Abstract
Objective
The purpose of this study was to establish new fusion criteria to complement existing Brantigan-Steffee fusion criteria. The primary purpose of intervertebral cage placement is to create a proper biomechanical environment through successful fusion. The existence of a traction spur is an essential predictable radiologic factor which shows that there is instability of a fusion segment. We studied the relationship between the existence of a traction spur and fusion after a posterior lumbar interbody fusion (PLIF) procedure.
Methods
This study was conducted using retrospective radiological findings from patients who underwent a PLIF procedure with the use of a cage without posterior fixation between 1993 and 1997 at a single institution. We enrolled 183 patients who were followed for a minimum of five years after the procedure, and used the Brantigan-Steffee classification to confirm the fusion. These criteria include a denser and more mature bone fusion area than originally achieved during surgery, no interspace between the cage and the vertebral body, and mature bony trabeculae bridging the fusion area. We also confirmed the existence of traction spurs on fusion segments and non-fusion segments.
Results
The PLIF procedure was done on a total of 251 segments in 183 patients (71 men and 112 women). The average follow-up period was 80.4 ± 12.7 months. The mean age at the time of surgery was 48.3 ± 11.3 years (range, 25 to 84 years). Among the 251 segments, 213 segments (84.9%) were fused after five years. The remaining 38 segments (15.1%) were not fused. An analysis of the 38 segments that were not fused found traction spur formation in 20 of those segments (52.6%). No segments had traction spur formation with fusion.
Conclusion
A new parameter should be added to the fusion criteria. These criteria should be referred to as 'no traction spur formation' and should be used to confirm fusion after a PLIF procedure.
Keywords: Posterior lumbar interbody fusion, Instability, Traction spur
INTRODUCTION
One primary goal of spinal fusion is to remove pain-generating tissues and to alleviate the patient's pain by stabilization of one or more motion segments. Posterior lumbar interbody fusion (PLIF) is widely used as a treatment method for chronic degenerative spondylosis8). The PLIF procedure maintains decompression of neural elements and stabilizes fusion segments through anterior column fusion after disc removal. Various types of intervertebral cages have been developed to maintain the stability of fusion segments during the healing process1,19,22). Introduction of these cages prevents the disc space from collapsing and maintains stability until the fusion mass has healed. Therefore, the primary purpose of intervertebral cage placement is to create a proper biomechanical environment through successful fusion. In order to accomplish this, it is necessary for the fusion segment to be built up as a stiff post-operative structure through the intervertebral cage.
A review of the relevant literature shows that few parameters have been used to confirm the existence of a fusion segment, with the only definitive criterion being surgical exploration6,13,14). However, this is an invasive procedure, and it is difficult to apply in a real clinical setting. More realistic and efficient methods involve radiological imaging such as CT and X-ray. The Brantigan-Steffee classification is widely used to confirm successful intervertebral fusion. These criteria include : the bone in fusion area is more dense and more mature than originally achieved during surgery, no interspace between the cage and the vertebral body, and mature bony trabeculae bridging in fusion area2). But, the existence of a traction spur is an essential predictable radiologic factor which shows that there is instability of a fusion segment7,12,16,18). Therefore, absence of traction spur formation can be used to confirm intervertebral fusion after a PLIF procedure.
In this study, we introduced a new criterion for successful fusion, the nonexistence of a newly formed traction spur, in addition to the standard Brantigan-Steffee classification criteria. We analyzed fusion state for stand-alone cages using radiological findings during a minimum follow-up period of five years. We assessed the relationships between traction spur formation and fusion after PLIF procedures.
MATERIALS AND METHODS
Patients
This study was conducted using retrospective radiological findings from patients who underwent PLIF procedures with the use of cages without posterior fixation between 1993 and 1997 at a single institution. Ray-threaded fusion cages (Ray TFC Surgical Dynamics, Norwalk, CT, USA) and Brantigan I/F cages (Depuy Acromed Corp., Raynham, MA, USA) were used in PLIF procedures. A total of 183 patients were evaluated, with each of the patients having a minimum follow-up period of five years. All of the patients had a PLIF procedure using the same surgical technique.
Surgical technique
During surgery, the patients were placed in the prone position under general anesthesia. Laminectomy, medial facetectomy and discectomy were performed using routine techniques for neural decompression with removal of the entire posterior longitudinal ligament and anterior annulus. The procedure was primarily focused on the complete removal of the intervertebral disc and the cartilaginous end late to the anterior annulus using a shaver and curettes. The laminar bone chips which were obtained during the posterior decompression were prepared by removal of all of the soft tissues for impaction into the cages. Two cages were inserted into the disc space more than 5 mm from the posterior cortical margin. We did not place any additional bone grafts around and/or between the cages. Posterior screw fixation was not performed after insertion of the cages.
Radiologic evaluation
We used Brantigan-Steffee classification to confirm the existence of fusion2). These criteria include: the bone in fusion area is more dense and more mature than originally achieved during surgery, no interspace between the cage and the vertebral body, and mature bony trabeculae bridging in fusion area2). If one of the three criteria was not met, we classified the patient as being in a non-fusion state. We also confirmed the existence of a newly formed traction spur on fusion segments and non-fusion segments. Newly formed traction spur formation was defined as pairs of osteophytes that arose from the disco-vertebral junction, terminated at the level of the vertebral border. Traction spur should be 2 mm or more in length according to the classification of Macnab et al.12) The direction and angle of traction spur formation were not investigated since traction spur has variable directions and angles depend on the levels of disc9).
The Brantigan I/F cages were radiolucent, making it easy to confirm the presence of dense, mature bone fusion inside the cage. However, titanium Ray-TFC cages did not allow us to confirm bone fusion inside the cage due to radiological artifacts. When a radiolucent halo was seen around the cage, we concluded that there was an interspace around the radiolucent halo. We accepted the existence of a radiolucent clear zone surrounded by a sclerotic zone as "non-fusion" by evaluating lateral radiographs and CT images of the radiolucent halo (Fig. 1). Bony bridging was considered present if it was complete or incomplete. Complete bony bridging was estimated by radiological union of the endplates without discontinuity of the bone density and trabecular continuity from endplate to endplate without any interface or incompletion (Fig. 2).
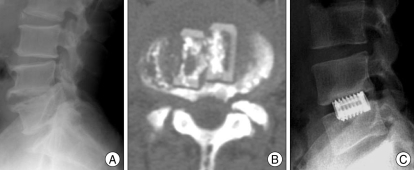
Fig. 1.
Lateral radiograph and Computerized tomography image showing a radiolucent halo around cages after posterior lumbar interbody fusion. A and B : lateral radiograph (A) and computerized tomography image (B) showing a radiolucent halo around cages at 64 months after posterior lumbar interbody fusion (PLIF) using brantigan interbody fusion cages. C : lateral radiograph showing a radiolucent halo around cages at 60 months after PLIF using ray-threaded fusion Cages
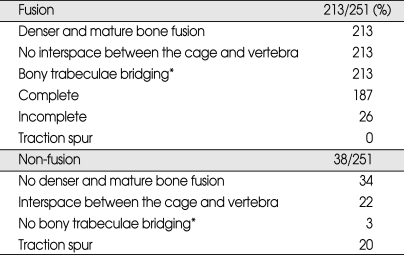
Fig. 2.
Lumbar plain lateral radiograph films showing complete bony trabeculae bridging beyond the cages after posterior lumbar interbody fusion. A : Lumbar plain lateral radiograph films showing complete bony trabeculae bridging beyond the cages at 68 months after posterior lumbar interbody fusion (PLIF) using Ray-threaded fusion cages. B : Lumbar plain lateral radiograph films showing complete bony trabeculae bridging beyond the cages at 64 months after PLIF using Brantigan Interbody fusion cages.
Clinical evaluation
The Oswestry disability index was used to evaluate the level of clinical satisfaction5). A Student's two-tailed t-test was used to compare the index scores obtained from the fused and non-fused groups. A p value less than 0.05 was considered to be statistically significant.
RESULTS
PLIF procedures were performed on a total of 251 segments in 183 patients (71 men and 112 women). The mean follow-up period was 80.4 ± 12.7 months. Men accounted for 39% of the patient population. The average age of patients was 48.3 years (range 25-84). The diseases responsible for enrollment of patients in the study included the following : herniated lumbar disc in 120 cases, spondyl-otic stenosis in 16 cases, degenerative spondylolisthesis in 30 cases, and spondylolytic spondylolisthesis in 17 cases (Table 1). Four patients had the procedure at the L2/3 level, 28 patients at the L3/4 level, 67 patients at the L4/5 level, 16 patients at the L5/S1 level, 34 patient at the L3/4/5 level, and 34 patients at the L4/5/S1 level (Table 1).
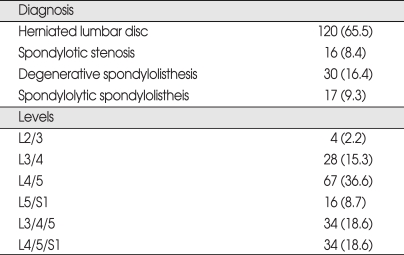
Table 1.
Preoperative diagnoses and levels of the procedures in 183 patients undergoing PLIF
PLIF : posterior lumbar interbody fusion
We found that 213 segments (213/251, 84.9%) of the 251 total segments were fused after a five year follow-up period. The remaining 38 segments (38/251, 15.1%) had not fused (Table 2). We observed posterior bony bridging in all segments which were fused (213/213, 100%) with complete bony bridging in 187 segments (187/213, 87.8%) and incomplete bony bridging in the remaining 26 segments (26/213, 12.2%). We could not discover any newly formed traction spur formation in all segments which were fused (0/213, 0%) (Table 2). We discovered traction spur formation in 20 of the 38 segments which were not fused (20/38, 52.6%). Bony bridging was not observed in three segments (3/38, 7.9%). We could not observe denser and mature bone fusion in six segments (34/38, 89.5%). There was a finding of radiolucent halo in the 22 segments (22/38, 57.9%) (Table 2).
Table 2.
Outcomes of procedures in 251 segments undergoing PLIF
*Bony trabeculae bridging was considered present if it was complete or incomplete. PLIF : posterior lumbar interbody fusion
The Oswestry disability index for the fused group (25% ± 18%) was slightly more favorable than for the non-fused group (34% ± 11%). However, there was no significant difference between these two groups (p > 0.05).
DISCUSSION
When performing a PLIF procedure using a cage, the most important goal for the surgeon is the success of intervertebral fusion. If fusion was not achieved after PLIF procedures, biomechanical stability was not maintained, and restoration of the height of the disc space cannot be achieved, causing continuous pain in patients. Successful intervertebral fusion after a PLIF procedure using a cage is defined as the formation of bony bridging by crossing the intervertebral space and an increase in bone density without a radiolucent gap between the cage and the vertebral body4). McAfee13) emphasized that the existence of bony bridging was the most important parameter for measurement of fusion success. Similarly, our results showed bony bridging in all of fused segments (Fig. 2).
According to Kim et. al.10), approximately 35% of patients who have fusion after a PLIF procedure will have some bony bridging forming around the cage after 12 months. Approximately 82% of these patients will have the bone fusion mass extend to the posterior vertebral cortical margin four years after the procedure. However, for patients who do not experience fusion, the bony mass can only be observed inside the cage. Even after some time, the bony bridging around the cage is not observed at all10). As we confirmed, in all patients with fused segments, bony bridging was observed around the cage. In patients with non-fused segments, there was no bony bridging around the cage. Therefore, the existence of bony bridging around the cage could be considered to be an important parameter for confirmation of fusion after a PLIF procedure.
Traction spur formation is the classic indirect radiographic sign related to spinal instability7,12,16,18). In 1973, Yadab20) reported on the importance of traction spurs, stating that traction spurs constituted the most useful indicators of vertebral segment instability. The proposed mechanism for this instability is that the traction spur is caused by increased tensile stresses exerted by Sharpey's fibers, or by fibers of the anterior longitudinal ligament on the periosteum of the vertebral body, in case of spinal instability11). Increased flexibility between the vertebral bodies leads to homogeneous mechanical stress during the ossification of bone under the cartilage of the vertebral body. Consequently, sclerotic or hyperplastic changes occur on the edge of the vertebral body, leading to the formation of a spur. Macnab12) further emphasized the characteristics of traction spurs and their associations with unstable lumbar disco-vertebral junctions and excessive and abnormal spinal mobility. Pate et al.17), demonstrated radiological and pathological correlations of traction spurs and spinal instability.
In our series, no newly formed traction spurs were seen in any fused segment. New traction spur formation, which was not seen in the pre-operative imaging, was discovered in 52.6% of the non-fused segments (Fig. 3). Therefore, formation of a traction spur after PLIF was used as one of useful parameter to predict non-fusion.
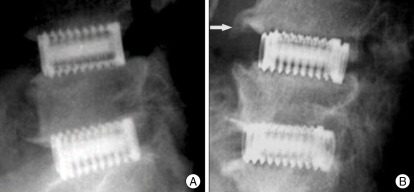
Fig. 3.
Lumbar plain lateral radiograph films showing traction spur formation on non-fused segments at POD of 62 months after posterior lumbar interbody fusion (PLIF) using Ray-threaded fusion cages. A : lumbar plain lateral radiograph films at 1 day after PLIF on the L4/5/S1 segment using Ray-threaded fusion cages. B : Lumbar plain lateral radiograph films showing a growing traction spur on the L4/5 segment (arrow) at 62 months after PLIF using Ray-threaded fusion cages.
There are some limitations that affect the interpretation of our study. First, a single facility performed the PLIF procedures in all patients, using the same surgical technique. However, because all procedures were not performed by a single surgeon, there may be differences in lumbar stability due to different skills of the surgeons or the degrees of laminectomy and facectectomy that were performed. Extensive facetectomy, which is necessary for a posterior interbody cage insertion, markedly destabilizes the spine21). Second, in patients treated with a Ray-TFC cage, metallic radiological artifacts caused by the titanium make it difficult to identify dense, mature bone fusion inside the cage. In these cases, it is difficult to apply Brantigan-Steffee criteria. Third, one of the concerns in interpreting the results of PLIF procedures is the difficulty in determining fusion success radiogaphically. Although, computerized tomography has been suggested as an alternative technique for assessing interbody fusion, it is difficult to apply in a real clinical setting because of medical cost problem. So, we define lumbar interbody fusion in terms of brantigan classification on plain radiograph images. In the PLIF with cages, Brantigan et al.3) reported that comparisons of plain radiographic diagnosis and fusion success at exploration indicated a sensitivity of 97.1%, a positive predictive value of fusion of 94.4%, and an overall accuracy of 93%. Lastly, as Miyakoshi et al.15) reported, patients with severe osteoporosis do not tend to develop traction spurs. Therefore, even when instability exists after PLIF procedures, patients with severe osteoporosis may not develop traction spurs.
Fusion may not occur after PLIF, even if traction spurs do not develop. However, the existence of tractions spur may predict non-fusion. For this reason, follow-up radiography after PLIF procedures should include a fusion criteria classification of 'no traction spur formation' (Table 3).
Table 3.
New radiographic fusion criteria for PLIF
PLIF : posterior lumbar interbody fusion
CONCLUSION
During a minimum five year radiological follow-up period after PLIF procedures using stand alone cage were performed in a large sample of patients, we confirmed that traction spur formation is a useful parameter to confirm non-fusion of vertebral segments. This predictive power exists independently of the Brantigan-Steffee classification. Therefore, a new classification of 'no traction spur formation' should be included in the fusion criteria to confirm non-fusion of vertebral segments after PLIF procedures.
References
- 1.Blumenthal SL, Ohnmeiss DD NASS. Intervertebral cages for degenerative spinal diseases. Spine J. 2003;3:301–309. doi: 10.1016/s1529-9430(03)00004-4. [DOI] [PubMed] [Google Scholar]
- 2.Brantigan JW, Steffee AD. A carbon fiber implant to aid interbody lumbar fusion. Two-year clinical results in the first 26 patients. Spine (Phila Pa 1976) 1993;18:2106–2107. doi: 10.1097/00007632-199310001-00030. [DOI] [PubMed] [Google Scholar]
- 3.Brantigan JW, Steffee AD, Lewis ML, Quinn LM, Persenaire JM. Lumbar interbody fusion using the Brantigan I/F cage for posterior lumbar interbody fusion and the variable pedicle screw placement system : two-year results from a Food and Drug Administration investigational device exemption clinical trial. Spine (Phila Pa 1976) 2000;25:1437–1446. doi: 10.1097/00007632-200006010-00017. [DOI] [PubMed] [Google Scholar]
- 4.Diedrich O, Perlick L, Schmitt O, Kraft CN. Radiographic characteristics on conventional radiographs after posterior lumbar interbody fusion : comparative study between radiotranslucent and radiopaque cages. J Spinal Disord. 2001;14:522–532. doi: 10.1097/00002517-200112000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. discussion 2952. [DOI] [PubMed] [Google Scholar]
- 6.Fraser RD. Interbody, posterior, and combined lumbar fusions. Spine (Phila Pa 1976) 1995;20:167S–177S. doi: 10.1097/00007632-199512151-00016. [DOI] [PubMed] [Google Scholar]
- 7.Frymoyer JW, Selby DK. Segmental instability. Rationale for treatment. Spine. 1985;10:280–286. doi: 10.1097/00007632-198504000-00017. [DOI] [PubMed] [Google Scholar]
- 8.Fuji T, Oda T, Kato Y, Fujita S, Tanaka M. Posterior lumbar interbody fusion using titanium cylindrical threaded cages : is optimal interbody fusion possible without other instrumentation? J Orthop Sci. 2003;8:142–147. doi: 10.1007/s007760300024. [DOI] [PubMed] [Google Scholar]
- 9.Kasai Y, Kawakita E, Sakakibara T, Akeda K, Uchida A. Direction of the formation of anterior lumbar vertebral osteophytes. BMC Musculoskelet Disord. 2009;10:4. doi: 10.1186/1471-2474-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim KS, Yang TK, Lee JC. Radiological changes in the bone fusion site after posterior lumbar interbody fusion using carbon cages impacted with laminar bone chips : follow-up study over more than 4 years. Spine (Phila Pa 1976) 2005;30:655–660. doi: 10.1097/01.brs.0000155421.07796.7f. [DOI] [PubMed] [Google Scholar]
- 11.Leone A, Guglielmi G, Cassar-Pullicino VN, Bonomo L. Lumbar intervertebral instability : a review. Radiology. 2007;245:62–77. doi: 10.1148/radiol.2451051359. [DOI] [PubMed] [Google Scholar]
- 12.Macnab I. The traction spur. An indicator of segmental instability. J Bone Joint Surg Am. 1971;53:663–670. [PubMed] [Google Scholar]
- 13.McAfee PC. Interbody fusion cages in reconstructive operations on the spine. J Bone Joint Surg Am. 1999;81:859–880. doi: 10.2106/00004623-199906000-00014. [DOI] [PubMed] [Google Scholar]
- 14.McAfee PC, Boden SD, Brantigan JW, Fraser RD, Kuslich SD, Oxland TR, et al. Symposium : a critical discrepancy-a criteria of successful arthrodesis following interbody spinal fusions. Spine. 2001;26:320–334. doi: 10.1097/00007632-200102010-00020. [DOI] [PubMed] [Google Scholar]
- 15.Miyakoshi N, Itoi E, Murai H, Wakabayashi I, Ito H, Minato T. Inverse relation between osteoporosis and spondylosis in postmenopausal women as evaluated by bone mineral density and semiquantitative scoring of spinal degeneration. Spine (Phila Pa 1976) 2003;28:492–495. doi: 10.1097/01.BRS.0000048650.39042.58. [DOI] [PubMed] [Google Scholar]
- 16.Nachemson A. Lumbar spine instability. A critical update and symposium summary. Spine (Phila Pa 1976) 1985;10:290–291. [PubMed] [Google Scholar]
- 17.Pate D, Goobar J, Resnick D, Haghighi P, Sartoris DJ, Pathria MN. Traction osteophytes of the lumbar spine : radiographic-pathologic correlation. Radiology. 1988;166:843–846. doi: 10.1148/radiology.166.3.3340781. [DOI] [PubMed] [Google Scholar]
- 18.Pitkänen MT, Manninen HI, Lindgren KA, Sihvonen TA, Airaksinen O, Soimakallio S. Segmental lumbar spine instability at flexion-extension radiography can be predicted by conventional radiography. Clin Radiol. 2002;57:632–639. doi: 10.1053/crad.2001.0899. [DOI] [PubMed] [Google Scholar]
- 19.Weiner BK, Fraser RD. Spine update lumbar interbody cages. Spine (Phila Pa 1976) 1998;23:634–640. doi: 10.1097/00007632-199803010-00020. [DOI] [PubMed] [Google Scholar]
- 20.Yadav SS. Traction spur. J Postgrad Med. 1973;19:136–138. [PubMed] [Google Scholar]
- 21.Zander T, Rohlmann A, Klockner C, Bergmann G. Influence of graded facetectomy and laminectomy on spinal biomechanics. Eur Spine J. 2003;12:427–434. doi: 10.1007/s00586-003-0540-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zdeblick TA, Phillips FM. Interbody cage devices. Spine. 2003;28:S2–S7. doi: 10.1097/01.BRS.0000076841.93570.78. [DOI] [PubMed] [Google Scholar]