Abstract
Adenosquamous carcinoma is rare, accounting for 3%-4% of all pancreatic carcinoma cases. These tumors are characterized by the presence of variable proportions of mucin-producing glandular elements and squamous components, the latter of which should account for at least 30% of the tumor tissue. Recently, several reports have described cases of adenosquamous carcinoma of the pancreas. However, as the number of patients who undergo resection at a single institute is limited, large studies describing the clinicopathological features, therapeutic management, and surgical outcome for adenosquamous carcinoma of the pancreas are lacking. We performed a literature review of English articles retrieved from Medline using the keywords ‘pancreas’ and ‘adenosquamous carcinoma’. Additional articles were obtained from references within the papers identified by the Medline search. Our subsequent review of the literature revealed that optimal adjuvant chemotherapy and/or radiotherapy regimens for adenosquamous carcinoma of the pancreas have not been established, and that curative surgical resection offers the only chance for long-term survival. Unfortunately, the prognosis of the 39 patients who underwent pancreatic resection for adenosquamous carcinoma was very poor, with a 3-year overall survival rate of 14.0% and a median survival time of 6.8 mo. Since the postoperative prognosis of adenosquamous carcinoma of the pancreas is currently worse than that of pancreatic adenocarcinoma, new adjuvant chemotherapies and/or radiation techniques should be investigated as they may prove indispensible to the improvement of surgical outcomes.
Keywords: Adenosquamous carcinoma of the pancreas, Pancreatectomy, Surgical outcome, Survival after pancreatic resection
INTRODUCTION
The majority of malignant tumors in the pancreas are adenocarcinomas. Adenosquamous carcinoma of the pancreas occurs less frequently with an incidence of 3%-4%[1]. These tumors are a malignant epithelial carcinoma of the pancreas and are characterized by the presence of variable proportions of both glandular and squamous components. At least 30% of the neoplasm should be comprised of the squamous component[1,2]. Recently, several reports have described cases of adenosquamous carcinoma of the pancreas[3-6]. However, as the number of patients who undergo resection at a single institute is limited, large studies describing the clinicopathological features, therapeutic management and surgical outcome for adenosquamous carcinoma of the pancreas are lacking.
To the best of our knowledge, our survey of the English literature reporting on adenosquamous carcinoma of the pancreas, which was found on Medline, revealed that only 39 intent-to-cure surgical resections had been performed and had clearly presented data (Table 1)[7-28]. The purpose of this study was to clarify the surgical outcome including survival rates after surgery, and to determine the prognostic factors of adenosquamous carcinoma of the pancreas by conducting a retrospective analysis of the 39 patients.
Table 1.
Clinical and pathological data for the 39 cases that underwent surgical resection for adenosquamous carcinoma of the pancreas
| Author | Ref | Yr | Age | Sex | Location | Surgery | Size (cm) | Cx | RT | Rec site | Survival |
| Ishikawa | 7 | 1980 | 67 | M | Body | DP | 10.0 | - | - | Widespread metastasis | 4 mo |
| 53 | F | Head | PD | 4.2 | - | - | 2 d | ||||
| 61 | M | Head | PD | 4.5 | - | - | 12 mo | ||||
| Wilczynski | 8 | 1984 | 68 | M | Head, body | PD | 4.5 | - | - | 20 d | |
| Yamaguchi | 9 | 1991 | 60 | M | Head | PD | ND | - | - | ND | 3 mo |
| 52 | F | Head | PD | ND | - | - | ND | 7 mo | |||
| 44 | F | Head | PD | ND | - | - | ND | 5 mo | |||
| 56 | F | Head | PD | ND | - | - | ND | 4 mo | |||
| 56 | M | Head | PD | ND | - | - | ND | 5 mo1 | |||
| 68 | F | Head | PD | ND | - | - | ND | 5 mo1 | |||
| 49 | F | Body | DP | ND | - | - | ND | 5 mo | |||
| 61 | M | Tail | DP | ND | - | - | ND | 14 mo1 | |||
| Motojima | 10 | 1992 | 52 | M | Body, tail | DP | 7.0 | ND | ND | Systemic metastasis | 3 mo |
| 75 | M | Head | PD | 3.0 | ND | ND | Liver | 10 mo | |||
| 75 | F | Head | PD | 6.0 | ND | ND | Liver | 8 mo | |||
| Tanaka | 11 | 1994 | 48 | F | Head | PD | 4.2 | + | - | ND | 7 mo |
| Makiyama | 12 | 1995 | 58 | M | Head | PD | 5.0 | - | - | Peritoneum | 18 mo |
| Onoda | 13 | 1995 | 64 | M | Body, tail | DP | 7.0 | + | - | Liver, peritoneum | 3 mo |
| Campman | 14 | 1997 | 65 | F | Body, tail | DP | 7.5 | ND | ND | ND | ND |
| Kuji | 15 | 1997 | 73 | M | Body, tail | TP | 6.0 | - | - | ND | 2 mo |
| Nabae | 16 | 1998 | 60 | M | Body | DP | 6.0 | - | IOR | ND | 4 mo |
| 73 | M | Head | PD | ND | - | - | Liver | 10 mo | |||
| Myung | 17 | 1998 | 64 | M | Head | PD | 3.5 | - | - | ND | 4 mo1 |
| Lozano | 18 | 1998 | 75 | M | Head, body | PD | 4.5 | + | + | ND | ND1 |
| 42 | M | Head | PD | 3.5 | + | + | ND | ND1 | |||
| Aranha | 19 | 1999 | 52 | M | Head | PD | 3.2 | + | + | Systemic metastasis | 13 mo |
| 62 | M | Head | PD | 3.0 | + | + | Systemic metastasis | 14 mo | |||
| Komatsuda | 20 | 2000 | 67 | M | Body | DP | 5.0 | - | - | Peritoneum | 6 mo |
| Yavus | 21 | 2000 | 51 | M | Head | PD | 4.0 | ND | ND | - | 36 mo1 |
| 48 | M | Head | PD | 2.0 | ND | ND | ND | ND | |||
| Yamaue | 22 | 2001 | 63 | F | Head | PD | 4.5 | + | + | - | 40 mo1 |
| Kardon | 23 | 2001 | ND | ND | Head | PD | ND | - | - | ND | 33 mo1 |
| Murakami | 24 | 2003 | 41 | M | Head | PD | 3.0 | - | + | Peritoneum | 5 mo |
| Rahemtullah | 25 | 2003 | ND | ND | Head | PD | ND | ND | ND | ND | 13 mo1 |
| ND | ND | Head | PD | ND | ND | ND | ND | ND | |||
| Alwaheeb | 26 | 2005 | 45 | M | Head | PD | 6.0 | - | - | ND | ND |
| Hsu | 27 | 2005 | 66 | M | Head | PD | 3.5 | - | - | ND | 2.5 mo |
| 38 | F | Head | PD | 3.8 | - | + | ND | 6.8 mo | |||
| Jamali | 28 | 2007 | 75 | M | Head | PD | 3.0 | + | - | Liver | 6 mo |
Cx: Chemotherapy; RT: Radiotherapy; Rec site: Recurrence site; ND: Not described; PD: Pancreaticoduodenectomy; DP: Distal pancreatectomy; TP: Total pancreatectomy.
Surviving patients.
PATIENTS
Our survey of the literature from 1980 to the end of 2007 revealed that 45 patients underwent surgical resection for adenosquamous carcinoma of the pancreas[7-28]. Of these, six patients were excluded due to a lack of clear data. The remaining 39 patients were analyzed in this study (Table 1) and included 25 men, 11 women, and three patients of unknown sex with a mean age of 59.0 years (range, 38-75 years). The prognosis outcome of each case was obtained from the published data. The clinicopathological data associated with the pancreatic adenosquamous carcinomas described in these case reports were evaluated, and included tumor location, type of operation, tumor size, whether chemotherapy and radiotherapy had been administered, recurrence sites, and survival times. All of the patients had undergone surgery involving an attempted curative resection. Survival rates were generated using the Kaplan-Meier method and compared using the log-rank test[29]. Values were expressed appropriately as the mean ± SD. Differences in proportions were evaluated by the Pearson chi-square test. A value of P < 0.05 was considered to be statistically significant.
DIAGNOSIS OF ADENOSQUAMOUS CARCINOMA OF THE PANCREAS
Table 1 lists 39 patients who had undergone surgical resection for adenosquamous carcinoma of the pancreas. Adenosquamous carcinomas have not been associated with any specific clinical syndromes[2,30]. Each of the 39 patients presented clinical symptoms such as abdominal pain, back pain, painless jaundice, anorexia, and/or body weight loss (data not shown). Accurate preoperative diagnosis of adenosquamous carcinoma of the pancreas is very difficult, because imaging studies have revealed no characteristic features that can facilitate the differentiation of this tumor type from ordinary invasive ductal carcinoma. One study reported that intense Gallium-67 citrate uptake was observed in adenosquamous carcinoma of the pancreas, indicating that Gallium-67 citrate scintigraphy might be useful in detecting these carcinomas[15]. However, more detailed imaging data are required to improve the ability to diagnose this rare disease.
Adenosquamous carcinoma of the pancreas appears to be larger than ordinary pancreatic adenocarcinoma. The tumors in the 27 cases for which the relevant data was available had a mean size of 4.8 ± 1.8 cm (range, 2-10 cm; Table 1). Preoperative cytological or pathological diagnosis of adenosquamous carcinoma of the pancreas is reportedly rare[12,16-18,21,24,26,30]. However, the two malignant cellular components of adenosquamous carcinoma can be recognized in aspirated smears[17,18,24]. A careful search for glandular differentiation is warranted when the squamous component predominates, particularly if squamous carcinoma specimens only are obtained by biopsy or fine needle aspiration biopsy[12,16]. Adenosquamous carcinoma of the pancreas has no specific radiological findings or serum data, including tumor markers such as carcinoembryonic antigen, carbohydrate antigen 19-9, or squamous cell carcinoma antigen[12,22]. Physicians should try to remember to consider adenosquamous carcinoma of the pancreas in the differential diagnosis of ordinary pancreatic adenocarcinoma, especially if the patient has severe abdominal symptoms and/or a large tumor size[2,30]. Recently, preoperative and intraoperative cytological examinations have been diagnostically correct, however these findings did not alter treatment decisions or survival[30].
MANAGEMENT FOR RESECTABLE ADENOSQUAMOUS CARCINOMA OF THE PANCREAS
Since adenosquamous carcinomas are uncommon tumors with a poor prognosis, the outcomes associated with various therapeutic interventions are not well defined.
Table 1 lists the tumor location and operative method used in the 39 cases analyzed here. Three main operative methods were performed: pancreaticoduodenectomy (PD) including pylorus-preserving PD (PPPD) in 30 cases (76.9%); distal pancreatectomy (DP) in eight cases (20.5%); and total pancreatectomy (TP) in one case (2.6%). Tumors were located in the head alone in 28 cases (76.9%), in the head and body in two cases, and in the body and/or tail of the pancreas in nine cases (23.1%). Although adenosquamous carcinoma of the pancreas has different clinicopathological features to pancreatic adenocarcinoma, the treatment strategy of patients with adenosquamous carcinoma is dealt with in the same manner as patients with adenocarcinoma. Surgical treatment remains the only curative management option that is seriously considered for adenosquamous carcinoma of the pancreas.
To date, only eight patients have received adjuvant chemotherapy, indicating that postoperative adjuvant chemotherapy is not usually administered to patients with adenosquamous carcinoma of the pancreas (Table 1). Tanaka et al reported that the size of an unresectable adenosquamous carcinoma of the pancreas was reduced by neo-adjuvant chemotherapy consisting of a combination of interferon-α, tumor necrosis factor-α, and 5-fluorouracil[11]. However, the patient only survived 7 mo after surgery[11]. In this case, although neo-adjuvant chemotherapy might not have contributed to prolonging the patient’s survival, the ability of the chemotherapy to reduce the size of the tumor from one that was unresectable to one that could be resected was confirmed. In the current study, the adjuvant chemotherapy group had a 2- or 3-year cumulative survival rate of 16.7% and a median survival period of 7 mo (Table 2). In comparison, the group who did not receive adjuvant chemotherapy had a 2-year cumulative survival rate of 9.2% and a median survival period of 5 mo (P = 0.364). Almost all of the patients in the adjuvant chemotherapy group were treated with a 5-fluorouracil-based regimen. Recently, adjuvant chemotherapy using new drug agents has been considered as the standard therapeutic option following resection for pancreatic adenocarcinoma, and several reports suggest that adjuvant chemotherapy with gemcitabine is responsible for a significant increase in patient survival[31-33]. Postoperative administration of gemcitabine also significantly delayed the development of recurrent disease after complete resection of pancreatic cancer compared with observation alone[34]. However, information regarding gemcitabine use in cases with adenosquamous carcinoma of the pancreas is not available as previous reports lack such data. Further investigations examining whether adjuvant chemotherapy using gemcitabine will improve surgical outcome in patients with adenosquamous carcinoma of the pancreas are therefore warranted.
Table 2.
Clinical characteristics after surgical resection for adenosquamous carcinoma of the pancreas
| Characteristics | No. of patients |
Survival rate (%) |
Median survival in months (range) | P value | ||
| 1 yr | 2 yr | 3 yr | ||||
| Overall | 39 | 25.5 | 14.0 | 14.0 | 6.8 (4.6-9.0) | |
| Age (yr) | ||||||
| < 60 | 16 | 26.9 | 9.0 | 9.0 | 6.8 (4.4-9.2) | 0.975 |
| > 60 | 20 | 20.4 | 13.6 | 13.6 | 6.0 (1.3-10.7) | |
| Gender | ||||||
| Male | 25 | 28.4 | 8.5 | 8.5 | 6.0 (1.1-10.9) | 0.842 |
| Female | 11 | 12.0 | 12.0 | 12.0 | 6.8 (5.0-8.6) | |
| Tumor location | ||||||
| Head | 30 | 34.8 | 17.9 | 17.9 | 8.0 (5.3-10.7) | 0.017 |
| Body or tail | 9 | 11.1 | - | - | 4.0 (2.6-5.4) | |
| Operation type | ||||||
| PD | 30 | 33.4 | 17.2 | 17.2 | 8.0 (5.2-10.8) | 0.063 |
| DP or TP | 9 | 12.5 | - | - | 4.0 (2.7-5.3) | |
| LN metastasis | ||||||
| Present | 14 | 20.0 | - | - | 5.0 (2.0-8.0) | 0.134 |
| Absent | 8 | 50.0 | 50.0 | 50.0 | 5 | |
| Chemotherapy | ||||||
| Yes | 8 | 50.0 | 16.7 | 16.7 | 7.0 (0.0-15.4) | 0.364 |
| No | 23 | 18.4 | 9.2 | - | 5.0 (3.0-7.0) | |
| Radiotherapy | ||||||
| Yes | 7 | 60.0 | 20.0 | 20.0 | 13.0 (0.0-26.3) | 0.284 |
| No | 23 | 18.0 | 9.0 | - | 6.0 (4.0-8.0) | |
PD: Pancreaticoduodenectomy; DP: Distal pancreatectomy; TP: Total pancreatectomy; LN metastasis: Lymph node metastasis.
There are no published prospective randomized controlled trials investigating radiotherapy treatment of pancreatic adenosquamous carcinoma following curative resection, only retrospective studies. Limitations of the present study include the errors and biases inherent in a small retrospective study design. Two retrospective studies investigating the benefit of radiotherapy following curative resection for pancreatic carcinoma showed no significant difference in the overall survival between patients who were or were not treated with radiotherapy[35,36]. In the current study, patients who had received intra- and/or postoperative radiotherapy had a 2- or 3-year cumulative survival rate of 20.0% and a median survival period of 13 mo (Table 2). By comparison, the non radiotherapy group had a 2-year cumulative survival rate of 9.0% and a median survival period of 6 mo (P = 0.284). There was no significant difference in survival between patients who did and did not receive radiotherapy.
PROGNOSIS AFTER PANCREATIC RESECTION
The overall 1-, 2-, and 3-year survival rates after pancreatic resection were 25.5%, 14.0%, and 14.0%, respectively (Figure 1). Table 1 shows operative mortality occurred in two patients during the early 1980s[7,8]. One patient died of myocardial infarction 2 d after undergoing PD and another died of numerous postoperative complications including electrolyte disturbance from massive abdominal fluid losses, acute renal failure and eventually congestive heart failure 20 d after undergoing PD[7,8]. Univariate analysis of the different prognostic factors predicted to contribute to patient prognosis showed that tumor location was the only unfavorable prognostic factor. Median survival of patients with a tumor located in the body and/or tail (4 mo) was significantly worse than those with tumors located in the head (8 mo) (Table 2). Prognostic differences based on tumor location may relate to tumor size, as the size of a distal pancreatic tumor (7.3 ± 1.8 cm) was significantly larger than that of a proximal pancreatic tumor (4.7 ± 1.9 cm, P = 0.002). Age, gender, type of operative procedure, and lymph node metastasis were not significant prognostic factors.
Figure 1.
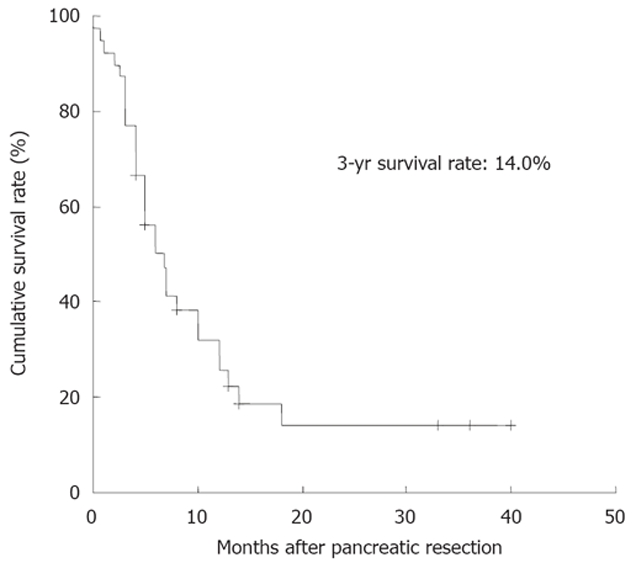
Survival after surgical resection for adenosquamous carcinoma of the pancreas (n = 39).
Recently, long-term survival after PD for pancreatic adenocarcinoma has improved, and the number of patients surviving for five or 10 years has increased[37-39]. On the other hand, the prognosis for the 39 patients with adenosquamous carcinoma in this study was poor, with a 3-year overall survival rate of only 14.0%, and includes two patients with hospital mortality. A patient surviving for five years post-resection has not been reported yet (Table 1). This suggests that adenosquamous carcinoma of the pancreas has greater malignant potential than adenocarcinoma of the pancreas. A previous report also found that squamous cell carcinomas grow at twice the speed of adenocarcinomas[31]. Therefore, once an adenocarcinoma has transformed into an adenosquamous carcinoma, the carcinoma may exhibit a higher degree of malignancy[40].
CONCLUSION
Even though curative resection for adenosquamous carcinoma of the pancreas was performed in the 39 patients, prognosis remained poor because systemic metastases in the liver and peritoneal dissemination were the major sites of recurrence (Table 1). In addition, tumor recurrence occurred during the early stages of the postoperative period in a large number of patients. Yamaue et al. reported that it might be preferable not to perform a pancreatic resection if a pancreatic tumor is diagnosed as an adenosquamous carcinoma[22]. Consensus of opinion regarding the surgical indication required for this type of tumor has not been reached yet. Elucidating a surgical treatment strategy based on the appropriate surgical indication is essential for improving the surgical outcome of adenosquamous carcinoma of the pancreas.
The results of this current study indicate that tumor location may be an important factor in determining the appropriate surgical indication. Namely, surgical resection may be better suited for proximal pancreatic tumors than for distal tumors because the proximal location of tumors was the only significant favorable prognostic factor found in this study. Furthermore, exploration of new radiation techniques and chemotherapeutic regimens using new drug agents such as gemcitabine may be required because conventional chemotherapy and radiotherapy treatments did not contribute to survival benefit. The incorporation of novel ‘molecularly targeted’ agents into therapy will also be required to improve surgical outcome.
Although adenosquamous carcinoma of the pancreas has a poor prognosis even after curative resection, we must continue to endeavor to improve the surgical outcome of this tumor, because despite its rarity, it occurs worldwide. More data, including epidemiological and pathological findings, will be required to determine the appropriate surgical indication for this tumor.
Footnotes
Peer reviewer: Salvatore Gruttadauria, Professor, Department of Abdominal Transplant Surgery, Mediterranean Institute for Transplantation and Advanced Specialized Therapies (IsMeTT), Via E. Tricomi, Palermo 90127, Italy
S- Editor Zhong XY L- Editor Logan S E- Editor Ma WH
References
- 1.Klöppel G, Hruban RH, Longnecker DS, Adler G, Kern SE, Partanen TJ. Tumours of the exocrine pancreas. In: Hamilton SR, Aaltonen LA, eds , editors. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Digestive System. Lyon: IARC Press; 2000. pp. 219–251. [Google Scholar]
- 2.Hruban RH, Pitman MB, Klimsta DS. Tumors of the pancreas. In: AFIP Atlas of Tumor Pathology. Series 4, Fascicle 6; 2007. pp. 165–168. [Google Scholar]
- 3.Nakao A, Fujii T, Sugimoto H, Kanazumi N, Nomoto S, Kodera Y, Inoue S, Takeda S. Oncological problems in pancreatic cancer surgery. World J Gastroenterol. 2006;12:4466–4472. doi: 10.3748/wjg.v12.i28.4466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, Schramm H, Fahlke J, Zuelke C, Burkart C, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007;297:267–277. doi: 10.1001/jama.297.3.267. [DOI] [PubMed] [Google Scholar]
- 5.Neoptolemos JP, Stocken DD, Friess H, Bassi C, Dunn JA, Hickey H, Beger H, Fernandez-Cruz L, Dervenis C, Lacaine F, et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med. 2004;350:1200–1210. doi: 10.1056/NEJMoa032295. [DOI] [PubMed] [Google Scholar]
- 6.Shaib Y, Davila J, Naumann C, El-Serag H. The impact of curative intent surgery on the survival of pancreatic cancer patients: a U.S. Population-based study. Am J Gastroenterol. 2007;102:1377–1382. doi: 10.1111/j.1572-0241.2007.01202.x. [DOI] [PubMed] [Google Scholar]
- 7.Ishikawa O, Matsui Y, Aoki I, Iwanaga T, Terasawa T, Wada A. Adenosquamous carcinoma of the pancreas: a clinicopathologic study and report of three cases. Cancer. 1980;46:1192–1196. doi: 10.1002/1097-0142(19800901)46:5<1192::aid-cncr2820460519>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 8.Wilczynski SP, Valente PT, Atkinson BF. Cytodiagnosis of adenosquamous carcinoma of the pancreas. Use of intraoperative fine needle aspiration. Acta Cytol. 1984;28:733–736. [PubMed] [Google Scholar]
- 9.Yamaguchi K, Enjoji M. Adenosquamous carcinoma of the pancreas: a clinicopathologic study. J Surg Oncol. 1991;47:109–116. doi: 10.1002/jso.2930470210. [DOI] [PubMed] [Google Scholar]
- 10.Motojima K, Tomioka T, Kohara N, Tsunoda T, Kanematsu T. Immunohistochemical characteristics of adenosquamous carcinoma of the pancreas. J Surg Oncol. 1992;49:58–62. doi: 10.1002/jso.2930490114. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka N, Ohoida J, Matuno T, Gouchim A, Iwagaki H, Moreira LF, Orita K. Response of adenosquamous carcinoma of the pancreas to interferon-alpha, tumor necrosis factor-alpha and 5-fluorouracil combined treatment. Anticancer Res. 1994;14:2739–2742. [PubMed] [Google Scholar]
- 12.Makiyama K, Takuma K, Zea-Iriarte WL, Ikuno N, Kawatomi M, Mori N, Ishino T, Yonemitsu N. Adenosquamous carcinoma of the pancreas. J Gastroenterol. 1995;30:798–802. doi: 10.1007/BF02349652. [DOI] [PubMed] [Google Scholar]
- 13.Onoda N, Kang SM, Sugano S, Yamashita Y, Chung YS, Sowa M. Mucoepidermoid carcinoma of the pancreas: report of a case. Surg Today. 1995;25:843–847. doi: 10.1007/BF00311465. [DOI] [PubMed] [Google Scholar]
- 14.Campman SC, Fajardo MA, Rippon MB, Kraegel SA, Ruebner BH. Adenosquamous carcinoma arising in a mucinous cystadenoma of the pancreas. J Surg Oncol. 1997;64:159–162. doi: 10.1002/(sici)1096-9098(199702)64:2<159::aid-jso13>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 15.Kuji I, Sumiya H, Taki J, Nakajima K, Yokoyama K, Kinuya S, Kinuya K, Ichikawa A, Konishi S, Michigishi T, et al. Intense Ga-67 uptake in adenosquamous carcinoma of the pancreas. Ann Nucl Med. 1997;11:41–43. doi: 10.1007/BF03164758. [DOI] [PubMed] [Google Scholar]
- 16.Nabae T, Yamaguchi K, Takahata S, Utsunomiya N, Matsunaga H, Sumiyoshi K, Chijiiwa K, Tanaka M. Adenosquamous carcinoma of the pancreas: report of two cases. Am J Gastroenterol. 1998;93:1167–1170. doi: 10.1111/j.1572-0241.1998.00299.x. [DOI] [PubMed] [Google Scholar]
- 17.Myung SJ, Kim MH, Lee SK, Seo DW, Kim YS, Min YI. Adenosquamous carcinoma of the pancreas: differentiation from pancreatic pseudocyst. Gastrointest Endosc. 1998;47:410–413. doi: 10.1016/s0016-5107(98)70230-5. [DOI] [PubMed] [Google Scholar]
- 18.Lozano MD, Panizo A, Sola IJ, Pardo-Mindan FJ. FNAC guided by computed tomography in the diagnosis of primary pancreatic adenosquamous carcinoma. A report of three cases. Acta Cytol. 1998;42:1451–1454. doi: 10.1159/000332185. [DOI] [PubMed] [Google Scholar]
- 19.Aranha GV, Yong S, Olson M. Adenosquamous carcinoma of the pancreas. Int J Pancreatol. 1999;26:85–91. doi: 10.1007/BF02781735. [DOI] [PubMed] [Google Scholar]
- 20.Komatsuda T, Ishida H, Konno K, Sato M, Watanabe S, Furuya T, Ishida J. Adenosquamous carcinoma of the pancreas: report of two cases. Abdom Imaging. 2000;25:420–423. doi: 10.1007/s002610000059. [DOI] [PubMed] [Google Scholar]
- 21.Yavuz E, Kapran Y, Ozden I, Bulut T, Dizdaroglu F. Pancreatobiliary adenosquamous carcinoma (report of two cases) Pathologica. 2000;92:323–326. [PubMed] [Google Scholar]
- 22.Yamaue H, Tanimura H, Onishi H, Tani M, Kinoshita H, Kawai M, Yokoyama S, Uchiyama K. Adenosquamous carcinoma of the pancreas: successful treatment with extended radical surgery, intraoperative radiation therapy, and locoregional chemotherapy. Int J Pancreatol. 2001;29:53–58. [PubMed] [Google Scholar]
- 23.Kardon DE, Thompson LD, Przygodzki RM, Heffess CS. Adenosquamous carcinoma of the pancreas: a clinicopathologic series of 25 cases. Mod Pathol. 2001;14:443–451. doi: 10.1038/modpathol.3880332. [DOI] [PubMed] [Google Scholar]
- 24.Murakami Y, Yokoyama T, Yokoyama Y, Kanehiro T, Uemura K, Sasaki M, Morifuji M, Sueda T. Adenosquamous carcinoma of the pancreas: preoperative diagnosis and molecular alterations. J Gastroenterol. 2003;38:1171–1175. doi: 10.1007/s00535-003-1226-4. [DOI] [PubMed] [Google Scholar]
- 25.Rahemtullah A, Misdraji J, Pitman MB. Adenosquamous carcinoma of the pancreas: cytologic features in 14 cases. Cancer. 2003;99:372–378. doi: 10.1002/cncr.11855. [DOI] [PubMed] [Google Scholar]
- 26.Alwaheeb S, Chetty R. Adenosquamous carcinoma of the pancreas with an acantholytic pattern together with osteoclast-like and pleomorphic giant cells. J Clin Pathol. 2005;58:987–990. doi: 10.1136/jcp.2004.025221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsu JT, Yeh CN, Chen YR, Chen HM, Hwang TL, Jan YY, Chen MF. Adenosquamous carcinoma of the pancreas. Digestion. 2005;72:104–108. doi: 10.1159/000088364. [DOI] [PubMed] [Google Scholar]
- 28.Jamali M, Serra S, Chetty R. Adenosquamous carcinoma of the pancreas with clear cell and rhabdoid components. A case report. JOP. 2007;8:330–334. [PubMed] [Google Scholar]
- 29.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 30.Madura JA, Jarman BT, Doherty MG, Yum MN, Howard TJ. Adenosquamous carcinoma of the pancreas. Arch Surg. 1999;134:599–603. doi: 10.1001/archsurg.134.6.599. [DOI] [PubMed] [Google Scholar]
- 31.O'Connor JK, Sause WT, Hazard LJ, Belnap LP, Noyes RD. Survival after attempted surgical resection and intraoperative radiation therapy for pancreatic and periampullary adeno-carcinoma. Int J Radiat Oncol Biol Phys. 2005;63:1060–1066. doi: 10.1016/j.ijrobp.2005.03.036. [DOI] [PubMed] [Google Scholar]
- 32.Neoptolemos JP, Dunn JA, Stocken DD, Almond J, Link K, Beger H, Bassi C, Falconi M, Pederzoli P, Dervenis C, et al. Adjuvant chemoradiotherapy and chemotherapy in resectable pancreatic cancer: a randomised controlled trial. Lancet. 2001;358:1576–1585. doi: 10.1016/s0140-6736(01)06651-x. [DOI] [PubMed] [Google Scholar]
- 33.Neuhaus P, Oettle H, Post H, Gellert K, Ridwelski K, Schramm H, Zurke C, Fahlke G, Langrehr J, Reiss H. A randomized, prospective, multicenter, phase III trial of adjuvant chemotherapy with gemcitabine vs. observation in patients with resected pancreatic cancer. Proc Am Soc Clin Oncol. 2005;23:311s. [Google Scholar]
- 34.Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, Schramm H, Fahlke J, Zuelke C, Burkart C, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007;297:267–277. doi: 10.1001/jama.297.3.267. [DOI] [PubMed] [Google Scholar]
- 35.Ihse I, Andersson R, Ask A, Ewers SB, Lindell G, Tranberg KG. Intraoperative radiotherapy for patients with carcinoma of the pancreas. Pancreatology. 2005;5:438–442. doi: 10.1159/000086546. [DOI] [PubMed] [Google Scholar]
- 36.Nakagohri T, Kinoshita T, Konishi M, Takahashi S, Tanizawa Y. Clinical results of extended lymphadenectomy and intraoperative radiotherapy for pancreatic adenoca-rcinoma. Hepatogastroenterology. 2007;54:564–569. [PubMed] [Google Scholar]
- 37.Nitecki SS, Sarr MG, Colby TV, van Heerden JA. Long-term survival after resection for ductal adenocarcinoma of the pancreas. Is it really improving? Ann Surg. 1995;221:59–66. doi: 10.1097/00000658-199501000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matsuno S, Egawa S, Fukuyama S, Motoi F, Sunamura M, Isaji S, Imaizumi T, Okada S, Kato H, Suda K, et al. Pancreatic Cancer Registry in Japan: 20 years of experience. Pancreas. 2004;28:219–230. doi: 10.1097/00006676-200404000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Schnelldorfer T, Ware AL, Sarr MG, Smyrk TC, Zhang L, Qin R, Gullerud RE, Donohue JH, Nagorney DM, Farnell MB. Long-term survival after pancreatoduodenectomy for pancreatic adenocarcinoma: is cure possible? Ann Surg. 2008;247:456–462. doi: 10.1097/SLA.0b013e3181613142. [DOI] [PubMed] [Google Scholar]
- 40.Iemura A, Yano H, Mizoguchi A, Kojiro M. A cholangio-cellular carcinoma nude mouse strain showing histologic alteration from adenocarcinoma to squamous cell carcinoma. Cancer. 1992;70:415–422. doi: 10.1002/1097-0142(19920715)70:2<415::aid-cncr2820700208>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]


