Abstract
Background
There is growing evidence that regular attendance at religious functions is associated with less cognitive decline (CD). However, little research has investigated factors that may moderate the religious attendance–CD relationship. The present study examined the effects of gender and depressive symptoms on the relationship between religious attendance and CD.
Methods
Data were drawn from waves 1 and 2 of the Duke Established Populations for Epidemiologic Studies of the Elderly, which were 3 years apart. Participants consisted of a sample of community-dwelling older adults aged 65 years and older (N = 2,938). Linear regression analyses were conducted controlling for important demographic-, socioeconomic-, and health-related variables. Cognitive functioning was assessed at both waves to examine change in errors over time.
Results
Greater religious attendance was related to less CD. In addition, there was a three-way interaction between religious attendance, gender, and depressive symptoms in predicting CD. Among women with higher levels of depressive symptoms, those who less frequently attended religious services experienced greater CD than those who more frequently attended religious services. The interaction between attendance and depressive symptoms in men did not reach significance.
Conclusions
Religious attendance may offer mental stimulation that helps to maintain cognitive functioning in later life, particularly among older depressed women. Given the possible benefits religious attendance may have on cognitive functioning, it may be appropriate in certain instances for clinicians to recommend that clients reengage in religious activities they may have given up as a result of their depression.
Keywords: Religion, Depression, Aged, Cognitive decline
A growing body of literature has documented the salutary effects of religious involvement on various health outcomes. Specifically, compared with individuals who attend religious functions less frequently, individuals who often attend religious services have lower levels of functional disability (1,2), lower prevalence of hypertension (3), and better functional recovery following an acute myocardial infarction (4). The association between religious involvement and lower mortality is robust (5), with weekly attendance at religious services accounting for an additional 2–3 years of life (6). Notable, of all the religious and spiritual measures available (e.g., private religious practice, religious affiliation, spirituality), it is religious attendance that has consistently demonstrated to be the most beneficial to a wide array of health outcomes.
Surprisingly, few studies have investigated the relationship between religious attendance and cognitive decline (CD). Cognitive impairment is an important health outcome affecting many elderly individuals, with the prevalence of dementia climbing from approximately 5% among those in their 70s to 24% for those in their 80s (7). A longitudinal study using data from the New Haven Established Populations for the Epidemiologic Studies of the Elderly (EPESE) Survey found that people who attended religious services once a week or more experienced less CD 3 years later than those who attended less than once a week (8). This effect remained significant after controlling for other forms of social engagement. The authors suggest that religious attendance, as a religious form of social engagement, has a unique influence on cognitive functioning. The effect of regular religious attendance on CD has been replicated in other epidemiological studies using samples of older Mexican Americans (9,10) and older adults from Taiwan (11).
Because research on the association of religious attendance to CD is limited, explanations for possible mechanisms that may account for this relationship are not yet well developed. Social elements of religious activities may promote mental stimulation that protects against CD. Indeed, research has found that social disengagement is a risk factor for CD among elderly individuals (12,13). Stimulating activities have been shown to help build cognitive reserve capacity that delays the manifestation of cognitive difficulties (14). Religious attendance may increase sensory stimulation through activities such as prayer, scripture reading, singing, sermons, philosophical discussions, and socializing.
Another explanation is that engagement in religious activities provides lessons for coping that, in turn, reduce levels of stress, anxiety, and depression. High levels of stress can lead to increased glucocorticoid production, which may damage the hippocampus and affect learning and memory (15).
A third explanation is that religious involvement encourages health-enhancing behaviors and discourages risky behaviors. For example, more frequent religious attendance is strongly associated with greater preventive care use, higher levels of exercise, less alcohol use, and never smoking (2,16).
Hill (17) suggested in a Guest Editorial in the Journal of Gerontology: Medical Sciences that additional research is needed to test whether this association extends to other regions and other racial–ethnic populations because the current research from the United States only applies to specific populations. Hill also stated that previous research has overemphasized main effects, and little is known about potential indirect effects of religious involvement on CD. Moreover, there is a need for adequate control of baseline mental and physical health because the healthiest elderly persons may have self-selected into religious attendance.
The present study attempted to address Hill’s recommendations using data from the Duke EPESE, which consisted of a large biracial sample of community-dwelling adults from the southeastern United States. Cognitive functioning was assessed both at baseline and at follow-up; therefore, we were able to measure change in cognitive functioning over time. We also controlled for variables associated with both religious attendance and CD, including age, health problems, physical functioning, literacy, and education. Importantly, this is one of the first studies to directly control for the potential effects of social support on CD to help determine whether religious attendance influences CD above and beyond general supportive functions. We expected those who more frequently attended religious services to have less CD than less frequent attendees.
Lastly, we examined potential moderators of the relationship between religious attendance and CD, specifically gender and depression. Gender differences have been reported between religious attendance and other important health outcomes such as mortality (5,18), psychological distress (19), disability (1), and depression (20), with the protective effect of religious attendance stronger among women. One explanation for these results is that men and women may express their religious faith differently. For example, women pray more frequently than men (21). Therefore, in our study, we expected religious attendance to have a greater influence on women than on men in reducing CD. Nevertheless, other studies have found no gender differences in the relationship between religious attendance and CD (8,9).
We were also interested in whether depressive symptoms moderated the religious attendance–CD relationship. There is growing evidence to support the link between higher levels of depression and faster CD (22–27). We hypothesized that individuals with higher levels of depressive symptoms, those at greater risk for CD, would experience more benefit cognitively from attending religious services regularly than those with lower levels of depressive symptoms. Indeed, a recent study found that among those with depression, the inverse relationship between church attendance and cognitive functioning was particularly strong (10).
We also examined whether the proposed interaction between depressive symptoms and religious attendance would be influenced by gender. Individuals at highest risk for CD may derive a unique benefit from activities that reduce CD. Given that individuals with higher levels of depressive symptoms are at greater risk for CD as compared with individuals with lower levels of depressive symptoms, and given that religious attendance has been shown to confer greater health benefits to women as compared with men, we hypothesized that the effect of religious attendance on CD would be particularly strong among women with high levels of depressive symptoms. Specifically, more frequent religious attendance would be uniquely beneficial for women with more depressive symptoms than those with fewer depressive symptoms.
METHODS
Participants
Data were drawn from the Duke EPESE, a multicenter epidemiological investigation of the physical, psychological, and social functioning of community-dwelling adults aged 65 years and older. The sample was composed of residents selected from five contiguous counties in North Carolina. The current study focuses on data from wave 1 (n = 4,162, 1986–1987) and wave 2 (n = 3,314, 1989–1990). The sampling design strategy has been reported in detail elsewhere (28). To summarize, data were collected through in-person interviews. Participants were administered a questionnaire that included detailed information about demographics, psychological, physical, social, and cognitive functioning.
Control Variables
We controlled for several variables that have been found to be associated with religious attendance and CD, including demographic variables, education, literacy, income, marital status, depressive symptoms, social support, as well as health and physical functioning variables.
Measures
A comprehensive demographic section documented the age, gender, race, marital status, income, years of education, and literacy of the participants. Participants were asked to select an income category best representing their income during the last year. Categories were 1 (0–1,999), 2 (2,000–2,999), 3 (3,000–3,999), etc. Participants were assigned a yearly income based on the midpoint of each category (e.g., for category 1, the midpoint of income was $999.50). Income was then entered as a variable ranging from $999.50 to $44,499.50. Interviewers also assessed participants’ literacy based on their ability to read several pieces of written information given to them during the first interview (29).
Religious Attendance
To assess religious attendance, participants were asked to indicate how often they go to religious meetings or services. Participants used a 6-point Likert-type scale anchored by “never/almost never” to “more than once a week”. Religious attendance was entered into the present analyses as a continuous variable so as not to lose variability within the item. However, it is important to note that the results remained relatively unchanged when religious attendance was dichotomized at once per week or more and less than once per week, the customary cutoff point used in the previous literature.
Cognitive Functioning
The 10-item Short Portable Mental Status Questionnaire (SPMSQ) (30) was used to measure global cognition at wave 1 (α = .74) and wave 2 (α = .93). Items assessed orientation and knowledge, such as the date, current president, and simple arithmetic. Research has shown good agreement between the SPMSQ and the diagnosis of dementia (31) as well as the Mental Status Questionnaire (32) and other measures of cognitive impairment (33). In contrast to other studies that have dichotomized the SPMSQ, in the current study, participants’ errors were summed across items to form a continuous scale (0–10 errors), with higher scores indicating more difficulty with cognitive functioning.
Social Support
The measure of perceived support was created from the sum of two items. One item asked if in times of trouble respondents could count on at least some family or friends for support. The other item asked if they could talk with at least some family or friends about their deepest problems. Responses on each item ranged from 1 “Hardly ever” to 3 “Most of the time.” The zero-order correlation between the two items (r = .4) is considered acceptable (34).
Measurement of Depressive Symptoms
A modified Center for Epidemiological Studies-Depression scale (CES-D) (35) was administered at wave 1 (Cronbach’s α = .82) (36). For ease of administration, a dichotomous response scale was used for each item, coded: 0 “No,” 1 “Yes.” Responses across the 20 items were summed to create a CES-D scale score (0–20). Higher scores indicate more depressive symptoms.
Physical Functioning
At baseline, three items from the Rosow–Breslau functional health scale (37) were used to assess physical functioning. Items involved unaided ability to do heavy housework, walk up and down stairs, and walk one-half mile (α = .79).
Chronic Health Problems
Physicians provided ratings to indicate the negative impact of various medical conditions (stroke, high blood pressure, cancer, diabetes, and hip fracture) on physical health. When a condition was present, the respondent was given a score equal to the mean physician severity rating for that condition. These scores were then summed across conditions. This measure is an index of the severity of overall health problems.
Data Analytic Strategy
Initial analyses were conducted to describe the demographics of the participants as well as the relevant variables included in the subsequent regression analyses.
First, a linear regression analysis was conducted in which we examined the main effect of religious attendance on CD while controlling for variables associated with cognitive functioning. Next, all the variables used in creating the interaction terms (gender, religious attendance, and depressive symptoms) were centered. We created interaction terms for the two-way interactions of gender and religious attendance, religious attendance and depressive symptoms, and depressive symptoms and gender. We then conducted linear regression analyses for each of the two-way interactions. Finally, a linear regression analysis was conducted to test for the three-way interaction between gender, depressive symptoms, and religious attendance. All the lower order two-way interactions were included in this final analysis to test for the three-way interaction.
RESULTS
Descriptive Statistics
Participants (N = 2,938) who survived to wave 2 were 45.5% white and 33.0% male. The average age of participants at wave 1 was 72.87 years (SD = 6.19). Table 1 provides descriptive statistics for the participants by frequency of religious attendance.
Table 1.
Description of the Study Sample by Religious Attendance Status at Time 1
| Sample as Whole (N = 2,938) | Frequent Attenders* (N = 1,665) | Infrequent Attenders (N = 1,273) | F Statistic or χ2 | p Value | |
| Race | χ2 = 0.084 | .772 | |||
| Black | n = 1,602 (54.5%) | n = 904 (54.3%) | n = 698 (54.8%) | ||
| White | n = 1,336 (45.5%) | n = 761 (45.7%) | n = 575 (45.2%) | ||
| Gender | χ2 = 3.692 | .055 | |||
| Male | n = 971 (33%) | n = 526 (31.6%) | n = 445 (35%) | ||
| Female | n = 1,967 (67%) | n = 1,139 (68.4%) | n = 828 (65%) | ||
| Age | 72.87 (6.19) | 72.7 (5.85) | 73.09 (6.61) | F = 2.875 | .09 |
| Education | 8.63 (4.06) | 9.24 (4.01) | 7.84 (3.98) | F = 88.043 | <.001 |
| Income | 10,631 (10,195) | 11,340 (10,313) | 9,705 (9,966) | F = 18.679 | <.001 |
| Literacy | χ2 = 24.775 | <.001 | |||
| Illiterate | n = 295 (10%) | n = 127 (7.6%) | n = 168 (13.2%) | ||
| Literate | n = 2,643 (90%) | n = 1,538 (92.4%) | n = 1,105 (86.8%) | ||
| Chronicity of health problems | χ2 = 13.47 | .001 | |||
| Low | n = 1,170 (39.8%) | n = 701 (42.1%) | n = 469 (36.8%) | ||
| Medium | n = 806 (27.4%) | n = 463 (27.8%) | n = 343 (26.9%) | ||
| High | n = 962 (32.7%) | n = 501 (30.1%) | n = 461 (36.2%) | ||
| Physical functioning problems | 0.803 (1.07) | 0.598 (0.917) | 1.071 (1.193) | F = 147.57 | <.001 |
| CES-D Time 1 | 3.13 (3.33) | 2.76 (3.09) | 3.61 (3.57) | F = 47.442 | <.001 |
| Marital status | χ2 = 2.188 | .139 | |||
| Married | 1,206 (41%) | 703 (42.2%) | 503 (39.5%) | ||
| Not married | 1,732 (59%) | 962 (57.8%) | 770 (60.5%) | ||
| Social support | 5.49 (0.1) | 5.56 (0.87) | 5.41 (0.96) | F = 18.817 | <.001 |
| SPMSQ Time 1 | 1.56 (1.45) | 1.36 (1.29) | 1.82 (1.59) | F = 74.643 | <.001 |
| SPMSQ Time 2 | 1.8 (2.23) | 1.44 (1.85) | 2.27 (2.58) | F = 105.07 | <.001 |
Notes: CES-D = Center for Epidemiological Studies-Depression scale; SPMSQ = Short Portable Mental Status Questionnaire. Higher scores represent more errors.
Frequent attenders were considered to attend religious services or meetings once per week or more.
Prediction of CD: Linear Regression Analysis
We performed a linear regression analysis with Time 1 religious attendance as the independent variable and Time 2 cognitive errors as the dependent variable, controlling for demographic variables (age, gender, race, and marital status), indices of socioeconomic status (income, literacy, and years of education), physical functioning, chronicity of health problems, Time 1 depressive symptoms, and social support. We also controlled for the number of incorrect responses on the SPMSQ at Time 1, thus removing the variance due to Time 1 cognitive functioning from Time 2 cognitive functioning and allowing for an examination of the effects of each of the other variables in relation to the change in cognitive errors over time (i.e., CD). We found increasing age, African American race, fewer years of education, illiteracy, problems with physical functioning, higher levels of depressive symptoms, and less social support to predict CD. The main effect of religious attendance on CD was significant, F(1,2920) = 11.06, p < .001. As religious attendance increased, CD decreased.
We ran separate linear regression analyses looking at each two-way interaction separately, controlling for all the variables mentioned previously; none of the analyses were significant.
As summarized in Table 2, we conducted a final linear regression analysis in which we entered the three-way interaction between gender, depressive symptoms, and religious attendance. This interaction was significant, F(1,2920) = 8.98, p < .01.
Table 2.
Linear Regression Model: Three-Way Interaction Between Gender, Depressive Symptoms, and Frequency of Religious Attendance in Predicting Cognitive Decline
| Unstandardized Coefficients |
Significance |
95% Confidence Interval |
Correlation |
||||
| B | SE | F | p Value | Lower | Upper | Partial | |
| F(17,2920) = 102.70, p < .001 (constant) | −3.194 | 0.542 | 34.73 | <.001 | −4.26 | −2.13 | |
| SPMSQ Time 1 | 0.61 | 0.03 | 522.58 | <.001 | 0.56 | 0.67 | .39 |
| Age | 0.07 | 0.01 | 149.12 | <.001 | 0.06 | 0.08 | .22 |
| Female gender | −0.12 | 0.08 | 2.06 | .15 | −0.28 | 0.04 | −.03 |
| African American race | 0.24 | 0.07 | 10.53 | .001 | 0.10 | 0.39 | .06 |
| Not married | 0.04 | 0.08 | 0.201 | .65 | −0.12 | 0.20 | .01 |
| Education | −0.03 | 0.01 | 6.79 | .009 | −0.05 | −0.01 | −.05 |
| Illiterate | −0.44 | 0.12 | 13.68 | <.001 | −0.67 | −0.21 | −.07 |
| Income | 0.00 | 0.00 | 1.44 | .23 | 0.00 | 0.00 | −.02 |
| Physical functioning problems | 0.20 | 0.04 | 31.65 | <.001 | 0.13 | 0.27 | .10 |
| Chronicity of health problems | −0.04 | 0.04 | 1.193 | .28 | −0.12 | 0.03 | −.02 |
| CES-D Time 1 | 0.03 | 0.01 | 6.506 | .01 | 0.01 | 0.05 | .05 |
| Social support | −0.08 | 0.04 | 5.10 | .02 | −0.16 | −0.01 | −.05 |
| Religious attendance at Time 1 | −0.07 | 0.02 | 11.06 | .001 | −0.11 | −0.03 | −.06 |
| Interaction of gender and depression | 0.03 | 0.02 | 1.31 | .25 | −0.02 | 0.07 | .02 |
| Interaction of gender and attendance | −0.03 | 0.04 | 0.44 | .51 | −0.11 | 0.06 | −.01 |
| Interaction of depression and attendance | −0.01 | 0.01 | 0.61 | .44 | −0.02 | 0.01 | −.01 |
| Interaction of gender, depression, and attendance | −0.04 | 0.01 | 8.98 | .003 | −0.06 | −0.01 | −.06 |
Note: CES-D = Center for Epidemiological Studies-Depression scale.
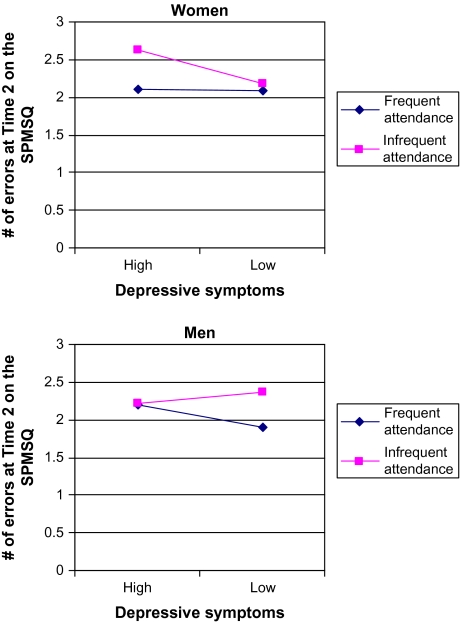
As shown in Figure 1, to interpret this interaction, we assessed the two-way interaction between depressive symptoms and religious attendance separately for women and for men. For men, the two-way interaction between depressive symptoms and religious attendance did not reach statistical significance. However, for women, the two-way interaction between depressive symptoms and religious attendance was significant, B = −0.019, F(1,1953) = 6.67, p = .01. To probe this interaction among women, we assessed the simple effect of religious attendance on CD at 1 SD above and below the mean of the centered CES-D score. For women with high levels of depressive symptoms, less frequent attendance at religious meetings or services was associated with more errors on the SPMSQ over time compared with more frequent attendance, B = −0.156, F(1,1953) = 18.51, p < .001. However, for women with lower levels of depressive symptoms, frequency of attendance of religious meetings or services was unrelated to CD. As illustrated in Figure 1, the effect of infrequent religious attendance on CD was more pronounced among women with higher levels of depressive symptoms than those with lower levels of depressive symptoms. (It is notable that there appeared to be an opposite effect for men such that the effect of religious attendance on CD was more pronounced among men with low levels of depressive symptoms than those with higher levels of depressive symptoms. However, this effect did not reach statistical significance.)
Figure 1.
Three-way interaction between gender, depression, and religious attendance in predicting cognitive decline, after controlling for demographic, socioeconomic, health-status, physical functioning, Time 1 cognitive functioning, and social support variables (Although there appears to be a two-way interaction between depressive symptoms and religious attendance among men, this interaction was not significant.). SPMSQ = Short Portable Mental Status Questionnaire.
DISCUSSION
Attendance of religious services has been shown to be related to several important health outcomes; however, little research to date has examined whether attendance of religious functions and services is related to CD. We found that more frequent religious attendance at Time 1 was related to less CD over a 3-year period even after controlling for demographic, health status, physical functioning, and socioeconomic variables, as well as social support. Although there was neither a significant two-way interaction between gender and religious attendance nor between depressive symptoms and religious attendance, there was a significant three-way interaction between gender, depressive symptoms, and religious attendance. Specifically, the negative impact of infrequent religious attendance on CD was most pronounced among older women with higher levels of depressive symptomatology.
Our study addresses several of the gaps in the current literature outlined by Hill (2008). First, we tested whether the association between religious attendance and CD extended to a biracial sample of community-dwelling older adults from the southeastern United States. Furthermore, we examined the potential indirect effects of religious involvement on CD by testing for interactions with gender and depressive symptoms. We also controlled for baseline mental and physical health to help disentangle the influence of these related variables on CD. In particular, the results obtained here provide evidence against the self-selection hypothesis or that cognitively intact individuals are more likely to attend religious services to begin with because we controlled for baseline cognitive functioning.
Religious attendance and involvement may offer cognitive stimulation that can reduce CD among older adults. Indeed, evidence for the cognitive reserve hypothesis (38) comes from literature that suggests engaging in social and intellectual leisure activities is related to better ability to cope with pathological changes in the brain (39). Engaging in such activities may lead to more efficient cognitive networks that delay the manifestation of cognitive difficulties.
Unlike Reyes-Ortiz and colleagues (2008), we did not find a two-way interaction between depressive symptoms and religious attendance such that more frequent attendance, compared with less frequent attendance, was related to less CD across individuals with varying levels of depressive symptoms. However, we did find that this relationship depended on gender, with the interaction between depressive symptoms and religious attendance present among females only. Perhaps, public religious activities hold different functions for women than for men or women differ from men in their level of involvement when attending religious services. For many women, church services may offer unique networking opportunities, structure and organization, and sense of purpose (19). In fact, there is a strong positive relationship between religious attendance and social contacts (visiting friends, entertaining guests) for women but not for men (40). Furthermore, given that women are more religious than men throughout the life span (41), they may experience greater cognitive benefit from their cumulative lifetime exposure to religious services. These particular functions of religious attendance may take on more meaning when women are depressed than when they are not depressed. For women, religious attendance may be a unique form of behavioral activation and engagement, which may be useful for reducing levels of distress and improving health. Little stimulation through low religious attendance, coupled with higher levels of depressive symptoms, may put some women at greater risk for CD. In addition, some have found that women are more likely than men to use religion as a form of consolation or coping when faced with health problems (42).
Several limitations of this study should be considered. Although religiosity is a multidimensional construct, religious attendance was assessed in our study using a single item. Indeed, Hill (17) states that this is a weakness of the current literature. Furthermore, cognitive functioning was assessed using a relatively brief screening measure. Although some have found the SPMSQ to be a sensitive and specific test for dementia (43), others have reported varying levels of sensitivity and specificity (44). Another limitation of the current study is that we cannot rule out potential third variables that may have been operating and were unaccounted for in the present analyses. People who attend religious services may have better lifestyle habits, such as refraining from drinking or smoking, which may be responsible for this relationship. Furthermore, religious attendance may reflect general level of mental activity (e.g., someone actively involved in a faith community may not only read scripture but may also be more likely to read in general). Lastly, it is possible that people who were experiencing cognitive problems may have disengaged from religious activities at Time 1, thus explaining the observed relationship.
Another important issue to acknowledge is the high rate of attrition between Time 1 and Time 2. People who died between these time points were more likely to be older and male as well as have less education, income, and social support. They were more likely to be illiterate and have physical health problems, higher levels of depressive symptoms, less social support, poorer cognitive functioning, and lower levels of religious attendance. Therefore, selective mortality may have attenuated the results, but the influence is difficult to gauge due to missing data. Thus, the results obtained may not be generalizable to the population as a whole.
Lastly, we examined participants’ current depressive symptoms as a continuous measure, not whether or not participants met criteria for clinical depression. Therefore, we recommend exercising caution in interpreting our results as applying to women who are clinically depressed. Rather, our results indicate that infrequent religious attendance may affect women with higher than average levels of depressive symptoms.
Given the rate of growth of the aging population in the United States and hence the number of individuals with cognitive impairments, it is critical to identify risk factors for CD to help target vulnerable groups. Our findings suggest that religious attendance may serve as a buffer against CD. However, women with higher levels of depressive symptoms who do not attend religious functions may be at greater risk of CD than those who do indeed attend religious services. Given that religious attendance has been shown to be a unique form of social engagement in this and other studies, clinicians may consider assessing religious involvement when asking about their clients’ levels of engagement in social activities. Additionally, it is common for clinicians to encourage depressed clients to resume activities they have disengaged in as part of the treatment for depression (i.e., behavioral activation). For female clients who may have previously enjoyed regularly attending church activities, this research may serve as a form of rationale provision (i.e., that reengagement may not only help with depressive symptoms but also with cognitive functioning in the future) to build client motivation.
FUNDING
National Institute on Aging (5R01-AG20614).
References
- 1.Idler E, Kasl SV. Religion among disabled and nondisabled persons II: attendance at religious services as a predictor of the course of disability. J Gerontol B Psychol Sci Soc Sci. 1997;52B(6):S306–S316. doi: 10.1093/geronb/52b.6.s306. [DOI] [PubMed] [Google Scholar]
- 2.Idler EL, Kasl SV. Religion among disabled and nondisabled persons I: cross-sectional patterns in health practices, social activities, and well-being. J Gerontol B Psychol Sci Soc Sci. 1997;52B(6):S294–S305. doi: 10.1093/geronb/52b.6.s294. [DOI] [PubMed] [Google Scholar]
- 3.Gillum R, Ingram DD. Frequency of attendance at religious services, hypertension, and blood pressure: the Third Health and Nutrition Examination Survey. Psychosom Med. 2006;68:382–385. doi: 10.1097/01.psy.0000221253.90559.dd. [DOI] [PubMed] [Google Scholar]
- 4.Martin KR, Levy BR. Opposing trends of religious attendance and religiosity in predicting elders’ functional recovery after an acute myocardial infarction. J Relig Health. 2006;45(3):440–451. [Google Scholar]
- 5.McCullough ME, Hoyt WT, Larson DB, Koenig HG. Religious involvement and mortality: a meta-analytic review. Health Psychol. 2000;19(3):211–222. doi: 10.1037//0278-6133.19.3.211. [DOI] [PubMed] [Google Scholar]
- 6.Hall DE. Religious attendance: more cost-effective than Lipitor? J Am Board Fam Med. 2006;19:103–109. doi: 10.3122/jabfm.19.2.103. [DOI] [PubMed] [Google Scholar]
- 7.Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: the Aging, Demographics, and Memory Study. Neuroepidemiology. 2007;29:125–132. doi: 10.1159/000109998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Ness PH, Kasl SV. Religion and cognitive dysfunction in an elderly cohort. J Gerontol B Psychol Sci Soc Sci. 2003;58B(1):S21–S29. doi: 10.1093/geronb/58.1.s21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hill TD, Burdette AM, Angel JL, Angel RJ. Religious attendance and cognitive functioning among older Mexican Americans. J Gerontol B Psychol Sci Soc Sci. 2006;61B(1):P3–P9. doi: 10.1093/geronb/61.1.p3. [DOI] [PubMed] [Google Scholar]
- 10.Reyes-Ortiz CA, Berges IM, Raji MA, Koenig HG, Kuo Y, Markides KS. Church attendance mediates the association between depressive symptoms and cognitive functioning among older Mexican Americans. J Gerontol A Biol Sci Med Sci. 2008;63A(5):480–486. doi: 10.1093/gerona/63.5.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yeager DM, Glei DA, Au M, Lin H, Sloan RP, Weinstein M. Religious involvement and health outcomes among older persons in Taiwan. Soc Sci Med. 2006;63:2228–2241. doi: 10.1016/j.socscimed.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 12.Barnes LL, Mendes de Leon CF, Wilson RS, Bienias JL, Evans DA. Social resources and cognitive decline in a population of older African Americans and whites. Neurology. 2004;63:2322–2326. doi: 10.1212/01.wnl.0000147473.04043.b3. [DOI] [PubMed] [Google Scholar]
- 13.Bassuk SS, Glass TA, Berkman LF. Social disengagement and incident cognitive decline in community-dwelling elderly persons. Ann Intern Med. 1999;131(3):165–173. doi: 10.7326/0003-4819-131-3-199908030-00002. [DOI] [PubMed] [Google Scholar]
- 14.Wilson RS, Bennett DA, Bienias JL, et al. Cognitive activity and incident AD in a population-based sample of older persons. Neurology. 2002;59(12):1910–1914. doi: 10.1212/01.wnl.0000036905.59156.a1. [DOI] [PubMed] [Google Scholar]
- 15.Lupien SJ, Fiocco A, Wan N, et al. Stress hormones and human memory function across the lifespan. Psychoneuroendocrinology. 2005;30(3):225. doi: 10.1016/j.psyneuen.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 16.Hill TD, Burdette AM, Ellison CG, Musick MA. Religious attendance and the health behaviors of Texas adults. Prev Med. 2006;42:309–312. doi: 10.1016/j.ypmed.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Hill TD. Religious involvement and healthy cognitive aging: patterns, explanations, and future directions. J Gerontol A Biol Sci Med Sci. 2008;63A(5):478–479. doi: 10.1093/gerona/63.5.478. [DOI] [PubMed] [Google Scholar]
- 18.Strawbridge WJ, Cohen RD, Shema SJ, Kaplan GA. Frequent attendance at religious services and mortality over 28 years. Am J Public Health. 1997;87:957–961. doi: 10.2105/ajph.87.6.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jarvis GE, Kirmayer LJ, Wienfeld M, Lasry J. Religious practice and psychological distress: the importance of gender, ethnicity, and immigrant status. Transcult Psychiatry. 2005;42(4):657–675. doi: 10.1177/1363461505058921. [DOI] [PubMed] [Google Scholar]
- 20.Norton MC, Skoog I, Franklin LM, et al. Gender differences in the association between religious involvement and depression: the Cache County (Utah) Study. J Gerontol B Psychol Sci Soc Sci. 2006;61B(3):P129–P136. doi: 10.1093/geronb/61.3.p129. [DOI] [PubMed] [Google Scholar]
- 21.Levin JS, Taylor RJ. Age differences in patterns and correlates of the frequency of prayer. Gerontologist. 1997;37(1):75–88. doi: 10.1093/geront/37.1.75. [DOI] [PubMed] [Google Scholar]
- 22.Sachs-Ericsson N, Joiner T, Plant AE, Blazer DG. The association of depression to cognitive decline in a community sample of elderly adults. Am J Geriatr Psychiatry. 2005;13:402–408. doi: 10.1176/appi.ajgp.13.5.402. [DOI] [PubMed] [Google Scholar]
- 23.Jorm A. Is depression a risk factor for dementia or cognitive decline? a review. Gerontology. 2000;46(4):219–227. doi: 10.1159/000022163. [DOI] [PubMed] [Google Scholar]
- 24.Green RC, Cupples LA, Kruz A, et al. Depression as a risk factor for Alzheimer disease: the MIRAGE Study. Arch Neurol. 2003;60(5):753–759. doi: 10.1001/archneur.60.5.753. [DOI] [PubMed] [Google Scholar]
- 25.Lopez O, Jagust WJ, DeKosky ST, et al. Prevalence and classification of mild cognitive impairment in the Cardiovascular Health Study Cognition Study: part 1. Arch Neurol. 2003;60(10):1385–1389. doi: 10.1001/archneur.60.10.1385. [DOI] [PubMed] [Google Scholar]
- 26.Zubenko GS, Zubenko WN, McPherson S, et al. A collaborative study of the emergence and clinical features of the major depressive syndrome of Alzheimer's disease. Am J Psychiatry. 2003;160(5):857–866. doi: 10.1176/appi.ajp.160.5.857. [DOI] [PubMed] [Google Scholar]
- 27.Geda Y, Knopman DS, Mrazek DK, et al. Depression, apolipoprotein E genotype, and the incidence of mild cognitive impairment: a prospective cohort study. Arch Neurol. 2006;63:435–440. doi: 10.1001/archneur.63.3.435. [DOI] [PubMed] [Google Scholar]
- 28.Cornoni-Huntley J, Blazer D, Lafferty M, Everett D, Brock D. Established Populations for Epidemiologic Studies of the Elderly: Resource Data Book. Bethesda, MD: National Institute on Aging; 1990. [Google Scholar]
- 29.Sachs-Ericsson N, Blazer DG. Racial differences in cognitive decline in a sample of community-dwelling older adults: the mediating role of education and literacy. Am J Geriatr Psychiatry. 2005;13(11):968–975. doi: 10.1176/appi.ajgp.13.11.968. [DOI] [PubMed] [Google Scholar]
- 30.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 31.Haglund RMJ, Schuckit MA. A clinical comparison of tests of organicity in elderly patients. J Gerontol. 1976;31:654–659. doi: 10.1093/geronj/31.6.654. [DOI] [PubMed] [Google Scholar]
- 32.Hooijer C, Dinkgreve M, Jonker C, Lindeboom J, Kay DWK. Short screening tests for dementia in the elderly population. I. A comparison between the AMTS, MMSE, MSQ, and SPMSQ. Int J Geriatr Psychiatry. 1992;7:559–571. [Google Scholar]
- 33.Wolber G, Romaniuk M, Eastman E, Robinson C. Validity of the Short Portable Mental Status Questionnaire with elderly psychiatric patients. J Consult Clin Psychol. 1984;4:712–713. doi: 10.1037//0022-006x.52.4.712. [DOI] [PubMed] [Google Scholar]
- 34.Briggs S, Cheek JM. The role of factor analysis in the development and evaluation of personality scales. J Pers. 1986;54:106–148. [Google Scholar]
- 35.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 36.Blazer D, Burchett B, Service C, George LK. The association of age and depression among the elderly: an epidemiologic exploration. J Gerontol. 1991;46:M210–M215. doi: 10.1093/geronj/46.6.m210. [DOI] [PubMed] [Google Scholar]
- 37.Rosow I, Breslau NA. Guttman health scale for the aged. J Gerontol. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 38.Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc. 2002;8:443–460. [PubMed] [Google Scholar]
- 39.Scarmeas N, Stern Y. Cognitive reserve and lifestyle. J Clin Exp Neuropsychol. 2003;25(5):625–633. doi: 10.1076/jcen.25.5.625.14576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hintikka J, Koskela K, Kontula O, Viinamaki H. Gender differences in associations between religious attendance and mental health in Finland. J Nerv Ment Dis. 2000;188(11):772–776. doi: 10.1097/00005053-200011000-00008. [DOI] [PubMed] [Google Scholar]
- 41.Levin JS, Taylor RJ, Chatters LM. Race and gender differences in religiosity among older adults: findings from four national surveys. J Gerontol. 1994;49:S137–S145. doi: 10.1093/geronj/49.3.s137. [DOI] [PubMed] [Google Scholar]
- 42.Ferraro KF, Koch JR. Religion and health among black and white adults: examining social support and consolation. J Sci Study Relig. 1994;33(4):362–375. [Google Scholar]
- 43.Erkinjuntti T, Sulkava R, Wikstrom J, Autio L. Short Portable Mental Status Questionnaire as a screening test for dementia and delirium among the elderly. J Am Geriatr Soc. 1987;35:412–416. doi: 10.1111/j.1532-5415.1987.tb04662.x. [DOI] [PubMed] [Google Scholar]
- 44.Albert M, Smith LA, Scherr PA, Taylor JO, Evans DA, Funkenstein HH. Use of brief cognitive tests to identify individuals in the community with clinically diagnosed Alzheimer’s Disease. Int J Neurosci. 1991;57:167–178. doi: 10.3109/00207459109150691. [DOI] [PubMed] [Google Scholar]