SYNOPSIS
Objectives
Asian American and Pacific Islanders (AAPIs) historically have faced multiple social and racial/ethnic health disparities in the United States. We gathered national-level health-care data on AAPIs and examined medically underserved health service areas for them.
Methods
We used 2000 U.S. Census data and the Bureau of Primary Health Care (BPHC) 2004 dataset for primary care physician full-time equivalents per 1,000 population, as well as AAPI population, AAPI poverty, and AAPI limited English proficiency, to develop an index of medically underserved AAPI counties (MUACs). The index identifies U.S. counties that do not adequately serve AAPIs.
Results
We identified 266 counties of medically underserved health service areas for AAPIs across the nation, representing 12% of all U.S. counties. One hundred thirty-eight (52%) MUACs were not designated as BPHC medically underserved counties. Of these counties, 20 (14%) had an AAPI population of at least 10,000, and 29 (21%) had an AAPI population of at least 5,000.
Conclusion
This project complements federal efforts to identify medically underserved health service areas and identifies U.S. counties that need new or expanded health services for medically underserved AAPIs.
Asian American and Pacific Islanders (AAPIs) are one of the fastest-growing racial/ethnic groups in the U.S., and currently account for 4.0% (12.5 million) of the total U.S. population.1 By 2050, AAPIs are projected to account for 11.0% (41 million) of the total U.S. population.2–4 However, very few AAPI health studies exist to date; AAPI health studies account for only 0.2% of federal health-related grants (1986–2000) and very few MEDLINE articles (1966–2000) reference AAPIs.5
AAPIs are socioeconomically diverse and represent more than 49 ethnic groups with more than 100 languages. AAPIs are also socioeconomically and linguistically disadvantaged compared with the non-Hispanic white population, with 14% vs. 8% poverty, 18% vs. 11% uninsured, and 50% vs. 2% limited English proficiency (LEP) rates nationally.2
AAPIs experience multiple health disparities, includ-ing higher prevalence rates of tuberculosis and hepatitis B, than other racial/ethnic groups.6–9 They are the only racial/ethnic group in which cancer is the leading cause of death, with higher cancer mortality rates among AAPIs than among other racial/ethnic groups.10–12 Despite these statistics, AAPIs are often portrayed as a “model minority” (i.e., an intelligent, hardworking group that has overcome barriers to social mobility and wellness).13 Existing health data on AAPIs are limited and often represent the group as a whole, masking the documented differences and disparities among the numerous AAPI subgroups.14
The rapidly growing AAPI population—particularly underserved AAPIs served by America's community health centers15–17—combined with scarcity of data presents a situation of increasing public health concern. In particular, there are currently no national data regarding AAPI service areas in our primary care system to support community health centers (CHCs) and to expand service areas to underserved AAPI counties. CHCs provide high-quality, cost-effective, and culturally appropriate primary and preventive health care to an increasing number of underserved patients—including nearly 450,000 AAPIs18—regardless of insurance status or ability to pay. An expansion of health centers is necessary to provide access to the rapidly growing number of AAPIs17 in many existing and new underserved areas. Identifying these areas of underserved AAPIs is essential for health centers to guide their expansion, as well as for grant writing, program planning, and allocating appropriate government resources for health-care delivery to AAPIs.
Since 1976, the U.S. Department of Health and Human Services (HHS) has used an index to identify medically underserved areas (MUAs) to allocate funding for public health systems, such as CHCs, in areas of greatest need. MUAs are generally defined by the federal government to include areas with a demonstrated shortage of personal health-care services. For MUAs, a composite index of four need indicators is compiled and compared with national means to determine an area's level of medical underservice. An index of medical underservice score is calculated based on the individual area's poverty rate, infant mortality rate, percentage of population aged 65 years and older, and number of primary care physicians per 1,000 population (P-to-1,000P ratio).19,20 The criteria for an MUA served as a starting point for developing our medically underserved AAPI county (MUAC) index, an index that is appropriate and relevant for identifying MUAs for AAPIs.
Recently, there has been a proposed rule for the designation of medically underserved populations and health professional shortage areas, with a new index of 12 indicators to assess federal health center designations,21,22 which has been a point of concern and contention for safety net health centers across the U.S. Preliminary assessments of the new index's impact on existing federally qualified health centers suggests that this index will adversely impact CHCs, leading to about 20% of CHCs losing their federal health center designation and associated funding.23 Closer examination of the new index's potential impact on AAPIs suggests that neither the old nor the new indices use key indicators that adequately capture medically underserved service areas for AAPI populations (Unpublished letter from Jeffrey Caballero, Association of Asian Pacific Community Health Organizations, to Andy Jordan, Health Resources and Services Administration, Department of Health and Human Services, 2008 May 19).
This study provides a national assessment at the county level to identify where AAPIs lack access to primary health care. Along with other studies investigating health-care designation methodologies,24–28 this analysis could help government agencies and public health workers create new health center infrastructures in areas with health facility needs. The study also contributes to presidential and congressional initiatives to improve the participation of underserved AAPIs in federal programs and to expand the number of people served by health centers.29,30
METHODS
Data sources
We conducted an AAPI health literature and data search to assess relevant AAPI-specific data and indicators.2,7,18,19 Our proposed MUAC index is new and includes the following indicators: AAPI population, AAPI poverty, AAPI LEP, and P-to-1,000P ratio, obtained from national public datasets. These include the U.S. Census 2000 Summary File 3 for the poverty and LEP data, U.S. Census 2000 Summary File 1 for the population data, and the Bureau of Primary Health Care (BPHC) 2004 dataset for the P-to-1,000P ratio data.2,19 The definition of LEP uses the U.S. Census categories of ability to speak, read, and write English less than “very well,” as similarly defined by the U.S. Census. The BPHC's concept of MUAs was developed to determine federal budgetary allocations for primary care services; it uses the following definition and weights:
MUA index (with minimum score of 0.0 and maximum score of 1.0) = 0.25 × % poverty + 0.20 × population aged 65 years and older + 0.26 × infant mortality rate + 0.29 × P-to-1,000P ratio.19
The BPHC developed weights according to the indicators' pertinence in identifying medical underservice, as defined by an interdisciplinary group of experts in health care and measurement, who rated them in order of importance to determine medical underservice.31 Of 3,141 counties in the U.S., the available county-level data for AAPI population, AAPI poverty, AAPI LEP, and P-to-1,000P ratio were 3,141; 2,999; 3,005; and 2,301 county cases, respectively. All cases were merged by county level, and 2,191 total county cases contained county-level data for all four indicators. We used these final 2,191 county cases for our analyses.
MUAC index development and analysis
There are several differences between the MUAC and the MUA indexes. The term “MUA” applies to the general population and does not include criteria that are critical for AAPIs, such as LEP. Data for infant mortality rates are unavailable for the AAPI population nationally at the county level and, therefore, are unavailable for use in the MUAC index. We assessed total AAPI population rather than the AAPI population aged 65 years and older, as AAPI populations account for only 4% of the total U.S. population and assessing only this advanced-age population would not adequately capture underserved AAPI concentrations across the U.S.3 In addition, more than two-thirds of AAPIs are foreign-born, and they tend to be younger than the general U.S. population.1
Finally, instead of giving equal weight to each indicator, we assigned varying weights that more adequately reflect the current U.S. population health contexts, with AAPI poverty assigned the most weight followed by AAPI LEP, AAPI population, and P-to-1,000P ratio. This weighting method ensured that the indicators that were more critical in predicting health status for underserved AAPIs were given more magnitude.
First, we assigned percentage of AAPI poverty at the highest weight of 0.40/1.00 given the evidence that it represents the most important determinant of population health in relation to the other three indicators. Poverty has been a global standard in measuring access barriers to needed health resources and is highly associated with access and health utilization.32 AAPIs living in poverty, in particular, have been a rapidly growing, neglected group because of the model minority myth13 and the lack of AAPI data.5
The percentage of AAPIs who have LEP was assigned the next-highest weight of 0.25. LEP has represented one of the greatest barriers to health-care access for AAPIs.33 Communication challenges due to language barriers are a common reason for AAPIs to avoid health services.34 In addition, approximately 35% of AAPIs live in linguistically isolated households (defined as a household in which no one aged 14 years or older can speak English “very well”). Disaggregating these data reveals more significant numbers: 61% of Hmong, 56% of Cambodian, 44% of Vietnamese, 41% of Korean, and 40% of Chinese households are linguistically isolated.2 LEP patients are also less likely to be given follow-up appointments, to take prescribed medication,35 to appear for follow-up appointments,34 and to participate in health-care programs for which they are eligible.36–39
We assigned percentage AAPI population a weight of 0.20. In general, regions with the highest concentrations of AAPIs also tend to be regions with the most ethnic enclaves where many underserved AAPIs reside.40–42
In contrast with the federal MUA index, we assigned the P-to-1,000P ratio variable with the lowest weight of 0.15 because it is not an AAPI-specific indicator. Adequate provider supply has been shown to be an important factor in morbidity and mortality.43 In addition, the fewer providers there are in an area, the less likely a person will be to have access to health-care services.
Overall, the MUAC index is designed to provide a method appropriately tailored to capture the underserved AAPI population. The final index is as follows:
MUAC index = 0.40 × % AAPI poverty + 0.25 × % AAPI LEP + 0.20 × % AAPI population + 0.15 × P-to-1,000P ratio
After finalizing the index, we applied the MUAC index to identify the AAPI underserved counties. An additional staff person independently downloaded the data and double-checked a random sample of 1% of the data from each variable. We merged data from the U.S. Census and BPHC using the geographic county -variable. We eliminated county cases without all four data points (n=950) for each of the indicators, which left 2,191 county cases for our final analysis. We conducted an analysis of the 950 counties that were eliminated and found that the mean AAPI population in these counties was less than 1% and reflects the U.S. Census policy of reporting data only for areas with more than 100 people (to protect people's confidentiality). It also reflects the broad unavailability of BPHC provider supply data. The means for each of the indicators of the excluded counties were 0.7% AAPI population (n=950), 14.6% AAPI poverty (n=808), 30.8% AAPI LEP (n=814), and 0.2% P-to-1,000P ratio (n=110). The states with the most excluded counties were Georgia (n=80) and Missouri (n=79).
We determined the total underserved standard score for the MUAC index by summing individual standard scores or weights for each of the four indicators. The percentage AAPI poverty underserved standard score (11.4) was based on the U.S. Census guidelines, which define a poverty area as one in which at least 20% of the population lives in poverty.2 The percentage AAPI LEP underserved standard score (15.9) was defined as three standard deviations (SDs) above the percentage LEP mean for the total U.S. county population (15.1%). The percentage AAPI population standard weighted score (5.5) was defined as one SD above the mean for percentage total U.S. minority or nonwhite population (36.5%). The P-to-1,000P ratio standard score (12.8) was based on HHS guidelines19 stating that a ratio of 1:3,500 or greater is defined as an underserved primary care service region. We used the designated weights for the four variables and calculated the underserved standard weighted scores for these variables. The sum of these underserved standard weighted scores provided the total MUAC index standard score (Table 1) to make comparisons of medically underserved AAPI status across counties. The final MUAC index scale ranged from 0 to 100 (where 0 = most underserved and 100 = least underserved).
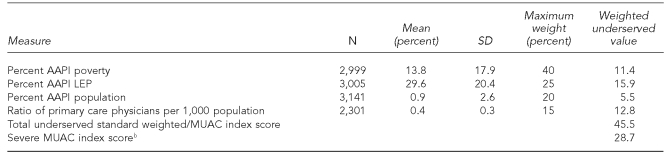
Table 1.
Indicators and underserved standard scores for defining MUAC indexa
aData sources: Census Bureau (US). Projections of the resident population by age, sex, race, and Hispanic origin: 1999 to 2100. Washington: Census Bureau; 2000. Also available from: URL: http://www.census.gov/population/projections/nation/detail/d2041_50.pdf [cited 2007 Nov 30] and Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions (US). Guidelines for medically underserved area and population designation [cited 2007 Mar 14]. Available from: URL: http://bhpr.hrsa.gov/shortage/muaguide.htm
bWe determined the severe MUAC index score by subtracting the MUAC SD (16.7) from the MUAC index score (45.5).
MUAC = medically underserved AAPI county
SD = standard deviation
AAPI = Asian American and Pacific Islander
LEP = limited English proficiency
The last column in Table 1 shows the weighted underserved value for each variable. These numbers determine the underserved area status across counties for each indicator. For example, if a county has a P-to-1,000P ratio weighted value less than 12.75 (indicating having less than one primary care physician per 3,500 population), then the county would be considered an underserved area in terms of the number of primary care physicians serving the county population. A mean of 13.8% of AAPIs across counties nationally were living in poverty. The mean P-to-1,000P ratio was 0.40, which is equivalent to about one primary care physician for every 2,500 population.
The total of these four weighted underserved values provided the MUAC index score of 45.5. Thus, any county nationally with a score equal to or below that number would be defined as an AAPI MUA. We also identified severe MUACs based on an MUAC index score of 28.7—one SD below the MUAC index score. The mean MUAC index score across counties nationally was 67.1 (SD=16.7).
To facilitate visual presentation, we used geographic information system software to display the MUACs. The software's ability to display complex visual data facilitated the analysis of relations of health variables, which are useful for understanding and monitoring health care.44
We identified the top five counties with both the lowest MUAC index scores and the largest AAPI populations. We also compared our MUACs with those identified by the national BPHC MUA data (described previously) and the unserved counties developed by the National Association of Community Health Centers. Unserved counties are defined as those with more than 35.3% of residents living below 200% of the federal poverty level and lacking a CHC.45
RESULTS
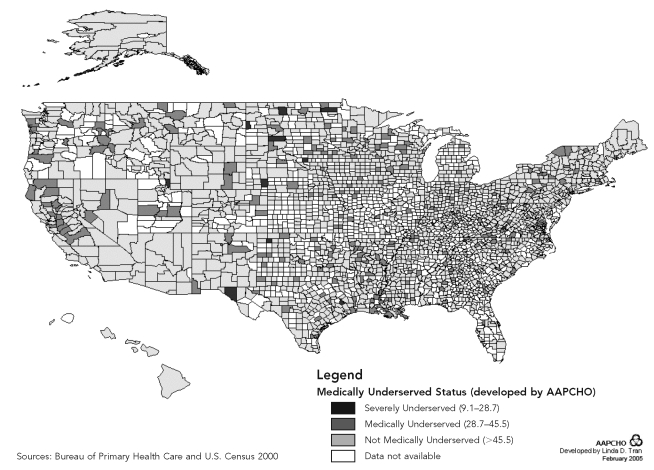
Based on the MUAC index, we identified 266 (12.1%) MUACs nationally (n=2,191) (Figure), with Aleutians East, Alaska, as the most underserved county (MUAC index = 9.1) and Pierce, North Dakota, as the least underserved county (MUAC index = 98.2). We classified 16 (0.1%) counties as severely medically underserved. Among the severely medically underserved counties, Philadelphia, Pennsylvania, had the highest number of AAPIs (n=68,383).
Figure.
Medically underserved AAPI U.S. counties, 2004a
aMUAC score mean: 67.1, standard deviation: 16.7, underserved criteria: MUAC '45.5, number of underserved counties: 266
NOTE: We determined the severely underserved category by subtracting the MUAC index standard deviation (16.7) from the MUAC index score (45.5).
AAPI = Asian American and Pacific Islander
MUAC = medically underserved AAPI county
AAPHCO = Association of Asian Pacific Community Health Organizations
Comparison with national MUA indexes
Nationally, 138 (51.9%) of the 266 MUACs were not designated as federal BPHC MUACs. Of these 138 MUACs not identified in the federal MUA index, 20 (14.5%) counties had an AAPI population of at least 10,000, and 29 (21.0%) counties had an AAPI population of at least 5,000. Counties consisting of at least 5,000 AAPIs had a mean MUAC index score of 38.8, well below the MUAC index standard score of 45.5. The mean AAPI poverty and LEP rates for these counties were 28.5% and 44.6%, respectively.
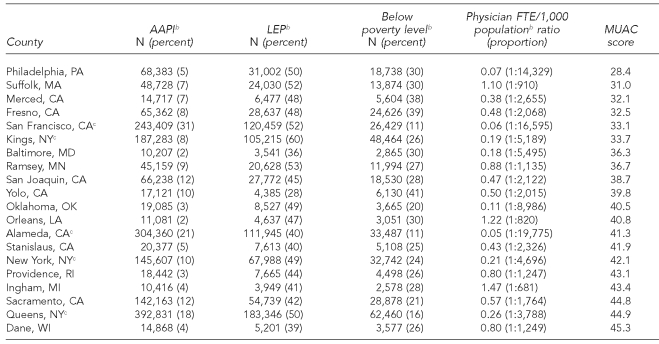
Further analysis of the profiles of these 29 MUACs excluded from the BPHC MUA designations revealed regional patterns. Nine of these counties were located in California and five were in New York. Philadelphia had the lowest MUAC index score of 28.4, with more than 68,000 AAPIs, a 29.8% poverty rate, a 50.4% LEP rate, and only a 0.07 P-to-1,000P ratio (approximately 14,300 population per one primary care physician). Suffolk, Massachusetts, followed with the second-lowest MUAC index score (31.0), with an AAPI population of close to 49,000, a 30.4% poverty rate, a 52.1% LEP rate, and a 1.10 P-to-1,000P ratio (approximately 910 population per one primary care physician). The county with the largest AAPI population in this group was Queens, New York, with a population of almost 400,000. Butte, California, had the highest AAPI poverty rate at 48.8% (data not shown), and Kings, New York, had the highest LEP rate at 60.3%. (See Table 2 for further details about high-risk AAPI counties.) Examples of MUACs that overlapped with MUAs included Aleutians East, Alaska (MUAC index = 9.1), and Vermillion Parish, Louisiana (MUAC index = 31.3) (data not shown).
Table 2.
MUACs with AAPI populations >10,000 that were excluded from the Bureau of Primary Health Care's Medically Underserved Area, County Levela
aData sources: Census Bureau (US). Projections of the resident population by age, sex, race, and Hispanic origin: 1999 to 2100. Washington: Census Bureau; 2000. Also available from: URL: http://www.census.gov/population/projections/nation/detail/d2041_50.pdf [cited 2007 Nov 30] and Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions (US). Guidelines for medically underserved area and population designation [cited 2007 Mar 14]. Available from: URL: http://bhpr.hrsa.gov/shortage/muaguide.htm
bWe calculated the MUAC index score using AAPI population, AAPI LEP population, AAPI poverty, and primary care physician FTE per 1,000 population ratio. The total underserved standard weighted/MUAC score = 45.5.
cCounties representing the top five MUACs with the greatest AAPI population
MUAC = medically underserved AAPI county
AAPI = Asian American and Pacific Islander
LEP = limited English proficiency
FTE = full-time equivalent
We compared the 138 MUACs not identified in the federal BPHC MUA index with the National Association of Community Health Centers' designations of unserved counties. Thirty-two of the 138 total MUACs (23.2%) overlapped with the National Association of Community Health Centers' unserved counties, with a mean MUAC index score of 37.6, a mean AAPI population of 1,069, a mean AAPI poverty rate of 39.2%, a mean AAPI LEP rate of 41.3%, and a 0.46 P-to-1,000P ratio (or approximately 2,174 population per one primary care physician). Of these 106 MUACs that did not match the federal MUA or National Association of Community Health Centers unserved county designations, St. Louis, Missouri, had the largest AAPI population (6,985), with an MUAC index score of 44.2, an AAPI poverty rate of 22.7%, an AAPI LEP rate of 51.2%, and a 1.17 P-to-1,000P ratio (or approximately 855 population per one primary care physician). Centre, Pennsylvania, had the second largest AAPI population (5,467), with an MUAC index score of 41.2, an AAPI poverty rate of 36.1%, an AAPI LEP rate of 34.8%, and a 0.48 P-to-1,000P ratio (approximately 2,080 population per one primary care physician).
MUACs with the largest AAPI populations
The five MUACs with the largest AAPI populations across the nation were located in California and New York. Among these five MUACs, San Francisco, California, was the most underserved and ranked in the first percentile across the nation, with an MUAC index score of 33.1, a 51.6% AAPI LEP rate, and a 0.06 P-to-1,000P ratio (approximately 16,600 population per one primary care physician). Kings, New York, was the second most underserved county, with an MUAC index score of 33.7, a 26.0% AAPI poverty rate, and a 60.3% AAPI LEP rate—the highest LEP rate among the top five MUACs. Alameda, California; New York, New York; and Queens, New York, followed closely behind.
DISCUSSION
This study identified major medically underserved AAPI counties on a national level and complements federal efforts to identify MUAs for new or existing health center expansions. It also provides a preliminary and innovative assessment of U.S. counties needing new and expanded community health services for AAPIs. This study also contributes to federal initiatives to improve participation of AAPIs in federal programs and to expand the number of people served by CHCs.
Efforts to identify AAPI MUAs are more critical than ever, given the new Proposed Rule22,46 and its potential impact on current and future CHCs that serve the rapidly growing medically underserved AAPIs across our nation. The new proposed health status and demographic measures do not appreciate the unique health and social factors that greatly affect AAPIs and other special populations. For AAPIs, one particular measure of social vulnerability to consider is data on LEP, which are available from the U.S. Census at the Census tract level.23 Overall, national guidelines from the Office of Management and Budget for tracking health and social indicators among AAPIs and other special populations across federal agencies need to be enforced and adhered to, so that medically underserved AAPIs are not excluded from the safety net simply due to lack of data.47
The proposed changes to the identification and designation of medically underserved populations and health professional shortage areas may be flawed for three major reasons. The first is that the proposed methodology was not developed in collaboration with an adequate sample of health centers and other relevant stakeholders. The Health Resources and Services Administration (HRSA) should engage these entities to establish a more appropriate methodology that does not negatively impact medically underserved populations and the health centers that serve them. The second concern is that the rule eliminates measures that are unique to CHCs serving special populations, such as those with LEP. This measure is of particular concern to CHCs serving AAPIs, as 35% of AAPIs live in linguistically isolated households and some ethnic groups (e.g., Hmong) have LEP rates as high as 61%.2 Finally, the changes include provisions that would make it extremely difficult for many CHCs that are currently in medically underserved populations/health professional shortage areas and serve medically underserved patients to retain their designation.23
Approximately 30% (n=1,100) of health center service areas would lose their designation with the proposed changes.48 Without these considerations, the proposed changes neglect the unique needs of many minority populations served by CHCs. As the number of uninsured people continues to rise, the CHC program is more vital than ever to this country's safety net. Due to these concerns, the proposed changes should be withdrawn. It is instead recommended that HRSA enter into a negotiated rule-making process in collaboration with CHCs and other stakeholders, taking into consideration the implications for identifying MUAs for AAPIs identified in this study.
In this study, we have provided a national county-level assessment and identified major MUACs. Results suggest the need to look more closely at the presence and location of existing services, whether they adequately target AAPIs, and areas of growth required to meet higher needs (e.g., in San Francisco). The model minority myth, diversity of languages, relative population size, and other socioeconomic characteristics may have led to the neglect of these medically underserved AAPI communities. MUACs identified clearly lack adequate primary care and other community services to support underserved AAPIs. Additional health center resources and culturally competent primary care providers are needed to adequately serve this population. However, the county-level data may be too broad, and we suggest the need for additional analysis within smaller communities to address the expansion of CHCs in sub-county-level areas identified in these MUACs.
In addition to CHCs, other safety net providers exist in MUACs that were not considered in our analysis. Thus, non-CHC providers (e.g., hospitals) serving MUACs may serve underserved AAPI populations. Nonetheless, CHCs play a vital, central role in providing culturally and linguistically appropriate comprehensive primary care that fits their AAPI patients' individual languages and cultural needs. Thus, they are an essential component of quality care for AAPIs.17
Limitations
This study had several limitations. First, it was limited by the lack of AAPI data publicly available at the county level. The MUAC index could be improved with more and better public data for AAPI health. Second, AAPI poverty may be confounded with total AAPIs, because low-income AAPIs tend to be concentrated in larger AAPI areas that may have a higher cost of living, thus possibly underestimating the number of AAPIs living in poverty. Third, census block, state, and other levels of analysis could complement this work and should be examined in future studies. For example, because of the large size of the identified MUACs, more research is needed to further delineate the need for new and expanded CHCs within the counties.
Fourth, although we identified 138 MUACs that did not overlap with BPHC MUACs, it should be noted that BPHC also uses health professional shortage areas or medically underserved populations in addition to MUA designations, so that special populations such as AAPIs can obtain a medically underserved population designation. However, unlike the MUA designation, this process is not formalized and burdens health centers to provide the data to obtain designation.
Fifth, units smaller than county levels, such as census tracts, may have been designated as BPHC MUAs. Thus, the comparison may not be on the same level and requires further examination. However, this also may reflect the BPHC MUA index limitations of not adequately capturing underserved AAPI regions and the need for federal health programs to reexamine the regional primary care resource allocation needs for medically underserved AAPIs. Overall, comprehensive community- and national-level assessments will be critical to better evaluate and address the wide AAPI socioeconomic and health disparities across our nation.
CONCLUSION
This study complements federal efforts to identify MUAs for new or existing health center expansion and provides a preliminary and innovative assessment of U.S. counties needing new and expanded community health services for underserved AAPIs. Our findings contribute to the presidential and congressional initiatives to improve participation of AAPIs in federal programs and to expand the number of people served by CHCs.
As part of the President's initiatives to double the number of CHCs21 and to expand CHCs to every poor county in America,23 the BPHC seeks information on priority areas to expand CHCs. These results can be used by policy makers not only to expand health-care services, but also to develop programs and services to improve health-care access for AAPIs. The information provided also can complement the BPHC's MUA designations (new or old) to help address and prioritize new health center budgetary allocations and expansion areas for AAPIs across the U.S.
Acknowledgments
The authors acknowledge Linda Tran, Mari Muraki, and Katherine Chen for their research and administrative support, as well as Michelle Proser for her comments and recommendations for this project.
Footnotes
This project was funded in part by the Department of Health and Human Services, Office of Minority Health, contract #2T02080101D.
No protocol approval was needed for this study. This project was a secondary data analysis of public-use datasets from the Health Resources and Services Administration Bureau of Primary Health Care and the U.S. Census.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official views of the Office of Minority Health.
REFERENCES
- 1.Census Bureau (US) 2004 American Community Survey. Washington: Census Bureau; 2005. [Google Scholar]
- 2.Census Bureau (US) Washington: Census Bureau; 2000. [cited 2007 Nov 30]. Projections of the resident population by age, sex, race, and Hispanic origin: 1999 to 2100. Also available from: URL: http://www.census.gov/population/projections/nation/detail/d2041_50.pdf. [Google Scholar]
- 3.Barnes JS, Bennett CE. The Asian population: 2000: Census 2000 brief; Census Bureau (US); Washington. 2002. [cited 2007 Nov 30]. Also available from: URL: http://www.census.gov/prod/2002pubs/c2kbr01-16.pdf. [Google Scholar]
- 4.Census Bureau (US) The Native Hawaiian and other Pacific Islander population: 2000: Census 2000 brief. Washington: Census Bureau (US); 2001. [cited 2007 Nov 30]. Also available from: URL: http://www.census.gov/prod/2001pubs/c2kbr01-14.pdf. [Google Scholar]
- 5.Ghosh C. Healthy People 2010 and Asian Americans/Pacific Islanders: defining a baseline of information. Am J Public Health. 2003;93:2093–8. doi: 10.2105/ajph.93.12.2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Asian Liver Center at Stanford University. FAQ about hepatitis B. [cited 2009 Jun 21]. Available from: URL: http://liver.stanford.edu/Edu/Edu_stat.php http://liver.stanford.edu/Education/faq.html.
- 7.Centers for Disease Control and Prevention (US). Fact sheet: racial/ethnic health disparities. [cited 2005 Apr 30]. press release 2004 Apr 2. Available from: URL: http://www.cdc.gov/od/oc/media/pressrel/fs040402.htm.
- 8.Miller BA, Kolonel LN, Bernstein L, Young JL, Swanson GM, West DW, et al., editors. Racial/ethnic patterns of cancer in the United States. Bethesda (MD): Department of Health and Human Services, Public Health Service, National Institutes of Health (US), National Cancer Institute, Cancer Statistics Branch; 1996. pp. 1988–1992. HHS publication no. (NIH) 96-4104. [Google Scholar]
- 9.Pamuk E, Makuc D, Heck K, Reuben C, Lochner K. Health, United States, 1998, with socioeconomic status and health chartbook; National Center for Health Statistics (US); Hyattsville (MD). 1998. [cited 2005 Apr 30]. Also available from: URL: http://www.cdc.gov/nchs/data/hus/hus98.pdf. [Google Scholar]
- 10.Chen MS., Jr. Cancer health disparities among Asian Americans: what we do and what we need to do. Cancer. 2005;104(12) Suppl:S2895–902. doi: 10.1002/cncr.21501. [DOI] [PubMed] [Google Scholar]
- 11.McCracken M, Olsen M, Chen MS, Jr, Jemal A, Thun M, Cokkinides V, et al. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA Cancer J Clin. 2007;57:190–205. doi: 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- 12.Ponce NA, Tseng W, Ong P, Shek YL, Ortiz S, Gatchell M. The state of Asian American, Native Hawaiian, and Pacific Islander health in California report. Los Angeles: University of California Asian American and Pacific Islander Policy Multi-Campus Research Program; 2009. [Google Scholar]
- 13.Chen MS, Hawks BL. A debunking of the myth of healthy Asian Americans and Pacific Islanders. Am J Health Promot. 1995;9:261–8. doi: 10.4278/0890-1171-9.4.261. [DOI] [PubMed] [Google Scholar]
- 14.Lin M-KK, Kazinets G, Ivey S, Moskowitz JM. Berkeley (CA): Center for Family and Community Health, University of California at Berkeley; 2006. [cited 2007 Nov 1]. The health of Asian Pacific Islander American adults in California; pp. 2001–2003. Also available from: URL: http://cfch.berkeley.edu/reports/reports.html/APIA%20health%202001-03%20report.pdf. [Google Scholar]
- 15.National Association of Community Health Centers. America's health centers. Washington: National Association of Community Health Centers; 2008. [Google Scholar]
- 16.Weir RC, Song H. Association of Asian Pacific Community Health Organizations member centers: 2007; Association of Asian Pacific Community Health Organizations; Oakland (CA). 2008. [cited 2009 Jun 21]. Also available from: URL: http://www.aapcho.org/altruesite/files/aapcho/Publications_FactSheets/2007%20UDS%20AAPCHO%20Fact%20Sheet%20-%20final.pdf. [Google Scholar]
- 17.Weir RC, Proser M. Health centers' role in reducing health disparities among Asian Americans and Pacific Islanders. Association of Asian Pacific Community Health Organizations and National Association of Community Health Centers; Washington. 2005. [cited 2007 Nov 1]. Also available from: URL: http://www.aapcho.org/altruesite/files/aapcho/Publications_FactSheets/AAPIDisparitiesFactSheet.pdf. [Google Scholar]
- 18.Department of Health and Human Services, Health Resources and Services Administration (US). The Health Center Program: 2006 national aggregate UDS data. 2006. [cited 2007 Nov 1]. Available from: URL: http://bphc.hrsa.gov/uds/2006data/National/NationalTable3Buniversal.htm.
- 19.Department of Health and Human Services, Health Resources and Services Administration (US). Guidelines for MUA and MUP designation. [cited 2007 Mar 14]. Available from: URL: http://bhpr.hrsa.gov/shortage/muaguide.htm.
- 20.Texas Department of State Health Services. Medically underserved area (MUA) and medically underserved population (MUP): designations in Texas. [cited 2007 Mar 14]. Available from: URL: http://www.dshs.state.tx.us/CHS/hprc/muacovr.shtm.
- 21.Jordan A. Briefing on the notice of proposed rulemaking for designation of underserved areas. Rockville (MD): National Association of Rural Health Clinics; 2008. [cited 2009 Jun 21]. Also available from: URL: http://ruralhealth.hrsa.gov/RHC/2008-03-11call_files/frame.htm. [Google Scholar]
- 22.Department of Health and Human Services (US). Designation of medically underserved populations and health professional shortage areas: proposed rule. Fed Reg. 2008;73(41) 42 C.F.R. parts 5 and 51c. [PubMed] [Google Scholar]
- 23.National Association of Community Health Centers. Summary of proposed rule on designation of medically underserved populations and health professional shortage areas. Fed Reg. 2008;73:11232. [Google Scholar]
- 24.Dial TH, Palsbo SE, Bergsten C, Gabel JR, Weiner J. Clinical staffing in staff- and group-model HMOs. Health Aff (Millwood) 1995;14:168–80. doi: 10.1377/hlthaff.14.2.168. [DOI] [PubMed] [Google Scholar]
- 25.Ricketts TC, Goldsmith LJ, Holmes GM, Randolph RM, Lee R, Taylor DH, et al. Designating places and populations as medically underserved: a proposal for a new approach. J Health Care Poor Underserved. 2007;18:567–89. doi: 10.1353/hpu.2007.0065. [DOI] [PubMed] [Google Scholar]
- 26.Kehrer BH, Wooldridge J. An evaluation of criteria to designate urban health manpower shortage areas. Inquiry. 1983;20:264–75. [PubMed] [Google Scholar]
- 27.Larson EH, Palazzo L, Berkowitz B, Pirani MJ, Hart LG. The contribution of nurse practitioners and physician assistants to generalist care in Washington State. Health Serv Res. 2003;38:1033–50. doi: 10.1111/1475-6773.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goodman DC, Fisher ES, Bubulz TA, Mohr JE, Poage JF, Wennberg JE. Benchmarking the US physician workforce. An alternative to needs-based or demand-based planning [published erratum appears in JAMA 1997;277:966] JAMA. 1996;276:1811–7. doi: 10.1001/jama.276.22.1811. [DOI] [PubMed] [Google Scholar]
- 29.Department of Health and Human Services, Health Resources and Services Administration (US). Testimony to the House Appropriations Subcommittee on Labor, Health and Human Services, Education, and Related Agencies by HRSA Administrator Elizabeth M. Duke. 2005 Mar 15. [cited 2007 Mar 19]. Available from: URL: http://newsroom.hrsa.gov/speeches/2005/DukeHouse.htm.
- 30.Office of the Press Secretary (US). President discusses health care information technology benefits; 2005 Jan 27; Cleveland. [cited 2007 Mar 19]. Available from: URL: http://www.whitehouse.gov/news/releases/2005/01/20050127-7.html.
- 31.Federal Register. Designation of medically underserved areas and population groups. Federal Register. 1975;40:40315–40320. [Google Scholar]
- 32.Wright RA, Andres TL, Davidson AJ. Finding the medically underserved: a need to revise the federal definition. J Health Care Poor Underserved. 1996;7:296–307. doi: 10.1353/hpu.2010.0246. [DOI] [PubMed] [Google Scholar]
- 33.Andrulis D, Goodman N, Pryor C. What a difference an interpreter can make: health care experiences of uninsured with limited English proficiency. The Access Project; April 2002; Boston. [cited 2004 Apr 30]. Also available from: URL: http://www.accessproject.org/downloads/c_LEPreportENG.pdf. [Google Scholar]
- 34.Douglas KC, Fujimoto D. Asian Pacific elders: implications for health care providers. Clin Geriatr Med. 1995;11:69–82. [PubMed] [Google Scholar]
- 35.Sarver J, Baker DW. Effect of language barriers on follow-up appointments after an emergency department visit. J Gen Intern Med. 2000;15:256–64. doi: 10.1111/j.1525-1497.2000.06469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Manson A. Language concordance as a determinant of patient compliance and emergency room use in patients with asthma. Med Care. 1988;26:1119–28. doi: 10.1097/00005650-198812000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Naish J, Brown J, Denton B. Intercultural consultations: investigation of factors that deter non-English speaking women from attending their general practitioners for cervical screening. BMJ. 1994;309:1126–8. [PMC free article] [PubMed] [Google Scholar]
- 38.Woloshin S, Bickell NA, Schwartz LM, Gany F, Welch HG. Language barriers in medicine in the United States. JAMA. 1995;273:724–8. [PubMed] [Google Scholar]
- 39.Woloshin S, Schwartz LM, Katz SJ, Welch HG. Is language a barrier to the use of preventive services? J Gen Intern Med. 1997;12:472–7. doi: 10.1046/j.1525-1497.1997.00085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Takaki RT. Strangers from a different shore: a history of Asian Americans. Boston: Little Brown; 1989. [Google Scholar]
- 41.Portes A, Rumbaut RG. Immigrant America: a portrait. Berkeley (CA): University of California Press; 1990. [Google Scholar]
- 42.Portes A, Rumbaut RG. Legacies: the story of the immigrant second generation. Berkeley (CA): University of California Press; 2001. [Google Scholar]
- 43.Shi L, Macinko J, Starfield B, Wulu J, Regan J, Politzer R. The relationship between primary care, income inequality, and mortality in US states, 1980–1995. J Am Board Fam Pract. 2003;16:412–22. doi: 10.3122/jabfm.16.5.412. [DOI] [PubMed] [Google Scholar]
- 44.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—the Public Health Disparities Geocoding Project. Am J Public Health. 2003;93:1655–71. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Proser M, Shin P, Hawkins D. Washington: National Association of Community Health Centers; [cited 2009 Jun 21]. A nation's health at risk part III: growing uninsured, budget cutbacks challenge president's initiative to put a health center in every poor county. March 2005. Also available from: URL: http://www.nachc.com/client/poorcountiesSTIB9.pdf. [Google Scholar]
- 46.Ricketts TC, Goldsmith LJ, Holmes GM, Randolph R, Lee R, Taylor DH, et al. Designating places and populations as medically underserved: a proposal for a new approach. J Health Care Poor Underserved. 2007;18:567–89. doi: 10.1353/hpu.2007.0065. [DOI] [PubMed] [Google Scholar]
- 47.Executive Office of the President, Office of Management and Budget (US) Revisions to the standards for the classification of federal data on race and ethnicity. [cited 2008 Jul 12]. Available from: URL: http://www.whitehouse.gov/omb/fedreg/ombdir15.html.
- 48.National Association of Community Health Centers. Letter to Andy Jordan, Health Resources and Services Administration, Department of Health and Human Services (US). 2008 May 12. [cited 2009 Jun 21]. Available from: URL: http://www.nachc.com/client/documents/exnewsletters/NACHC-Draft-Comments%20-on-Shortage-Designation-NPRM.pdf.