Abstract
While it is well understood that multiple and cumulative environmental stressors negatively impact health at the community level, existing ethical research review procedures are designed to protect individual research participants but not communities. Increasing concerns regarding the ethical conduct of research in general and environmental and genetic research in particular underscore the need to expand the scope of current human participant research regulations and ethical guidelines to include protections for communities. In an effort to address this issue, West Harlem Environmental Action (WE ACT), a nonprofit, community-based environmental justice organization in New York City that has been involved in community–academic partnerships for the past decade, used qualitative interview data to develop a pilot model for community review of environmental health science research.
Research efforts to disentangle the wide array of complex and interacting factors that contribute to health disparities between minority and majority population subgroups have not been able to measurably reduce these differences. Adequate data on all segments of the population, especially those that suffer disproportionate levels of morbidity and mortality, are critical to understanding the effects of race, ethnicity, class, gender, culture, and environment on health. Yet, persistent challenges in the recruitment and retention of diverse groups of participants in biomedical and behavioral research prevent the science from moving forward.1 Community-based participatory research (CBPR) has and can continue to transform the scientific landscape, reinvest marginalized communities in the research process, and improve public policy.2 The objective of this approach is to engage communities as a whole and residents individually in biomedical and behavioral research at inception—from study design to implementation, oversight, result interpretation and dissemination of findings—and, in so doing, create a mutually beneficial research enterprise that incorporates the concerns, needs, and interests of the study community as well as of the researcher.3 Over the past decade, the development of successful community academic partnerships between researchers, local community organizations, and residents have contributed to improved community health.4 In principle, CBPR requires that the researcher and the community be equal partners in the quest for scientific knowledge.
In fact, the role of “community-based entities” in most research remains largely advisory.5 The ability of lay collaborators to shape the research agenda in an informed and comprehensive manner has been limited for a number of reasons, among them issues of lay capacity and training, reluctance on the part of some researchers to engage the community in internal decision making, minimal community involvement in the institutional research review process, and a scarcity of financial resources.6 Increasing concerns regarding community consent to human participant research in general, and environmental and genetic research in particular, underscore the need to expand the scope of human participant research ethical guidelines to include statutory protections for communities.7 Currently, academic centers employ a variety of informal methods to engage community organizations and residents in research, ranging from hiring university-based community liaisons, local community organizers, or community members as research staff, to convening community advisory boards (CABs), and partnering with community-based organizations.8
The National Institute for Environmental Health Sciences (NIEHS) was the first branch of the National Institutes of Health to recognize the importance of using a CBPR approach. In 1993, NIEHS began to sponsor academic–community partnerships.9 West Harlem Environmental Action (WE ACT), a nonprofit, community-based environmental justice organization in New York City was among the first recipients of NIEHS collaborative support. This article summarizes initial findings from the qualitative component of WE ACT's NIEHS-funded education and demonstration project on best practices for bolstering community protections in human-participants research through developing an effective community research review process. We begin with a brief history of environmental justice and health, and WE ACT's alliance with NIEHS.10
FRAMING THE ISSUE
Residents of communities burdened with environmental hazards are placed at a greater risk for environmental exposures than is the general population. Whether this is the result of economic forces (decreased property values because of the environmental hazards) or strategic planning (targeted placement of environmental hazards), environmental stressors negatively impact health.11 In 1982, when soil contaminated with polychlorinated biphenyls was dumped in a low-income community of color in Warren County, North Carolina, the adverse health effects garnered national attention.12 Equipped with newfound visibility, environmental justice groups began to mobilize and seek redress.13 In 1991, the United Church of Christ Commission for Racial Justice helped to convene organizations in Washington, DC, for The First National People of Color Environmental Leadership Summit. Guided by the 17 Principles of Environmental Justice, the coalition began to agitate for policy change.14 On February 11, 1994, President Bill Clinton issued Executive Order 12898, mandating federal agencies to include environmental justice in their mission and address the disproportionate pollution burden in communities of color.15 In 1995, the federal Interagency Working Group on Environmental Justice, established a year earlier, held its first public meeting to promote new federal initiatives and gauge community sentiment. In 1996, the White House Council on Environmental Quality issued a draft guidance on incorporating environmental justice into the National Environmental Protection Act requirements. And, in 1999, the Institute of Medicine issued a report entitled Environmental Justice: Research, Education and Health Policy Needs.16 At the same time that the fundamental link between environmental justice and health was being established, NIEHS brought together academic researchers and community organizations in an interagency symposium titled Health Research Needs to Ensure Environmental Justice. Under the leadership of its director, Kenneth Olden, NIEHS sought to ensure that community concerns were incorporated into the agencies' research agenda and created 2 new funding mechanisms designed to provide federal support for community involvement in biomedical and behavioral research: Environmental Justice: Partnerships for Communication, in 1993, and Community-based Participatory Research, in 1995. 17
WE ACT participated in a leadership capacity both in the formal convening of the Environmental Justice Movement at the 1991 summit and in the 1994 NIEHS symposium, making it one of the key environmental justice organizations using science to impact practice and public policy. A multiyear NIEHS grant led to WE ACT's creation of the Northern Manhattan Environmental Justice Partnership and provided WE ACT with the resources to develop linguistically appropriate and culturally sensitive materials and methods for reporting and disseminating environmental justice research findings to scientists, health care providers, and community residents. The project also trained 300 community residents to be advocates for environmental health and justice in their own communities. Additional funding from NIEHS and the Environmental Protection Agency enabled WE ACT to establish a long-term partnership with the Columbia Center for Children's Environmental Health and launch and sustain the Healthy Home, Healthy Child, and Our Housing is Our Health campaigns. Having been involved in the environmental justice movement and in environmental health sciences research for almost 2 decades, WE ACT interacts with researchers and community organizations both on a local and national level. This scientific inquiry represents a natural progression in WE ACTs efforts to strengthen community protections in environmental health science research.
METHODS
We focused on academic research institutions because they provide a unique opportunity to explore the structural dynamics underlying existing practices from different vantage points. Qualitative data capturing the perspectives of research scientists, frontline field research workers, community researchers, CAB members, and institutional review board (IRB) members were gathered and used to understand the current process of ethical review for community-based environmental health research, evaluate and identify the aspects of current ethical decision-making practice that may enhance or impede community review, and develop an effective community research review model.
The process for creating the community research review model was iterative. In the prestudy phase, we conducted informal telephone interviews with a convenience sample of NIEHS-funded university and community-based environmental health researchers to develop a topical interview guide that reflected the diverse perspectives of both the academy and community. We then conducted focus groups with university-based field research workers, and semistructured individual interviews with university-based research scientists to identify the distinct ethical challenges that emerge during the conduct of environmental health research. Based on thematic analysis of this initial body of data, we drafted a conceptual model of the community research review process. In the second phase we conducted a series of dialogues with a mix of university-based research scientists, field research workers, and community-based researchers and advisors to understand the practical limitations and deficiencies of the community research-review process and revise the model accordingly.18 In the final stage, we conducted individual semistructured interviews with administrative and lay members of an academic IRB to identify potential issues that might arise in the implementation process.
Prospective study participants were identified from publicly available institutional and NIEHS contact information lists. All research scientists, field research workers, and CAB members from 2 university-based NIEHS-funded research centers were invited to participate in the study via an introductory e-mail describing the study protocol. Follow-up phone calls were then made to those agreeing to participate and either individual interviews, group interviews, or both were scheduled. For the dialogues, we used the same recruitment methodology to draw a purposeful convenience sample from registration lists of NIEHS community and academic environmental justice and participatory research grantees, inviting equal numbers of university-based and community-based researchers and affiliates to participate. Snowball sampling was used to recruit IRB and community-based organization members to the study.19
We conducted informal phone interviews with a convenience sample of 8 community-based organization affiliates and 9 environmental health researchers drawn from an NIEHS environmental justice and CBPR grantee list. Participants were contacted via e-mail and phone. Interviews ranged in length from 20 minutes to an hour, with the average interview lasting 30 minutes. The goal was to gather background data on knowledge, attitudes, and perceptions of environmental health research, research ethics, and community review of research. We used the raw interview data to develop a topical outline and preliminary interview guide based on 3 domains: environmental health research design, attitudes and perceptions of ethics and ethical practice in environmental health research, and CBPR and the research review process (see the box on the next page).
Topical Outline and Preliminary Guide
- Environmental Health Research
- Meaning
- Definition
- Goals
- Limitations
- Benefits
- Design
- Role of community members
- Role of community-based organizations
- Role of researchers
- Role of academic institutions
- Of community advisory board members
- Attitudes and Perceptions of Ethics and Ethical Practice in Research
- Ethics
- Definition
- Ethical dilemmas and challenges
- Mechanisms to address dilemmas
- Ethics training of researchers and community advisory board members
- Ethical Responsibility
- Of community members
- Of community-based organizations
- Of researchers
- Of academic institutions
- Of community advisory board members
- Community-Based Participatory Research and Review Process
- Meaning
- Define concept of community review and community-based participatory research
- Goals of collaboration
- Limitations
- Benefits
- Review Process
- Role of community members
- Role of community-based organizations
- Role of researchers
- Role of academic institutions
- Role of community advisory board members
Data Collection
Using the topical guide, we conducted a series of audiotaped, semistructured individual and group interviews with a purposeful convenience sample of environmental health research scientists and field workers, CAB members, community advocates, and IRB members.20
In the initial phase, we conducted 2 audiotaped focus groups with a 6-member field-work team from a university-based NIEHS-funded environmental health research center. The team comprised study community members. The data were used to identify the specific set of practical and ethical issues encountered over the course of an ongoing long-term community-based environmental health research project. Each focus group lasted approximately 2 hours. Following a cognitive interview design, we used the focus group data to formulate a list of discussion probes for the 3 domains of the interview guide.21
In total, we conducted 20 individual, audiotaped, semistructured interviews with university-based research scientists (n = 11), CAB members (n = 5), and IRB members (n = 4). Interviews ranged in length from 1 to 2 hours, with the average interview lasting 90 minutes. The interviews focused on the concept and design of collaborative partnerships and CBPR, ethical responsibility, and the ethical dilemmas and challenges of community-based environmental health research.
Dialogues
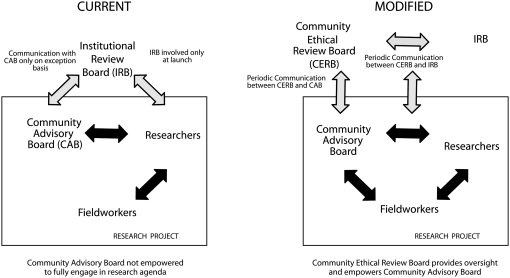
Based on the semistructured interview data, we created a draft model to employ in 4 audiotaped dialogues with environmental health researchers and community advocates on the design and conceptual framework for community research review (Figure 1).
FIGURE 1.
Draft of conceptual review models.
Each dialogue contained between 7 and 8 discussants and lasted approximately 1 hour, excluding the informed consent process, which required an additional 10 to 15 minutes.
The initial dialogue took place at the annual advisory board meeting of a university-based NIEHS-funded research center in New York City with a mixed group of community advocates and advisory board members (n = 4) and university research scientists and field research workers (n = 4). We evaluated the draft model and then used the feedback to develop a working research review model. The second iteration of the Community Ethical Research Review Model was vetted at the 2007 NIEHS Environmental Justice Program Grantee Meeting in Boston, Massachusetts, with a group of community-based environmental health researchers (n = 7) and a group of academia-based environmental health researchers (n = 8). We then refined the framework for the model based on the observations and comments of the discussants. The final version of the pilot model was then assessed in a dialogue with 8 staff members of a local community-based environmental justice organization.
Data Analysis
All interviews, focus groups, and dialogues employed in the analysis were conducted by B. X. W. The interview data were independently analyzed by B. X. W. and a research scientist with expertise in qualitative-research methods. Using a grounded-theory approach, each research scientist manually coded the data.22 For a second level of thematic analysis, the textual data were entered into a qualitative data analysis package (Atlas.Ti) and into content-analysis-generated categories and codes.23 All codes were saved within Atlas as nodes. The nodes were then reordered, labeled, and grouped into families. The interrater reliability rate was 96%. Interviews containing discordant themes were jointly analyzed, recoded, and merged into existing thematic categories.24 Information obtained from a literature review was then used to cross-check the themes. Once the research team agreed on a set of final themes, the themes were incorporated into the model and subsequently presented to subsets of participants during a series of dialogues.25 The thematic content analysis revealed some distinct differences in the perspectives of university-based environmental health researchers and community-based environmental health researchers and advisors. For summary purposes, we grouped the major themes within the interview protocol's 3 domains (see the box on the next page).
Thematic Content Analysis
I. Environmental Health Research Design
A. University-based Researchers:
• Seek to increase scientific knowledge about the effects of environmental exposures on health
• Develop methods for identifying and reducing harmful exposures
• Must address funding agency's agenda
B. Community-based Researchers and Advisors:
• Seek to increase community knowledge about the effects of environmental exposures on health through education
• Improve community health
• Must address community agenda
II. Attitudes and Perceptions of Ethics and Ethical Practice in Environmental Health Research
A. Ethical Responsibility
• University-based researchers define ethical responsibility in terms of science and compliance with human participant research regulations
• Community-based researchers and advisors define ethical responsibility in terms of community benefits
B. Ethical Practice Issues
• University-based researchers believe that:
a. Community members' lack of scientific knowledge limits their ability to understand the research
b. Current research ethics training requirements are minimal
c. Ethics training should be provided to study participants and community members
d. Full data disclosure is complicated by unclear interpretive guidelines and inconclusive results
e. Translation of scientific data into lay language is difficult
• Community-based researchers and advisors believe that:
a. Lack of scientific knowledge limits the communities ability to voice concerns about the research
b. University-based researchers need training in ethics and cultural sensitivity
c. Ethics training should be provided to study participants, community members, and researchers
d. Researchers do not want to disclose findings and disseminate data to the community
III. Community-based Participatory Research (CBPR) and the Research Review Process
A. Community-based Participatory Research
• University-based researchers:
a. Do not differentiate between a community-based approach to research and CBPR
b. View true CBPR (full community participation) as a nonessential, time consuming, and labor- and resource-intensive process
• Community-based researchers and advisors:
a. Differentiate between community based research and CBPR
b. View true CBPR (full community participation) as an opportunity for the community to drive the research
B. Current Research Review Process
• University-based researchers believe that the current process:
a. Protects the researcher, the institution, and the participants but not the community
b. Is cumbersome and time consuming
c. Provides ongoing oversight in the form of researcher initiated protocol modifications and renewal
d. Provides participants with the opportunity to report misconduct
• Community-based researchers and advisors believe that the current process:
a. Protects participants, researchers, and the institution but not the community
b. Requires initial evaluation and approval, but minimal ongoing oversight
c. Does not provide participants will a confidential process for reporting misconduct
d. Does not provide participants with an opportunity to ask questions about the research
RESULTS
There was wide variation in the definition and understanding of CBPR design. Many university-based researchers described their community-based environmental health research projects as CBPR, yet they only partially adhered to its principles. For the most part, these research scientists seemed unaware that CBPR requires full community engagement in all phases of the research, from inception through result dissemination. As in the case of the university-based researcher quoted below, the data demonstrate an overwhelming tendency to narrowly and arbitrarily select aspects of CBPR design:
We defined [CBPR] by having Community Advisors on the Advisory Committee that were really Executive Committee. That's key. I mean that's where the decisions, a lot of the decision making, is. And then hiring people from the community as basically the staff. And, you know, that's probably the key because that's where really, in terms of the sort of the day to day running, that's where you're … really interfacing [with the community].
The data also revealed ambivalence on the part of many university-based researchers to an expanded community role in research:
I'd like to add that community people are not scientists and so while, yes, we ask them for their opinion, we have to make sure we're asking the right people for their opinion. People who understand, from a very clear understanding of what we're doing and trying to do. Should they be given absolute power? Of course not, they're not scientists. We're the ones that are doing this. But they should be able to understand what we are doing.
I don't think the community needs to be involved in every single stage of the study. I think that is unrealistic… . So I don't think that at every track that an investigator needs to be going through evaluation… . You should listen to the community perhaps, not always, but in some cases, yes. And then afterward communicate it back, um, and in between … it's always good to communicate. But I don't believe that community members should be heavily involved in the design of the study. I don't think they have that commitment, but there will be exceptions.
By contrast, community-based researchers and advisors envision a myriad of ways to increase community involvement and conduct CBPR, which some described as “community-built research”:
We do community-built research; we're not separated. I bring a set of expertise to the table that's different than the community [as a] researcher, but we are the same group. We don't meet separately; we meet together, and we discuss research issues together. We discuss methodology together… . The community builds the research itself.
I think that [community] can also play a role in communicating results, helping the translation of results to other community residents. Some community residents can be ambassadors if you will, for the research that is done, you know, helping in the publicizing, beyond the doorstep of their community… . I believe that there is a role for community in reviewing … research before it actually becomes a formalized project.
It is important for the researchers … to understand the community where they are [working]… . You can really see the community-based participatory organizations; our roles are really to bridge that gap and then to help to make sure that the research is done okay and these findings get back to the community, that the community is aware of what is found, what is the outcome, what's next, what is the next step.
Differences in “ethical orientation” may be at the root of this conceptual divide. University-based researchers describe ethical issues in environmental health research in terms of scientific integrity and regulatory compliance, whereas community-based researchers and advisors describe ethical issues in terms of protecting study participants. University-based researchers stated:
I think [of] the ethical goals that I mentioned before from a scientific perspective. Having integrity scientifically … presenting real data, and secondly, treating human subjects respectfully, and thirdly, having a commitment to work in a real partnership with community partners. And that might be the priority order that scientist might place on 1 of those 3 things.
The academic institution is probably primarily interested in the scientific integrity, of not getting into trouble that way, and human subjects' protections, and not getting into trouble that way. And they are more interested legally in not getting into trouble … and reducing vulnerability on those 2 fronts primarily.
Community-based researchers commented:
Say you are doing something, like on asthma in the homes … if you go in and see lead paint, are you going to report it? When I first brought it up with my university-based researchers … they've never even thought of that. They haven't even thought of it. And then their first reaction was that might hurt our study … if you have to refer those people if you see lead paint.
Research ethics worry me. The research should be helping to support local agendas, not coming down and saying this is [it]. And that's why I keep saying I need to understand how … [the research] would help me make sure the people I work with are protected.
Both university-based researchers and community-based researchers acknowledged shortcomings in the current research review process, which provides little ongoing oversight and, in turn, protection for participants. One university-based researcher who serves on the IRB expressed the major flaw in the current process as follows:
Once you [a researcher] have gotten your [institutional research review] approval, we are pretty much in the trust mode. Pretty much. You know things can become so blatant that even if you did not want to report it you have to report it anyway. Pretty much we are trusting the researcher to do the right thing. Yes, there is a renewal to see if your research is going to continue. But is there real oversight? No, I don't think so.
Community-based researchers unanimously cited guidelines for ongoing oversight and a broad base of community representation as central to effective community research review:
And the outcome it seems to me it just as important as the beginning of a project. So there should be some guidelines for consistency and oversight … I can see intervals throughout the process that the community ethical review board is responsible for doing some kind of real oversight … in the beginning, at the end, and in the middle.
For many, the community ethical research review board (CERB) provides an opportunity to address these concerns and avoid the problems encountered with the CAB model. Community-based researchers and advisors identified several structural aspects that would be critical to the success of the CERB:
So the question is … who will be on a community ethical review board? The other question is how are you going to do that appointment so it doesn't replicate what we currently see. Is that what happened to the CAB? Because most of the Chinese research projects have been going [in]to situations where there's not a preexisting community ethical review board. And there's probably not even a structure from which [one] could easily develop one, or a community [could] easily develop one. So, in terms of helping us [in] thinking about implementing this model, the who and also the how, in a way, … you're not replicating … how CABS are.
The subject has to have representation somewhere in this process … I love the community ethical review board, but I'm wondering how essentially it can work for the [research] subject's power, to eventually become more resourceful … How do you keep it going so that it is really representative of the people of the community?
Both university-based and community-based researchers and advisors thought the CERB should serve as a forum for community members and researchers to engage in a dialogue about community health issues but voiced concerns about resource and time demands and education and training. According to a university-based researcher:
So I think getting people talking to each other, understanding what both of their concerns are, is a starting point. Because if the researcher doesn't understand the concerns of the community, they are not going to be interested in working with the community.
A community-based researcher said:
It's not going to be regulatory in that sense … it will be a place where any investigator, and particularly trainees, … fellows and people who don't know their way around … are going to talk to each other.
The participants expressed concern that community research review would create additional layers of bureaucracy and paperwork. Two university-based researchers commented:
It's slow, and it takes longer to do things, at least from the scientific researcher side. A researcher might decide to study some other thing because they could not get it done quicker … than if they had to go through a community-based process. A truly community-based process, where there is a lot of give and take, takes longer.
You know researchers are under lots of time pressure, and they don't want to devote money that they could easily see how they could spend on what they think is most important about their research. If [community review] has to come out of an existing budget, [it won't get done] unless they're told they have to.
Other community-based researchers and advisors stated:
I immediately think that [community review] costs money. Extra meetings cost money. I have to go out and raise money to do that [community review] meeting. If I don't need it, I don't want it, because I'm going to have to go out and find money to pay for it, or my staff has to work more.
The [potential] burden on our communities just overwhelms me; I work in a very small community … the manpower burden that we would be imposing on them. So if they came forward and said we think that we want to do this [community review] model, that's different to me. But, if we go in and say we need the CAB and now we want you also to set up this other [community review] board, and I'm working with 1400 residents total. I don't know where I'm going to find people who have that kind of time.
Education and training in basic environmental health research and ethics was also an issue for both groups. Whereas university-based research scientists focused on community education, community-based researchers and advisors indicated a need for both community- and university-based researcher education. A university-based researcher said:
The problem is getting the community educated enough to be able to have some significant input [into] the research. I am going to be blunt and brutal … to have the researcher think that their [community members'] contributions are worthwhile in terms of the design. So clearly I think a lot of researchers recognize they need the community in terms of participation and having a good relationship with the community or they are not going to be able to do their research, but I think that most researchers would say that the community does not understand enough about either the science or the mechanisms of doing research to have significant input into the design. So I think at the moment that that is a real stumbling block.
A community-based researcher commented:
You got training issues. Some researchers are engaged in the community-based work, but they are limited because their training does not … prepare them long enough to engage or interact with communities… . I think [the model] needs to involve some training about how to interact with communities. It needs to involve, you know, case studies where things went disastrously wrong. It needs to involve reverse role playing.
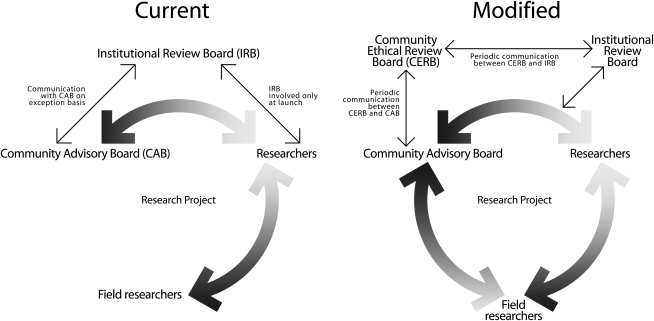
Model Development
We integrated these observations into the framework for the CERB model and refined our draft accordingly. We developed graphics for 2 research review models, 1 representative of the current institutional research review process as described in the focus group and individual interview data and the other representative of a revised community research review process that reflects the data from the dialogues.
Figure 2 provides a side-by-side view of the current research review process and the community ethical research review process.26 The CAB is either project or research-center specific, and its voluntary members are chosen by the principal investigator of the study or center during project design. They are not required to receive ethics training or human participant research certification. The CAB's purpose is to voice community concerns and interests.
FIGURE 2.
Research review models.
The Institutional Review Board
The IRB is an independent administrative arm of the university that serves as a regulatory authority for all research projects. Its members are institutional employees. Each research review committee has 1 or 2 noninstitutional members from the community that the institution compensates for their time. They are chosen by the IRB head and are required to receive the same ethics training and human participant research certification as all other institutional researchers. The IRB's purpose is to ensure compliance with the federal regulations and ethical standards, which govern human participant research, as outlined in the Belmont Report.
The Community Ethical Research Review Board
The CERB is envisioned as an independent arm of the community that will serve as a moral and ethical authority for all community-based research projects within its geographic catchments area or local community board district boundaries. Its members will include equal numbers of community residents and community stakeholders, recruited through a designated local community-based organization that receives federal funding to serve as a coordinating center for the CERB.27 Members will receive certification in human participant's research from an identified university that partners with the community-based organization, as well as environmental health research and ethics training from the community-based organization. The CERBs purpose is 4-fold: (1) to ensure that research protocols follow a CBPR approach; (2) to provide an autonomous forum for community residents, research study participants, local community-based organizations, and researchers and CAB members to raise research-related questions or concerns; (3) to provide ongoing oversight of community-based research through regularly scheduled mandatory meetings with CAB members and the IRB; and (4) to provide the community with a confidential mechanism for filing grievances and complaints about unethical research practices. It will have moral and ethical authority but, in its nascent stage, no statutory authority.
Institutional Research Review
Under the current review process, communication between the CAB and the IRB is truncated. Once a protocol receives IRB approval, there is no required interaction between the researcher and the IRB or additional review other than for modifications and renewals. The principal investigator independently assembles a CAB for each project or center and is solely responsible for its unmonitored function. CAB members may use the same mechanisms as study participants to contact the IRB with any questions or concerns that arise or to report misconduct. In theory, frontline field research workers have the same option to contact either the IRB or the CAB with any ethical issues, dilemmas, or concerns that arise in the field; in practice they are taken directly to the researchers. This creates an inherent conflict of interest, given the asymmetrical power dynamic between research scientists and the research workers they employ.
Community Research Review
The modified process for community review connects the communication circle and empowers the community, the CAB, and the frontline field research workers to identify any unanticipated ethical issues or adverse effects. The CERB differs from the IRB in 4 key regards. First, it creates a channel of unfettered communication between the CAB and the fieldworkers by establishing a direct link between the 2 groups. Under the current system, there is no formal mechanism for interaction between them. Second, it builds community capacity through education. Unlike CAB members, CERB members will be required to receive environmental-health research and ethics training. Third, it creates an independent research process and provides frequent monitoring through confidential and regularly scheduled quarterly meetings, as well as mandatory information exchange with both the CAB and the IRB. Lastly, whereas the CAB is project based and the IRB is institution based, the CERB is community based. The CERB's singular role is to shield research participants and their communities from harm.28
Key Findings
Qualitative data were used to understand the practical boundaries of the research review process and identify ways in which communities can contribute to the design, implementation, conduct, and review of environmental health research. We identified significant differences in the ethical orientation of university- and community-based participants. University-based researchers define ethical responsibility in terms of scientific advancement and compliance with human participant research regulations. They embrace the principles of CBPR in concept but not necessarily in practice because it requires time, labor, and resources. For this group, community participation is fundamentally viewed as a means to improve participant recruitment and retention rates. For community-based researchers and advisors, ethical responsibility is defined in terms of community benefits and human participant protections. Although equally concerned about the potential time and resource burden, they embrace the principles of CBPR and full community engagement in research as a means to improve community health. Both university-based and community-based participants indicated that environmental health sciences research and ethics education and training were essential to coalition building around the community review process. Mechanisms to address these issues and to provide agency and value across groups will be critical to effective community ethical research review.
DISCUSSION
Most IRBs were revamped in the wake of several high-profile cases. Between January 1999 and June 2000, the Office for Protection from Research Risks temporarily suspended federally funded research at several major academic institutions, including Duke University, Fordham University, and the University of Pennsylvania, for failing to ensure the safety of human research participants.29 In 2001, Office for Protection from Research Risks' successor, the Office for Human Research Protections, suspended research at Johns Hopkins University after an otherwise healthy research participant died.30 At that time, Johns Hopkins University had amassed the most federal funding and the most notoriety. The landmark Grimes vs Kennedy Krieger Institute, Inc, case had uncovered errors of omission and comission on the part of the Johns Hopkins University IRB in both research approval and monitoring. In that study, the participant consent forms did not clearly indicate the risk that children might be exposed to dangerous levels of lead dust particles. The consent forms also failed to mention that changes in blood lead levels over time, whether positive or negative, were being used as measures to assess the effectiveness of the lead abatement procedures. Under the auspices of the Johns Hopkins' IRB, parents were not informed in a timely manner of elevated blood lead levels in their children.31 Consequently, the Maryland Court of Appeals determined that parents can only consent to a child's participation in nontherapeutic research if there is minimal risk.32 The court's ruling included a scathing indictment of institutional research review:
The Institutional Review Boards, IRBs, are, primarily, in-house organs. In our view, they are not designed, generally, to be sufficiently objective in the sense that they are as sufficiently concerned with the ethicality of the experiments they review as they are with the success of the experiments… . Here, the IRB, whose primary function was to insure safety and compliance with applicable regulations, encouraged the researchers to misrepresent the purpose of the research in order to bring the study under the label of “therapeutic” and thus under a lower safety standard of regulation. The IRB's purpose was ethically wrong, and its understanding of the experiment's benefit incorrect.33
Recent data from the Office for Human Research Protections, Division of Compliance Oversight, demonstrate an ongoing pattern of IRB lapses. Between January 2008 and April 2009, the Division of Compliance Oversight issued final “letters of determination” to 34 institutions in which areas of noncompliance in IRB-sanctioned research had been identified. After reviewing revised IRB protocols, the division found that 8 of the 34 institutions were still in violation and would need to take further corrective action.34
Community Ethical Research Review Board Impact and Sustainability
Despite widespread institutional reforms and amplified public and governmental scrutiny, IRBs remain unable to fully safeguard disadvantaged populations and communities. This suggests intrinsic flaws in the institutional research review process. CERBs can help IRBs fulfill their increased obligation to protect the rights and welfare of human participants “[w]hen some or all of the subjects [are] … economically or educationally disadvantaged persons.”35 Moreover, community research review has the potential to impact science and health in both direct and indirect ways. In addition to augmenting IRB oversight, CERBs will increase public trust in biomedical and behavioral research in accordance with the National Institutes of Health recommendations to
encourage change in the culture of the scientific community to ensure that medical research is viewed in the context of a long-term commitment to the community, not a one-time research study; educate and reorient the current research community to the importance of treating the public as a partner in the research process; set the expectation across the entire research community, NIH-funded research and beyond, that study results and outcomes should be shared with the research participants and the larger community promptly and consistently; engage researchers, educators, and academic institutions in incorporating the public's perspective consistently at every level of training and in both the conduct of clinical research and the publication of findings from that research; focus on educational strategies to help patients and communities better understand clinical research; enhance research participation.36
Fortunately, the federal government has the capacity to leverage its substantial investment in collaborative research efforts with institutions and community stakeholders and rapidly incorporate community ethical review into the national research agenda. Community-based organizations already partnered with academic research institutions can function as CERB-coordinating centers, and identify, recruit, and educate CERB members. The Department of Health and Human Services can either establish new funding mechanisms and mandates to support and sustain CERB operational costs or draw upon existing Department of Health and Human Services–sponsored research projects. For example, the National Institutes of Health–funded Clinical and Translational Science Awards, Community Engagement Key Function Committee is currently creating a national model for community engagement. CERB development and implementation across its nationwide consortium (39 academic health centers that will expand to 60 institutions by 2012) could become part of the prototype.
Limitations
We developed a community research review board model for environmental health sciences that incorporates the diverse perspectives of research scientists, field research workers, local community residents, researchers, advisory board members, and IRB members. As with all broad studies, this one risks overgeneralization. We drew a purposeful convenience sample of NIEHS community and academic environmental justice and participatory research grantees and their affiliates. Consequently, this data set does not include the range of experience of less mainstream environmental health researchers and community-based organizations. In addition, the model's design framework will need to be modified and adapted for other types of research and may not be replicable in other research settings.37 The model's use is limited, almost exclusively, to urban academic institutions in the United States with a similarly structured research environment and review process, because it presumes a resource capacity for CBPR and for training community members to serve as research reviewers.
Conclusions
Research institutions, regulators, and scientists lack adequate methods to assess ethical challenges related to community risk and community consent. For environmental health sciences research, which seeks to understand the ways in which multiple and cumulative environmental health stressors (e.g., hazardous housing conditions, polluting industries, small- and mobile-source emissions, illegally dumped waste) negatively impact health at the community level, it is critical to ensure the safety and welfare of communities.
Currently, IRBs evaluate research involving vulnerable populations and communities using federal regulations designed to protect individual research participants. The analytic framework for research review, Ethical Principles and Guidelines for Research Involving Human Subjects, was written 3 decades ago.38 Since that time, manifold scientific advances, most notably the human genome project, coupled with the shift toward a CBPR approach, have created an imperative to extend Belmont's boundaries and expand the principles of “respect for persons, beneficence and justice,” and their applications “informed consent, risk/benefit assessment, selection of subjects of research,”39 to include community protections. CERBs are an important first step in that direction.
Acknowledgments
This work was supported by the National Institute for Environmental Health Sciences (grant 8R5ES12090A).
The authors wish to thank Lesley Green-Rennis, Liam O'Fallon, Gwen Collman, and Scott Sherman; Team WE ACT, in particular Evelyn Joseph, Ogonnaya Dotson-Newman, Anhthu Hoang, and Ursula N. Embola; all the study participants who shared their invaluable insights with us; and Richard V. Miller, Columbia University Department of Biomedical Communications, who did the graphic design for the Community Ethical Review Models.
Human Participant Protection
The research was conducted under the Columbia University institutional review board.
Endnotes
- 1. Brown, D. R., and M. Topcu. 2003. Willingness to participate in clinical treatment research among older African Americans and Whites. Gerontologists 43(1):62–72. Dekonig, K., and M. Martin. 1996. Participatory research in health: issues and experiences. London, England: Zed Books. Hughes, G. D., Sellers, D. B., Fraser, L. B., Jr, Knight, B., and G. A. Areghan. 2003. Barriers and strategies for sustained participation of African American men in cohort studies. Ethn Dis 13:534–536. [PubMed]
- 2.Vasquez V.B, Minkler M, P Shepard. 2006. Promoting environmental health policy through participatory research: a case study from Harlem, New York. J Urban Health 83(1):101–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. See, for example, the work of Israel, B. A., Schurman, S. J., and J. S. House. 1989. Action research on occupational stress: involving workers as researchers. Int J Health Sci 19(1):135–155; Israel, B. A., Schurman, S. J., and M. K, Hugentobler. 1992. Conducting action research: relationships between organization members and researchers. J Appl Behav Sci 28:74–101; Israel, B., et al. 1994. Health education and community empowerment: conceptualizing and measuring perceptions of individual, organizational, and community control. Health Edu 21:149–170; Hatch, J., et al. 1993. Community research: partnership in Black communities. Am J Prev Med 9(suppl):27–31; Mittelmark, M., et al. 1993. Realistic outcomes: lessons from community-based research and demonstration programs for the prevention of cardiovascular diseases. J Public Health Policy 14:437–462.
- 4. See Division of Extramural Research and Training, National Institute of Environmental Health Sciences. May 15, 2000. Environmental Justice Program Evaluation Report.
- 5. Strauss, R. P., Sengupta, S., Quinn, S. C., et al. 2001. The role of community advisory boards: involving communities in the informed consent process. Am J Public Health 91(12):1938–1943. Foster, M. W., Sharp, R. R., Freeman, W. L., Chino, M., Bernstein, D., and T. H. Carter. 1999. The role of community review in evaluating the risks of human genetic variation research. Am J Hum Genet. 64:1719–1727.
- 6. Green, L. W., and S. L. Mercer. 2001. Can public health researchers and agencies reconcile the push from funding bodies and the pull from communities? Am J Public Health 91(12):1926–1929; Israel, B. A., Schulz, A. J., and E. A. Parker. 1998. Review of community-based research: assessing partnership approaches to improve public health. Ann Rev Public Health 19:173–202; Israel, B. A., Schulz, A. J., and E. A. Parker. 2001. Community-based participatory research: policy recommendations for promoting a partnership approach in health research. Edu Health 14(2):182–197.
- 7. Beskow, L., et al. 2001. Informed consent for population based research involving genetics. JAMA 286:2315; Weijer, C., and E. J. Emanuel. 2000. Protecting communities in biomedical research. Science 289:1142; Coleman C. H., Menikoff J. A., and J. A. Goldner, et al. 2005. The Ethics and Regulation of Research with Human Subjects. Newark, NJ: Matthew Bender Co:3–50.
- 8.Shepard P M, Northridge M E, Prakash S, G Stover. 2002. Preface: advancing environmental justice through community-based participatory research. Environ Health Perspect 110(2):139–14011836141 [Google Scholar]
- 9. O'Fallon, L. R, and A. Dearry. 2001. Community-based participatory research as a tool to advance environmental health sciences. Environ Health Perspect 110(suppl 2):155–159. Olden, K., Guthrie, J., and S. Newton. 2001. A bold new direction for environmental health research. Am J Public Health. 2002;91:1964–1967. [DOI] [PMC free article] [PubMed]
- 10. One of the first environmental organizations in New York State to be run by people of color, and the first environmental justice organization in New York City, WE ACT was founded and incorporated in 1988 as the result of local community struggles around environmental threats and resulting health disparities created by institutionalized racism and the lack of social and political capital, all dynamics that led to the siting and poor management of the North River Sewage Treatment Plant, the siting and operation of 6 out of 7 New York City diesel bus depots in northern Manhattan, the operation in our community of the only 24-hour Marine Transfer Station in Manhattan, the use of northern Manhattan communities as New York City's dumping ground, and the exclusion of communities of color from democratic decision making. In 1988, WE ACT sued the NYC Department of Environmental Protection for operating the North River Sewage Treatment Plant as a public and private nuisance. The lawsuit was settled in 1994 for $1.1 million, and WE ACT hired its first 3 staff members with a grant from the settlement funds. Today, WE ACT has 17 full-time staff members.
- 11.Cole L, S Foster. 2001. From the Ground Up: Environmental Racism and the Rise of the Environmental Justice Movement. New York: New York Univ Press [Google Scholar]
- 12. See Bryant, B. 2002. Environmental Advocacy: Working for Economic and Environmental Justice. In Bullard, R., ed. 1993. Confronting environmental racism: voices from the grassroots. Boston: South End Press; Mohai, P., and B. Bunyan, eds. 1992. Race and the Incidence of Environmental Hazards: A Time for Discourse. Boulder: Westview Press.
- 13. In 1990, the University of Michigan held a conference on Race and the Incidence of Environmental Hazards, which gave rise to a monograph on environmental justice case studies and the Office of Environmental Equity at the Environmental Protection Agency. See Bullard, 1993, ibid.
- 14. Ibid.
- 15. President William J. Clinton. February 11, 1994. Executive Order 12898—Federal Actions to Address Environmental Justice in Minority Populations and Low-Income Populations. The White House. 59 F.R. 7629. February 16, 1994. See Bullard, op. cit. note 12.
- 16.Institute of Medicine 1999. Toward Environmental Justice: Research, Education and Health Policy Needs. Washington, DC: Institute of Medicine [Google Scholar]
- 17. Ibid.; op. cit. note 12; Executive Order 12898, op.cit. note 15; Bonorris, S., Isaacs, J., and K. Brown, eds. 2004. Environmental Justice for All: A Fifty-State Survey of Legislation, Policies, and Initiatives. San Francisco: Section of Individual Rights and Responsibilities American Bar Association, Section of Environment, Energy and Resources, Public Law Research Institute Hastings College of the Law, University of California.
- 18. Dialogues are moderator-guided group conversations that facilitate the exploration of diverse perspectives, because the voice of each discussant is afforded equal value. Instead of research questions, a topical guide is used to minimize the moderator's intervention in the discussion and allow for unfettered exchange among participants. At the core of the dialectical transformation are the perceptions of discussants, their thoughts and actions, ambivalence, and concerns. Thus, in exploring the potential issues associated with community review in environmental health research, and the ways to address these issues, discussants reflect on the concept and design of the model and its potential ethical dilemmas and challenges.
- 19.Carter S, L Henderson. 2005. Approaches to Qualitative Data Collection in Social Science. Bowling A., Ebrahim S., Handbook of health research methods: investigation, measurement and analysis, 215–230. Maidenhead, England: Open University Press, McGraw-Hill Education [Google Scholar]
- 20. Ibid.
- 21.DeMaio T J, J M Rothgeb. 1996. Cognitive Interviewing Techniques: In the lab and in the Field. Answering questions: methodology for determining cognitive and communicative processes in survey research, 177–195 San Francisco: Jossey-Bass [Google Scholar]
- 22.Strauss A, J Corbin. 1998. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks: Sage Publications [Google Scholar]
- 23.Muhr T. 2004. Atlas, ti v5.2. Berlin: Scientific Software Development [Google Scholar]
- 24. Op. cit. note 19.
- 25.Donovan J, Sanders S. 2005. Issues in the Analysis of Qualitative Data in Health Services Research. In Handbook of health research methods: investigation, measurement and analysis, 515–533. Maidenhead, England: Open University Press, McGraw-Hill Education [Google Scholar]
- 26. It is important to note that the communication-flow circle is specific to each research project or research center.
- 27. In all likelihood, a community partner of one of the local academic institutions would be designated as the coordinating site for each fiscal year. Regardless, at least 1 member of each local institution's community partner would serve on the board.
- 28. We envision each CERB covering 6 to 8 community districts, depending on population density. In New York City, Manhattan and the Bronx each contain 12 community districts, whereas the more-heavily populated boroughs of Queens and Brooklyn contain 14 and 18, respectively, and Staten Island contains 3. Each community district comprises health areas that are aggregates of census tracts, thus allowing for analysis of publicly available health data.
- 29. See http://www.ahrp.org/ethical/govInvestigations.php (accessed May 14, 2009)
- 30. See http://www.ahrp.org/infomail/0701/19.php (accessed May 14, 2009)
- 31. Grimes vs Kennedy Krieger Institute, Inc, 782 A.2d 807 (MD 2001). Available at: http://www.courts.state.md.us/coa/2001/128a00.pdf (accessed June 18, 2009)
- 32. This decision has not garnered the full support of the research community. See: Hoffman, D., and K. Rothenberg. 2002. Whose duty is it anyway? The Kennedy Krieger opinion and its implications for public health research. J Health Care Law Policy 6:109–147. Kopelman, L. M. 2002. Group benefit and protection of pediatric research subjects: Grimes v Kennedy Krieger and the lead abatement study. Account Res 9(3–4):177–192. Pearce, M. 2002. Children as subjects in nontherapeutic research: Grimes v Kennedy Krieger Institute, Inc. J Legal Med. 23:421–436. Pinder, L. 2002. Commentary on the Kennedy Krieger Institute Lead Paint Repair and Maintenance Study. Neurotoxicol Teratol 24:477–479. Nelson, R. M. Non-therapeutic research, minimal risk, and the Kennedy Krieger lead abatement study. IRB 23:7–11. Pollak, J. 2002. The lead-based paint abatement repair and maintenance study in Baltimore: historic framework and study design. J Health Care Law Policy 6:89–108. Ross, L. 2002. In defense of the lead abatement studies. J Law Med Ethics 30:50–57.
- 33. Ibid., at 11–12.
- 34. Personal communication between B. X. W. and Lisa Buchannan, Division of Compliance Oversight (DCO), June 2009. See http://www.hhs.gov/ohrp/compliance/letters/index.html (accessed June 10, 2009). These data are based upon a manual review by B. X. W. of all of the “letters of determination” issued during this time period. DCO opens a case when it finds areas of noncompliance in HHS-sponsored research and requires an institution to take corrective action to meet federal standards under 45 CFR, section 46. The 35 letters represent cases where the Office of Human Research Protections (OHRP) found areas of noncompliance after review and required corrective actions that have now undergone evaluation. For the most part, (with the exception of the 8 cases requiring additional corrective action) the DCO issued these letters to acknowledge that the corrective actions taken by the noncompliant institutions were sufficient and the case is closed. Hence, many of the 35 cases were opened prior to 2008 and 2009 as DCO estimates average case turnaround time at approximately 6 months. During this same period, DCO opened a new case of institutional noncompliance and placed nine more allegations under review. (In the text, I refer to 34 cases, and in this note, I refer to 35. This is because 1 case was deferred to the FDA for oversight.)
- 35. Criteria for IRB approval of research, 45 C.F.R. section 46.11145 CFR §46, subpart A (the Common Rule)
- 36.Council of Public Representatives 2005. Report and Recommendations on Public Trust in Clinical Research for the NIH Director. Bethesda: National Institutes of Health; Also see Kass N. E., Sugarman J., Faden R., et al. Trust, the fragile foundation of contemporary biomedical research. Hastings Cent Rep 26(5):25–29 [PubMed] [Google Scholar]
- 37. For example, in clinical research projects in which the data reporting goes to the IRB but also goes to a data safety monitoring board that then has to report to the research sponsor, the model is inadequate.
- 38.The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research 1979. The Belmont Report: Ethical Principles and Guidelines for Research Involving Human Subjects. Washington DC: The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research [Google Scholar]
- 39. Ibid.