Abstract
Objective
The purpose of this study was to determine the efficacy, radiological findings, clinical outcomes and complications in patients with lumbar stenosis and osteoporosis after the use of polymethylmethacrylate (PMMA) augmentation of a cannulated pedicle screw.
Methods
Thirty-seven patients with degenerative spinal stenosis and osteoporosis (T-score < -2.5) underwent lumbar fusion using the Dream Technology Pedicle Screw (DTPS™, Dream Spine Total Solutions, Dream STS, Seoul, Korea) between 2005 and 2007. The clinical outcomes were evaluated by using the visual analog scale (VAS) and the Prolo scale. Radiologic findings were documented through computed tomography (CT) and plain films.
Results
Thirty-seven patients were evaluated and included, 2 males and 35 females with an average bone mineral density (BMD) of 0.47g/cm2. The average age of the patients was 68.7 (range, 57-88). The preoperative VAS for low back and leg pain (7.87 ± 0.95 and 8.82 ± 0.83) were higher as compared with postoperative VAS (2.30 ± 1.61 and 1.42 ± 0.73) with statistical significance (p = 0.006, p = 0.003). According to the Prolo scale, 11, 22, one and three patients were in excellent, good, fair and poor conditions, respectively. The average amount of the injected cement per one cannulated screw was 1.83 ± 0.11 mL.
Conclusion
The results show favorable outcome both clinically and radiographically for 37 patients who underwent lumbar fusion using DTPS™ and PMMA. Based on the results, the use of this surgical method can be a safe and effective option for the operation on the osteoporotic spine.
Keywords: PMMA, Pedicle screw, Osteoporosis, Lumbar stenosis
INTRODUCTION
As aged individuals in the world increase rapidly, degenerative spinal disease and osteoporosis also become rapidly as major global medical problems. Pedicle screw instrumentation is currently being widely used in spine surgery to obtain internal stabilization in these patients. When pedicle screws are used in elderly osteoporotic patients, however, the screw-interface is easily stripped; as a result, the risk of screw-loosening and back-out after surgery have also increased. Insertion of a successful pedicle screw fixation for the elderly patient with osteoporosis has thus been a challenging goal for spine surgeons. Data from several laboratory studies using cadaver spines16,20,33,35,42) have demonstrated that the use of a bone cement-augmented pedicle screw fixation has resulted in a significantly-increased axial pull-out force and transverse bending stiffness. In the osteoporotic spine, polymethylmethacrylate (PMMA) cement, one type of such bone cement, has also been shown to increase the holding power of screws in osteoporotic bone6,19,29,35,36,42,47).
In spite of these benefits, reports concerning the clinical use of PMMA have been sparse13,40,44). This hesitancy for the employment of PMMA has been due to the undesirable exothermic reaction which accompanies it hardening and which occurs in close proximity to neural elements41). There is also the risk of PMMA leakage into the spinal canal, neural foramina, or paravertebral veins. To compensate for the weaknesses inherent with the use of PMMA alone, novel cannulated pedicle screws have been designed and developed, its holes existing at the distal end of the screw. The biomechanical test results of these new kind of screws have been presented12,22,37,45). These screws are novel in their design and concept and clinical results after the use of one these screws are presented in the present paper. The advantage of this screw is its ability to enable PMMA injection in to it after the screw's insertion into the pedicle. The PMMA then spreads into the threads of the screw so as to improve the screw's structural performance. Another major benefit of this screw is the need to use only a consistently small amount of cement.
Thus, the primary aim of this study was to determine the clinical efficacy and safety of a screw augmentation procedure using a novel spine cement fixation system in patients with coexisting lumbar stenosis and osteoporosis. The postoperative outcomes of patients treated with this device were also reviewed.
MATERIALS AND METHODS
Between August 2005 and June 2007, a consecutive series of 37 osteoporotic patients with T-scores less than -2.5 and coexisting lumbar stenosis were accumulated. These patients underwent lumbar fusion by one surgeon at a single institution using the DTPS™ a novel pedicle screw and spine cement kit. Patients were followed postoperatively for a minimum of 23 months with an average of follow-up 33.3 months (range, 23-45 mos). The mean patient age was 68.7 years (range, 57-88 yr); there were two men and 35 women. Monosegmental fusion was performed on 30 patients and bi- and trisegmental fusions on four and three patients, respectively. The preoperative diagnoses included degenerative spondylotic stenosis in 26 patients, degenerative spondylolisthesis in 6 and spondylolytic spondylolisthesis in 5. Patients were evaluated for osteoporosis of the lumbar spine via determination of the bone mineral density (BMD) using dual-energy X-ray absorptiometry (DXA) (HOLOGIC Discovery Wi, Hologic Inc, Waltham, Massachusetts, USA). Baseline BMD values were obtained from the reference date of the Japan Society for Bone and Mineral Research (JSBMR)26) i.e., and osteoporosis was diagnosed if a patient's T-score was equal to or less than -2.5 (T-score ≤ 2.5), the World Health Organization's (WHO's) diagnostic criteria for osteoporosis18). The mean BMD of the patients was 0.47 g/cm2. The patients were classified according to their T-scores into four Groups : nine patients (24.3%) had T-scores between -2.5 and -2.9, 12 (32.4%) between -3.0 and -3.4, 10 (27.0%) between -3.5 and -3.9, and six patients (16.2%) had T-scores of less than -4.0. All of the patients had varying degrees of neurogenic intermittent claudication and low back pain as their presenting complaints. Each patient had undergone at least six months of nonoperative care prior to surgery. After informed consent was obtained from the patients, operations were performed on those who chose to undertake the PMMA augmentation using DTPS™, for their lumbar fusions. The patients' demographic characteristics and procedural data are listed in Table 1. The patients' data are recorded for the pre- and postoperative visual analog scale (VAS) and Prolo scores30), and complications including extravasation of cement, embolus and infection. For the radiographic evaluation of pedicle screw loosening and nonunion, anteroposterior and lateral and standing flexion-extension lumbosacral plain X-rays were obtained pre- and postoperatively and at the outpatient clinic follow-up periodically. Computerized tomography (CT) was done with all of the patients to determine bone cement leakage in the spinal canal. To confirm or rule-out pulmonary embolism after surgery, the immediate postoperative posteroanterior chest X-ray was performed. Screw-loosening was defined as a radiolucency of one millimeter (mm) or wider at the bone-screw interface. Fusion status was evaluated on the final follow-up films using the criteria listed in Table 2. A solid fusion was determined by the presence of at least two criteria in the list. A single-level nonunion was also considered as failure of bone fusion irrespective of the operative level.
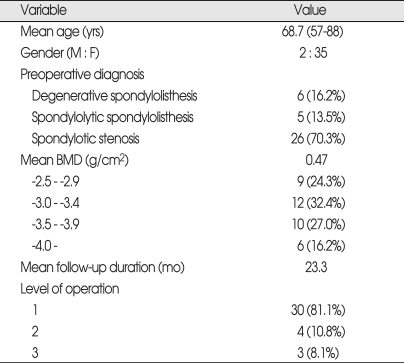
Table 1.
Demographic and clinical characteristics in 37 patients with PMMA-augmented screw fixation for stabilization of the osteoporotic spine
PMMA : polymethylmethacrylate, BMD : bone mineral density
Table 2.
Fusion rates according to solid fusion criteria
PMMA : polymethylmethacrylate
Spinal Cementing Fixation system (DTPS™ system)
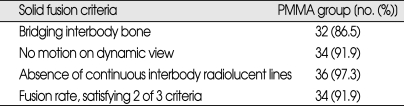
The DTPS™ system consists of two parts : 1) a cannulated pedicle screw (Fig. 1A and 2) a spine cement kit (Fig. 1B). The pedicle screw (6.5 or 7.5 mm in diameter and 40 or 45 mm in length) has a cannulation diameter of either 2.5 mm for the 6.5 mm screw or 3.0 mm for the 7.5 mm screw and 4 holes, is designed so that each set of two holes are situated opposite to the other set of two holes, at the distal end of the screw (Fig. 1A). The bone cement is injected and with this screw design, penetrates into the trabeculae of surrounding bone through the four holes (Fig. 2). After insertion of the cannulated pedicle screws into the osteoporotic vertebral body, the spine cement kit (Fig. 1C) is able to effectively inject the proper amount of bone cement so as to fixate the head of the pedicle screw firmly before placement of a rigid rod. It is also designed to enable discontinuation of the injection of bone cement at a point at which extravasation is observed by fluoroscopy imaging.
Fig. 1.
The photographs show screw, spine cement kit and adpapter. A : Dream Technology Pedicle Screw (DTPS™, Dream STS, Seoul, Korea) screw has a cannulation diameter of either 2.5 mm for the 6.5 mm screw or 3.0 mm for the 7.5 mm screw and 4 holes, is designed so that each set of two holes (black arrow) are situated opposite to the other set of two holes (white arrow), at the distal end of the screw. B : A spine cement kit : An adapter is to connect cannulated screw. Spreader is to push polymethylmethacrylate into body through screw. C : The photograph shows combination of DTPS™ screw and adapter.
Fig. 2.
A schematic and lateral radiograph show the injected polymethylmethacrylate (PMMA) spreading through the bone. A : A schematic demonstrates that the injected PMMA spreads through the bone via four holes of screw and penetrates into the trabeculae of surrounding bone. B : Postoperative lateral radiograph shows that PMMA spreads and penetrates through the trabeculae of surrounding bone.
Surgical procedure
Under general anesthesia, in the prone position, the lesion was approached by a posterior midline incision. To expose the lumbar stenosis pathology sufficiently, the right and left facet joint capsules and the ligamentum flavum were removed, and complete decompression of the affected nerve roots running in the inferomedial portion of the pedicle was performed. The intervertebral disc was exposed and discectomy performed. After confirming the complete decompression of the compromised nerve roots, tapping using a tapper on the transpedicular screw placement site was done. For the safe and accurate procedure, the pedicle screw insertion was performed under the guidance of fluoroscopy. In addition to bone chips from the laminectomy, local cancellous bone from the facetectomies was used to fill a Polytheretherketone (PEEK) interbody cage (Stryker Orthopaedics, Mahwah, NJ, USA) and to pack the disc space area between inserted cage and the vertebrae. Since the pedicle screw is used a mono-axial system, it is difficult to rotate it after PMMA injection. Thus, the rod must be shaped to accommodate normal lumbar lordosis and must be placed on the head of the screw prior to the injection PMMA. Contrast media was injected under fluoroscopic guidance to keep the neural canal protected from potential cement leakage. "Vertebroplastic radiopaque resinous material" (DePuy Acromed, Raynham, MA, USA) was used, a form of PMMAbone cement, and it was mixed according to the manufacturers recommendations. For injection of the bone cement, the cannulated pedicle screw and spine cement kit was used and continuous lateral fluoroscopy was carried out during all steps of the procedure. If there was no migration of the bone cement to the posterior part of the vertebra observed on continuous lateral fluoroscopy, the bone cement was continuously injected. A student's t-test was used to compare continuous variables including preoperative and final VAS and the Prolo scale. In all analyses, a p value of < 0.05 was considered to be significant.
RESULTS
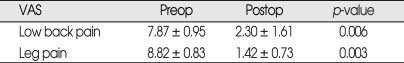
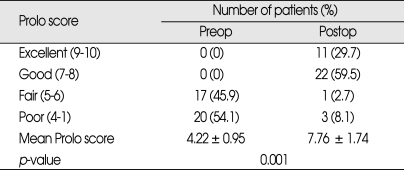
For this study, 168 cannulated screws were used. Each screw was filled with 1.83 ± 0.11 mL (range 1.7-2.0 mL) of PMMA. PMMA leakage into the neural canal with its concomitant myelopathy or radiculopathy did not occur, however local extravasations of PMMA into the ventral aspect of the vertebral body were observed in two cases (5.4%). There were no pulmonary emboli or cases of osteomyelitis. After the surgery, two patients developed fluid collection in operative wound area resulting from dural laceration with CSF leakage, both of which subsided without further intervention. Fusion status was judged based in the criteria listed on the Table 2. For solid fusion, at least two criteria needed to be satisfied, and 34 of 37 patients (91.9%) met this condition. Three patients who could not achieve a solid fusion belonged to the group who had T-scores less than -4.0. Pedicle screw loosening was observed in one patient (2.7%). This patient was one of three non-union cases and a three-level surgery had been performed in this case: firm bone union for L3-L4 and L4-L5 was observed, but L2-L3 failed to fuse. One year postoperatively, there were no radiographic abnormalities observed (Fig. 3A). However, two years after surgery, a screw-loose was found, which manifested as radiolucency in the bone-screw interface (Fig. 3B). Pre- and postoperative VAS's in all patients in this study were compared for both low back pain and leg pain. The postoperative VAS for low back pain and leg pain (2.30 ± 1.61 and 1.42 ± 0.73) has been decreased compared to preoperative VAS' (7.87 ± 0.95 and 8.82 ± 0.83). This data was statistically significant (p = 0.006, p = 0.003) (Table 3). Using the method of Prolo et al.30), the result revealed that the preoperative values were an average of 4.22 ± 0.95 and the postoperative, 7.76 ± 1.74, which was statistically signi-ficant (p = 0.01) (Table 4). There were no screw fractures or construct failures.
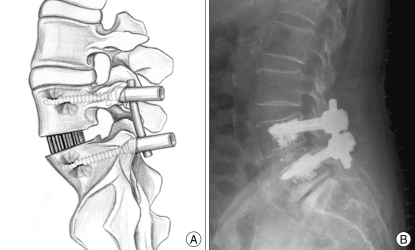
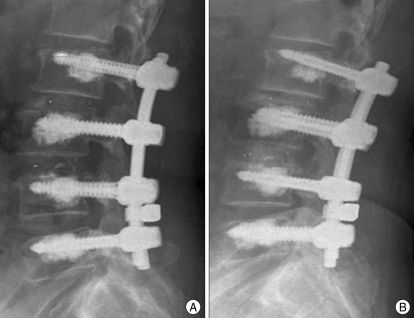
Fig. 3.
A 67-year-old woman complained of lower back pain and neurological intermittent claudication and was diagnosed with multiple lumbar stenosis with instability. She had undergone tri-segmental lumbar fusion operation. A : Simple lateral radiograph on postoperative one year shows no abnormality. B : Compared with postoperative one year, simple lateral radiograph on postoperative two years shows movement of L2 pedicle screws and radiolucency around the screws.
Table 3.
The comparison between pre- and post-operative VAS for lower back and leg pain
VAS : Visual analog scale
Table 4.
Mean Prolo scores and distribution of the scores for 37 patients with PMMA-augmented screw fixation for stabilization of the osteoporotic spine
PMMA : polymethylmethacrylate
DISCUSSION
Due to increased human life-spans and improvements in the quality of life, the trend is that the frequency of transpedicular screw fixation for degenerative spinal disease in patients with poor bone quality is on the rise. In the severely osteoporotic spine, the anchoring power of the transpedicular screw is decreased and the probability of the failure of screw fixation is high. To achieve successful transpedicular screw fixation, the strength of the contact area between the screw and the vertebra becomes the most important factor. In osteoporotic spines, firm fixation strength cannot be obtained due to the loss of healthy bone structures, and thus additional procedures to improve screw fixation are required.
The use of bone cement in orthopedic procedures involving joint prosthesis fixation has been in effect since the late 1960s, with consistent demonstration of a strengthened bone-prosthesis interface2,39). Data from recent spine studies have revealed the same concepts to be applicable to PMMA-augmented pedicle screw fixation here10,16,20,33,35,42), which has also been used to increase the purchase of screws in osteoporotic bone. Regarding the traditional use of PMMA in the osteoporotic spine, first a pilot is drilled. Then, PMMA is injected into pilot prior to screw insertion. PMMA is spread by pressure into the vertebral body due to the pedicle screw insertion with a risk of leakage into the spinal canal, neural foramina or paravertebral veins. Even if leakage of PMMA into the spinal canal is observed, insertion of the pedicle screw into the pedicle cannot be interrupted. The use of PMMA in this application also carries the risk of complication due to an exothermic reaction as the PMMA hardens, the latter being undesirable when it occurs in close proximity to neural elements41). The risk of PMMA extravasation in various series ranged between 27-74%7,15,17,27,28,32), with resultant neurological deficits such as radiculopathy and cord compression occurring in 3.7 and 0.5%, respectively3). In order to prevent this series complication, the recent use of bone cement injection using a cannulated pedicle screw is regarded as a promising option13,14). The present study as well as other published results had no cases of radiculopathy or myelopathy due to PMMA-extravasation. According to Frankel et al.'s paper13), PMMA extravasation occurred in 39%. In this study, the occurrence was only 5.4% because of the low mean amount of PMMA injected for each pedicle screw. In our study, it was 1.83 ± 0.11 mL (range, 1.7-2.0 mL) while the mean amount of PMMA in Frankel et al.'s cases13) was 2.89 ± 0.72 mL (range, 2.0-5.0 mL). On the other hand, for Fransel et al.'s cases14), though only three patients were presented, 1.5 mL of PMMA was used in each patient and no extravasation of the bone cement occurred14). In addition, according to the cadaveric study of Frankel et al.12), regarding the amount of PMMA injected into the vertebral body, the patients were divided into a "small-amount" group (≤ 2.8 mL/pedicle) and a "high-amount" group (≥ 5.5 mL/pedicle). The pullout strength result for each group was similar, therefore, the authors recommended using lower amounts of cement for pedicle screw augmentation procedures12).
There is no substitute for careful surgical technique by an experienced surgeon using correct tap positioning with adequate fluoroscopy to image the extent and direction of PMMA injection. Any fluoroscopic demonstration of cement extravasation, especially in a posterior direction, should immediately result in the termination of injection and abandonment of further injection.
Pulmonary embolism after vertebroplastic procedures has been well-documented in the literature, with its incidence ranging from 1-11%1,4). After vertebroplastic procedures, pulmonary embolism was shown to usually be asymptomatic, but occasionally it could lead to death4,31,34,46). A predisposing factor for PMMA migration into the venous system is that the vertebral venous system does not possess valves. To avoid this life-threatening complication, several authors proposed various precautions. Several authors enabled rapid detection of PMMA extravasation into the perivertebral veins and spinal canal by performing the procedure under the guidance of CT or intraoperative biplanar radiography. Another important factor is the correct handling of the vertebroplasty material : the mixture must be prepared strictly according to the manufacturer's directions. The mixture should be injected during the transitional period in which the PMMA passes from fluid to solid and not too earlier. Following extravasation of PMMA into the venous system, the injection must be stopped immediately. A routine chest X-ray following the procedure, regardless of the respiratory symptoms, is therefore recommended by many authors4,13). Fortunately for our cases, pulmonary embolism did not occur. Great care must be used by the surgeon to prevent pulmonary embolism after vertebroplastic procedures.
In all of our cases, posterior lumbar interbody fusion (PLIF) using two PEEK cages and autologous local bone was performed. Because of the osteoporosis and the advanced age of the patients, cancellous bone from the iliac crest was not utilized for the posterior lumbar fusion thus reducing the operative time and reducing in perioperative complications. According to many publications, only the use of a local bone graft can achieve a reliable fusion rate21,24,38). The present study demonstrated that 34 patients (91.9%) of 37 patients satisfied the fusion criteria. One of the benefits of using PLIF cages is preventing the screw relaxation. By supporting the anterior spinal column with the interbody fusion, the possibility of an increased load on the screws in the weak cancellous bone caused by flexion-extension movement of the lumbar vertebra can be diminished. It is difficult to compare the fusion rate with other studies since there are no publications using a similar technique as ours. From the studies of others, the mean age was younger than the patients of the present study but, during 2 years of follow up, the fusion rates were similar (89-95%)5,8,11,24). The fusion rate of our study is comparatively high, given the patient conditions, i.e., an older age group and the presence of osteoporosis. Usually, for severe osteoporosis, the anchoring strength of the screw to the vertebra is lacking, when transpedicular screw fixation is used, so that the fixation failure of the pedicle screw occurs very often and raises the possibility of nonunion. Transpedicular screw placement with PMMA is considered as one of the options resulting in a better holding strength and ultimately a better chance of union.
The problems of screw-loosening, which may lead to nonunion of the spine, has not been solved completely by pedicle screw fixation, as it's rate still ranges from 0.6% to 11% in the literature cases reviewed by Esses et al.9). The risk of screw-loosening is an inevitable concern when this procedure is performed in the osteoporotic spine. It has been demonstrated that BMD in the lumbar vertebra affects the stability of pedicle screws in vitro25,35,43). In vivo, however, there are very few studies that describe the influence of BMD on the stability of pedicle screws. Okuyama et al.23) performed a study with patients who underwent PLIF and stated that the mean BMD of patients with "union" and "without screw loosening" was significantly greater than those with "nonunion" and "screw loosening". They also stated that BMD is a crucial factor influencing the development of loosening and nonunion in pedicle screw fixation. In this study, screw loosening was observed in one patient (2.7%) and nonunion in 3 patients (8.1%). All those patients had severe osteoporosis (T-score less than -4.0). And moreover, 50% of the total 6 patients who had T-scores less than -4.0, did not achieve fusion after all. Otherwise, the patients with T-scores of -3.9 and above did not experience both screw loosening and nonunion. Thus, BMD can be the most important factor which affects pedicle screw fixation regarding screw loosening and nonunion. Even PMMA augmentation using cannulated pedicle screw fixation cannot be regarded as a complete solution for a serious osteoporosis, i.e., T score ≤ -4.0. It should be remembered that PMMA augmentation simply increases the physical interaction of titanium implants with the interstices of cancellous bone. Ultimately, repetitive cyclic loading in the absence of an effective interbody fusion will result in implant and PMMA loosening.
CONCLUSION
According to the results of this paper, PMMA-augmentation with cannulated pedicle screw fixation is an excellent instrumentation method for use in the osteoporotic spine. It is a safe and effective procedure with a low complication rate compared with other methods. The injection of PMMA through a cannulated pedicle screw has been shown to be beneficial when an instrumented fusion is necessary for osteoporotic spine by adding fixation strength. However, more cases and longer follow-up duration are needed. In addition, further evaluations regarding the effectiveness of the PMMA augmentation method for the fusion in patients with severe osteoporosis will be required in the future.
References
- 1.Amar AP, Larsen DW, Esnaashari N, Albuquerque FC, Lavine SD, Teitelbaum GP. Percutaneous transpedicular polymethylmethacrylate vertebroplasty for the treatment of spinal compression fractures. Neurosurgery. 2001;49:1105–1114. discussion 1114-1115. [PubMed] [Google Scholar]
- 2.Cameron HU, Jacob R, Macnab I, Pilliar RM. Use of polymethylmethacrylate to enhance screw fixation in bone. J Bone Joint Surg Am. 1975;57:655–656. [PubMed] [Google Scholar]
- 3.Chiras J, Depriester C, Weill A, Sola-Martinez MT, Deramond H. [percutaneous vertebral surgery. Technics and indications] J Neuroradiol. 1997;24:45–59. [PubMed] [Google Scholar]
- 4.Choe DH, Marom EM, Ahrar K, Truong MT, Madewell JE. Pulmonary embolism of polymethyl methacrylate during percutaneous vertebroplasty and kyphoplasty. AJR Am J Roentgenol. 2004;183:1097–1102. doi: 10.2214/ajr.183.4.1831097. [DOI] [PubMed] [Google Scholar]
- 5.Cook SD, Barbera J, Rubi M, Salkeld SL, Whitecloud TS., 3rd Lumbosacral fixation using expandable pedicle screws. An alternative in reoperation and osteoporosis. Spine J. 2001;1:109–114. doi: 10.1016/s1529-9430(01)00020-1. [DOI] [PubMed] [Google Scholar]
- 6.Cook SD, Salkeld SL, Stanley T, Faciane A, Miller SD. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J. 2004;4:402–408. doi: 10.1016/j.spinee.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 7.Cortet B, Cotten A, Boutry N, Flipo RM, Duquesnoy B, Chastanet P, et al. Percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures : An open prospective study. J Rheumatol. 1999;26:2222–2228. [PubMed] [Google Scholar]
- 8.Dehoux E, Fourati E, Madi K, Reddy B, Segal P. Posterolateral versus interbody fusion in isthmic spondylolisthesis : functional results in 52 cases with a minimum follow-up of 6 years. Acta Orthop Belg. 2004;70:578–582. [PubMed] [Google Scholar]
- 9.Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine (Phila Pa 1976) 1993;18:2231–2238. doi: 10.1097/00007632-199311000-00015. discussion 2238-2239. [DOI] [PubMed] [Google Scholar]
- 10.Flahiff CM, Gober GA, Nicholas RW. Pullout strength of fixation screws from polymethylmethacrylate bone cement. Biomaterials. 1995;16:533–536. doi: 10.1016/0142-9612(95)91126-j. [DOI] [PubMed] [Google Scholar]
- 11.Fogel GR, Toohey JS, Neidre A, Brantigan JW. Is one cage enough in posterior lumbar interbody fusion : a comparison of unilateral single cage interbody fusion to bilateral cages. J Spinal Disord Tech. 2007;20:60–65. doi: 10.1097/01.bsd.0000211251.59953.a4. [DOI] [PubMed] [Google Scholar]
- 12.Frankel BM, D'Agostino S, Wang C. A biomechanical cadaveric analysis of polymethylmethacrylate-augmented pedicle screw fixation. J Neurosurg Spine. 2007;7:47–53. doi: 10.3171/SPI-07/07/047. [DOI] [PubMed] [Google Scholar]
- 13.Frankel BM, Jones T, Wang C. Segmental polymethylmethacrylate-augmented pedicle screw fixation in patients with bone softening caused by osteoporosis and metastatic tumor involvement : a clinical evaluation. Neurosurgery. 2007;61:531–537. doi: 10.1227/01.NEU.0000290899.15567.68. discussion 537-538. [DOI] [PubMed] [Google Scholar]
- 14.Fransen P. Increasing pedicle screw anchoring in the osteoporotic spine by cement injection through the implant. Technical note and report of three cases. J Neurosurg Spine. 2007;7:366–369. doi: 10.3171/SPI-07/09/366. [DOI] [PubMed] [Google Scholar]
- 15.Gaughen JR, Jr, Jensen ME, Schweickert PA, Kaufmann TJ, Marx WF, Kallmes DF. Relevance of antecedent venography in percutaneous vertebroplasty for the treatment of osteoporotic compression fractures. AJNR Am J Neuroradiol. 2002;23:594–600. [PMC free article] [PubMed] [Google Scholar]
- 16.Hernigou P, Duparc F. Rib graft or cement to enhance screw fixation in anterior vertebral bodies. J Spinal Disord. 1996;9:322–325. [PubMed] [Google Scholar]
- 17.Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures : Technical aspects. AJNR Am J Neuroradiol. 1997;18:1897–1904. [PMC free article] [PubMed] [Google Scholar]
- 18.Kanis JA, Melton LJ, 3rd, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9:1137–1141. doi: 10.1002/jbmr.5650090802. [DOI] [PubMed] [Google Scholar]
- 19.Kostuik JP, Errico TJ, Gleason TF. Techniques of internal fixation for degenerative conditions of the lumbar spine. Clin Orthop Relat Res. 1986:219–231. [PubMed] [Google Scholar]
- 20.Lotz JC, Hu SS, Chiu DF, Yu M, Colliou O, Poser RD. Carbonated apatite cement augmentation of pedicle screw fixation in the lumbar spine. Spine (Phila Pa 1976) 1997;22:2716–2723. doi: 10.1097/00007632-199712010-00003. [DOI] [PubMed] [Google Scholar]
- 21.Madan SS, Boeree NR. Comparison of instrumented anterior interbody fusion with instrumented circumferential lumbar fusion. Eur Spine J. 2003;12:567–575. doi: 10.1007/s00586-002-0516-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McKoy BE, An YH. An injectable cementing screw for fixation in osteoporotic bone. J Biomed Mater Res. 2000;53:216–220. doi: 10.1002/(sici)1097-4636(2000)53:3<216::aid-jbm5>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 23.Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Influence of bone mineral density on pedicle screw fixation : A study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine J. 2001;1:402–407. doi: 10.1016/s1529-9430(01)00078-x. [DOI] [PubMed] [Google Scholar]
- 24.Okuyama K, Kido T, Unoki E, Chiba M. PLIF with a titanium cage and excised facet joint bone for degenerative spondylolisthesis- in augmentation with a pedicle screw. J Spinal Disord Tech. 2007;20:53–59. doi: 10.1097/01.bsd.0000211243.44706.2b. [DOI] [PubMed] [Google Scholar]
- 25.Okuyama K, Sato K, Abe E, Inaba H, Shimada Y, Murai H. Stability of transpedicle screwing for the osteoporotic spine. An in vitro study of the mechanical stability. Spine (Phila Pa 1976) 1993;18:2240–2245. doi: 10.1097/00007632-199311000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Orimo H, Hayashi Y, Fukunaga M, Sone T, Fujiwara S, Shiraki M, et al. Diagnostic criteria for primary osteoporosis : year 2000 revision. J Bone Miner Metab. 2001;19:331–337. doi: 10.1007/s007740170001. [DOI] [PubMed] [Google Scholar]
- 27.Peh WC, Gilula LA, Peck DD. Percutaneous vertebroplasty for severe osteoporotic vertebral body compression fractures. Radiology. 2002;223:121–126. doi: 10.1148/radiol.2231010234. [DOI] [PubMed] [Google Scholar]
- 28.Pérez-Higueras A, Alvarez L, Rossi RE, Quinones D, Al-Assir I. Percutaneous vertebroplasty : Long-term clinical and radiological outcome. Neuroradiology. 2002;44:950–954. doi: 10.1007/s00234-002-0856-1. [DOI] [PubMed] [Google Scholar]
- 29.Pfeifer BA, Krag MH, Johnson C. Repair of failed transpedicle screw fixation. A biomechanical study comparing polymethylmethacrylate, milled bone, and matchstick bone reconstruction. Spine (Phila Pa 1976) 1994;19:350–353. doi: 10.1097/00007632-199402000-00017. [DOI] [PubMed] [Google Scholar]
- 30.Prolo DJ, Oklund SA, Butcher M. Toward uniformity in evaluating results of lumbar spine operations. A paradigm applied to posterior lumbar interbody fusions. Spine (Phila Pa 1976) 1986;11:601–606. doi: 10.1097/00007632-198607000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Righini M, Sekoranja L, Le Gal G, Favre I, Bounameaux H, Janssens JP. Pulmonary cement embolism after vertebroplasty. Thromb Haemost. 2006;95:388–389. [PubMed] [Google Scholar]
- 32.Ryu KS, Park CK, Kim MC, Kang JK. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg. 2002;96:56–61. doi: 10.3171/spi.2002.96.1.0056. [DOI] [PubMed] [Google Scholar]
- 33.Sarzier JS, Evans AJ, Cahill DW. Increased pedicle screw pullout strength with vertebroplasty augmentation in osteoporotic spines. J Neurosurg. 2002;96:309–312. doi: 10.3171/spi.2002.96.3.0309. [DOI] [PubMed] [Google Scholar]
- 34.Seo JS, Kim YJ, Choi BW, Kim TH, Choe KO. MDCT of pulmonary embolism after percutaneous vertebroplasty. AJR Am J Roentgenol. 2005;184:1364–1365. doi: 10.2214/ajr.184.4.01841364. [DOI] [PubMed] [Google Scholar]
- 35.Soshi S, Shiba R, Kondo H, Murota K. An experimental study on transpedicular screw fixation in relation to osteoporosis of the lumbar spine. Spine (Phila Pa 1976) 1991;16:1335–1341. doi: 10.1097/00007632-199111000-00015. [DOI] [PubMed] [Google Scholar]
- 36.Steffee AD, Biscup RS, Sitkowski DJ. Segmental spine plates with pedicle screw fixation. A new internal fixation device for disorders of the lumbar and thoracolumbar spine. Clin Orthop Relat Res. 1986:45–53. [PubMed] [Google Scholar]
- 37.Takigawa T, Tanaka M, Konishi H, Ikuma H, Misawa H, Sugimoto Y, et al. Comparative biomechanical analysis of an improved novel pedicle screw with sheath and bone cement. J Spinal Disord Tech. 2007;20:462–467. doi: 10.1097/bsd.0b013e318030d2d6. [DOI] [PubMed] [Google Scholar]
- 38.Trouillier H, Birkenmaier C, Rauch A, Weiler C, Kauschke T, Refior HJ. Posterior lumbar interbody fusion (PLIF) with cages and local bone graft in the treatment of spinal stenosis. Acta Orthop Belg. 2006;72:460–466. [PubMed] [Google Scholar]
- 39.Urist MR. Acrylic cement stabilized joint replacements. Curr Probl Surg. 1975:1–54. doi: 10.1016/s0011-3840(75)80007-4. [DOI] [PubMed] [Google Scholar]
- 40.Wenger M, Markwalder TM. Surgically controlled, transpedicular methyl methacrylate vertebroplasty with fluoroscopic guidance. Acta Neurochir (Wien) 1999;141:625–631. doi: 10.1007/s007010050352. [DOI] [PubMed] [Google Scholar]
- 41.Wilkes RA, Mackinnon JG, Thomas WG. Neurological deterioration after cement injection into a vertebral body. J Bone Joint Surg Br. 1994;76:155. [PubMed] [Google Scholar]
- 42.Wittenberg RH, Lee KS, Shea M, White AA, 3rd, Hayes WC. Effect of screw diameter, insertion technique, and bone cement augmentation of pedicular screw fixation strength. Clin Orthop Relat Res. 1993:278–287. [PubMed] [Google Scholar]
- 43.Wittenberg RH, Shea M, Swartz DE, Lee KS, White AA, 3rd, Hayes WC. Importance of bone mineral density in instrumented spine fusions. Spine (Phila Pa 1976) 1991;16:647–652. doi: 10.1097/00007632-199106000-00009. [DOI] [PubMed] [Google Scholar]
- 44.Wuisman PI, Van Dijk M, Staal H, Van Royen BJ. Augmentation of (pedicle) screws with calcium apatite cement in patients with severe progressive osteoporotic spinal deformities An innovative technique. Eur Spine J. 2000;9:528–533. doi: 10.1007/s005860000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yazu M, Kin A, Kosaka R, Kinoshita M, Abe M. Efficacy of novel-concept pedicle screw fixation augmented with calcium phosphate cement in the osteoporotic spine. J Orthop Sci. 2005;10:56–61. doi: 10.1007/s00776-004-0862-8. [DOI] [PubMed] [Google Scholar]
- 46.Yoo KY, Jeong SW, Yoon W, Lee J. Acute respiratory distress syndrome associated with pulmonary cement embolism following percutaneous vertebroplasty with polymethylmethacrylate. Spine (Phila Pa 1976) 2004;29:E294–E297. doi: 10.1097/01.brs.0000131211.87594.b0. [DOI] [PubMed] [Google Scholar]
- 47.Zindrick MR, Wiltse LL, Widell EH, Thomas JC, Holland WR, Field BT, et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986:99–112. [PubMed] [Google Scholar]