspinous-U" on posterior stabilization of the lumbar spine following decompressive surgery in lumbar spinal stenosis : Minimum 27-month follow-up. [Google Scholar]
- 13.Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion : review of the literature. Spine. 2004;29:1938–1944. doi: 10.1097/01.brs.0000137069.88904.03. [DOI] [PubMed] [Google Scholar]
- 14.Park YS, Kim YB, Lee DG, Kim KT, Nam TK. Dynamic stabilization with an interspinous process device (the Wallis system) for degenerative disc disease and lumbar spinal stenosis. Korean J Spine. 2008;5:258–263. [Google Scholar]
- 15.Prolo DJ, Oklund SA, Butcher M. Toward uniformity in evaluating results of lumbar spine operations. A paradigm applied to posterior lumbar interbody fusions. Spine (Phila Pa 1976) 1986;11:601–606. doi: 10.1097/00007632-198607000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Richards JC, Majumdar S, Lindsey DP, Beaupré GS, Yerby SA. The treatment mechanism of an interspinous process implant for lumbar neurogenic intermittent claudication. Spine (Phila Pa 1976) 2005;30:744–749. doi: 10.1097/01.brs.0000157483.28505.e3. [DOI] [PubMed] [Google Scholar]
- 17.Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine (Phila Pa 1976) 2006;31:442–449. doi: 10.1097/01.brs.0000200092.49001.6e. [DOI] [PubMed] [Google Scholar]
- 18.Siddiqui M, Smith FW, Wardlaw D. One-year results of X Stop interspinous implant for the treatment of lumbar spinal stenosis. Spine (Phila Pa 1976) 2007;32:1345–1348. doi: 10.1097/BRS.0b013e31805b7694. [DOI] [PubMed] [Google Scholar]
- 19.Simmons ED, Jr, Simmons EH. Spinal stenosis with scoliosis. Spine (Phila Pa 1976) 1992;17:S117–S120. doi: 10.1097/00007632-199206001-00009. [DOI] [PubMed] [Google Scholar]
- 20.Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine : a multi-center study of a novel non-fusion system. Eur Spine J. 2002;11(Suppl 2):S170–S178. doi: 10.1007/s00586-002-0438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor J, Pupin P, Delajoux S, Palmer S. Device for intervertebral assisted motion : technique and initial results. Neurosurg Focus. 2007;22:E6. doi: 10.3171/foc.2007.22.1.6. [DOI] [PubMed] [Google Scholar]
- 22.Verhoof OJ, Bron JL, Wapstra FH, van Royen BJ. High failure rate of the interspinous distraction device (X-Stop) for the treatment of lumbar spinal stenosis caused by degenerative spondylolisthesis. Eur Spine J. 2008;17:188–192. doi: 10.1007/s00586-007-0492-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilke HJ, Drumm J, Häussler K, Mack C, Steudel WI, Kettler A. Biomechanical effect of different lumbar interspinous implants on flexibility and intradiscal pressure. Eur Spine J. 2008;17:1049–1056. doi: 10.1007/s00586-008-0657-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wiseman CM, Lindsey DP, Fredrick AD, Yerby SA. The effect of an interspinous process implant on facet loading during extension. Spine (Phila Pa 1976) 2005;30:903–907. doi: 10.1097/01.brs.0000158876.51771.f8. [DOI] [PubMed] [Google Scholar]
- 25.Yoon SM, Lee SG, Park CW, Yoo CJ, Kim DY, Kim WK. Late complications of the single level 'interspinous U' in lumbar spinal stenosis with mild segmental instability. Korean J Spine. 2008;5:89–94. [Google Scholar]
- 26.Yoon SM, Lee SG, Kim EY, Kim WK. Follow-up comparison study of single-level posterior dynamic stabilization in lumbar degenerative disease 'Interspinous U' vs. 'DIAM'. Korean J Spine. 2008;5:136–141. doi: 10.14245/kjs.2012.9.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, et al. A multicenter, prospective, randomized trial evaluating the X STOP interspinous process decompression system for the treatment of neurogenic intermittent claudication two-year follow-up results. Spine (Phila Pa 1976) 2005;30:1351–1358. doi: 10.1097/01.brs.0000166618.42749.d1. [DOI] [PubMed] [Google Scholar]