SYNOPSIS
Objectives
We inventoried and reviewed the birth and fetal death certificates of all 50 U.S. states to identify nonstandard data items that are environmentally relevant, inexpensive to collect, and might enhance environmental public health tracking.
Methods
We obtained online or requested by mail or telephone the birth certificate and fetal death record forms or formats from each state. Every state data element was compared to the 2003 standards promulgated by the National Center for Health Statistics to identify any items that are not included on the standard. We then evaluated these items for their utility in environmentally related analyses.
Results
We found three data fields of potential interest. First, although every state included residence of mother at time of delivery on the birth certificate, only four states collected information on how long the mother had lived there. This item may be useful in that it could be used to assess and reduce misclassification of environmental exposures among women during pregnancy. Second, we found that father's address was listed on the birth certificates of eight states. This data field may be useful for defining paternal environmental exposures, especially in cases where the parents do not live together. Third, parental occupation was listed on the birth certificates of 15 states and may be useful for defining parental workplace exposures. Our findings were similar for fetal death records.
Conclusion
If these data elements are accurate and well-reported, their addition to birth, fetal death, and other health records may aid in environmental public health tracking.
Environmental public health tracking (EPHT) is the ongoing collection, integration, analysis, and dissemination of data from environmental hazard monitoring, human exposure tracking, and health effect surveillance.1 In 2000, a Pew Environmental Health Commission Report proposed that a national network be established to track priority chronic diseases and possible environmental risk factors, and that information from this network be used to identify high-risk populations, examine health concerns at the state level, assess linkages between these diseases and environmental factors, and begin to develop and implement prevention strategies.2
In response, the Centers for Disease Control and Prevention (CDC) created a program in 2002 to implement EPHT and develop the national network. Priority environmental hazards included criteria and hazardous air pollutants, drinking water contaminants, and lead. Priority health conditions included asthma, cancer, birth defects, and other adverse reproductive events.3 Adverse reproductive events have an advantage over other indicators, such as cancer incidence, in that they may show evidence for environmental effects more readily, given the relatively short and recent biologically relevant window for exposure. The ultimate goal of EPHT is to promote disease prevention by integrating knowledge of the environmental factors that affect health into research, surveillance, and practice.4
While still early in its development, the current EPHT surveillance system depends on birth, fetal death and death certificates, cancer registry records, hospital billing data, emergency department visit records, and other health data routinely collected and made available by health departments, registries, and other institutions. Some of these records have long been used by public health agencies to monitor on an ongoing basis measures of health status and outcomes, and health indicators such as low birthweight, preterm birth, and late fetal and perinatal mortality.5,6. They have also been used to study the associations between environmental exposures and adverse reproductive outcomes.7–11
The content, format, and standardization of birth and fetal death certificates, together with other vital records, are reviewed periodically by the National Center for Health Statistics (NCHS) to help promote a consistent, reliable, and usable source of information nationwide. NCHS works in collaboration with the National Association for Public Health Statistics and Information Systems, which also helps develop standards and principles to effectively administer public health statistics and information systems. The focus has been on sociodemographic risk factors and medical and pregnancy histories, but not on items that may be of environmental significance. Most recently, NCHS convened a panel of expert consultants to assess the usefulness of existing data items, identify unmet needs, and make recommendations for change.12 As a result, substantial revisions were made to the 2003 version of the birth and fetal death certificates, which are currently being promulgated by NCHS as the new standards.13
In part, because the focus has been on traditional health concerns rather than possible environmental etiology, we know of no evaluation of the data items on birth or fetal death records for their environmental health relevance. To address that issue, we inventoried and reviewed existing data elements on the birth and fetal death certificates of all 50 U.S. states relative to the 2003 standard to identify nonstandard data items that are environmentally relevant, inexpensive to collect, and might enhance EPHT analyses.
METHODS
We employed a multistep procedure to obtain the state birth and fetal death certificates. First, we searched the website of each state department of health and found that 10 states had their birth and fetal death certificates available online. We sent a personally signed letter on university letterhead addressed to the vital records registrar of the remaining 40 states explaining the purpose of the investigation and requesting a copy of the birth and fetal death certificate, file layout, or data dictionary. Twelve states responded to the letter with the requested information within two weeks; telephone calls were made to the other 28 states. Five states sent the information soon after the phone call, while 23 required additional follow-up. In most cases, this follow-up involved identifying the specific person within the vital records unit who was responsible for data processing requests and resending or faxing the letter to legitimize the request. Upon receipt of this information, most of the health departments were very willing to assist. Only three cases required further action. These measures included recruiting the aid of a CDC staff member who worked as a state liaison and requesting assistance from EPHT staff in selected states to gather the information. We obtained records from 49 states within six months, and that of the final state two months later.
We summarized the results in a matrix, which included in each row the data elements and in each column the individual states. We made a notation in each cell indicating whether the element was synonymous with the standard, different from the standard but provided similar information, or not included on the standard.
RESULTS
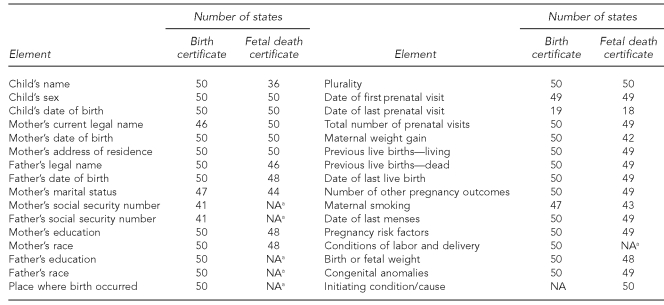
Not all states have yet converted to the 2003 standards, but as shown in Table 1, many of the data elements for the 2003 standard are included on the state certificates of birth or fetal death records (e.g., mother's name and other identifying information). Medical and health information from the standards also is included routinely on the state certificates and records including prenatal care, pregnancy history, and characteristics of the labor and delivery. (A more detailed version of Table 1 is available from the authors.)
Table 1.
Number of U.S. states with selected data elements from the 2003 U.S. standard certificate of birth or record of fetal death
aElement not included on standard certificate
NA = not available
Every state included mother's city or town of residence at delivery on the birth certificate (Table 1), and 46 states also included street address. Although it was not included on the standard, Connecticut, Maine, Missouri, and Washington also included a birth certificate element reporting how long the mother has lived at her current residence or in her present town at time of birth (Table 2).
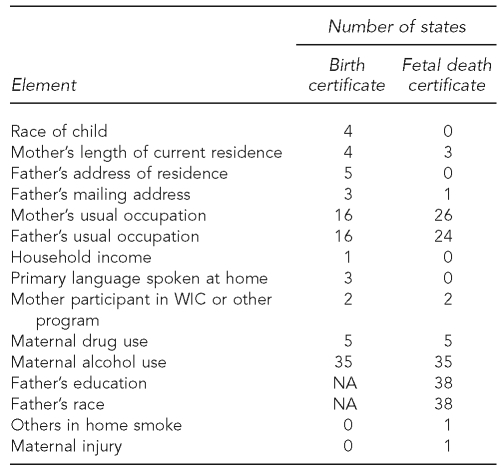
Table 2.
Number of U.S. states with selected data elements not included on U.S. standard certificate of birth or record of fetal death
WIC = Women, Infants and Children
NA = not available
Father's residence was not a data element on the standard birth certificate but was included on the certificates of New York and South Dakota (Table 2). It was also listed in the Paternity Acknowledgement section of the certificates of Florida, Massachusetts, and Rhode Island. New Jersey, Texas, and Vermont included father's mailing address only, although mailing address is not the same as location.
Table 2 also indicates that although parental occupation was not included on the 2003 standard, it was listed on the birth certificates of 16 states. Individual states also included other data elements not listed on the standard certificate. For example, Tennessee requested household income, and California and Missouri asked about whether the mother participated in the Women, Infants and Children; Aid to Families with Dependent Children; Medicaid; or Food Stamps programs. Thirty-five states inquired about maternal alcohol use and five asked about maternal drug use during pregnancy.
In general, the results for the fetal death certificates were similar to those for the birth certificates (Tables 1 and 2). Maine, Missouri, and Washington, for example, included length of mother's residence at current address or town. New Jersey included an element regarding father's mailing address. Interestingly, occupation was more commonly asked on the fetal death certificate, with 26 states asking about mother's occupation and 24 states asking about father's occupation, compared with 15 states for the birth certificate. The fetal death certificates also included a few elements not included on the birth certificates. For instance, Massachusetts had elements regarding whether the fetal death was related to a maternal injury, including work-related injuries, and Michigan had an item regarding whether others in the household smoke.
DISCUSSION
Regarding mother's residence, geocoded street address has been a key element in defining maternal exposures such as air pollution in studies of adverse reproductive outcomes.11,14,15 Automated geocoding methods for residential locations usually introduce some degree of positional error, especially in rural areas,16 but the impact of this error is often minimized in environmental studies, as the exposure data typically are regional rather than house/address-specific. This element is useful in determining whether the mother lived at the same address throughout her pregnancy. Using such information in analytic studies would help reduce the misclassification of exposure that may occur when only maternal address at birth is available, as studies suggest that 20% to 30% of all mothers move during pregnancy.17–20 In addition, length of residence may assist in measuring duration of exposure to environmental contaminants.
Father's residential location may be useful in determining paternal environmental exposures in cases in which the parents do not live together, which in New York is estimated to be approximately 19% of all births (Personal communication, P. Herztfeld, New York State Department of Health, May 2008). Exposure at the paternal residence also is relevant to reproductive and developmental abnormalities, as these outcomes have been associated with paternal exposures to therapeutic and recreational drugs, to chemicals in the workplace and environment, and to ionizing radiation.21 For germ cell mutations, however, the relevant period of exposure for the father is the recent past but for the mother is her lifetime.22 Mother's and father's occupation is of interest for EPHT, both as a source of workplace exposures23–25 and as a potential confounder for environmental exposures. Other potential confounders include lifestyle factors such as maternal smoking and alcohol consumption.
The accuracy and completeness of these data elements must be evaluated before they may be recommended for EPHT. Previous studies indicate that the sensitivity and specificity of birth certificate data vary considerably by item.26 For example, birthweight, delivery method, demographic characteristics, Apgar score, and insurance are usually accurately reported, while tobacco and alcohol use, medical risk factors, obstetric procedures, and complications of labor and delivery tend to be underreported.27,28 In another study, missing data for specific elements ranged from 0% to 24%.29
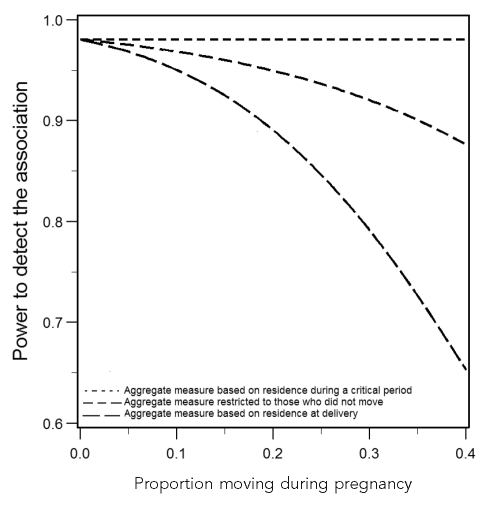
Even if the data are of sufficient quality and completeness, research is needed to evaluate the value of these data elements for studies including environmental etiology. To help assess the ability of a study to detect an association when an area-wide measure of exposure is based on residence at time of delivery rather than on residence at the biologically relevant window for exposure (e.g., first trimester for certain toxicants), we performed a series of numerical analyses based on the formulation of Thompson and Wartenberg.30 We compared the power to detect an association when the exposure was: (1) based on maternal residence during the critical period, (2) restricted only to those women who did not move during pregnancy, or (3) based on maternal residence at time of delivery.
As shown in the Figure, the numerical results demonstrated a substantial loss of power due to using residence at delivery rather than residence at the biologically relevant period. The results also demonstrated that, in the absence of information on the specific location from which individuals have moved, statistical power can be enhanced by excluding from the analysis those individuals who are known to have moved. This increase in power can be achieved because the loss in sample size is outweighed by the reduction of exposure misclassification (assuming no temporal variation in exposure at the residence location at time of birth). These results are consistent with the data from Ritz et al.,31 which showed stronger associations between preterm delivery and first trimester exposure to carbon monoxide when their analyses were restricted to women who did not move during pregnancy. To further evaluate this issue, we are conducting a study using birth certificate data from Washington regarding how long the mother lived at her current address to assess whether mothers who move during pregnancy differ from those who do not move, in terms of demographic characteristics, medical history, and lifestyle factors, and the extent to which residential mobility results in environmental exposure misclassification (Unpublished data, Brown S, Hoskins R, Wartenberg D. Maternal mobility and predictors of maternal mobility among pregnant women in Washington State, 1999–2001. 2008).
Figure.
Effect of residential mobility on the power of environmental studies
aThe number of geographic areas is 27, with the prevalence of a binary exposure ranging from 0.26 to 0.74, and a sample size of 25,000 in each area. It is assumed that the occurrence of the outcome is 85 per 1,000 for exposed individuals and 75 per 1,000 for unexposed individuals—values that are consistent with the frequency of low birthweight in the population and with the small magnitude of effect that is typical in environmental studies. Mobility is assumed to be random with respect to individual-level and area-wide measures of exposure.
The addition of data elements (e.g., length of maternal residence) to birth and fetal death certificates may be a useful and cost-effective means of enhancing the ability of state health departments to track adverse reproductive outcomes and assess associations with environmental risk factors, if their accuracy and completeness can be demonstrated and they are shown to reduce misclassification of exposure. Maternal residential history is also relevant for other health endpoints such as childhood cancers, particularly with respect to current controversies on environmental etiology.32–34 Length of patient residence may be another useful addition to hospital discharge and emergency department records for the surveillance of acute events, such as asthma exacerbation and myocardial infarction.
CONCLUSION
Our inventory and review of these records indicated that maternal length of residence at current address or town is probably the nonstandard element of greatest relevance to EPHT. Its use in etiologic research could reduce misclassification of maternal environmental exposures during pregnancy—a common source of error in studies of adverse reproductive outcomes—and help to improve statistical power. Father's address may also be of relevance in cases in which the parents do not live together, given the role of paternal environmental exposures on birthweight and other pregnancy outcomes. Parental occupation may be of interest in assessing workplace exposures, and other unusual elements pertaining to sociodemographic and lifestyle factors may be useful as potential confounders. If these data elements can be reported completely and accurately, then their addition to birth and fetal death certificates and other health records may be a valuable and cost-effective method for state health departments to improve their capacity to conduct EPHT.
Footnotes
This work was funded, in part, by cooperative agreement U19 EH000102 from the National Center for Environmental Health, Centers for Disease Control and Prevention.
REFERENCES
- 1.McGeehin MA, Qualters JR, Niskar AS. National Environmental Public Health Tracking Program: bridging the information gap. Environ Health Perspect. 2004;112:1409–13. doi: 10.1289/ehp.7144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baltimore: Pew Charitable Trusts; 2000. America's environmental health gap: why the country needs a nationwide health tracking network: technical report. Pew Environmental Health Commission. [Google Scholar]
- 3.Litt J, Tran N, Malecki KC, Neff R, Resnick B, Burke T. Identifying priority health conditions, environmental data, and infrastructure needs: a synopsis of the Pew Environmental Health Tracking Project. Environ Health Perspect. 2004;112:1414–8. doi: 10.1289/ehp.7147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kyle AD, Balmes JR, Buffler PA, Lee PR. Integrating research, surveillance, and practice in environmental public health tracking. Environ Health Perspect. 2006;114:980–4. doi: 10.1289/ehp.8735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin, JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S. Births: final data for 2004. Natl Vital Stat Rep. 2006 Sep 29;55:1–102. [PubMed] [Google Scholar]
- 6.MacDorman MF, Hoyert DL, Martin JA, Munson ML, Hamilton BE. Fetal and perinatal mortality, United States, 2003. Natl Vital Stat Rep. 2007 Feb 21;55:1–18. [PubMed] [Google Scholar]
- 7.Wartenberg D, Agamennone VJ, Ozonoff D, Berry RJ. A microcomputer-based vital records database with interactive graphic assessment for states and localities. Am J Public Health. 1989;79:1531–6. doi: 10.2105/ajph.79.11.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berry M, Bove F. Birth weight reduction associated with residence near a hazardous waste landfill. Environ Health Perspect. 1997;105:856–61. doi: 10.1289/ehp.97105856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sonnenfeld N, Hertz-Picciotto I, Kaye WE. Tetracholoroethylene in drinking water and birth outcomes at the US Marine Corps Base at Camp Lejeune, North Carolina. Am J Epidemiol. 2001;154:902–8. doi: 10.1093/aje/154.10.902. [DOI] [PubMed] [Google Scholar]
- 10.Wilhelm M, Ritz B. Residential proximity to traffic and adverse birth outcomes in Los Angeles County, California, 1994–1996. Environ Health Perspect. 2003;111:207–16. doi: 10.1289/ehp.5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sram RJ, Binkova B, Dejmek J, Bobak M. Ambient air pollution and pregnancy outcomes: a review of the literature. Environ Health Perspect. 2005;113:375–82. doi: 10.1289/ehp.6362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics Division of Vital Statistics (US) Report of the Panel to Evaluate the U.S. Standard Certificates. Hyattsville (MD): National Center for Health Statistics; 2000. [Google Scholar]
- 13.National Center for Health Statistics, Division of Vital Statistics (US) 2003 revisions of the U.S. standard certificates of live birth and death and the fetal death report. Hyattsville (MD): National Center for Health Statistics. 2009. [cited 2009 Jun 16]. Also available from: URL: http://www.cdc.gov/nchs/vital_certs_rev.htm.
- 14.Ritz B, Wilhelm M, Zhao Y. Air pollution and infant death in southern California. Pediatrics. 2006;118:493–502. doi: 10.1542/peds.2006-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maisonet M, Correa A, Misra D, Jaakkola JJ. A review of the literature on the effects of ambient air pollution on fetal growth. Environ Res. 2004;95:106–15. doi: 10.1016/j.envres.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Cayo MR, Talbot TO. Positional error of automated geocoding of residential addresses. Int J Health Geogr. 2003;2:10. doi: 10.1186/1476-072X-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khoury MJ, Stewart W, Weinstein A, Panny S, Lindsay P, Eisenberg M. Residential mobility during pregnancy: implications for environmental teratogenesis. J Clin Epidemiol. 1988;41:15–20. doi: 10.1016/0895-4356(88)90004-2. [DOI] [PubMed] [Google Scholar]
- 18.Shaw GM, Halinka Malcoe L. Residential mobility during pregnancy for mothers of infants with or without congenital cardiac anomalies. Arch Environ Health. 1991;46:310–2. doi: 10.1080/00039896.1992.9938355. [DOI] [PubMed] [Google Scholar]
- 19.Fell DB, Dodds L, King WD. Residential mobility during pregnancy. Paediatr Perinat Epidemiol. 2004;18:408–14. doi: 10.1111/j.1365-3016.2004.00580.x. [DOI] [PubMed] [Google Scholar]
- 20.Canfield MA, Ramadhani TA, Langlois PH, Waller DK. Residential mobility patterns and exposure misclassification in epidemiologic studies of birth defects. J Expo Sci Environ Epidemiol. 2006;16:538–43. doi: 10.1038/sj.jes.7500501. [DOI] [PubMed] [Google Scholar]
- 21.Friedler G. Paternal exposures: impact on reproductive and developmental outcome. An overview. Pharmacol Biochem Behav. 1996;55:691–700. doi: 10.1016/s0091-3057(96)00286-9. [DOI] [PubMed] [Google Scholar]
- 22.Aitken RJ, De Iuliis GN. Value of DNA integrity assays for fertility evaluation. Soc Reprod Fertil Suppl. 2007;65:81–92. [PubMed] [Google Scholar]
- 23.Fransman W, Roeleveld N, Peelen S, De Kort W, Kromhout H, Heederik D. Nurses with dermal exposure to antineoplastic drugs: reproductive outcomes. Epidemiology. 2007;18:112–9. doi: 10.1097/01.ede.0000246827.44093.c1. [DOI] [PubMed] [Google Scholar]
- 24.Jurewicz J, Hanke W, Makowiec-Dabrowska T, Sobala W. Exposure to pesticides and heavy work in greenhouses during pregnancy: does it affect birth weight? Int Arch Occup Environ Health. 2005;78:418–26. doi: 10.1007/s00420-005-0614-x. [DOI] [PubMed] [Google Scholar]
- 25.Lin S, Hwang SA, Marshall EG, Marion D. Does paternal occupational lead exposure increase the risks of low birth weight or prematurity? Am J Epidemiol. 1998;148:173–81. doi: 10.1093/oxfordjournals.aje.a009621. [DOI] [PubMed] [Google Scholar]
- 26.Roohan PJ, Josberger RE, Acar J, Dabir P, Feder HM, Gagliano PJ. Validation of birth certificate data in New York State. J Community Health. 2003;28:335–46. doi: 10.1023/a:1025492512915. [DOI] [PubMed] [Google Scholar]
- 27.Reichman NE, Hade EM. Validation of birth certificate data. A study of women in New Jersey's HealthStart program. Ann Epidemiol. 2001;11:186–93. doi: 10.1016/s1047-2797(00)00209-x. [DOI] [PubMed] [Google Scholar]
- 28.Northam S, Knapp TR. The reliability and validity of birth certificates. J Obstet Gynecol Neonatal Nurs. 2006;35:3–12. doi: 10.1111/j.1552-6909.2006.00016.x. [DOI] [PubMed] [Google Scholar]
- 29.Dobie SA, Baldwin LM, Rosenblatt RA, Fordyce MA, Andrilla CH, Hart LG. How well do birth certificates describe the pregnancies they report? The Washington State experience with low-risk pregnancies. Matern Child Health J. 1998;2:145–54. doi: 10.1023/a:1021875026135. [DOI] [PubMed] [Google Scholar]
- 30.Thompson WD, Wartenberg D. Additive versus multiplicative models in ecologic regression. Stochast Environ Res Risk Assess. 2007;21:635–46. [Google Scholar]
- 31.Ritz B, Wilhelm M, Hoggatt KJ, Ghosh JKC. Ambient air pollution and preterm birth in the Environment and Pregnancy Outcomes Study at the University of California, Los Angeles. Am J Epidemiol. 2007;166:1045–52. doi: 10.1093/aje/kwm181. [DOI] [PubMed] [Google Scholar]
- 32.Kinlen L. Evidence for an infective cause of childhood leukemia: comparison of a Scottish new town with nuclear reprocessing sites in Britain. Lancet. 1988;2:1323–7. doi: 10.1016/s0140-6736(88)90867-7. [DOI] [PubMed] [Google Scholar]
- 33.Smith MA, Simon R, Strickler HD, McQuillan G, Ries LA, Linet MS. Evidence that childhood acute lymphoblastic leukemia is associated with an infectious agent linked to hygiene conditions. Cancer Causes Control. 1998;9:285–98. doi: 10.1023/a:1008873103921. [DOI] [PubMed] [Google Scholar]
- 34.Greaves MF, Alexander FE. An infectious etiology for common acute lymphoblastic leukemia in childhood? Leukemia. 1993;7:349–60. [PubMed] [Google Scholar]