Abstract
Purpose
To describe two cases of vitreous metastases of primary cutaneous B-cell lymphoma (PCBCL).
Methods
Observational case series.
Results
A 73-year-old man and an 81-year-old woman, both with a history of PCBCL, diffuse large cell type, presented with decreased visual acuity due to vitritis. Both patients underwent vitreous biopsy that demonstrated B-cell lymphoma, large cell type, and confirmed metastases of cutaneous B-cell lymphoma to the vitreous.
Conclusion
PCBCL, diffuse large cell type, is a rare form of non-Hodgkin lymphoma that can metastasize to the vitreous without visible chorioretinal involvement.
Keywords: primary cutaneous B-cell lymphoma, metastases, vitritis
Introduction
Primary cutaneous lymphomas are non-Hodgkin lymphomas that appear exclusively in the skin at the time of diagnosis. The skin is the most frequent location of extranodal non-Hodgkin lymphoma with an incidence of primary cutaneous lymphoma of 0.7 per 100,000 person-years.1 For comparison, the incidence of non-Hodgkin lymphoma arising primarily in the brain is 0.3 per 100,000 person-years.1
Primary cutaneous lymphomas can be further subdivided into primary cutaneous B-cell lymphomas (PCBCLs) and primary cutaneous T-cell lymphomas (PCTCLs). PCBCLs occur less frequently than PCTCLs and account for only 20–25% of primary cutaneous lymphomas.2 The three main subtypes of PCBCL are marginal zone, follicle center, and diffuse large cell, leg type.2 Of note, PCBCL, diffuse large cell, leg type, can arise in sites other than the legs. The marginal zone type and follicle center type rarely disseminate to extracutaneous sites,2 whereas 43% of patients with diffuse large cell, leg type develop extracutaneous disease with a mean time to extracutaneous spread of 20 months.3 The central nervous system (CNS) is the most common site of visceral dissemination with 27% of extracutaneous metastases occurring in the CNS.3
We present, to our knowledge, the first two patients to be reported in the literature with PCBCL, diffuse large cell type, metastasizing intraocularly.
Case Reports
Case 1
A 73-year-old man presented with 10 days of vision loss in the left eye. The past ocular history was unremarkable. The patient was diagnosed 2 years previously with PCBCL, diffuse large cell type, with lambda light chain restriction, of the skin of the left arm. After initial treatment with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), he developed recurrences in the left arm, right leg, and trunk and was treated with eight cycles of etoposide, methotrexate, lomustine, and prednisone. He was in remission the 5 months before presentation.
The visual acuity measured 20/20 OD, 20/25 OS. Both anterior segments were unremarkable. Biomicroscopy of the anterior vitreous showed 2+ white cells OD and 3+ white cells OS (Figure 1A). The retina and choroid were normal in appearance bilaterally.
FIGURE 1.
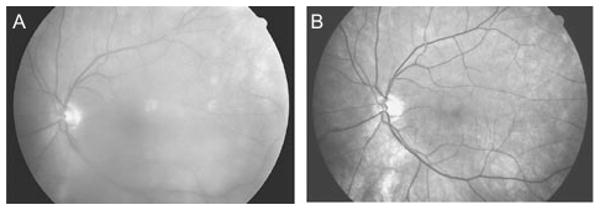
(A) Fundus photograph of left eye at presentation. (B) Fundus photograph of left eye after diagnostic pars plana vitrectomy and completion of radiation treatment.
Immunophenotypic analysis of vitreous obtained at diagnostic vitrectomy revealed lambda light chain restricted B-cell lymphoma, consistent with dissemination of PCBCL to the vitreous. Head computed tomography and cytological examination of the CSF were negative for metastasis.
One month after whole brain and bilateral ocular irradiation, the visual acuity measured 20/20 in each eye, and biomicroscopy disclosed trace vitreous cells OD and no vitreous cells OS (Figure 1B). No retinal or choroidal lesions were present. The patient died of septicemia 2 months later.
Case 2
An 81-year-old woman presented with blurred vision of the right eye for 1 month. Her past ocular history was notable only for bilateral cataract surgery. She had been diagnosed with PCBCL, diffuse large cell type with kappa light chain restriction, of her left lower extremity 5 years before presentation with multiple cutaneous recurrences (Figure 2A). She had undergone three surgical resections along with chemotherapy (including anthracyclines, cyclophosphamide, vincristine, prednisone, fludarabine, mitoxantrone, and rituximab), and radiation, having completed therapy 2 months before presentation.
FIGURE 2.
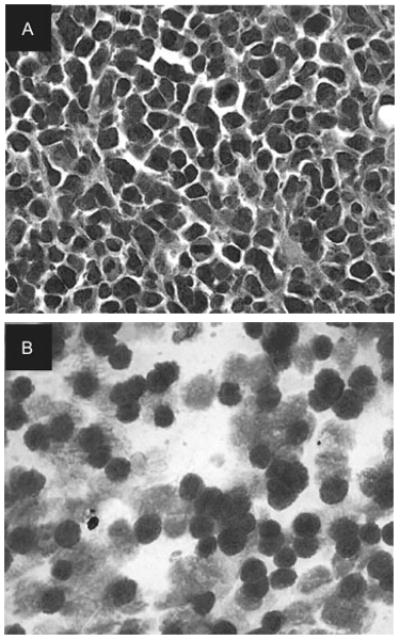
(A) Histopathology of skin biopsy showing anaplastic lymphoid cells with pleomorphic nuclei in mitosis (hematoxylin & eosin stain, 200×). (B) Cytology of vitreous biopsy showing atypical lymphoid cells containing large irregular nuclei, few reactive lymphocytes, and macrophages (Giemsa stain, 400×).
The visual acuity was 20/40 OD, 20/30 OS. Both anterior segments were quiet. Biomicroscopy of the anterior vitreous revealed 4+ cells OD (Figure 3A), but was quiet OS. No retinal or choroidal lesions were visible bilaterally.
FIGURE 3.
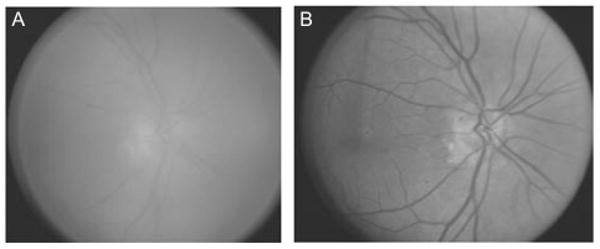
(A) Fundus photograph of right eye at presentation. (B) Fundus photograph of right eye after diagnostic pars plana vitrectomy and completion of radiation treatment.
The patient underwent a vitreous biopsy 9 days after presentation (Figure 2B). Molecular analysis revealed similar monoclonal IgH gene rearrangements in the skin and vitreous, consistent with PCBCL metastases to the vitreous (Figure 4). After vitrectomy, a clear fundus view revealed no chorioretinal lesions.
FIGURE 4.
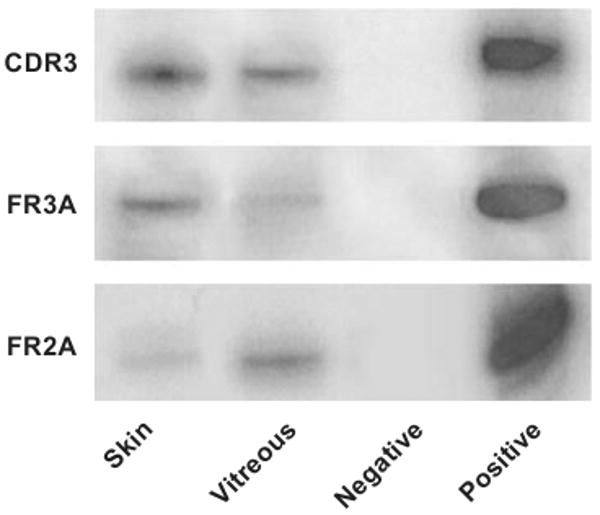
PCR analyses of IgH gene rearrangements. PCR amplification of DNA from microdissected cells of the skin and vitreous specimens are positive using three primers for IgH genes. The PCR products of the skin and vitreous samples are identical.
After right globe irradiation, the visual acuity measured 20/30 in each eye. Biomicroscopy disclosed quiet vitreous without chorioretinal lesions in each eye (Figure 3B). MRI of the brain was unremarkable. The patient died 3 months later from a complicated skin infection.
Comment
Intraocular lymphomas develop in two main forms: (1) arising within the CNS and infiltrating the retina or arising in the retina (i.e., primary CNS lymphoma, PCNSL/primary intraocular lymphoma, PIOL), and (2) originating outside the CNS and metastasizing to the eye, usually the uvea. Traditional thought has been that intraocular PCNSL typically manifests as vitritis and retinal/subretinal infiltrates whereas intraocular lymphomatous metastases more often present in the uvea due to hematogenous spread.4 Interestingly, our cases of PCBCL presented as vitritis, not choroidal infiltrates, mimicking the characteristic presentation of PIOL. Our cases of disseminated PCBCL and several documented cases of disseminated PCTCL5 challenge the assumption that intraocular lymphomatous metastases present with clinically evident choroidal involvement.
These two cases represent the first cases of PCBCL with intraocular metastases described in the literature. PCBCL metastases should be considered in patients presenting with apparent vitritis without clinically obvious retinal or choroidal lesions, especially in patients with a prior diagnosis of PCBCL.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
No financial disclosures or material support was received for the research.
References
- 1.Groves FD, Linet MS, Travis LB, Devesa SS. Cancer surveillance series: non-Hodgkin's lymphoma incidence by histologic subtype in the United States from 1978 through 1995. J Natl Cancer Inst. 2000;92(15):1240–1251. doi: 10.1093/jnci/92.15.1240. [DOI] [PubMed] [Google Scholar]
- 2.Willemze R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005;105(10):3768–3785. doi: 10.1182/blood-2004-09-3502. [DOI] [PubMed] [Google Scholar]
- 3.Grange F, Beylot-Barry M, Courville P, et al. Primary cutaneous diffuse large B-cell lymphoma, leg type: clinicopathologic features and prognostic analysis in 60 cases. Arch Dermatol. 2007;143(9):1144–1150. doi: 10.1001/archderm.143.9.1144. [DOI] [PubMed] [Google Scholar]
- 4.Chan CC, Gonzales JA. Primary Intraocular Lymphoma Singapore. London, Hackensack NJ: World Scientific Publishing Co.; 2007. [Google Scholar]
- 5.Levy-Clarke GA, Greenman D, Sieving PC, et al. Ophthalmic manifestations, cytology, immunohistochemistry, and molecular analysis of intraocular metastatic T-cell lymphoma: report of a case and review of the literature. Surv Ophthalmol. 2008;53(3):285–295. doi: 10.1016/j.survophthal.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]


