Abstract
AIM: To clarify the effectiveness of CO2 insufflation in potentially difficult colonoscopy cases, particularly in relation to the experience level of colonoscopists.
METHODS: One hundred twenty potentially difficult cases were included in this study, which involved females with a low body mass index and patients with earlier abdominal and/or pelvic open surgery or previously diagnosed left-side colon diverticulosis. Patients receiving colonoscopy examinations without sedation using a pediatric variable-stiffness colonoscope were divided into two groups based on either CO2 or standard air insufflation. Both insufflation procedures were also evaluated according to the experience level of the respective colonoscopists who were divided into an experienced colonoscopist (EC) group and a less experienced colonoscopist (LEC) group. Study measurements included a 100-mm visual analogue scale (VAS) for patient pain during and after colonoscopy examinations, in addition to insertion to the cecum and withdrawal times.
RESULTS: Examination times did not differ, however, VAS scores in the CO2 group were significantly better than in the air group (P < 0.001, two-way ANOVA) from immediately after the procedure and up to 2 h later. There were no significant differences between either insufflation method in the EC group (P = 0.29), however, VAS scores for CO2 insufflation were significantly better than air insufflation in the LEC group (P = 0.023) immediately after colonoscopies and up to 4 h afterwards.
CONCLUSION: CO2 insufflation reduced patient pain after colonoscopy in potentially difficult cases when performed by LECs.
Keywords: CO2 insufflation, Colonoscopy, Difficult colonoscopy, Experienced colonoscopist, Training
INTRODUCTION
Colonoscopy has a high profile because of its increasingly important role in successfully preventing, detecting and treating colorectal cancer[1,2], however, some patients experience considerable abdominal pain and discomfort when the procedure is performed using air insufflation. In particular, the so-called “difficult colonoscopy” cases[3-6], which involve female patients with a relatively low body mass index (BMI), patients with a history of abdominal and/or pelvic open surgery and male patients with diverticulosis, often require prolonged insertion to the cecum, thus this procedure can cause increased abdominal pain and discomfort for such patients.
Factors accounting for longer examination times and increased abdominal pain and discomfort can be derived from both a patient’s condition and the examining colonoscopist’s skill and experience[7-9]. Novice and even moderately skilled colonoscopists must improve their technical abilities by gaining experience in successfully handling difficult colonoscopies to become qualified experts, as a suitably high-level colonoscopy training environment has not been established as yet[10,11].
CO2 insufflation has been reported to reduce patient abdominal pain and discomfort during and after colonoscopies[12-15]. Although the safety and efficacy of CO2 insufflation during colonoscopies have been assessed in earlier studies, air insufflation is still the standard method due to a lack of suitable equipment and inadequate information as to when and on whom CO2 insufflation should be used during colonoscopy examinations.
We decided to conduct a prospective randomized controlled trial to test the hypothesis that CO2 insufflation reduces patient abdominal pain and discomfort during and after colonoscopy examinations in potentially difficult cases.
MATERIALS AND METHODS
Study protocol
Consecutive patients considered potentially difficult cases for colonoscopic intubation were included in this prospective randomized controlled trial which took place between September 2006 and October 2007. The aim of this study was to clarify the effectiveness of CO2 insufflation during colonoscopy examinations, with the primary objectives of assessing both patient tolerance and the safety of CO2 insufflation in these potentially difficult cases. A secondary objective was to clarify any differences between the two insufflation methods in relation to the experience level of the participating colonoscopists. This study was approved by the Ethics Committee at Okayama University Hospital.
Patients
Patients considered potentially difficult colonoscopy cases, based on published information and clinical experience, were selected, and included females with a relatively low BMI (BMI < 22), patients with a history of abdominal and/or pelvic open surgery, with the exception of low risk procedures for adhesions such as appendectomy or hernia repair, and male patients with previously diagnosed left-side diverticulosis[3-6].
The indications for colonoscopy examination were the standard clinical criteria: colorectal cancer screening, surveillance for polyps, a positive fecal occult blood test, abdominal symptoms or anemia. Exclusion factors included severe heart or lung disease, a prior colorectal resection, inflammatory bowel disease, severe hematochezia and repeat colonoscopy for therapeutic procedures including polypectomy.
Written informed consent was obtained from each patient and enrolled patients were randomly divided into two groups for colonoscopy examinations using either CO2 or standard air insufflation. Group allocation for both patients and colonoscopists was performed by specially assigned nurses using standard randomization lists which contained consecutive patient numbers. Each number was linked to one of the two study groups for allocation purposes. These lists were not accessible by the participating colonoscopists.
Colonoscopy using CO2 insufflation
Patients underwent bowel preparation with sodium picosulfate the day before their examinations and two liters of polyethylene glycol solution-containing lavage the morning of their colonoscopies. Scopolamine butylbromide (20 mg) was administered intramuscularly to suppress bowel movement, while patients with cardiac disease or benign prostatic hypertrophy received glucagon (1 IU) intramuscularly. Patients were not sedated, although midazolam (2-3 mg, iv) was administered based on the examining colonoscopist’s judgment or when requested by the patient due to abdominal pain or distension. Examinations were performed using a pediatric variable-stiffness colonoscope (PVSC) with a distal tip diameter of 11.3 mm (PCF-Q260AI, Olympus Co, Tokyo, Japan).
Procedures were randomly performed by eight colonoscopists who had earlier been divided into two groups according to their colonoscopy experience: four highly experienced colonoscopists (EC) group each of whom had been in colonoscopy practice for over 10 years (TU, JK, KT and SH), and four less experienced colonoscopists (LEC) group with 5-7 years of colonoscopy practice during which each had performed 900-1500 colonoscopies (MK, SI, KH and HF).
If an examining colonoscopist from the LEC group failed to pass through the sigmoid-descending colon junction within 15 min or a patient complained of severe pain, a colonoscopist from the EC group replaced the initial examiner before midazolam was administered and continued insertion to the cecum. When such a case involved a colonoscopist from the EC group as the initial examiner, a more experienced member of the EC group would continue the procedure. After reaching the cecum, the initial examiner proceeded with withdrawal of the colonoscope.
A “complete colonoscopy” was defined as successful insertion to the cecum bottom or terminal ileum. Insertion to the cecum and withdrawal time was recorded for every colonoscopy.
CO2 insufflation and monitoring system
CO2 was administered using a commercial CO2 regulator (Gas Regulator, Crown, Model FR-IIS-P; Yutaka Engineering, Tokyo, Japan) connected to a CO2 bottle. The regulator delivered CO2 at the rate of 2 L/min. CO2 and air insufflations were used in a blind fashion both to patients and colonoscopists with full-day colonoscopy sessions randomly assigned CO2 or air insufflation to avoid unblinding caused by set-up changes between patients.
CO2 partial pressure was continuously measured using a transcutaneous CO2 monitoring system (TOSCA 500; Radiometer Basel AG, Switzerland). Processed transcutaneous CO2 readings (PtcCO2) correlate closely with directly obtained arterial blood gas results[16,17]. Sensors were attached to a patient’s ear lobe with a monitor-specific clip. A colonoscopy assistant recorded readings and an independent observer monitored gas readings to avoid potential serious side effects. CO2 insufflation was stopped immediately if PtcCO2 registered > 60 mmHg during any colonoscopy examination.
Pain and discomfort measurement
A 100-mm visual analogue scale (VAS) consisting of a horizontal line 100 mm in length was used for measuring patient abdominal pain and discomfort (0 mm = painless, 100 mm = extremely painful)[18]. Patients recorded the pain level experienced upon reaching the cecum bottom, immediately following their examinations and 30 min, 1, 2, 4 and 6 h afterwards. The VAS score was the distance measured to the nearest millimeter from the left end of the line to the point of the patient’s mark.
Another member of the medical staff, who did not know how the procedures were performed, interviewed the patients 30 min after completion of their colonoscopies. A questionnaire was then given to the patients to take home to complete as instructed at intervals of 1, 2, 4 and 6 h and the completed forms were then mailed to the hospital the following day. The completed questionnaires were subsequently mailed to our medical office. No follow-up phone calls were made as 98% of all questionnaires were promptly returned.
Statistical analysis
A preliminary pilot study was conducted to estimate the SD in pain measurements. With an assumed SD of 19 mm, the study sample size was calculated at 110 patients in order to have an 80% power with two-sided α levels of 0.05 to detect any differences in VAS scores between the two insufflation groups (≥ 10 mm was considered clinically important).
The outcomes for our secondary objective to clarify any differences between the two insufflation methods in relation to the experience level of participating colonoscopists were analyzed on an intention-to-treat basis, given the fact that a number of the initial examining colonoscopists were replaced during the insertion phase of the procedure. Statistical comparisons were made using chi-square and Fisher’s exact tests. ANOVA was used for repeated measures statistical analysis of pain. Some variables were not distributed normally, thus the Wilcoxon rank sum test was applied for supplementary analysis to compare groups at each measurement point. Statistical analyses were performed using Prism version 5.0 (GraphPad Software, San Diego, CA, USA) and JMP version 6.3 (SAS Institute, Cary, NC, USA). A P value < 0.05 was considered significant.
RESULTS
Baseline characteristics
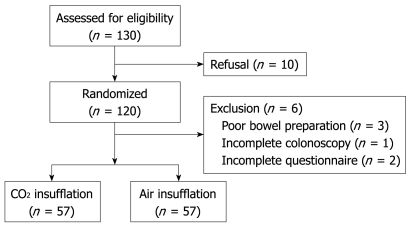
A total of 130 patients were asked to participate and 120 consenting patients were randomized into two groups prior to their colonoscopy examinations (Figure 1). Three poor bowel preparation patients were not included and one (0.85%, 1/117) incomplete intubation patient in the air insufflation group with a history of abdominal and pelvic open surgery, whose examination was performed by an EC, was not submitted for consideration. Completed questionnaires were received from 98% of the 116 remaining patients, thus a final total of 114 patients (68% female/32% male) were analyzed in this study. Exactly half or 57 patients were examined using CO2 insufflation and the other 57 patients were examined with air insufflation. There were no significant differences in baseline patient characteristics including eligibility criteria for potentially difficult cases between the two groups (Table 1).
Figure 1.
Patient flow chart.
Table 1.
Patient characteristics (n = 114) n (%)
| CO2 group (n = 57) | Air group (n = 57) | P value | |
| Median age, yr (IQR) | 65 (59-73) | 62 (47-71) | 0.107 |
| Females | 39 (68) | 38 (67) | 1.00 |
| Eligibility criteria for difficult cases1 | |||
| Females with relatively low BMI (< 22) | 35 (61) | 36 (63) | 0.133 |
| Previous abdominal and/or pelvic open surgery | 41 (72) | 37 (65) | 0.546 |
| Males with previously diagnosed left-side diverticulosis | 6 (11) | 2 (4) | 0.271 |
| One or more previous colonoscopies | 16 (28) | 15 (26) | 1.00 |
Some patients had more than one difficult case factor. IQR: Interquartile range; BMI: Body mass index.
Outcome measures comparing CO2 and air insufflation groups
There were no significant differences in procedure times including intubation, withdrawal and total time between the two groups (Table 2). Midazolam was administered to two patients (4%) in each group. There were no instances of PtcCO2 > 60 mmHg in the CO2 insufflation patients or any procedure-related complications in either group.
Table 2.
Use of antispasmodic drugs & median procedure times for CO2 & air insufflation groups
| CO2 group (n = 57) | Air group (n = 57) | P value | |
| Patients receiving antispasmodic drug (%) | 54 (95) | 56 (98) | 0.616 |
| Median total procedure time, min (IQR) | 22.5 (17.9-29.6) | 22.3 (16.3-43.9) | 0.734 |
| Insertion to cecum | 10.3 (6.5-16.6) | 9.6 (5.8-16.2) | 0.601 |
| Withdrawal | 11.9 (10.1-13.6) | 12.0 (9.8-14.2) | 0.986 |
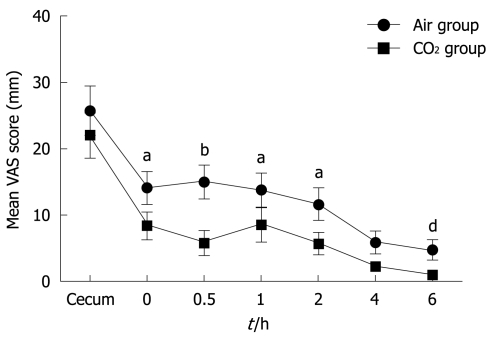
Figure 2 shows the mean VAS scores during and after colonoscopy examinations. VAS scores in the CO2 insufflation group were significantly better than those in the air insufflation group (P < 0.001, ANOVA for repeated measures). The overall mean difference was 5.3 mm (95% CI: 3.5-7.1, P < 0.001). Comparison by nonparametric analysis at each measurement point produced results favoring CO2 insufflation immediately following the examinations and up to 2 h afterwards. The maximum mean difference of 9.2 mm (95% CI: 0.4-18.0, P = 0.0049) was recorded 30 min after the examinations.
Figure 2.
Mean VAS scores at corresponding measurement points during and after colonoscopy examinations in CO2 and air insufflation groups. VAS scores for CO2 insufflation were significantly better than those for air insufflation (dP < 0.001, ANOVA for repeated measures). aP < 0.05, bP < 0.01 vs the CO2 group at each measurement point by Wilcoxon rank sum test. VAS: Visual analogue scale.
Subgroup analysis
Based on the subgroup analysis relative to experience level of the participating colonoscopists, we evaluated 53 patients (46%) in the EC group and 61 patients (54%) in the LEC group. There were no significant differences in eligibility criteria for potentially difficult cases between the two groups, however, the EC group achieved insertion to the cecum significantly faster, while withdrawal and total procedure times were also significantly shorter than those in the LEC group (Table 3). The number of replacements by another colonoscopist was larger in the LEC group (5) than in the EC group (1), however, there was no significant difference between the two groups.
Table 3.
Median procedure times for colonoscopist groups
| EC group (n = 53) | LEC group (n = 61) | P value | |
| Median total procedure time, min (IQR) | 19.5 (15.3-25.8) | 23.8 (19.2-34.5) | 0.005 |
| Insertion to cecum | 7.7 (5.1-13.2) | 12.5 (7.0-18.9) | 0.036 |
| Withdrawal | 10.9 (10.0-13.0) | 12.5 (10.2-15.1) | 0.003 |
| Examiner replaced during intubation | 1 | 5 | 0.213 |
EC: Experienced colonoscopist; LEC: Less experienced colonoscopist.
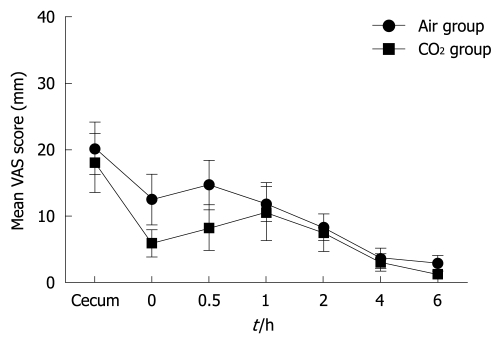
Figure 3 shows the mean VAS scores for 27 CO2 insufflation patients and 26 air insufflation patients during and following colonoscopy examinations performed by the EC group. There were no significant differences in the mean VAS scores between the two patient groups (P = 0.29, ANOVA for repeated measures). A comparison of the two patient groups at each measurement point also revealed no significant differences. The maximum mean difference of 6.5 mm (95% CI: -3.7-16.6, P = 0.207) occurred 30 min after the examinations.
Figure 3.
Mean VAS scores at corresponding measurement points during and after colonoscopy examinations for experienced colonoscopists (EC group) in CO2 and air insufflation groups. There were no significant differences in VAS scores between the two insufflation groups for EC group (P = 0.29, ANOVA for repeated measures).
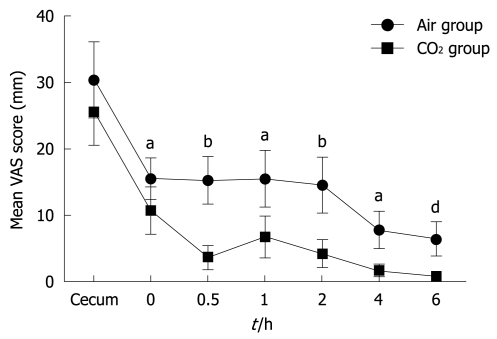
In the LEC group, 30 CO2 insufflation patients were evaluated along with 31 air insufflation patients. The mean VAS scores in the CO2 insufflation group were significantly better than those in the air insufflation group (P = 0.023, ANOVA for repeated measures) (Figure 4). The overall mean difference was 7.5 mm (95% CI: 4.9-10.0, P < 0.001). A comparison of the two groups by nonparametric analysis at each measurement point produced results favoring CO2 insufflation from immediately after the examinations up to 4 h later with the maximum mean difference of 11.6 mm (95% CI: 3.4-19.8, P = 0.006) occurring 30 min after the examinations.
Figure 4.
Mean VAS scores at corresponding measurement points during and after colonoscopy examinations for less experienced colonoscopists (LEC group) in CO2 and air insufflation groups. VAS scores for CO2 insufflation were significantly better compared to air insufflation for LEC group (dP = 0.023, ANOVA for repeated measures). aP < 0.05, bP < 0.01 vs the CO2 group at each measurement point by Wilcoxon rank sum test.
DISCUSSION
The increase in patient abdominal pain and discomfort often encountered in difficult colonoscopy examination cases is a concern that needs to be satisfactorily resolved by colonoscopists. In this study, we successfully demonstrated the clinical effectiveness of CO2 insufflation in potentially difficult colonoscopy examination cases. We also clarified the efficacy of CO2 insufflation for LECs compared to highly ECs.
CO2 with its characteristic rapid rate of absorption into surrounding tissue has been reported to be more suitable than atmospheric air in various clinical settings[12-15]. In fact, several randomized trials have shown that CO2 insufflation reduced post-colonoscopy abdominal pain and discomfort compared to conventional air insufflation in ambulatory settings. Bretthauer et al[15] demonstrated that CO2 insufflation was not only effective, but also safe during colonoscopies in patients receiving conscious sedation. Saito et al[19] introduced the use of CO2 insufflation during lengthier colorectal endoscopic submucosal dissections in patients receiving conscious sedation. Their results demonstrated the effectiveness and safety of CO2 insufflation as well as a resultant reduction in total dosage of midazolam. CO2 insufflation has also been applied in endoscopic retrograde cholangiopancreatography (ERCP)[20] and endoscopic dilatation therapy using a double balloon endoscope[21]. There have been few detailed investigative reports on the use of CO2 insufflation during difficult colonoscopy cases. In addition, the effect of the relative experience of colonoscopists using CO2 insufflation has not been previously analyzed.
This study validated our theory that CO2 insufflation is more effective than air insufflation in potentially difficult colonoscopy cases with the comparative difference for the two procedures being particularly discernable between LECs and ECs. Colonoscopy is a technically demanding procedure requiring considerable instruction and on-the-job experience for optimal performance. A suitable training program and sufficient opportunities to improve practical skills in a clinical setting are essential for beginners as well as colonoscopists with a moderate degree of experience[10,11,22].
Difficult colonoscopy examinations performed by LECs require additional time as do ERCP and therapeutic endoscopic procedures, and can cause patient abdominal pain and discomfort both during the procedure and afterwards. The results of our study demonstrated a difference not only in intubation times, but also in withdrawal and overall examination times according to the experience of the participating colonoscopists. Avoiding prolonged insufflation especially during insertion, however, might have led to similar results in the LEC group concerning the clinical effectiveness of CO2 in reducing patient pain and discomfort.
Lee et al[8] recommended that trainees perform over 150 examinations in a colonoscopy training program to be technically competent for diagnostic colonoscopy. Our results revealed significant differences in examination times and patient abdominal pain and discomfort after colonoscopy between the EC and LEC groups. The four colonoscopists in the LEC group had each performed a minimum of 900 colonoscopies, thus the question arises as to whether a minimum of 150 cases referred to in the report by Lee above, is sufficient for conducting examinations in potentially difficult colonoscopy cases.
A recent study in Ontario, Canada analyzed factors associated with incomplete colonoscopies based on the following settings: an academic hospital, a community hospital and private medical offices. The incomplete colonoscopy rate was highest in private offices with an odds ratio increase of more than three-fold[3], thus introducing CO2 insufflation may be particularly useful in reducing patient complaints in non-hospital environments. We refrained from using novice colonoscopists in this study because of the formidable nature of potentially difficult colonoscopy cases. Such novices should only conduct difficult colonoscopies after gaining the necessary experience performing routine colonoscopy examinations.
A number of techniques and devices have reportedly been effective in reducing patient abdominal pain and discomfort during difficult colonoscopies, improving the rate of successful insertion to the cecum, shortening insertion time to the cecum and reducing the dosage of sedatives[23] including the use of a pediatric colonoscope[24], variable stiffness colonoscope[25], gastroscope[26], double balloon endoscope[27] and hood attached to the top of the colonoscope[28]. A PVSC featuring both variable stiffness on demand and a thin diameter was used in our trial. Previously, this instrument was shown not to be superior to adult or standard pediatric colonoscopes[29-32]. However, there have been reports that use of the PVSC made it possible to complete colonoscopies that would have been much more difficult or impossible to perform using an adult colonoscope, including patients who had undergone hysterectomies[31] and patients with diverticular disease and severe stenosis[32].
There was only one case (0.85%) of incomplete insertion to the cecum in our study and just four (3.5%) patients required sedation. Complete screening colonoscopy without sedation or with on-demand sedation in academic medical centers has been reported to be in the 88%-99% range[33-36], with the optimum intubation rate obtained using a PVSC. In this study, the PVSC more than likely contributed to the impressive successful intubation rates and reduction in pain during insertion to the cecum achieved in both groups, as well as the favorable intubation times for each group. In several studies performed by ECs at academic medical centers, insertion to the cecum times varied between 7-13 min for colonoscopies performed without sedation or with on-demand sedation[33-36]. Our median intubation times of 7.7 and 12.5 min for ECs and LECs, respectively, were in line with these earlier reports.
In conclusion, we clearly demonstrated the clinical effectiveness of CO2 insufflation in potentially difficult colonoscopy examination cases performed without sedation. We also successfully clarified the efficacy of CO2 insufflation for LECs.
COMMENTS
Background
Colonoscopy is the preferred method for preventing, detecting and treating colorectal cancer, however, prolonged cecal intubation can cause increased patient abdominal pain and discomfort especially in difficult cases, such as female patients with a relatively low body mass index, patients with a history of abdominal and/or pelvic open surgery and male patients with diverticulosis. CO2 with its rapid rate of absorption has been reported to be more suitable than atmospheric air as an insufflation agent in various clinical settings, although air insufflation is still the standard method due to a lack of suitable equipment and inadequate information as to when and on whom CO2 insufflation should be used during colonoscopy examinations.
Research frontiers
This prospective randomized controlled study was conducted to clarify the effectiveness of CO2 insufflation in potentially difficult cases, particularly in relation to colonoscopist experience level.
Innovations and breakthroughs
The clinical effectiveness of CO2 insufflation was clearly demonstrated in potentially difficult colonoscopy examination cases performed without sedation. The procedure that was followed also clarified the efficacy of CO2 insufflation for less experienced colonoscopists (LEC) particularly in comparison to more experienced colonoscopists.
Applications
The use of CO2 insufflation can be incorporated into existing and future colonoscopy training programs in order to further improve the technical skills of colonoscopists.
Peer review
The authors successfully demonstrated that CO2 insufflation with its rapid rate of CO2 absorption and improved efficacy reduced patient pain in potentially difficult cases particularly when colonoscopy examinations were performed by LECs.
Footnotes
Supported by The Japanese Foundation for Research and Promotion of Endoscopy (JFE)
Peer reviewer: Douglas K Rex, Professor, Department of Medicine, Indiana University School of Medicine, Indiana University Hospital, No. 4100, 550 N, University Boulevard, Indianapolis, IN 46202, United States
S- Editor Li LF L- Editor Webster JR E- Editor Zheng XM
References
- 1.Winawer SJ, Zauber AG, Ho MN, O'Brien MJ, Gottlieb LS, Sternberg SS, Waye JD, Schapiro M, Bond JH, Panish JF. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977–1981. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 2.Winawer S, Fletcher R, Rex D, Bond J, Burt R, Ferrucci J, Ganiats T, Levin T, Woolf S, Johnson D, et al. Colorectal cancer screening and surveillance: clinical guidelines and rationale-Update based on new evidence. Gastroenterology. 2003;124:544–560. doi: 10.1053/gast.2003.50044. [DOI] [PubMed] [Google Scholar]
- 3.Shah HA, Paszat LF, Saskin R, Stukel TA, Rabeneck L. Factors associated with incomplete colonoscopy: a population-based study. Gastroenterology. 2007;132:2297–2303. doi: 10.1053/j.gastro.2007.03.032. [DOI] [PubMed] [Google Scholar]
- 4.Kim WH, Cho YJ, Park JY, Min PK, Kang JK, Park IS. Factors affecting insertion time and patient discomfort during colonoscopy. Gastrointest Endosc. 2000;52:600–605. doi: 10.1067/mge.2000.109802. [DOI] [PubMed] [Google Scholar]
- 5.Anderson JC, Gonzalez JD, Messina CR, Pollack BJ. Factors that predict incomplete colonoscopy: thinner is not always better. Am J Gastroenterol. 2000;95:2784–2787. doi: 10.1111/j.1572-0241.2000.03186.x. [DOI] [PubMed] [Google Scholar]
- 6.Nelson DB, McQuaid KR, Bond JH, Lieberman DA, Weiss DG, Johnston TK. Procedural success and complications of large-scale screening colonoscopy. Gastrointest Endosc. 2002;55:307–314. doi: 10.1067/mge.2002.121883. [DOI] [PubMed] [Google Scholar]
- 7.Bernstein C, Thorn M, Monsees K, Spell R, O'Connor JB. A prospective study of factors that determine cecal intubation time at colonoscopy. Gastrointest Endosc. 2005;61:72–75. doi: 10.1016/s0016-5107(04)02461-7. [DOI] [PubMed] [Google Scholar]
- 8.Lee SH, Chung IK, Kim SJ, Kim JO, Ko BM, Hwangbo Y, Kim WH, Park DH, Lee SK, Park CH, et al. An adequate level of training for technical competence in screening and diagnostic colonoscopy: a prospective multicenter evaluation of the learning curve. Gastrointest Endosc. 2008;67:683–689. doi: 10.1016/j.gie.2007.10.018. [DOI] [PubMed] [Google Scholar]
- 9.Eckardt AJ, Swales C, Bhattacharya K, Wassef WY, Phelan NP, Zubair S, Martins N, Patel S, Moquin B, Anwar N, et al. Open access colonoscopy in the training setting: which factors affect patient satisfaction and pain? Endoscopy. 2008;40:98–105. doi: 10.1055/s-2007-995469. [DOI] [PubMed] [Google Scholar]
- 10.Bowles CJ, Leicester R, Romaya C, Swarbrick E, Williams CB, Epstein O. A prospective study of colonoscopy practice in the UK today: are we adequately prepared for national colorectal cancer screening tomorrow? Gut. 2004;53:277–283. doi: 10.1136/gut.2003.016436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bisschops R, Wilmer A, Tack J. A survey on gastroenterology training in Europe. Gut. 2002;50:724–729. doi: 10.1136/gut.50.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bretthauer M, Thiis-Evensen E, Huppertz-Hauss G, Gisselsson L, Grotmol T, Skovlund E, Hoff G. NORCCAP (Norwegian colorectal cancer prevention): a randomised trial to assess the safety and efficacy of carbon dioxide versus air insufflation in colonoscopy. Gut. 2002;50:604–607. doi: 10.1136/gut.50.5.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sumanac K, Zealley I, Fox BM, Rawlinson J, Salena B, Marshall JK, Stevenson GW, Hunt RH. Minimizing postcolonoscopy abdominal pain by using CO(2) insufflation: a prospective, randomized, double blind, controlled trial evaluating a new commercially available CO(2) delivery system. Gastrointest Endosc. 2002;56:190–194. doi: 10.1016/s0016-5107(02)70176-4. [DOI] [PubMed] [Google Scholar]
- 14.Church J, Delaney C. Randomized, controlled trial of carbon dioxide insufflation during colonoscopy. Dis Colon Rectum. 2003;46:322–326. doi: 10.1007/s10350-004-6549-6. [DOI] [PubMed] [Google Scholar]
- 15.Bretthauer M, Lynge AB, Thiis-Evensen E, Hoff G, Fausa O, Aabakken L. Carbon dioxide insufflation in colonoscopy: safe and effective in sedated patients. Endoscopy. 2005;37:706–709. doi: 10.1055/s-2005-870154. [DOI] [PubMed] [Google Scholar]
- 16.Gisiger PA, Palma JP, Eberhard P. OxiCarbo®, a single sensor for the non-invasive measurement of arterial oxygen saturation and CO2 partial pressure at the ear lobe. Sens Actuators B Chem. 2001;76:527–530. [Google Scholar]
- 17.Heuss LT, Chhajed PN, Schnieper P, Hirt T, Beglinger C. Combined pulse oximetry/cutaneous carbon dioxide tension monitoring during colonoscopies: pilot study with a smart ear clip. Digestion. 2004;70:152–158. doi: 10.1159/000081515. [DOI] [PubMed] [Google Scholar]
- 18.Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–236. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 19.Saito Y, Uraoka T, Matsuda T, Emura F, Ikehara H, Mashimo Y, Kikuchi T, Kozu T, Saito D. A pilot study to assess the safety and efficacy of carbon dioxide insufflation during colorectal endoscopic submucosal dissection with the patient under conscious sedation. Gastrointest Endosc. 2007;65:537–542. doi: 10.1016/j.gie.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 20.Bretthauer M, Seip B, Aasen S, Kordal M, Hoff G, Aabakken L. Carbon dioxide insufflation for more comfortable endoscopic retrograde cholangiopancreatography: a randomized, controlled, double-blind trial. Endoscopy. 2007;39:58–64. doi: 10.1055/s-2006-945036. [DOI] [PubMed] [Google Scholar]
- 21.Hirai F, Matsui T, Yao K, Sou S, Seki T. Efficacy of carbon dioxide insufflation in endoscopic balloon dilation therapy by using double balloon endoscopy. Gastrointest Endosc. 2007;66:S26–S29. doi: 10.1016/j.gie.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 22.Grassini M, Verna C, Battaglia E, Niola P, Navino M, Bassotti G. Education improves colonoscopy appropriateness. Gastrointest Endosc. 2008;67:88–93. doi: 10.1016/j.gie.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 23.Rex DK, Chen SC, Overhiser AJ. Colonoscopy technique in consecutive patients referred for prior incomplete colonoscopy. Clin Gastroenterol Hepatol. 2007;5:879–883. doi: 10.1016/j.cgh.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 24.Marshall JB, Perez RA, Madsen RW. Usefulness of a pediatric colonoscope for routine colonoscopy in women who have undergone hysterectomy. Gastrointest Endosc. 2002;55:838–841. doi: 10.1067/mge.2002.124562. [DOI] [PubMed] [Google Scholar]
- 25.Brooker JC, Saunders BP, Shah SG, Williams CB. A new variable stiffness colonoscope makes colonoscopy easier: a randomised controlled trial. Gut. 2000;46:801–805. doi: 10.1136/gut.46.6.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kozarek RA, Botoman VA, Patterson DJ. Prospective evaluation of a small caliber upper endoscope for colonoscopy after unsuccessful standard examination. Gastrointest Endosc. 1989;35:333–335. doi: 10.1016/s0016-5107(89)72804-2. [DOI] [PubMed] [Google Scholar]
- 27.Kaltenbach T, Soetikno R, Friedland S. Use of a double balloon enteroscope facilitates caecal intubation after incomplete colonoscopy with a standard colonoscope. Dig Liver Dis. 2006;38:921–925. doi: 10.1016/j.dld.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 28.Kondo S, Yamaji Y, Watabe H, Yamada A, Sugimoto T, Ohta M, Ogura K, Okamoto M, Yoshida H, Kawabe T, et al. A randomized controlled trial evaluating the usefulness of a transparent hood attached to the tip of the colonoscope. Am J Gastroenterol. 2007;102:75–81. doi: 10.1111/j.1572-0241.2006.00897.x. [DOI] [PubMed] [Google Scholar]
- 29.Shumaker DA, Zaman A, Katon RM. Use of a variable-stiffness colonoscope allows completion of colonoscopy after failure with the standard adult colonoscope. Endoscopy. 2002;34:711–714. doi: 10.1055/s-2002-33442. [DOI] [PubMed] [Google Scholar]
- 30.Rex DK. Effect of variable stiffness colonoscopes on cecal intubation times for routine colonoscopy by an experienced examiner in sedated patients. Endoscopy. 2001;33:60–64. doi: 10.1055/s-2001-11179. [DOI] [PubMed] [Google Scholar]
- 31.Shumaker DA, Zaman A, Katon RM. A randomized controlled trial in a training institution comparing a pediatric variable stiffness colonoscope, a pediatric colonoscope, and an adult colonoscope. Gastrointest Endosc. 2002;55:172–179. doi: 10.1067/mge.2002.121189. [DOI] [PubMed] [Google Scholar]
- 32.Kaffes AJ, Mishra A, Ding SL, Hope R, Williams SJ, Gillespie PE, Bourke MJ. A prospective trial of variable stiffness pediatric vs. standard instrument colonoscopy. Gastrointest Endosc. 2003;58:685–689. doi: 10.1016/s0016-5107(03)02017-0. [DOI] [PubMed] [Google Scholar]
- 33.Yörük G, Aksöz K, Unsal B, Buyraç Z, Buran T, Yazicioğlu N, Yildiz C, Yalçin HC. Colonoscopy without sedation. Turk J Gastroenterol. 2003;14:59–63. [PubMed] [Google Scholar]
- 34.Ladas SD. Factors predicting the possibility of conducting colonoscopy without sedation. Endoscopy. 2000;32:688–692. doi: 10.1055/s-2000-9027. [DOI] [PubMed] [Google Scholar]
- 35.Konishi K, Kaneko K, Kurahashi T, Yamamoto T, Kushima M, Kanda A, Tajiri H, Mitamura K. A comparison of magnifying and nonmagnifying colonoscopy for diagnosis of colorectal polyps: A prospective study. Gastrointest Endosc. 2003;57:48–53. doi: 10.1067/mge.2003.31. [DOI] [PubMed] [Google Scholar]
- 36.Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Sedation-free colonoscopy. Dis Colon Rectum. 2005;48:855–859. doi: 10.1007/s10350-004-0860-0. [DOI] [PubMed] [Google Scholar]