Abstract
Objective
The purpose of this study was to evaluate the efficacy of a transforaminal suprapedicular approach, semi-rigid flexible curved probe, and 3-dimensional reconstruction computed tomography (3D-CT) with discogram in the endoscopic treatment of non-contained lumbar disc herniations.
Methods
The subjects were 153 patients with difficult, non-contained lumbar disc herniations undergoing endoscopic treatment. The types of herniation were as follows : extraforaminal, 17 patients; foraminal, 21 patients; high grade migration, 59 patients; and high canal compromise, 56 patients. To overcome the difficulties in endoscopic treatment, the anatomic structures were analyzed by 3D reconstruction CT and the high grade disc was extracted using a semi-rigid flexible curved probe and a transforaminal suprapedicular approach.
Results
The mean follow-up was 18.3 months. The mean visual analogue scale (VAS) of the patients prior to surgery was 9.48, and the mean postoperative VAS was 1.63. According to Macnab's criteria, 145 patients had excellent and good results, and thus satisfactory results were obtained in 94.77% cases.
Conclusion
In a posterolateral endoscopic lumbar discectomy, the difficult, non-contained disc is considered to be the most important factor impeding the success of surgery. By applying a semi-rigid flexible curved probe and using a transforaminal suprapedicular approach, good surgical results can be obtained, even in high grade, non-contained disc herniations.
Keywords: Intervertebral disc herniation, Percutaneous discectomy, Posterolateal approach
INTRODUCTION
Herniated disc material can be contained or noncontained. In the case of noncontained disc herniation, relatively large amount of disc material can be displaced and even sequestered and migrated. Therefore, it is not easy to remove disc fragments successfully by minimal invasive surgical treatment.
Although new techniques have been developed for percutaneous endoscopic discectomies, a microscopic discectomy has been the standard method for treatment of lumbar disc diseases1,2,19,20). Especially in cases of non-contained disc herniations, it is difficult to remove the disc fragment safely by a percutaneous endoscopic method. Recently, improved results of percutaneous endoscopic discectomies have been reported1,5,8,10,13,17,18,20,21,29). The percutaneous endoscopic approach is limited by the difficulty in reaching the lesion due to anatomic barriers and it has been the major cause of post-operative remnant disc materials. Specifically, in cases of a compromised high grade canal or high grade migrated disc herniation, it is difficult to reach to the lesion in the epidural space initially or in the migrated disc area14-16). To overcome such limitations of endoscopic methods, we analyzed anatomic structures by three-dimensional (3D) reconstruction computed tomography (CT) images with a discogram pre-operatively and applied a transforaminal suprapedicular approach for high grade inferior-migrated disc herniations, and a posterolateral approach for high grade non-contained disc hermiations using a semi-rigid flexible curved probe. The purpose of this study was to determine the usefulness of pre-operative 3D reconstruction CT images with a discogram and a semi-rigid flexible curved probe.
MATERIALS AND METHODS
Between August 2004 and October 2007, the study population consisted of 153 consecutive patients with radiculopathies due to high grade, non-contained-type disc herniations in which a rigid endoscope assessment was difficult and they were treated with PELD5). All patients met the following criteria : 1) unilateral radicular leg pain, 2) high grade, migrated or compromised disc herniation and foraminal or extraforaminal non-contained disc herniations without stenosis at a single-level, 3) no history of previous lumbar surgery, 4) failure of appropriate conservative treatment, and 5) no calcified disc herniations. All of the cases were classified into 4 types (high canal compromise, high grade downward migration, foraminal, and extraforaminal), according to pre-operative magnetic resonance (MR) images and CT scans with discograms. The symptoms corresponded with the pre-operative images. According to the pre-operative images, the types of herniations were as follows : high grade migration type far-downward from the center to the inferior margin of the lower pedicle14,15), 59 cases; high canal compromised type herniation exceeding 50% of the canal cross-sectional area compromise14), 56 cases; non-contained extraforaminal type, 17 cases; and non-contained foraminal type, 21 cases.
Anesthesia
Epidural anesthesia was performed in all cases. Either 100 µg of fentanyl and 0.5% pucain were diluted by 1/2 and prepared as a 0.25% solution and approximately 15-20 cc was injected into the epidural space or 15-20 cc of 0.5% pucain stock solution was injected into the epidural space. Anesthesia was assessed by checking the sensory level, and surgery was then performed9,11,23,26). During surgery, the anesthesia was not sufficient to block the nerve root completely, so we could detect the patient's sensory and motor changes.
Surgical technique
The sequence of surgery was identical to the general transforaminal endoscopic procedure1,21,22,25). Prior to the procedure, using indigo-carmine dye, evocative chromodiskography18,22) was performed. In the cases of high canal compromised and high grade communicated migration types, assessment was via a posterolateral approach was used26,27,30). In the cases of a high grade non-communicated inferior sequestrated type, we accessed the pathology by an extreme lateral route24) and suprapedicular approach12) simultaneously. A 1 cm skin incision was made 8-12 cm from the midline according to the herniated disc type. An operative sheath (YESS System; Wolf, Knittlingen, Germany) was installed in the disc space. If the case required disc decompression, it was better to first perform decompression identical to the posterolateral procedure1,17,21,22). After completion of the decompression, the cannula was removed carefully from the foraminal space, and moved to the target disc fragment. In the endoscopic view, the blue-stained disc fragment was visible at the upper quadrant of the view, but a straight probe or forceps could not reach the disc area, so we used a semi-rigid flexible curved probe (RZ Medizin Technik GmBH, Tuttlimigen, Germany) to carefully hook and pull the disc material out to the center of the endoscopic view. Then, a forceps could reach the disc fragment and easily remove it. In the case of a high grade inferior migrated disc herniation, an immediate suprapedicular approach was preferred. In the suprapedicular approach, after disc extraction, the pedicle was surrounded by abundant soft tissues, fat, and blood vessels. The superior margin of the pedicle was secured by removing these structures completely using a high voltage bipolar probe manufactured by Ellman (Ellman Innovation, New York, NY, USA) and forceps. If the pedicle and upper margin of the lower vertebra were properly prepared, a sufficient space to perform the suprapedicular approach was obtained. If the disc material was extracted and thus nerve root decompression was sufficient, massive bleeding could obscure the structural findings in the endoscopic view. However, this bleeding could be controlled by bipolar coagulation and saline irrigation, and the sufficiently movable traversing nerve root could be assessed. Upon performing the procedure, the epidural space and the traversing nerve root was exposed, and occasionally the ruptured disc material was exposed first and thus it could be removed readily. However, the inferior migrated ruptured material was present below the traversing nerve root in most cases, and care was exercised so as not to injure the traversing nerve root.
Evaluation
Based on the MRI and 3D CT image with the discogram prior to surgery, the migration and lesion types were analyzed. Approximately 1-4 hours after surgery, the remnant disc was assessed by checking with a MRI. One month after surgery, the improvement level of the patient was evaluated by the Visual Analogue Pain Score (VAS), including neurologic tests and MacNab's criteria.
RESULTS
There were 68 male and 85 female patients. The age distribution of patients is as follows : adolescence (6), 20s (21), 30s (33), 40s (36), 50s (28), 60s (24), and 70s (5). According to our classification of non-contained disc herniations, the extraforaminal type affected 17 patients [L2-3 (1), L3-4 (5), L4-5 (5), and L5-S1 (6)], the foraminal type affected 21 patients, [L2-3 (1), L3-4 (5), L4-5 (10), and L5-S1 (5)], the high grade migration type affected 59 patients [L2-3 (1), L3-4 (11), L4-5 (47), and L5-S1 (0)], and the high canal compromised type affected 56 patients [L2-3 (0), L3-4 (12), L4-5 (44), and L5-S1 (0)]. Mean follow-up was 18.3 month (range 8-36 months). The mean preoperaitive visual analogue scale (VAS) for leg pain was 9.48, At the last follow-up examination, after an average period of more than 6 months postoperatively, the mean VAS for leg pain was was 1.63.
According to MacNab's criteria, 99 patients (64.71%) had excellent results, 46 patients (30.07%) had good results; thus, satisfactory results were achieved in 145 patients (94.77%). Six patients (3.92%) had fair results, and 2 patients (1.31%) had poor results. In one case, a huge paravertebral hematoma developed after surgery; however, after bed rest, it resolved without any neurologic deficits. In 3 cases, transient paresis developed, but resolved during follow-up over a 1 week period. In another case, a cerebral infarction unrelated to surgery developed, and thus treatment was performed. In 9 cases, transient hypesthesia developed, and in 8 patients the transient hypesthesia resolved during follow-up in 1-3 weeks, but 1 patient had sustained symptoms after 6 months.
DISCUSSION
Herniated disc material can be contained or noncontained. Disc herniation is described as contained, if the displaced portion is covered by outer annulus. The noncontained disc herniation is defined when absent any such covering. A disc with a contained herniation would not leak into the vertebral canal fluid that has been injected into the disc. Containment refers to the integrity of the outer annulus covering the disc herniation9).
In the cases of noncontained disc herniation, relatively large amount of disc material is displaced and often sequestered and migrated. Therefore, it is not easy to remove successfully by surgical treatment.
The success rates of discectomy for lumbar disc herniation have improved greatly and range from 80% to 96%. Generally, microscopic discectomy after laminotomy is still considered the gold standard2,3,7,14,19), but recently numerous studies involving endoscopic discectomy have been reported, and the outcomes have been improving gradually1,2,10,13-17,20-22,29). However, the lateral approach endoscopic discectomy has many limitations due to anatomic barriers, such as the iliac wing. The height of the working disc space should be adequate8) and the working disc space must be approached through the foraminal space, which is difficult10). Therefore, due to anatomic reasons, the indications for endoscopic surgery are limited and endoscopic surgery is relatively contraindicated for non-contained high grade canal compromise or migration type cases18,20).
In the case of a high canal compromised type herniation, the epidural space is very narrow (Fig. 1). Therefore, a decompressive discetomy should be done in advance so as not to injure the nerve via compression when endoscopic devices enter into the disc space. The working cannula and endoscope should not enter the disc space deeply until identifying the yellow ligaments and annulus fibrosus; after identifying the yellow ligaments and annulus fibrosus, these structures should be carefully cut and a small hole should be made in the annulus, through which the disc materials are removed by forceps from the superficial to deeper disc.
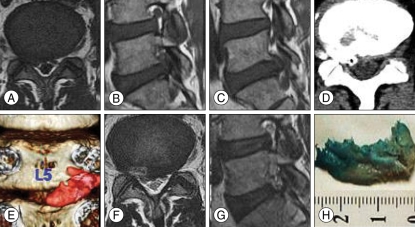
Fig. 1.
High grade canal compromised type. Pre-operative magnetic resonance (MR) images show herniated disc material encroaching the canal by more than one-half (A and B). Discogram with computed tomogtaphy image show non-contained disc herniation (C). Post-MR image showing disc materials removed successfully and the dural sac re-expanded (D and E).
If sufficient vacant disc space is secured by a decompressed discectomy, the endoscope can be carefully advanced into the central disc space. At that time, the dura is not invisible because it is hidden by ruptured expulsed disc material, so we carefully catch the disc fragments with forceps and extract the disc material, and finally identify the dura and nerve root surrounded by epidural fat.
In the cases of foraminal and extraforaminal types of herniation, the disc material is located closer than the other types and behind and under the exiting nerve root (Fig. 2). For the purpose of securing a safety zone, the angle of the endoscope accessing the ruptured disc material would be steeper (angle, 30-45°). Without a decompressive discectomy, fragments can be identified and removed easily in the intervertebral foraminal space. In the cases of extraforaminal or far lateral disc type herniations, the PELD can remove the disc material effectively and decompress the nerve root safely without fusion. In cases of high grade inferior migration-type lumbar disc herniation, the success rate of endoscopic discectomy is lower18,20) because the endoscopic access to the lesion is interrupted by anatomic structures and a rigid endoscope and a probe cannot reach the lesion. Some surgeons have reported that other methods, such as the extreme lateral access24) and epiduroscopic approach18), and flexible working channel scope could solve such problems (Fig. 3)10). The transforaminal suprapedicular approach is a method to remove the migrated disc through the foraminal narrow space above the pedicle of the lower vertebra. The transforaminal suprapedicular approach has several advantages. The manipulation is performed at the foraminal level and thus it could have a sufficient angle to reach the migrated disc, the epidural space could be approached readily, and sufficient assessment of root decompression and disc extraction is feasible. If a working cannula is installed in the disc space and subsequently the cannula is moved to the upper margin of the lower vertebral pedicle, the surrounding soft tissues can be clearly arranged by a high voltage bipolar probe (Ellman Innovation, New York, NY, USA) and forceps. The suprapedicular entry space can be prepared (Fig. 1C, D). Through this route, the inferior-migrated disc material can be extracted by performing an epiduroscopic approach with the use of a semi-rigid flexible curved probe. To remove the disc materials successfully by PELD in the noncontained disc herniation, it is important to know the information about disc material, such as volume, single or multiple pieces, direction, anatomic relationship, and location of the target disc fragment. This information can be obtained by 3D reconstruction CT and help to determine the direction of the working cannula accessing the disc fragments. According to 3D reconstruction CT images, the target disc material can be accessed and the disc material can be safely extracted. However, targeted disc fragments are often visible in the endoscopic view, but straight forceps cannot reach the target. Then, a semi-rigid curved probe is inserted into the target disc material. This probe is manipulated to hook the disc material and move it to the center space on endoscopic view, then the disc material is caught firmly by straight forceps and disc material is successfully and safely extracted.
Fig. 2.
High grade non-contained foraminal disc. Pre-operative magnetic resonance (MR) images shows right huge non-contained L5-S1 foraminal disc (A, B and C). Preoperative 3D computed tomography image with discogram shows disc material herniated through the foramen between the right L5 and S1 pedicle (D and E) Post-operative MR images shows foraminal disc material extracted completely (F, G and H).
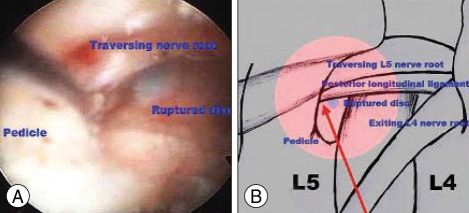
Fig. 3.
Suprapedicular approach. The epidural space is exposed by clearing around the pedicle, and the lesional disc can be removed through this point. A : Intra-operative view. B : Schematic drawing. The red round area indicates the intra-operative view (A), Red arrow : Pathway of suprapedicular approach.
CONCLUSION
In many cases of non-contained high grade disc herniations, especially in high grade canal compromised or high grade inferior migrated types, it is difficult to remove disc material successfully and safely by the percutaneous endoscopic approach. In these cases, it is important to know information about disc materials and accurately analyze the anatomic limitations by pre-operative 3D CT with a discogram study. It helps us to determine the proper endoscopic surgical approach route to the disc material. During the endoscopic approach, a semi-rigid flexible curved probe and suprapedicular approach is very useful to remove the disc materials that straight forceps cannot reach in the endoscopic view.
Acknowledgements
This paper was supported by research fund from Chosun University in 2009.
References
- 1.Abdullah AF, Wolber PG, Warfield JR, Gunadi IK. Surgical management of extreme lateral lumbar disc herniations : review of 138 cases. Neurosurgery. 1988;22:648–653. doi: 10.1227/00006123-198804000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation : surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976) 2004;29:E326–E332. doi: 10.1097/01.brs.0000134591.32462.98. [DOI] [PubMed] [Google Scholar]
- 3.Andrews DW, Lavyne MH. Retrospective analysis of microsurgical and standard lumbar discectomy. Spine (Phila Pa 1976) 1990;15:329–335. doi: 10.1097/00007632-199004000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Asch HL, Lewis PJ, Moreland DB, Egnatchik JG, Yu YJ, Clabeaux DE, et al. Prospective multiple outcomes study of outpatient lumbar microdiscectomy : should 75 to 80% success rates be the norm? J Neurosurg. 2002;96:34–44. doi: 10.3171/spi.2002.96.1.0034. [DOI] [PubMed] [Google Scholar]
- 5.Choi G, Lee SH, Bhanot A, Raiturker PP, Chae YS. Percutaneous endoscopic discectomy for extraforaminal lumbar disc herniations : extraforaminal targeted fragmentectomy technique using working channel endoscope. Spine (Phila Pa 1976) 2007;32:E93–E99. doi: 10.1097/01.brs.0000252093.31632.54. [DOI] [PubMed] [Google Scholar]
- 6.Choi G, Lee SH, Raiturker PP, Lee S, Chae YS. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery. 2006;58:S59–S68. doi: 10.1227/01.neu.0000192713.95921.4a. discussion S59-S68. [DOI] [PubMed] [Google Scholar]
- 7.Donceel P, Du Bois M. Fitness for work after lumbar disc herniation : a retrospective study. Eur Spine J. 1998;7:29–35. doi: 10.1007/s005860050023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Epstein NE. Evaluation of varied surgical approaches used in the management of 170 far-lateral lumbar disc herniations : Indications and results. J Neurosurg. 1995;83:648–656. doi: 10.3171/jns.1995.83.4.0648. [DOI] [PubMed] [Google Scholar]
- 9.Fardon DF, Milette PC Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976) 2001;26:E93–E113. doi: 10.1097/00007632-200103010-00006. [DOI] [PubMed] [Google Scholar]
- 10.Fritsch EW, Heisel J, Rupp S. The failed back surgery syndrome : Reasons, intraoperative findings and long term results : A report of 182 operative treatments. Spine (Phila Pa 1976) 1996;21:626–633. doi: 10.1097/00007632-199603010-00017. [DOI] [PubMed] [Google Scholar]
- 11.Kambin P, Cohen LF, Brooks M, Schaffer JL. Development of degenerative spondylosis of the lumbar spine after partial discectomy. Comparison of laminotomy, discectomy and posterolateral discectomy. Spine (Phila Pa 1976) 1995;20:599–607. doi: 10.1097/00007632-199503010-00018. [DOI] [PubMed] [Google Scholar]
- 12.Knop-Jergas BM, Zucherman JF, Hsu KY, DeLong B. Anatomic position of a herniated nucleus pulposus predicts the outcome of lumbar discectomy. J Spinal Disord. 1996;9:246–250. [PubMed] [Google Scholar]
- 13.Kotilainen E. Long-term outcome of patients suffering from clinical instability after microsurgical treatment of lumbar disc herniation. Acta Neurochir (Wien) 1998;140:120–125. doi: 10.1007/s007010050072. [DOI] [PubMed] [Google Scholar]
- 14.Lee SH, Kang BU, Ahn Y, Choi G, Choi YG, Ahn KU, et al. Operative failure of percutaneous endoscopic lumbar discectomy : a radiologic analysis of 55 cases. Spine (Phila Pa 1976) 2006;31:E285–E290. [PubMed] [Google Scholar]
- 15.Lee S, Kim SK, Lee SH, Kim WJ, Choi WC, Choi G, et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation : classification of disc migration and surgical approaches. Eur Spine J. 2007;16:431–437. doi: 10.1007/s00586-006-0219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewis PJ, Weir BK, Broad RW, Grace MG. Long-term prospective study of lumbosacral discectomy. J Neurosurg. 1987;67:49–53. doi: 10.3171/jns.1987.67.1.0049. [DOI] [PubMed] [Google Scholar]
- 17.Lew SM, Mehalic TF, Fagone KL. Transforaminal percutaneous endoscopic discectomy in the treatment of far-lateral and foraminal lumbar disc herniations. J Neurosurg. 2001;94:216–220. doi: 10.3171/spi.2001.94.2.0216. [DOI] [PubMed] [Google Scholar]
- 18.Mayer HM, Brock M. Percutaneous endoscopic discectomy : surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993;78:216–225. doi: 10.3171/jns.1993.78.2.0216. [DOI] [PubMed] [Google Scholar]
- 19.McCulloch JA. Principles of Microsurgery for Lumbar Disc Diseases. New York: Raven Press; 1989. [Google Scholar]
- 20.Mekhail N, Kapural L. Intradiscal thermal annuloplasty for discogenic pain : an outcome study. Pain Pract. 2004;4:84–90. doi: 10.1111/j.1533-2500.2004.04203.x. [DOI] [PubMed] [Google Scholar]
- 21.Ozer AF, Oktenoglu T, Sasani M, Bozkus H, Canbulat N, Karaarslan E, et al. Preserving the ligamentum flavum in lumbar discectomy : a new technique that prevents scar tissue formation in the first 6 months postsurgery. Neurosurgery. 2006;59:ONS126–ONS133. doi: 10.1227/01.NEU.0000220078.90175.E6. discussion ONS126-ONS133. [DOI] [PubMed] [Google Scholar]
- 22.Porchet F, Chollet-Bornand A, de Tribolet N. Long-term follow up of patients surgically treated by the far-lateral approach for foraminal and extraforaminal lumbar disc herniations. J Neurosurg. 1999;90:59–66. doi: 10.3171/spi.1999.90.1.0059. [DOI] [PubMed] [Google Scholar]
- 23.Ross JS, Robertson JT, Frederickson RC, Petrie JL, Obuchowski N, Modic MT, et al. ADCON-L European Study Group. Association between peridural scar and recurrent radicular pain after lumbar discectomy : magnetic resonance evaluation. Neurosurgery. 1996;38:855–861. discussion 861-863. [PubMed] [Google Scholar]
- 24.Ruetten S, Meyer O, Godolias G. [Epiduroscopic diagnosis and treatment of epidural adhesions in chronic back pain syndrome of patients with previous surgical treatment : first results of 31 interventions.] Z Orthop Ihre Grenzgeb. 2002;140:171–175. doi: 10.1055/s-2002-31536. [DOI] [PubMed] [Google Scholar]
- 25.Sasani M, Ozer AF, Oktenoglu T, Canbulat N, Sarioglu AC. Percutaneous endoscopic discectomy for far lateral lumbar disc herniations : prospective study and outcome of 66 patients. Minim Invasive Neurosurg. 2007;50:91–97. doi: 10.1055/s-2007-984383. [DOI] [PubMed] [Google Scholar]
- 26.Tsou PM, Alan Yeung C, Yeung AT. Posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain : a minimal access visualized intradiscal surgical procedure. Spine J. 2004;4:564–573. doi: 10.1016/j.spinee.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 27.Tsou PM, Yeung AT. Transforaminal endoscopic decompression for radiculopathy secondary to intracanal noncontained lumbar disc herniations : outcome and technique. Spine (Phila Pa 1976) J. 2002;2:41–48. doi: 10.1016/s1529-9430(01)00153-x. [DOI] [PubMed] [Google Scholar]
- 28.Williams RW. Microlumbar discectomy. A 12-year statistical review. Spine (Phila Pa 1976) 1986;11:851–852. [PubMed] [Google Scholar]
- 29.Wu X, Zhuang S, Mao Z, Chen H. Microendoscopic discectomy for lumbar disc herniation : surgical technique and outcome in 873 consecutive cases. Spine (Phila Pa 1976) 2006;31:2989–2694. doi: 10.1097/01.brs.0000244615.43199.07. [DOI] [PubMed] [Google Scholar]
- 30.Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation. Surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976) 2002;27:722–731. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]