Abstract
Objectives. As part of a community-based participatory research effort, we estimated the preventable burden of childhood asthma associated with air pollution in the southern California communities of Long Beach and Riverside.
Methods. We calculated attributable fractions for 2 air pollution reduction scenarios to include assessment of the newly recognized health effects associated with residential proximity to major roads and impact from ship emissions.
Results. Approximately 1600 (9%) of all childhood asthma cases in Long Beach and 690 (6%) in Riverside were attributed to traffic proximity. Ship emissions accounted for 1400 (21%) bronchitis episodes and, in more modest proportions, health care visits for asthma. Considerably greater reductions in asthma morbidity could be obtained by reducing nitrogen dioxide and ozone concentrations to levels found in clean coastal communities.
Conclusions. Both Long Beach and Riverside have heavy automobile traffic corridors as well as truck traffic and regional pollution originating in the Los Angeles–Long Beach port complex, the largest in the United States. Community-based quantitative risk analyses can improve our understanding of health problems and help promote public health in transportation planning.
Community groups in southern California have been increasingly concerned about the health effects of exposure to some of the highest levels of urban air pollution in the United States. Statewide risk assessments have concluded that substantial cardiovascular and respiratory disease mortality and large numbers of cardiorespiratory emergency visits and hospitalizations, asthma exacerbations, and chronic bronchitis are attributable to high levels of particulate matter and ozone (O3).1,2 However, only rarely has this methodology been applied to smaller geographical scales taking into account local air pollution conditions and sources.
Information about the local health burden of air pollution would be useful for evaluating proposals to expand port facilities and transportation infrastructure in the Los Angeles air basin. Expansion at the adjacent ports of Long Beach and Los Angeles, the largest port complex in the country, has resulted in an increasing contribution to the region's air pollution. Air emissions from ships, yard equipment, railroads, and trucks account for about 10% of the daily particulate matter, 24% of nitrogen oxides, and 73% of the daily sulfur oxides in the entire Los Angeles air basin.3 Ship emissions alone contribute substantially to coastal and inland air pollution.4 A doubling or tripling of cargo through the region by 2025 is predicted,5,6 threatening decades of progress in reducing levels of air pollution.
As part of a community-based participatory research effort to provide information that could help communities evaluate plans for port expansion, we estimated the burden of childhood asthma attributable to air pollution in the southern California cities of Long Beach (population 136 000) and Riverside (population 76 500). Residents from these communities have challenged port expansion on the basis of concerns about the health effects of ship emissions and of traffic proximity, which have not been well characterized in prior health risk assessments.7,8
Novel features of our effort include an assessment of the impact of residential proximity to major roads on the burden of childhood asthma. Recent research suggests that traffic proximity is not only associated with severity and persistence of asthma in children but also with increased risk of asthma onset.9–11 In addition, we have evaluated the burden of childhood asthma attributable to ship emissions as an example of a specific source of port-related pollution effects.
METHODS
We quantified the number of yearly childhood asthma-related illnesses that could be prevented if air quality were improved in the Long Beach and Riverside communities by deriving population-attributable risk fractions. The derivation of population-attributable risk fractions combines several elements. These include the concentration–response functions (CRFs; the quantitative association between markers of air pollution and selected outcomes derived from epidemiological studies), the frequency of health conditions in the population of interest, the current population exposure to the markers of air pollution selected, and the population exposure hypothesized after scenarios of air pollution reduction.
The CRFs for the outcomes selected for this study are shown in Table 1. Choice of outcomes was limited by the availability of the frequency of health conditions for the population under study. We based the CRFs for bronchitis episodes among those with asthma, and lifetime asthma, on the southern California Children's Health Study (CHS), a large population-based study of air pollution and respiratory health, which included the Long Beach and Riverside areas.17 For other outcomes, appropriate studies had not been conducted in southern California populations, so we selected CRFs if they had been used in previous peer-reviewed health impact assessments or were conducted in populations similar to the populations under study. If these criteria could not be met, recent studies were preferred over older studies. We tested the comparability of results by using alternative CRFs for these outcomes in uncertainty analyses. The statistical models used to derive CRFs most often provide odds ratios (ORs) from logistic regression models rather than relative risks. To control for overestimation of the ORs for frequent events, we corrected ORs with a standard formula.18,19 Table 1 presents published and corrected CRFs.
TABLE 1.
Health Outcomes and Concentration Response Functions (CRFs) Among Children: Long Beach and Riverside, CA
| Outcome | Unit of CRF | Age, y | CRF (95% CI) | Corrected CRF (95% CI) | Study |
| Bronchitis episodes among those with asthma | |||||
| NO2 | 1 ppb (24-h annual average) | 9–13 | 1.070 (1.020, 1.130) | 1.042 (1.012, 1.076) | McConnell et al.12 |
| O3 | 1 ppb (10:00 am–6:00 pm average) | 9–13 | 1.060 (1.000, 1.120) | 1.057 (1.000, 1.113) | McConnell et al.12 |
| Clinic visits for asthma | |||||
| NO2 | 24 ppb (24-h average) | 0–14 | 1.061 (1.012, 1.113) | 1.055 (1.011, 1.102) | Hajat et al.13 |
| O3 | 50 ppb (24-h average) | 2–14 | 1.054 (1.013, 1.096) | 1.049 (1.012, 1.086) | Ostro et al.14 |
| Emergency department visits for asthma | |||||
| NO2 | 50 μg/m3 (27 ppba) (24-h average) | ≤15 | 1.026 (1.006, 1.049) | 1.024 (1.006, 1.045) | Sunyer et al.15 |
| O3 | 10 ppb (daily 1-h max) | 1–16 | 1.024 (1.015, 1.033) | 1.022 (1.014, 1.030) | Ostro et al.2 |
| Hospital admissions for asthma | |||||
| NO2 | 27.1 μg/m3 (14.4 ppba) (24-h average) | ≤15 | 1.079 (1.054, 1.090) | 1.079 (1.054, 1.090) | Lee et al.16 |
| O3 | 23 μg/m3 (11.5 ppbb) (8-h mean) | ≤15 | 1.060 (1.041, 1.079) | 1.060 (1.041, 1.079) | Lee et el.16 |
| Prevalent asthma: traffic exposure | Living < 75 m from busy road for long-term residents | 5–7 | 1.64 (1.10, 2.44) | 1.515 (1.086, 2.059) | McConnell et al.10 |
Note. CI = confidence interval; NO2 = nitrogen dioxide; O3 = ozone. Published CRFs were corrected with the formula CRF/[1+It(CRF-1)], where It is the frequency of the outcome in the population.
Conversion factor for NO2: 1 ppb = 1.88 μg/m3.
Conversion factor for O3: 1 ppb = 2 μg/m3.
Burden of disease was estimated for nitrogen dioxide (NO2) and O3, which were available for both risk assessment scenarios we considered. Nitrogen dioxide has been found to have a regional distribution and effects across southern California communities similar to that for particulate pollution.20 There are high levels of NO2 in Long Beach and of both NO2 and O3 in Riverside. In Long Beach, NO2 is generated largely by combustion emissions from automobiles and other mobile sources related to goods movement (i.e., ships, harbor craft and other vehicles at the port, and rail and truck traffic). Ozone is a product of atmospheric photochemistry, heavily influenced by upwind emissions of primary air pollutants (such as those from the port and vehicular traffic). Dominant regional wind trajectories transport emissions from the port communities (including Long Beach) to the Riverside area, approximately 50 miles inland4 (see the figure available as a supplement to the online version of this article at http://www.ajph.org).
The Riverside area is also one of several communities that has undergone rapid development to accommodate increased population and to facilitate cargo processing from the ports in large mega-warehouses before redistribution to the rest of the country, resulting in heavy truck and automobile traffic. Current community population exposures were estimated from the 8-year mean concentration (1996–2004) of NO2 and O3 measured at continuously operating CHS monitoring stations in each community.4,17 The frequency of health conditions in the population of interest and exposure levels in the 2 communities are shown in Table 2.
TABLE 2.
Population Baseline Frequencies and Exposure Data Among Children: Long Beach and Riverside, CA
| Description | Long Beach, CA | Riverside, CA | Data Source |
| Population or baseline frequencies | |||
| Total population of children aged 0–17 y | 136 181 | 76 491 | 2000 US Census Bureau |
| Fraction of children with asthma (prevalence)a | 0.1284 | 0.1488 | CHSb |
| Fraction of children with asthma with reported bronchitis symptomsc | 0.387 | 0.387 | McConnell et al.12 |
| Fraction of children with reported clinic visits for asthmad | 0.710 | 0.7521 | CHSb |
| Fraction of children with asthma with reported emergency department visits for asthmae | 0.581 | 0.3793 | CHSb |
| Number of hospital admissions for asthma (ICD-9, 493) | 264 | 120 | California Breathing, 2003f |
| Fraction of children living < 75 m from busy roads | 0.199 | 0.1291 | Methods based on Künzli et al.21 |
| Population exposure—current conditions | |||
| NO2 | 33 ppb | 26 ppb | CHS Web page17 |
| O3 | 29 ppb | 57 ppb | CHS Web page17 |
| Exposure reduction from current levels | |||
| Scenario 1: no ship emissions | |||
| NO2 | −5.9 ppb | −2.0 ppb | Vutukuru and Dabdub4 |
| O3 | Not considered | Not considered | |
| Scenario 2: clean communities | |||
| NO2 | −18 ppb | −11 ppb | Clean CHS communities17 |
| O3 | Not considered | −27 ppb | Clean CHS communities17 |
Note. CHS = Children's Health Study; ICD-9 = International Classification of Diseases, Ninth Revision.22
Defined as use of controller medications for asthma in previous year or physician-diagnosed asthma with any wheeze in previous year.
CHS, unpublished data; R. McConnell, MD, University of Southern California, Los Angeles, written communication, 2008.
Defined as daily coughs for 3 months in a row, congestion or phlegm for at least 3 months in a row, or bronchitis. Average 12 CHS communities.
Based on answer to the question, “Has your child ever been to a doctor for wheezing?” among those that have ever had wheezing or whistling.
Based on answer to the question, “Has your child ever been to an emergency room or a hospital for wheezing?” among those that have asthma.
California Breathing, unpublished data, 2003; Environmental Health Investigations Branch, written communication, California Department of Health Services, 2008.
Exposure-Reduction Scenarios
We provided estimates for 2 scenarios of exposure reduction. Scenario 1 quantified the burden of disease related to the contribution from ships alone while ignoring all other port-related activities. This scenario was based on a recent study that modeled the impact of emissions from ocean-going ships on NO2 concentrations during episodic conditions in southern California.4 Ship emissions were estimated to contribute 5.9 ppb and 2 ppb of NO2 in Long Beach and Riverside, respectively.4 (Although the contribution of ship emissions to O3 was also estimated from this study, the episodic conditions were appropriate only for estimating the contribution to long-term NO2 exposure.)
Scenario 2 estimated the reduction in disease that would result if NO2 levels were reduced to concentrations present in the cleaner coastal southern Californian communities (about 15 ppb).17 Under this scenario, current population exposure to NO2 would have to be lowered by 18 ppb and 11 ppb in Long Beach and Riverside, respectively. For O3, we assumed that the annual 8-hour mean concentration would be decreased to 30 ppb, corresponding to a 27 ppb exposure reduction in Riverside. Because of chemical reactions with high concentrations of nitrogen oxide, O3 levels in Long Beach are, on average, lower than levels found in many coastal communities. Thus, O3 burden was not evaluated for Long Beach. Population exposure under the 2 exposure-reduction scenarios considered are presented in Table 2.
The CHS and other recent studies have demonstrated associations between living close to busy roads and asthma prevalence.10,11,23 For the asthma prevalence attribution, we used the CRF determined in a previous CHS study demonstrating an association with a busy road within 75 meters of children's homes.10 The detailed methods used to derive the number of children living within 75 meters of a busy road are described elsewhere.9 The census block population was uniformly assigned to grids representing households, and the distance from the nearest major road to these grids was assigned by using geo-referenced software tools (ArcGIS Version 9.2, ESRI, Redland, CA). As an exposure-reduction scenario, we assumed that the current number of children living in the first 75 meters of busy roads would be reduced to zero, or that the high concentrations of toxicants along traffic arteries would fall to levels existing in areas more than 75 meters from busy roads.
The attribution of prevalent cases of asthma to residential traffic proximity has substantial implications for the burden of asthma-related exacerbation caused by air pollution. If air pollution increases risk of developing asthma, then all acute future consequences of having asthma should be attributed to air pollution in those individuals, regardless of subsequent causes of exacerbations.21 Therefore, we extended our analysis to account for the burden of asthma associated with these effects by using recently published methods.9 First, the number of asthma cases associated with living close to busy roads was estimated. Then, for each regional pollutant scenario, we estimated the yearly number of each asthma-related exacerbation outcome because of all causes (not just air pollution) among these cases by using the attributable-fraction formula.
For each regional pollutant scenario, we also estimated the yearly number of each respiratory outcome attributable to pollution among children with asthma not attributable to traffic proximity, a standard approach in health risk assessment of regional pollutant effects. These estimates were then added to the number of asthma exacerbations among children with asthma attributable to traffic proximity to obtain the total number of each exacerbation attributable to air pollution.
Sensitivity Analyses
To reflect statistical uncertainty, results are presented with both a point estimate and an upper and lower bounds corresponding to the 95% confidence interval of the CRF. We used Monte Carlo simulations to generate uncertainty distributions for outcomes that required combining 2 sets of CRFs when taking into account asthma onset caused by living close to busy roads. Several steps of the risk analysis have assumptions and uncertainties that limit our results. These limitations are addressed in the “Discussion” section. We also conducted a series of additional sensitivity analyses to illustrate the impact on our estimates of alternative approaches.
RESULTS
Approximately 1600 cases of childhood asthma in Long Beach (9% of all cases) and 690 in Riverside (6% of all cases) were attributable to traffic proximity (Table 3), on the basis of evidence that living close to busy roads causes new-onset asthma. These local traffic proximity effects are independent of the effects of regional pollutants and so were the same for each regional pollutant scenario.
TABLE 3.
Number of Outcomes Attributable to Air Pollution Per Year Among Children: Long Beach and Riverside, CA
| Scenario 1: No Ship Emissions |
Scenario 2: Clean Communities |
||||||||
| Attributable to Air Pollution, No. (95% CI) | Attributable to Other Causes,a No. (95% CI) | Totalb |
Attributable to Air Pollution, No. (95% CI) | Attributable to Other Causes,a No. (95% CI) | Totalb |
||||
| Community and Outcome | Baseline Estimate, No. | No. Cases (95% CI) | % (95% CI) | No. Cases (95% CI) | % (95% CI) | ||||
| Traffic exposure | |||||||||
| Long Beach: asthma cases | 17 486 | 1600 (1500, 1800) | NA | 1600 (1500, 1800) | 9.2 (8.6, 10.3) | 1600 (1500, 1800) | NA | 1600 (1500, 1800) | 9.2 (8.6, 10.3) |
| Riverside: asthma cases | 11 382 | 690 (630, 750) | NA | 690 (630, 750) | 6.1 (5.5, 6.6) | 690 (630, 750) | NA | 690 (630, 750) | 6.1 (5.5, 6.6) |
| NO2 | |||||||||
| Long Beach | |||||||||
| Bronchitis episodes among those with asthma | 6767 | 1400 (400, 2300) | 500 (400, 600) | 1900 (980, 2700) | 28.1 (14.5, 39.9) | 3400 (1200, 4900) | 310 (170, 530) | 3700 (1700, 5100) | 54.7 (25.1, 75.4) |
| Emergency room visits for asthma | 10 166 | 54 (7, 100) | 940 (860, 1020) | 1000 (910, 1100) | 9.8 (9.0, 10.8) | 160 (20, 300) | 930 (860, 1000) | 1100 (950, 1200) | 10.8 (9.3, 11.8) |
| Clinic visits for asthma | 12 410 | 160 (30, 290) | 1100 (1000, 1200) | 1300 (1200, 1400) | 10.5 (9.7, 11.3) | 500 (90, 860) | 1100 (1000, 1200) | 1600 (1200, 2000) | 12.9 (9.7, 16.1) |
| Hospital admissions for asthma | 264 | 10 (8, 12) | 24 (22, 26) | 34 (31, 36) | 12.9 (11.7, 13.6) | 30 (24, 35) | 22 (20, 24) | 51 (46, 57) | 19.3 (17.4, 21.6) |
| Riverside | |||||||||
| Bronchitis episodes among those with asthma | 4405 | 340 (90, 590) | 250 (220, 270) | 590 (350, 820) | 13.4 (7.9, 18.6) | 1600 (470, 2400) | 170 (120, 240) | 1700 (710, 2500) | 38.6 (16.1, 56.8) |
| Emergency room visits for asthma | 4317 | 8 (1, 15) | 260 (240, 280) | 270 (240, 290) | 6.3 (5.6, 6.7) | 42 (5, 73) | 260 (240, 280) | 300 (260, 340) | 6.9 (6.0, 7.9) |
| Clinic visits for asthma | 8560 | 40 (7, 70) | 510 (470, 560) | 550 (500, 600) | 6.4 (5.8, 7.0) | 200 (40, 370) | 500 (460, 550) | 710 (550, 870) | 8.3 (6.4, 10.2) |
| Hospital admissions for asthma | 120 | 2 (1, 2) | 4 (4, 4) | 6 (5, 6) | 5.0 (4.2, 5.0) | 8 (7, 10) | 4 (3, 4) | 12 (11, 14) | 10.0 (9.2, 11.7) |
| Ozone | |||||||||
| Riverside | |||||||||
| Bronchitis episodes among those with asthma | 4405 | NC | NC | NC | NC | 3100 (170, 4200) | 80 (14, 250) | 3200 (420, 4200) | 72.6 (9.5, 93.3) |
| Emergency room visits for asthma | 4317 | NC | NC | NC | NC | 250 (160, 330) | 245 (223, 267) | 508 (417, 595) | 11.8 (9.7, 13.8) |
| Clinic visits for asthma | 8560 | NC | NC | NC | NC | 220 (20, 410) | 250 (220, 270) | 490 (410, 580) | 5.7 (4.8, 6.8) |
| Hospital admissions for asthma | 120 | NC | NC | NC | NC | 12 (9, 16) | 4 (3, 4) | 16 (13, 19) | 13.3 (10.8, 15.8) |
Note. CI = confidence interval; NA = not applicable; NC = not considered. Uncertainty distributions obtained by Monte Carlo simulations.
Among those with asthma caused by pollution.
Not to be summed from other columns.
Without taking into account the impact of traffic-induced asthma, we estimated that eliminating ship emissions would result in reduction of the number of asthma-related bronchitis episodes among those with asthma by 1400 (21% of all cases) in Long Beach and 3400 (8% of all cases) in Riverside, and that total number of health care facility visits, including emergency room visits, clinic visits, and hospital admissions, would decrease by 224 (1% of all visits) in Long Beach and 50 (0.4%) in Riverside (see the first column under scenario 1 in Table 3). Further reduction of NO2 concentrations to levels found in clean communities in Southern California would result in corresponding reductions in asthma exacerbation that are 3- to 5-fold those observed in scenario 1 (see first column under scenario 2 in Table 3). For example, if NO2 were reduced to levels found in clean communities, 3400 bronchitis episodes in Long Beach (50% of all episodes) and 1600 in Riverside (36% of all episodes) could be prevented. Ozone reduction in Riverside to background levels would reduce the number of bronchitis episodes among those with asthma by 3100 (70% of all episodes), and the number of health care facility visits for asthma by 482 (4% of all visits).
There was substantial impact of residential traffic proximity on asthma exacerbation, because exacerbation of asthma from any cause was attributable to traffic proximity among children who would not have developed asthma if they did not live near busy roadways. For example, the preventable proportion of bronchitis episodes increased from 1400 (21% of all episodes) to 1900 (28% of all episodes) in Long Beach (third column under scenario 1 in Table 3) and from 3400 (50% of all episodes) to 3700 (55% of all episodes; third column under scenario 2 in Table 3), after accounting for effects of NO2 among children with asthma attributed to traffic proximity. The biggest relative impact of traffic proximity–attributable asthma on exacerbation was for asthma-related clinic visits, emergency department visits, and hospital admissions.
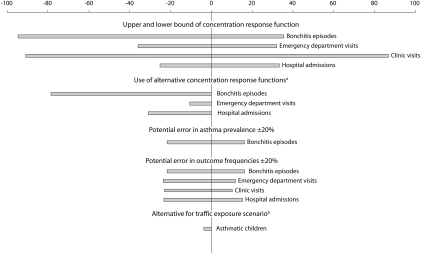
Figure 1 shows selected sensitivity analyses for Riverside, which were conducted to evaluate the impact of assumptions made in the primary analyses and the associated uncertainty. The uncertainty is expressed as a percent change from estimates in Table 3 for cases attributable to O3 and for asthma cases caused by traffic proximity. The 95% confidence interval of the CRF is the source of large uncertainty; however, the available CRFs for the outcomes considered in this study were limited. The upper and lower bounds range around plus or minus 30% for hospital admissions and plus or minus 90% for clinic visits. Large bounds were also found for cases attributable to NO2 (results not shown).
FIGURE 1.
Sensitivity analysis examining uncertainty of results for number of cases of asthma exacerbation attributable to ozone (O3) and for number of cases of asthma attributable to traffic proximity in Riverside, CA.
Note. Uncertainty is expressed as the percentage change from estimates.
aReferences for alternative concentration response function are Delfino et al.24 for bronchitis episodes, Tolbert et al.25 for emergency department visits, and Sheppard et al.26 for hospital admissions.
bDifference in air pollution–attributable asthma cases with a reduction scenario assuming that 5% of the population will remain living within 75 m of busy road instead of 0% as in the core estimates.
Figure 1 also shows the impact of using alternative CRFs, which were generally less influential than statistical uncertainty but had important effects for some outcomes. For O3, bounds varied between −10% for emergency room visits and −80% for bronchitis episodes. Error in asthma prevalence (±20%) assumed for the risk assessment and in outcome incidence (±20%) had relatively modest impact on estimates of the burden of bronchitis, emergency room visits, and other outcomes, compared with other uncertainties. The plus or minus 20% error in outcome frequencies was selected to include a plausible range of diagnostic misclassification. For example, asthma frequencies in the CHS varied depending on alternative definitions of asthma, which was 14% if defined as physician-diagnosed asthma; 13% if defined as current severe symptoms and use of controller medications, or lifetime asthma with current wheeze; and 15% if defined as current wheeze during the previous year.10
Finally, Figure 1 shows the impact on asthma prevalence of a reduction scenario in which 5% of the Riverside population were assumed to live within 75 meters of a busy road instead of 0% as in the primary analysis. In this case, the proportion of all Riverside asthma cases attributable to air pollution would be only 4% lower than the primary estimate. However, this modest difference would have important impacts on the number of superimposed acute exacerbations attributable to reduction of regional air pollutants.
DISCUSSION
This health risk assessment was undertaken to provide credible estimates of the burden of air pollution-attributable childhood asthma for community groups concerned about the impact of the continued expansion of goods movement in southern California. We focused on childhood asthma, because its importance has been underappreciated in traditional risk assessment, and this study is one of the first, to our knowledge, to estimate the population burden of asthma and asthma exacerbation caused by traffic proximity. Our results indicate that heavy traffic corridors in Long Beach and Riverside are responsible for a large preventable burden of childhood asthma prevalence, accounting for 6% to 9% of all cases of this most common chronic disease of childhood. Ozone from upwind sources and NO2 from ships and from both regional and local sources were responsible for a significant burden of asthma exacerbation. Asthma cases attributable to traffic proximity had a large impact on the total burden of exacerbations, especially for common outcomes with weak (or no) association with regional air pollution in previous studies, because no exacerbation would have occurred in these children had asthma not developed because of residential traffic proximity.
The contribution of goods movement through the port to the burden of childhood asthma is difficult to quantify. However, the morbidity associated with ship emissions alone indicates that the port is an important contributor to the public health impact of air pollution in the Los Angeles basin. Port expansion has been promoted as an “economic engine” for the region,6 and there are currently several large transportation infrastructure development projects underway to facilitate the expected increase in goods moving through the region to the rest of the country.
However, there has been only limited formal evaluation of the health impact of this development, and a comprehensive assessment of health costs has not been weighed against the potential benefit. Such an assessment would currently not be possible for specific downwind communities such as Riverside, because no model is available to estimate the contribution of all port activities to exposure to secondary pollutants in specific areas. Nevertheless, in a community already identified as having poor air quality, port-related growth is likely to contribute disproportionately to the pollution-related burden of disease, compared with projected changes in automobile pollution, which currently accounts for most regulated regional pollutants. Regulation of ship, locomotive, and truck emissions has lagged behind that for automobiles. Moreover, increased expansion of cargo distribution centers in the Riverside area and associated influx of heavy duty diesel trucks carrying containers to warehouses will likely result in increased truck traffic on major roads in proximity to homes.
Transportation planning in local communities requires local information to develop effective policies, because state and national estimates of air pollution–related burden of disease that average effects over a large population are not adequate for evaluating local health impact in areas with high pollution. Although this study provides an example of how local health risk assessment might fill this need, our results underestimate the impact of air pollution. In addition, asthma morbidity results in impaired quality of life for the affected child and other family members. School and corresponding work absenteeism and the added use of health care facilities because of air pollution also have an important impact on local economies.27,28 World Health Organization guidelines list a range of other health outcomes that could be considered in children, including infant mortality, effects on birthweight, and bronchitis among those who do not have asthma.29 Air pollution also may cause other adverse birth outcomes, cardiorespiratory ailments in adults, and lung cancer. In a recent health risk assessment in the port area, the largest carcinogenic risk from exposure to diesel and other air toxics in the Los Angeles air basin occurred in Long Beach area.30,31
Large statistical uncertainty of the CRFs and their limited availability for asthma-related outcomes affects the certainty of our results, as shown in Figure 1. Additional epidemiological studies for the outcomes and populations considered would be useful to generate more accurate CRFs. Several other limitations and uncertainties may affect our estimates. Scenario 2 provided a more complete assessment of the burden of childhood asthma exacerbation attributable to air pollution because the reference levels were from clean coastal communities. Models of the regional consequences of primary emissions from the port and from port-related goods movement are still incomplete, but it is clear that even if there were no port emissions, the levels of pollution in the study communities would not be reduced to “clean” levels.
We used regional air pollution exposure estimates that did not incorporate the children's location and activity patterns in the assessment of the impact of pollution on asthma exacerbations. In communities located close to ports and next to busy roadways, children may experience higher personal levels of exposure than those measured at a single community monitoring site (which are intentionally located away from major roadways).
Other uncertainties include the attribution of uniform risk to children at all residential distances within 75 meters of a major roadway, a simplification of the continuous decline to approximately 200 meters we have observed.10 We also extrapolated the effects of traffic proximity on asthma prevalence developed from young school children in the CHS to the entire population of children aged up to 17 years. These uncertainties can only be partially quantified; thus, we did not perform sophisticated quantitative models of uncertainty.
Finally, we did not estimate the additive benefits of disease prevented by reduction of NO2 and O3. Although the epidemiological evidence for the outcomes selected suggests that O3 has independent effects from NO2, there is some evidence that there may be some synergistic effects.32 The 4 exacerbation outcomes examined in this study may overlap in some children, as a child visiting an emergency room may also have been hospitalized. Therefore, summation of estimates of disease burden across outcomes may result in some duplicate counting. Also, it is likely that the same children with asthma who experience chronic exacerbations of asthma symptoms are also more likely to require medical care. There are no data available to evaluate the extent of such duplicate counting on the individual level. However, air pollution represents a burden both on the quality of life of children, and on the health care system, and, thus, parallel presentation of all effects is appropriate.
We interpreted the attributable number of each outcome as those that would be prevented if air pollution were reduced. This assumption is supported by the few studies, including the CHS, that have observed a reduction of respiratory outcomes with periods of improvements in air quality because of annual fluctuations in air quality, or moving to another location.33–36 However, one generic limitation with risk assessments of this type is that cases attributable to air pollution and to other exposures may together appear to cause more than 100% of all cases (or as interventions to prevent more than 100%), because disease attributable to air pollution in a susceptible individual might well develop because of competing risk factors if there were no air pollution. For example, it is not known what fraction of children would develop asthma because of other causes if traffic proximity were eliminated. Competition between risk (or protective) factors is relevant to the correct interpretation of attributable cases, but these relationships are not well understood.
Another important uncertainty involves the causal relationship between asthma and pollutants associated with traffic proximity. Although the causal link between air pollution and asthma exacerbation is now recognized,37 some controversy remains as to whether air pollution causes asthma. However, emerging evidence from toxicologic and epidemiological studies, including several from the CHS in these study communities, supports a causal relationship.11,38
In conclusion, community-based quantitative risk analyses can improve our understanding of health problems and help promote public health in local transportation planning. Our results demonstrate that the burden of asthma prevalence and exacerbation caused by traffic proximity can be substantial in communities with large numbers of homes in close proximity to major roadways. There is an urgent need for more detailed evaluation of the health consequences both of large-scale transportation infrastructure development and of port-related air pollution in areas that already have a high burden of disease associated with air pollution.
Acknowledgments
This work has been supported by the Southern California Children's Environmental Health Center, the National Institute of Environmental Health Sciences (grants 5P01ES09581, 5P30ES07048, 5P01ES011627, 5R01ES014447, 1R01ES016535, and 5R03ES014046), the US Environmental Protection Agency (grants R831845 and R831861), the Hastings Foundation, and the Center for Research in Environmental Epidemiology, Fundación Insitut Municipal d'Investigació Mèdica, and Catalan Institute for Research and Advanced Studies, Barcelona, Spain.
The authors acknowledge the insights of the staff and members of the Long Beach Alliance for Children With Asthma and the Center for Community Action and Environmental Justice, specifically Elina Green and Penny Newman, in helping the authors understand community environmental health concerns in Long Beach and Riverside, CA. The authors also acknowledge the California South Coast Air Quality Management District.
Human Participant Protection
No approval was required.
References
- 1.California Air Resources Board, Office of Environmental Health Hazard Assessment Staff Report: Public Hearing to Consider Amendment to the Ambient Air Quality Standards for Particulate Matter and Sulfates. Sacramento, CA: Air Resources Board; 2002. Available at: ftp://ftp.arb.ca.gov/carbis/research/aaqs/std-rs/pm-final/exesum.pdf. Accessed September 20, 2008 [Google Scholar]
- 2.Ostro BD, Tran H, Levy JI. The health benefits of reduced tropospheric ozone in California. J Air Waste Manag Assoc. 2006;56:1007–1021 [DOI] [PubMed] [Google Scholar]
- 3.Air Quality Management Plan. Diamond Bar, CA: South Coast Air Quality Management District; 2007. Available at: http://www.aqmd.gov/aqmp/07aqmp/07AQMP.html. Accessed September 18, 2008 [Google Scholar]
- 4.Vutukuru S, Dabdub D. Modeling the effects of ship emissions on coastal air quality: a case study of southern California. Atmos Environ. 2008;42:3751–3764 [Google Scholar]
- 5.Los Angeles-Inland Empire Railroad Main Line Advanced Planning Study. Los Angeles, CA: Los Angeles Economic Development Corporation; 2002. Available at: http://www.scag.ca.gov/goodsmove/pdf/LABasinMainLine2002.pdf. Accessed September 18, 2008 [Google Scholar]
- 6.Goods Movement [fact sheet]. Los Angeles, CA: Southern California Association of Governments; 2007. Available at: http://www.scag.ca.gov/factsheets/pdf/2007/goodsmove07.pdf. Accessed September 18, 2008 [Google Scholar]
- 7.Hricko A. Global trade comes home. Community impacts of good movements. Environ Health Perspect. 2008;116(2):A78–A81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hricko AM. Ships, trucks, and trains: effects of goods movement on environmental health. Environ Health Perspect. 2006;114(4):A204–A205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Künzli N, Kaiser R, Medina S, et al. Public-health impact of outdoor and traffic-related air pollution: a European assessment. Lancet. 2000;356(9232):795–801 [DOI] [PubMed] [Google Scholar]
- 10.McConnell R, Berhane K, Yao L, et al. Traffic, susceptibility, and childhood asthma. Environ Health Perspect. 2006;114(5):766–772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salam MT, Islam T, Gilliland FD. Recent evidence for adverse effects of residential proximity to traffic sources on asthma. Curr Opin Pulm Med. 2008;14(1):3–8 [DOI] [PubMed] [Google Scholar]
- 12.McConnell R, Berhane K, Gilliland F, et al. Prospective study of air pollution and bronchitic symptoms in children with asthma. Am J Respir Crit Care Med. 2003;168:790–797 [DOI] [PubMed] [Google Scholar]
- 13.Hajat S, Haines A, Goubet SA, Atkinson RW, Anderson HR. Association of air pollution with daily GP consultations for asthma and other lower respiratory conditions in London. Thorax. 1999;54:597–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ostro BD, Eskeland GS, Sanchez JM, Feyzioglu T. Air pollution and health effects: a study of medical visits among children in Santiago, Chile. Environ Health Perspect. 1999;107:69–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sunyer J, Spix C, Quenel P, et al. Urban air pollution and emergency admissions for asthma in four European cities: the APHEA Project. Thorax. 1997;52:760–765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee SL, Wong WH, Lau YL. Association between air pollution and asthma admission among children in Hong Kong. Clin Exp Allergy. 2006;36:1138–1146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Children's Health Study. Epidemiologic investigation to identify chronic effects of ambient air pollutants in Southern California [Web page]. Los Angeles, CA: University of Southern California; 2004. Available at: http://www.arb.ca.gov/research/chs/chs.htm. Accessed July 10, 2008 [Google Scholar]
- 18.Schmidt CO, Kohlmann T. When to use the odds ratio or the relative risk. Int J Public Health. 2008;53:165–167 [DOI] [PubMed] [Google Scholar]
- 19.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691 [DOI] [PubMed] [Google Scholar]
- 20.Gauderman WJ, Avol E, Gilliland F, et al. The effect of air pollution on lung development from 10 to 18 years of age. N Engl J Med. 2004;351:1057–1067 [DOI] [PubMed] [Google Scholar]
- 21.Künzli N, Perez L, Lurmann F, Hricko A, Penfold B, McConnell R. An attributable risk model for exposures assumed to cause both chronic disease and its exacerbations. Epidemiology. 2008;19(2):179–185 [DOI] [PubMed] [Google Scholar]
- 22.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980 [Google Scholar]
- 23.Brauer M, Hoek G, Smit HA, et al. Air pollution and development of asthma, allergy and infections in a birth cohort. Eur Respir J. 2007;29:879–888 [DOI] [PubMed] [Google Scholar]
- 24.Delfino RJ, Zeiger RS, Seltzer JM, Street DH. Symptoms in pediatric asthmatics and air pollution: differences in effects by symptom severity, anti-inflammatory medication use and particulate averaging time. Environ Health Perspect. 1998;106:751–761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tolbert PE, Mulholland JA, MacIntosh DL, et al. Air quality and pediatric emergency room visits for asthma in Atlanta, Georgia, USA. Am J Epidemiol. 2000;151:798–810 [DOI] [PubMed] [Google Scholar]
- 26.Sheppard L, Levy D, Norris G, Larson TV, Koenig JQ. Effects of ambient air pollution on nonelderly asthma hospital admissions in Seattle, Washington, 1987-1994. Epidemiology. 1999;10:23–30 [PubMed] [Google Scholar]
- 27.Air Quality Management Plan. Diamond Bar, CA: South Coast Air Quality Management District; 2003 [Google Scholar]
- 28.Wang LY, Zhong Y, Wheeler L. Direct and indirect costs of asthma in school-age children. Prev Chronic Dis. 2005;2(1):A11. [PMC free article] [PubMed] [Google Scholar]
- 29.WHO Air Quality Guidelines for Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide. Global Update 2005. Summary of Risk Assessment. Geneva, Switzerland: World Health Organization; 2005. WHO/SDE/PHE/OEH/06.02 [Google Scholar]
- 30.Multiple Air Toxics Exposure Study in the South Coast Air Basin. MATES III. Diamond Bar, CA: South Coast Air Quality Management District; 2008 [Google Scholar]
- 31.Health Risk Assessment of Major Railyards in California. Sacramento, CA: Air Resources Board; 2008. Available at: http://www.arb.ca.gov/railyard/hra/hra.htm. Accessed September 19, 2008 [Google Scholar]
- 32.National Research Council Estimating Mortality Risk Reduction and Economic Benefits From Controlling Ozone Air Pollution. Washington, DC: The National Academies Press; 2008 [PubMed] [Google Scholar]
- 33.Avol EL, Gauderman WJ, Tan SM, London SJ, Peters JM. Respiratory effects of relocating to areas of differing air pollution levels. Am J Respir Crit Care Med. 2001;164(11):2067–2072 [DOI] [PubMed] [Google Scholar]
- 34.McConnell R, Berhane K, Gilliland F, et al. Air pollution and bronchitic symptoms in Southern California children with asthma. Environ Health Perspect. 1999;107:757–760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bayer-Oglesby L, Grize L, Gassner M, et al. Decline of ambient air pollution levels and improved respiratory health in Swiss children. Environ Health Perspect. 2005;113:1632–1637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heinrich J, Hoelscher B, Frye C, et al. Improved air quality in reunified Germany and decreases in respiratory symptoms. Epidemiology. 2002;13:394–401 [DOI] [PubMed] [Google Scholar]
- 37.Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006;355:2226–2235 [DOI] [PubMed] [Google Scholar]
- 38.McConnell R, Berhane K, Gilliland F, et al. Asthma in exercising children exposed to ozone: a cohort study. Lancet. 2002;359(9304):386–391 [DOI] [PubMed] [Google Scholar]