Abstract
AIM: To analyze the clinical characteristics of patients diagnosed with Fitz-Hugh-Curtis syndrome.
METHODS: The clinical courses of patients that visited St. Mary’s Hospital with abdominal pain from January 2005 to December 2006 and were diagnosed with Fitz-Hugh-Curtis syndrome were examined.
RESULTS: Fitz-Hugh-Curtis syndrome was identified in 22 female patients of childbearing age; their mean age was 31.0 ± 8.1 years. Fourteen of these cases presented with pain in the upper right abdomen alone or together with pain in the lower abdomen, and six patients presented with pain only in the lower abdomen. The first impression at the time of visit was acute cholecystitis or cholangitis in 10 patients and acute appendicitis or pelvic inflammatory disease in eight patients. Twenty-one patients were diagnosed by abdominal computer tomography (CT), and the results of abdominal sonography were normal for 10 of these patients. Chlamydia trichomatis was isolated from 18 patients. Two patients underwent laparoscopic adhesiotomy and 20 patients were completely cured by antibiotic treatment.
CONCLUSION: For women of childbearing age with acute pain in the upper right abdomen alone or together with pain in the lower abdomen, Fitz-Hugh-Curtis syndrome should be considered during differential diagnosis. Moreover, in cases suspected to be Fitz-Hugh-Curtis syndrome, abdominal CT, rather than abdominal sonography, assists in the diagnosis.
Keywords: Chlamydia trichomatis, Abdominal pain, Fitz-Hugh-Curtis syndrome
INTRODUCTION
Acute abdominal pain is one of the most common symptoms experienced by patients visiting hospitals, particularly the emergency room. Pain in the right upper abdomen is a symptom of biliary diseases, such as gall bladder (GB) stones or cholecystitis, and it may also be present in duodenal ulcers, liver abscess, subphrenic abscess, herpes zoster infection, etc. In addition, pain in the right upper abdomen, alone or together with pain in the lower abdomen, is associated with Fitz-Hugh-Curtis syndrome, although this condition is infrequent among hospital patients.
Fitz-Hugh-Curtis syndrome is characterized by inflammation in perihepatic capsules with concomitant pelvic inflammation without involvement of hepatic parenchyma[1-3]. Most Fitz-Hugh-Curtis syndrome patients are women of childbearing age who visit hospitals because of acute pain and tenderness in the right upper abdomen. The pain in the right upper abdomen is caused by adhesion of the anterior hepatic surface and the abdominal wall[4]. The pain tends to become more severe upon body movement, breathing, etc, and, thus, it is difficult to distinguish it from acute cholecystitis, pleurisy, right pyelonephritis, etc in many cases[5]. Furthermore, in some cases, it presents with pain in the lower abdomen only, without the characteristic pain in the right upper abdomen, and it is thus misdiagnosed as acute appendicitis or some other form of peritonitis[6].
Recently, with the development of imaging tests and antibiotics, Fitz-Hugh-Curtis syndrome has been classified as a benign disease that can be diagnosed and treated readily by non-invasive methods[7], for example, by abdominal computer tomography (CT) scan and oral antibiotics, respectively. Nevertheless, without sufficient understanding of this disease, it could be misdiagnosed as another acute disease with similar clinical symptoms, and thus patients may undergo unnecessary surgery or tests.
Until now, Fitz-Hugh-Curtis syndrome has been considered a gynecological disease; however, the major complaint is pain in the right upper abdomen. Hence, clinicians that focus on the digestive tract frequently encounter such patients during the primary diagnosis. This study analyzed the clinical characteristics of patients diagnosed with Fitz-Hugh-Curtis syndrome at our hospital.
MATERIALS AND METHODS
Patients
This study was performed with 22 patients that visited St. Mary’s Hospital, Catholic University, from January 2005 to December 2006, due to abdominal pain and were diagnosed with Fitz-Hugh-Curtis syndrome. In the study, the diagnostic standard of Fitz-Hugh-Curtis syndrome was the following: (1) abdominal CT scan showed pelvic inflammation with contrast enhancement of hepatic capsules; (2) patients had an adhesion between the liver and the diaphragm or the liver and the anterior abdominal wall detected by laparoscopic surgery. CT images were acquired using multi-detector scanners, Lightspeed VCT (General Electric, Milwaukee, WI, USA). A total of 120 mL of iopromide, Ultravist 300 (Bayer Schering Pharma AG, Berlin, Germany) was administrated at a rate of 3 mL/s with an automatic power injector. Images were obtained before and at 60-70 s after iv contrast material injection. In all phases, scanning was initiated at the dome of the right hemidiaphragm and scans of the entire abdomen to the symphysis pubis were obtained. Slice thickness was 5 mm. To gain a definitive diagnosis of pathogens, we performed PCR tests, used sexually transmitted disease detection kits to detect Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, Ureaplasma urealyticum, Mycoplasma hominis, Mycoplasma genitalium, and performed serological tests, including enzyme immunoassay for Chlamydia IgM and ELISA for Chlamydia IgG.
Study design
We retrospectively reviewed the records of 22 patients who were diagnosed with Fitz-Hugh-Curtis syndrome. Patients’ medical records, disease histories, physical and systemic examinations, and first impression by the clinicians that performed the initial diagnosis were examined. Laboratory tests, blood chemistry, serological tests, direct smears of specimens, and bacterial culture tests were performed. For radiological tests, the results of ultrasound tests and CT were examined. Diagnostic and therapeutic laparoscopic surgery, antibiotic treatments after diagnosis, and prognosis were examined for each patient.
RESULTS
Characteristic of patients
Our study sample included 22 Fitz-Hugh-Curtis syndrome patients diagnosed at our hospital. The patients were all women of childbearing age with a mean age of 31.0 ± 8.1 years (range 19-49 years). Their most recent sexual activity was between 3 d and 1 mo prior to the visit and the frequency of sexual activity was also provided. Except for two patients for whom symptoms were relatively meager and who were thus admitted through outpatient clinics, 20 patients visited the emergency room because of acute abdominal pain. The interval from the development of symptoms to a hospital visit was diverse, ranging from the same day to 2 wk, with an average of 5.8 ± 4.5 d (Table 1).
Table 1.
Clinical manifestation of 22 patients with Fitz-Hugh-Curtis syndrome
| mean ± SD (range) | |
| Age (yr) | 31.0 ± 8.1 (19-49) |
| Last intercostal history (d) | 11.0 ± 10.9 (3-30) |
| Hospital visit duration (d) | 5.8 ± 4.5 (0-14) |
| Number (%) | |
| Chief complaints | |
| RUQ pain | 7 (32) |
| RUQ and lower abdominal pain | 7 (32) |
| Lower abdominal pain | 6 (27) |
| Epigastric pain | 1 (4.5) |
| Fever and lymphadenopathy | 1 (4.5) |
| First impression | |
| Acute cholecystitis | 10 (46) |
| Acute appendicitis | 5 (23) |
| Pelvic inflammatory disease | 3 (13) |
| Peritonitis | 1 (4.5) |
| Hepatitis | 1 (4.5) |
| Gastric ulcer | 2 (9) |
Chief complaint
The chief complaint requiring a visit to the hospital was pain in the right upper abdomen in seven patients (32%), pain in the right upper abdomen and pain in the lower abdomen in seven cases (32%), pain in the lower abdomen in six cases (27%), fever in one case (4.5%), and epigastric pain in one case (4.5%). With the exception of one case, fever was absent in the patients (Table 1).
First impression
After the first impression of the clinicians that examined the patients initially, 10 patients were diagnosed with acute cholecystitis or a GB stone, eight patients were diagnosed with acute appendicitis or pelvic inflammatory disease, and four patients were diagnosed with acute pyelonephritis, acute hepatitis, acute gastritis, or peptic ulcer disease (Table 1).
Test results
Various test methods were used for diagnosis. In 21 patients (95.5%), an abdominal CT scan was performed and Fitz-Hugh-Curtis syndrome was diagnosed according to its characteristics, the finding of contrast enhancement in the hepatic capsules. One of the patients was diagnosed as having Fitz-Hugh-Curtis syndrome by an abdominal CT scan and was treated; however, due to deterioration in her symptoms, laparoscopic surgery was performed and adhesion between the anterior side of the liver and the abdominal wall was confirmed. The remaining patient developed acute peritonitis during pregnancy and was diagnosed by laparoscopic surgery without abdominal CT scan. Among the 21 patients diagnosed by abdominal CT scan, abdominal sonography was performed in 10 of them prior to abdominal CT scan and the results were normal in all cases.
According to blood chemistry tests, the number of leukocytes averaged 11.532/mm3, which was slightly higher than normal. Liver function test results were within the normal range in most patients, with the exception of 1 patient with a result 4 times greater than the upper normal limit. ESR averaged 51.3 mm/h which was elevated five times more than normal (normal value, 0-10 mm/h). C-reactive protein (CRP) averaged 52.3 mg/L, which was over 10 times higher than normal (normal value, less than 5 mg/L). The serological antibody tests to C. trichomatis and PCR tests to six common sexually transmitted disease pathogens indicated the presence of C. trichomatis in 18 patients, T. vaginalis in one patient, U. urealyticum in one patient, and M. hominis in one patient. One patient was diagnosed during emergency surgery and, thus, the serology tests were not performed. Direct specimen smears were all negative. A cell culture test was performed for seven patients (three cases for Streptococcus agalactiae, one case for U. urealyticum, one case for Staphylococcus aureus, one case for Candida albicans, and one case for Escherichia coli) and the findings concurred with the results of the serological chlamydia antibody tests of and PCR tests performed to determine the presence of pathogens (Table 2).
Table 2.
Laboratory and radiographic study of 211 patients with Fitz-Hugh-Curtis syndrome, which was diagnosed by abdominal CT
| mean ± SD (range) | |
| Laboratory study (n = 21) | |
| WBC (1000/mm3) | 11.5 ± 3.4 (3.5-16.2) |
| AST (IU/L) | 22.1 ± 30.1 (10-156) |
| ALT (IU/L) | 17.0 ± 24.8 (5-126) |
| ESR (mm/h) | 51.2 ± 28.9 (18-120) |
| CRP (mg/L) | 52.1 ± 41.9 (2-154) |
| Positive result of number (%) | |
| Serologic test or PCR (n = 21) | |
| C. trichomatis | 18 (85.7) |
| T. vaginalis | 1 (4.8) |
| U. urealyticum | 1 (4.8) |
| M. hominis | 1 (4.8) |
| Microbiologic culture (n = 21) | |
| S. agalactiae | 3 (14.3) |
| U. urealyticum | 1 (4.8) |
| S. aureus | 1 (4.8) |
| C. albicans | 1 (4.8) |
| E. coli | 1 (4.8) |
| Positive result of number (%) | |
| Radiographic study2 | |
| Abdomen CT (n = 21) | 21 (100) |
| Abdomen ultrasonography (n = 10) | 0 (0) |
Among the 22 patients, one was diagnosed by laparoscopic surgery without a study;
Abdominal CT was performed in 21 patients, and only 10 patients among them were investigated by abdominal ultrasonography.
Treatment and progress
Of 22 patients, 20 patients (91%) improved following general or combinatorial antibiotic therapy and conservative care. One patient did not respond to antibiotic therapy; her pain became more severe but her symptoms improved after adhesiotomy by laparoscopic surgery. One patient developed acute peritonitis during pregnancy and, thus, laparoscopic surgery was performed for the purpose of diagnosis and treatment; she improved after adhesiotomy. Doxycycline was administered as a single antibiotic to five patients, and in combination to 14 patients. For those patients that received combination therapy, triple drug therapy consisted of metronidazole and aminoglycoside with ampicillin/sulbactam or cephalosporin and dual drug therapy consisted of an aminoglycoside with ampicillin/sulbactam or metronidazole with cephalosporin. Three patients received 2 drug therapy for 1 wk and their clinical symptoms were improved (Table 3).
Table 3.
Clinical characteristics of 22 patients with Fitz-Hugh-Curtis syndrome
| No. | Age | Symptom (pain) | Duration | Impression | Diagnosis | Treatment | Prog |
| 1 | 39 | Low abdomen | 5 | PID | CT | Doxycycline | |
| 2 | 23 | RUQ | 7 | Cholecystitis | CT | Doxycycline | |
| 3 | 35 | RLQ | 5 | Appendicitis | CT + Sono | Cepha + Amino + Metro | |
| 4 | 19 | Low abdomen | 5 | Appendicitis | CT + Sono | Doxycycline | |
| 5 | 22 | RUQ | 7 | Cholecystitis | CT + Sono | Cepha + Amino + Metro | |
| 6 | 29 | RUQ + low abdomen | 6 | Appendicitis | CT + Sono | Cepha + Metro | |
| 7 | 26 | RUQ | 3 | Cholecystitis | CT | Cepha + Amino + Metro | |
| 8 | 21 | Epigastrium | 3 | Gastric ulcer | CT + Sono | Cepha + Amino + Metro | |
| 9 | 37 | Fever | 10 | Hepatitis | CT | Doxycycline | |
| 10 | 41 | RUQ | 14 | Cholecystitis | CT | Amp + Amino + Metro | |
| 11 | 49 | Low abdomen | 10 | PID | CT | Amp + Amino + Metro | |
| 12 | 33 | RUQ + low abdomen | 0 | Cholecystitis | CT | Doxycycline | |
| 13 | 45 | RUQ | 1 | Cholecystitis | CT + Sono | Cepha + Metro | |
| 14 | 32 | RUQ | 5 | GB stone | CT + Sono | Amp + Amino+ Metro | |
| 15 | 34 | RUQ + low abdomen | 14 | PID | CT + Sono | Cepha + Amino + Metro | Lapa |
| 16 | 27 | RUQ + low abdomen | 2 | GB stone | CT + Sono | Cepha + Amino + Metro | |
| 17 | 31 | Low abdomen | 14 | Pyelonephritis | Amp + Amino | Lapa | |
| 18 | 25 | RUQ + low abdomen | 1 | Cholecystitis | CT | Amp + Amino + Metro | |
| 19 | 38 | RUQ + low abdomen | 1 | Appendicitis | CT + Sono | Amp + Amino + Metro | |
| 20 | 33 | RLQ | 4 | Appendicitis | CT | Amp + Amino + Metro | |
| 21 | 22 | RUQ + low abdomen | 1 | Cholecystitis | CT | Amp + Amino + Metro | |
| 22 | 27 | RUQ pain | 10 | Gastritis | CT | Amp + Amino + Metro |
RUQ: Right upper quadrant abdominal; RLQ: Right lower quadrant abdominal; PID: Pelvic inflammatory disease; GB: Gallbladder; CT: Computed tomography; Sono: Ultrasonography; Cepha: Cephalosporin; Amino: Aminoglycoside; Metro: Metronidazole; Amp: Ampicillin/sulbactam; Prog: Prognosis; Lapa: Laparoscopic adhesiolysis.
DISCUSSION
Fitz-Hugh-Curtis syndrome is characterized by perihepatic inflammation appearing with pelvic inflammation primarily in women of childbearing age. It occurs in 12.0%-13.8% of pelvic inflammation cases[8,9]. In 1930, Curtis[1] reported the violin-string appearance between the anterior hepatic surface and the abdominal wall in gonorrhea patients. Furthermore, in 1934, Fitz-Hugh[2] reported gonococcal peritonitis accompanied by pain in the right upper abdomen. Previously, N. gonorrhoeae was considered to be the major pathogen of this syndrome; however, in 1985, Lopes-Zeno et al[4] showed that C. trachomatis, not N. gonorrhoeae, was the major pathogen. In the past, the definitive diagnosis was made using methods that confirmed adhesion in the vicinity of the liver by laparoscopic surgery or open abdominal surgery. Recently, the disease was diagnosed and experienced infrequently as it was diagnosed by non-invasive methods such as serological tests for specific antibodies to pathogens that induce pelvic inflammation, PCR, and abdominal CT scan.
It has been suggested that the mechanisms of development of Fitz-Hugh-Curtis syndrome include inflammation in hepatic capsules caused by inflammation in the reproductive system through the peritoneal cavity; migration of pathogens from the peritoneal membrane to the liver via blood; migration of pathogens from the peritoneal membrane to the liver through lymph ducts; and a hyperimmune response to C. trichomatis; nonetheless, the precise mechanism has not been elucidated yet[10].
The pain in the right upper abdomen that appears as the main symptom during the acute phase develops as a sudden sharp pain that becomes more severe in response to deep breathing, body movements, coughing, etc, and it develops as a result of congestion of hepatic capsules, spotted hemorrhage, and fibrous exudates. Occasionally, the pain may radiate to the right shoulder. Lower abdominal pain may appear simultaneously with the right upper abdomen pain or intermittently with the abdominal pain. If pain progresses to a chronic state without pain in the lower abdomen, the pain in the right upper abdomen generally appears continuously or may become dull.
In our study, 14 of 22 patients (64%) showed right upper quadrant (RUQ) pain; the typical symptom of Fitz-Hugh-Curtis syndrome. Seven of 14 patients displayed only RUQ pain, and in the other seven patients RUQ pain was accompanied by pain in the lower abdomen. The other eight patients (36%) had no typical RUQ pain symptom but experienced pain in the epigastrium or only in the lower abdomen, or they had fever and other systemic symptoms. Even when there is no pain in the right upper abdomen, which is the characteristic of Fitz-Hugh-Curtis syndrome when it occurs as perihepatic inflammation, the possibility of Fitz-Hugh-Curtis syndrome can not be ruled out completely[11,12]. Though it is not typical, diagnosis of Fitz-Hugh-Curtis syndrome with the major symptom of pain in the lower abdomen with pelvic inflammation or systemic symptoms should be considered. It has been reported that cases in which pain in the upper abdomen develops without pain in the lower abdomen are rare[13,14]; however, in this study, seven patients (32%) developed pain only in the right upper abdomen. This takes place in patients who have recovered from an acute episode of pelvic inflammatory disease without appropriate treatment[10]. These cases have to be cautiously differentiated from diseases for which the major symptom is pain in the right upper abdomen, such as acute cholecystitis. Although our study did not explore this, there are cases that display pain in the left upper abdomen by perisplenitis as the main symptom of Fitz-Hugh-Curtis syndrome. Hence, we think that cases of non-typical symptoms should be fully considered[15].
For the diagnosis of Fitz-Hugh-Curtis syndrome and the earlier findings of laboratory tests, the only method for definite diagnosis used to be assessment of adhesions in the vicinity of the liver by invasive laparoscopic surgery; however, diagnosis has recently been made possible by a non-invasive abdominal CT scan resulting in contrast enhancement in hepatic capsules caused by perihepatic inflammation during the acute phase of Fitz-Hugh-Curtis syndrome[7,16,17]. In this study, 21 cases (95.5%) were diagnosed by abdominal CT scan. Laparoscopic surgery was performed in only two patients for the purpose of diagnosis and treatment. In addition, differential diagnosis of Fitz-Hugh-Curtis syndrome from hepato-biliary diseases was performed for patients presenting with pain in the right upper abdomen by abdominal sonography. In our study, abdominal sonography was performed on 10 patients in the emergency room. All of these patients showed normal findings. Because abdominal sonography observations are mainly concentrated on the GB or liver, which are usually considered major causes of pain in the right upper abdomen, there is a failure to notice pelvic inflammatory disease which can be observed in the pelvic cavity. There may also be discrepancies in the expertise of different sonographers. Although abdominal sonography is of great help as a primary diagnostic tool to prove the causality of pain in the right upper abdomen, there are clear limitations in using only abdominal sonography to diagnose Fitz-Hugh-Curtis syndrome. Therefore, in sexually active women of childbearing age presenting with pain in the right upper abdomen or pain in the right upper abdomen together with pain in the lower abdomen, that have normal liver function test results and for whom Fitz-Hugh-Curtis syndrome is strongly suspected, an abdominal CT scan may diagnose the syndrome more rapidly and accurately. For the identification of causative pathogens, uterine cervical specimens have been used most frequently, although rectal, urinary tract and salivary specimens can be used[10]. To confirm the presence of the major pathogen C. trachomatis, a culture test is widely applied and, more recently, ligase chain reaction (LCR), PCR, and a specific antibody test have been used to identify the pathogen. In our study, PCR and specific antibody tests were performed to identify the pathogen; tests were positive for C. trichomatis in 18 patients (82%), and testing for N. gonorrhoeae, which has been known to be the most prevalent pathogen in the past, was negative. Other pathogens were detected in the remaining three patients and it is thought that pathogens other than C. trichomatis that induce pelvic inflammation could be causative of Fitz-Hugh-Curtis syndrome. Lactobacilli maintain normal vagina flora, but if normal vagina flora is altered, an inflammation is usually induced by G. vaginalis, C. albicans, T. vaginalis, M. hominis, and the cervix becomes inflamed due to C. trichomatis, N. gonorrhoeae, T. vaginalis, and C. albicans. C. trichomatis and N. gonorrhoeae cause pelvic inflammation. Generally, the culture test is the basic test for the identification of causative pathogens; however, in our study, the major causative pathogen C. trichomatis was not identifiable by culture tests. C. trichomatis cannot be identified in general bacterial culture tests as culture tests for C. trichomatis require special media that is not used in general bacterial culture. Therefore, for cases suspected to be Fitz-Hugh-Curtis syndrome, culture tests should be performed using the special media for C. trichomatis to enable accurate diagnosis. Hepatic enzyme values are normal or slightly elevated in Fitz-Hugh-Curtis syndrome, which is of help in differentiating it from hepatitis[18]. In Fitz-Hugh-Curtis syndrome, the liver function test is normal or slightly elevated and the ESR, although still controversial, has been reported to be increased in some cases[19]. Recently, CRP has been reported to be a marker that reflects the clinical course of this disease[20,21]. In most of our cases, the results of liver function tests were normal except for one patient with a result four times greater than the upper normal limit, and leukocyte values were slightly increased. ESR were elevated five times and CRP was elevated over 10 times more than the normal in our study. However, it is difficult to diagnose Fitz-Hugh-Curtis syndrome definitely by serum biochemistry and serological tests; therefore, they are only partially able to aid in the diagnosis of Fitz-Hugh-Curtis syndrome.
Antibiotics against the identified causative bacteria were administered as treatment and, for cases that were unresponsive to antibiotic therapy, surgery was performed to remove the adhesion in the vicinity of the liver. Standardized treatments were not available so antibiotics targeting C. trichomatis, N. gonorrhoeae, gram negative bacilli, and anaerobic bacteria were administered. Oral antibiotics were administered for 2 wk and non-oral antibiotics were administered for 48 h after the improvement of clinical symptoms[22]. It has been reported that treatment reactions in most patients are good. This was the case in our study, with the exception of one case in which laparoscopic surgery was performed following the deterioration of symptoms. Most patients improved following antibiotic treatment. Moreover, the lesions were absent on abdominal CT scan performed after the treatment (Figure 1).
Figure 1.
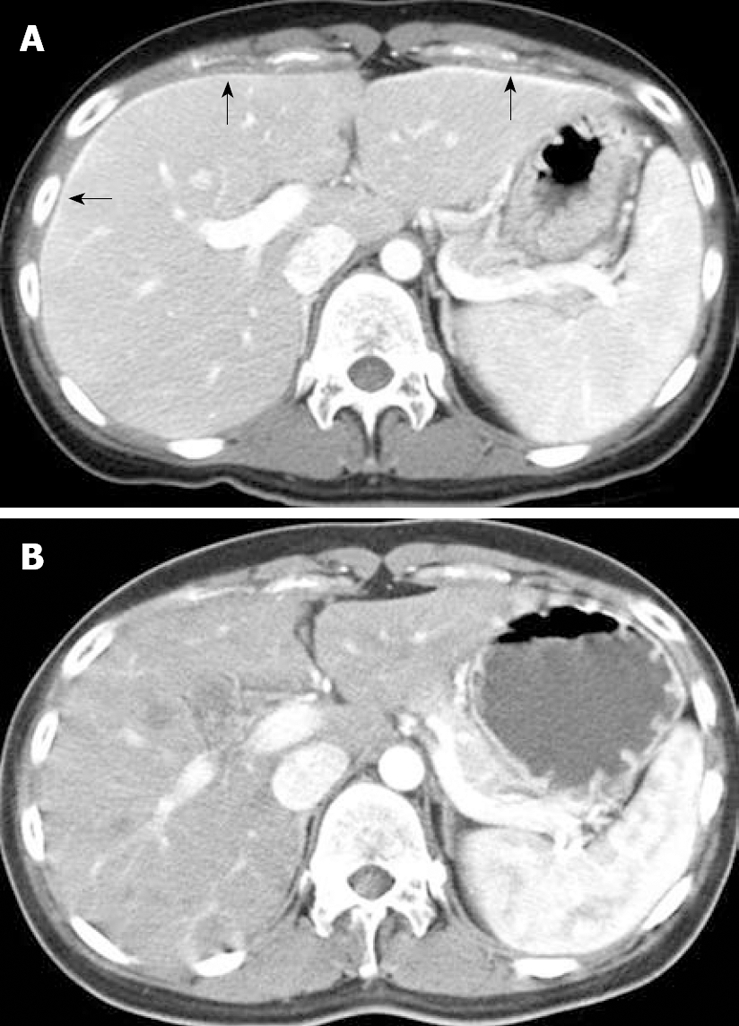
Contrast-enhanced CT. A: Linear enhancement of the surface at both lobes of the liver (arrow); B: CT images 1 mo after treatment indicate normal liver.
The diagnosis rate of Fitz-Hugh-Curtis syndrome has increased due to the recent development of imaging tests. Most patients recover completely after treatment with appropriate antibiotics. Nevertheless, this syndrome is often misdiagnosed as other diseases with similar clinical symptoms which results in unnecessary treatment and hospital stays. Therefore, if sexually active women visit a hospital because of pain in the right upper abdomen or pain in the right upper abdomen and pain in the lower abdomen, Fitz-Hugh-Curtis syndrome should be considered. For patients suspected to have Fitz-Hugh-Curtis syndrome, an abdominal CT scan, rather than abdominal sonography, may be helpful since it provides a more rapid and accurate diagnosis.
COMMENTS
Background
Fitz-Hugh-Curtis syndrome has been considered a gynecological disease; however, the major complaint is pain in the right upper abdomen. Hence, clinicians that focus on the digestive tract frequently encounter such patients during primary diagnosis.
Research frontiers
Fitz-Hugh-Curtis syndrome has been classified as a benign disease. Nevertheless, without sufficient understanding of this disease, it may be misdiagnosed as other acute diseases with similar clinical symptoms. This study analyzed the clinical characteristics of patients diagnosed with Fitz-Hugh-Curtis syndrome.
Innovations and breakthroughs
Abdominal sonography is of great help as a primary diagnostic tool to prove the causality of pain in the right upper abdomen. However, there is a clear limitation to diagnosis of Fitz-Hugh-Curtis syndrome by using only abdominal sonography. Because the observations are mainly concentrated on the hepato-biliary disease, there is a failure to notice pelvic inflammatory disease. For patients suspected to have Fitz-Hugh-Curtis syndrome, an abdominal CT scan, rather than abdominal sonography, may be helpful.
Applications
The results show that in sexually active women of childbearing age presenting with pain in the right upper abdomen or pain in the right upper abdomen together with pain in the lower abdomen and normal liver function test results, Fitz-Hugh-Curtis syndrome should be considered during differential diagnosis.
Terminology
Fitz-Hugh-Curtis syndrome is characterized by inflammation in perihepatic capsules with concomitant pelvic inflammation. Most Fitz-Hugh-Curtis syndrome patients visit hospitals due to acute pain and tenderness in the right upper abdomen. The diagnosis is made by a non-invasive abdominal CT scan resulting in contrast enhancement in hepatic capsules caused by perihepatic inflammation. The treatment is antibiotic therapy against the identified causative bacteria.
Peer review
This is an interesting study which was well organized. It demonstrated that although Fitz-Hugh-Curtis syndrome is a benign disease that can be diagnosed by non-invasive methods and treated by antibiotics, it is often misdiagnosed as other acute diseases which results in unnecessary treatment and hospital stays.
Acknowledgments
We acknowledge the help of Ka Young Kim from Korean Minjok Leadership Academy, who provided great support to data analysis and excellent secretarial assistance.
Footnotes
Supported by The Catholic University of Korea
Peer reviewer: William Dickey, Altnagelvin Hospital, Londonderry, Northern Ireland BT47 6SB, United Kingdom
S- Editor Li DL L- Editor O'Neill M E- Editor Lin YP
References
- 1.Curtis AH. A cause of adhesions in the right upper quadrant. JAMA. 1930;94:1221–1222. [Google Scholar]
- 2.Fitz-Hugh T Jr. Acute gonococcic peritonitis of the right upper quadrant in women. JAMA. 1934;102:2094–2096. [Google Scholar]
- 3.Hyun JJ, Kim JY, Bak YT, Lee CH, Choi SY. Education and imaging. Gastrointestinal: Fitz-Hugh-Curtis syndrome. J Gastroenterol Hepatol. 2006;21:1493. doi: 10.1111/j.1440-1746.2006.04632.x. [DOI] [PubMed] [Google Scholar]
- 4.Lopez-Zeno JA, Keith LG, Berger GS. The Fitz-Hugh-Curtis syndrome revisited. Changing perspectives after half a century. J Reprod Med. 1985;30:567–582. [PubMed] [Google Scholar]
- 5.Wood JJ, Bolton JP, Cannon SR, Allan A, O'Connor BH, Darougar S. Biliary-type pain as a manifestation of genital tract infection: the Curtis-Fitz-Hugh syndrome. Br J Surg. 1982;69:251–253. doi: 10.1002/bjs.1800690507. [DOI] [PubMed] [Google Scholar]
- 6.Shanahan D, Gau D. Chlamydial Fitz-Hugh/Curtis syndrome. Lancet. 1986;1:1216. doi: 10.1016/s0140-6736(86)91199-2. [DOI] [PubMed] [Google Scholar]
- 7.Nishie A, Yoshimitsu K, Irie H, Yoshitake T, Aibe H, Tajima T, Shinozaki K, Nakayama T, Kakihara D, Matsuura T, et al. Fitz-Hugh-Curtis syndrome. Radiologic manifestation. J Comput Assist Tomogr. 2003;27:786–791. doi: 10.1097/00004728-200309000-00017. [DOI] [PubMed] [Google Scholar]
- 8.Semchyshyn S. Fitz-Hugh and Curtis syndrome. J Reprod Med. 1979;22:45–48. [PubMed] [Google Scholar]
- 9.Onsrud M. Perihepatitis in pelvic inflammatory disease--association with intrauterine contraception. Acta Obstet Gynecol Scand. 1980;59:69–71. doi: 10.3109/00016348009160085. [DOI] [PubMed] [Google Scholar]
- 10.Peter NG, Clark LR, Jaeger JR. Fitz-Hugh-Curtis syndrome: a diagnosis to consider in women with right upper quadrant pain. Cleve Clin J Med. 2004;71:233–239. doi: 10.3949/ccjm.71.3.233. [DOI] [PubMed] [Google Scholar]
- 11.Ricci P, Lema R, Sola V, Fernandez C, Fabres C, Fernandez E, Pardo J. Fitz-Hugh-Curtis syndrome: Three cases of incidental diagnosis during laparoscopy. J Obstet Gynaecol. 2008;28:352–354. doi: 10.1080/01443610802058411. [DOI] [PubMed] [Google Scholar]
- 12.Counselman FL. An unusual presentation of Fitz-Hugh-Curtis syndrome. J Emerg Med. 1994;12:167–170. doi: 10.1016/0736-4679(94)90694-7. [DOI] [PubMed] [Google Scholar]
- 13.Muller-Schoop JW, Wang SP, Munzinger J, Schlapfer HU, Knoblauch M, Tammann RW. Chlamydia trachomatis as possible cause of peritonitis and perihepatitis in young women. Br Med J. 1978;1:1022–1024. doi: 10.1136/bmj.1.6119.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katzman DK, Friedman IM, McDonald CA, Litt IF. Chlamydia trachomatis Fitz-Hugh-Curtis syndrome without salpingitis in female adolescents. Am J Dis Child. 1988;142:996–998. doi: 10.1001/archpedi.1988.02150090094033. [DOI] [PubMed] [Google Scholar]
- 15.Gatt D, Jantet G. Perisplenitis and perinephritis in the Curtis-Fitz-Hugh syndrome. Br J Surg. 1987;74:110–112. doi: 10.1002/bjs.1800740213. [DOI] [PubMed] [Google Scholar]
- 16.Cho HJ, Kim HK, Suh JH, Lee GJ, Shim JC, Kim YH. Fitz-Hugh-Curtis syndrome: CT findings of three cases. Emerg Radiol. 2008;15:43–46. doi: 10.1007/s10140-007-0635-8. [DOI] [PubMed] [Google Scholar]
- 17.Nozu T, Komiyama H. Fitz-Hugh-Curtis syndrome. Intern Med. 2006;45:221–222. doi: 10.2169/internalmedicine.45.1645. [DOI] [PubMed] [Google Scholar]
- 18.Litt IF, Cohen MI. Perihepatitis associated with salpingitis in adolescents. JAMA. 1978;240:1253–1254. [PubMed] [Google Scholar]
- 19.Keane JA, McKimm RJ, David CM. Perihepatitis associated with pelvic infection: the Fitz-Hugh-Curtis syndrome. N Z Med J. 1982;95:725–728. [PubMed] [Google Scholar]
- 20.Lim SC, Park YW, Choi HJ, Kim YH. Clinical experiences of Fitz-Hugh-Curtis syndrome. Korean J Obstet Gynecol. 2006;49:1738–1744. [Google Scholar]
- 21.Chung HJ, Choi HY, Cho YJ, Han KH, Kim YD, Jung SM, Kim JU, Cheon GJ. [Ten cases of Fitz-Hugh-Curtis syndrome] Korean J Gastroenterol. 2007;50:328–333. [PubMed] [Google Scholar]
- 22.McCormack WM. Pelvic inflammatory disease. N Engl J Med. 1994;330:115–119. doi: 10.1056/NEJM199401133300207. [DOI] [PubMed] [Google Scholar]


