Abstract
Research with the Important People instrument has demonstrated that social support for abstinence is related to alcohol treatment outcomes but less work has been done on the role of network support in drug treatment outcomes. A drug and alcohol version of the Important People instrument (IPDA) was developed and administered to 141 patients in residential treatment for cocaine dependence. Three components were found, all with acceptable internal consistency: (1) substance involvement of the network, (2) general/treatment support, and (3) support for abstinence. These components and three fundamental network characteristics (size of daily network, size of network, and importance of the most important people) were investigated as correlates of pretreatment and posttreatment alcohol and drug use. The general/treatment support component and network size were inversely related to pretreatment days using drugs while network substance involvement positively correlated with pretreatment drinking frequency. Size of the daily network predicted less drinking, less drug use, and less problem severity during the 6 months after treatment whereas general/treatment support and support for abstinence did not predict outcome. Network substance involvement decreased for patients who stayed abstinent but not for those who later relapsed. Results suggest that increasing the number of people the patient sees daily while replacing substance-involved with abstinent-supportive people may improve treatment outcomes. Treatment programs may use the IPDA to identify clients most likely to benefit from changes in their social networks.
Keywords: social support, social network, drug outcomes, relapse, cocaine
1. Introduction
Studying social network characteristics in addiction research derives from social/environmental theoretical models (e.g., Connors & Tarbox, 1985) and coping/social learning theoretical models of addiction (e.g., Monti, Kadden, Rohsenow, Cooney, & Abrams, 2002). Social network characteristics have been demonstrated to be related to the initiation and continuation of drug use (e.g., Hawkins, Catalano, & Miller, 1992) drug cessation, maintenance of abstinence, and relapse. The role of social support in the process of addiction recovery is of particular relevance in guiding treatment development.
Donovan (2005) presents a useful framework for distinguishing relapse factors into distal, intermediate, proximal, and transitional factors upon which social network characteristics can be mapped. In terms of social networks, distal factors include a family history of an alcohol or drug problem, intermediate factors include social support, proximal factors would include social pressure, and transitional factors include the reaction of the social network to a lapse. Lack of social support has been associated with drinking to cope (Holahan, Moos, Holahan, Cronkite, & Randall, 2004), dropping out of substance use treatment (Dobkin, Civita, Paraherakis, & Gill, 2002), and failure to maintain abstinence after treatment (Hser, Grella, Hsieh, Anglin, & Brown, 1999). Emotional support and functional social support are highly predictive of long-term abstinence from alcohol and/or other drugs (Beattie & Longabaugh, 1999; Havassy, Hall, & Wasserman, 1991; McMahon, 2001; Witkiewitz & Marlatt, 2004). Poor quality of social support and level of support for abstinence have also been related to relapse (Dobkin et al.; Brown, Vik, & Craemer, 1989). In addition, the success of marital and network therapy for alcohol and drug problems (Galanter, 1993; O’Farrell & Fals-Stewart, 2006), and the proliferation of mutual-support groups across the globe (Makela, 1996) suggest that a variety of social network characteristics may play a critical role in recovery from substance use. Mutual support groups have been found to increase the likelihood of initiating abstinence while beginning treatment in the NIDA Collaborative Cocaine Treatment Study (Weiss et al., 1996) and to promote long-term abstinence, with AA participation during the second and third year following treatment improving the likelihood of abstinence (Bond, Kaskutas, & Weisner, 2003).
1.1. The Important People and Activities Interview
The Important People and Activities (IPA) interview (Beattie and Longabaugh, 1999; Allen & Wilson, 2003) is one frequently used measure of alcohol-specific social network influences. A strength of the IPA is that it assesses many different aspects of social support that may be important in substance use recovery, and assesses them over a wide range of relationships. The interview identifies members of the social network who have been important in the last 6 months and then asks respondents to rate each member on frequency of contact, importance, extent of general support received, drinking status, drinking frequency, reaction towards the subject’s drinking, and support for treatment or abstinence. Because the IPA assesses a wide variety of aspects of support in recovery, it is ideal for studies comparing the effects of various aspects of alcohol-relevant social support. For example, Beattie and Longabaugh (1999) found that both general and abstinent-specific support predicted 3 month outcomes but only abstinence-specific support predicted long term outcomes. Furthermore, Zywiak, Longabaugh, and Wirtz (2002) found a larger daily network and greater percentage of abstainers and/or recovering alcoholics in the network predicted better outcomes [Project MATCH Research Group (PMRG), 1998]. In its various permutations the IPA has operationalized support for abstinence and support for drinking as two ends of the same continuous variable.
A second strength of the IPA is that it has received extensive research attention with alcohol dependent patients in a variety of multi-site randomized clinical trials. In addition to Project MATCH (PMRG, 1997; 1998) the IPA has been used in Project COMBINE (COMBINE Research Group, 2003) and the United Kingdom Alcohol Treatment Trial (The UKATT Research Team, 2001) yielding a variety of significant research findings. For example, in Project MATCH, IPA variables predicted patient outcomes during the 12-month follow-up (PMRG, 1997) and 3 years later, and also evidenced a 3-year matching effect (PMRG, 1998): patients reporting a higher network drinking frequency at baseline had better 3-year outcomes when assigned to 12-Step Facilitation rather than Motivational Enhancement Therapy. The large and growing IPA research literature (e.g., Mohr, Averna, Kenny, & Del Boca, 2001) provides a solid context for interpreting the results of new studies that use this measure.
We expanded the IPA to assess variables in regard to substance use, to complement the assessment of alcohol-related indices, since alcohol and drug use often co-occur. The purpose of this study was to adapt the IPA to substance use in general and to report its reliability and concurrent validity with data from substance dependent patients in residential treatment. We also examine which indices and composites best predicted substance use outcomes following substance abuse treatment. Further, we describe several treatment implications of these findings.
2. Methods
2. 1. Participants
Patients were recruited from a state-funded inner-city residential substance abuse treatment program with a state-wide catchment area. They were recruited for a larger assessment study focused on assessment of craving and other predictors of outcome (Rohsenow, Martin, & Monti, 2005). The abstinence-oriented 1-2 month treatment program used 12-step groups, education, relapse prevention groups, family therapy and outpatient aftercare.
2.2. Overview of Procedures
All procedures were approved by the Institutional Review Boards of Brown University, the Providence VA Medical Center, and the clinical site, and were consistent with the principles in the Declaration of Helsinki. Recruitment with informed consent was typically done on the second day of treatment and the 4-hour assessment battery was conducted during free time in the first week of treatment. Current DSM-IV cocaine dependence was the inclusion criterion and active psychosis was the exclusion criterion (none of the potential participants interviewed were actively psychotic). Drug use outcomes were assessed 3 and 6 months after discharge with confirmation of abstinence by urine drug screens. Study procedures are described in additional detail in Rohsenow et al. (2005) and Rohsenow, Martin, Eaton, and Monti (2007).
2.3. Measures
The Important People Drug and Alcohol (IPDA) interview was adapted from the Important People and Activities measure used in Project MATCH (PMRG, 1998). The activities section was not used. The IPDA asks respondents to provide the first name and relationship of up to 12 network members who have been important to them in the last 6 months (at baseline) or 3 months (at follow up). (The 3-month window paralleled the schedule of follow-ups.) For each network member identified, using fully-anchored scales for every rating, the respondent rated frequency of contact on a 7-point scale from once in the past 6 months (1) to daily (7); how important the person is to them rated on a 6-point scale from not at all important (1) to extremely important (6); extent to which the person was generally supportive of them rated on a 6-point scale from not at all supportive (1) to extremely supportive (6); drinking status rated on a 5-point scale (recovering alcoholic, abstainer, light drinker, moderate drinker, or heavy drinker); drinking frequency rated on an 8-point scale from not in past 6 months (0) to daily (7); how this person has reacted to their drinking rated on a 5-point scale from left or made you leave when you’re drinking (1) to encouraged (5); and how this person has felt about their coming for treatment rated on a 6-point scale from strongly opposes it (1) to strongly supports it (6). These seven questions are identical to the ones in the IPA. In addition we added the following three questions about each person listed: drug use status rated on a 5-point scale (recovering drug user, abstainer, light drug user, moderate drug user, or heavy drug user); drug use frequency rated on an 8-point scale from not in past 6 months (0) to daily (7); and reaction towards the subject’s drug use rated on a 5-point scale from left or made you leave when you're using drugs (1) to encouraged (your using drugs) (5). The option don’t know or doesn’t know about it is available for each question after the first three (contact frequency, importance, and general support), and (the patient) was abstinent (during the) last 3 months is an option for the network reaction questions at follow-up interviews. The IPDA was administered at the baseline assessment and again at the 3-month and 6-month follow-up interviews.
Cocaine-related and alcohol-related diagnoses were assessed at baseline using the criteria of the structured clinical interview for DSM-IV, patient version (First, Spitzer, Gibbon, & Williams, 1995) administered by a research therapist. All other measures were administered by research interviewers. Frequency of alcohol and drug use was determined using the Timeline Followback (TLFB; Sobell & Sobell, 1980; Ehrman & Robbins, 1994) administered at treatment entry for the 6 months before treatment entry and at the 3 and 6 month follow-up interviews for the 6 months following discharge. The number of days of cocaine, alcohol and other drug use were collected and converted to percentages of days in the window. (The number of heavy drinking days was collected but was collinear with number of drinking days, rs from .83 to .93, and therefore was not used.) Procedures for increasing the validity of self-reports as recommended by Sobell and Sobell (1986) included creating a set and setting of confidentiality, sharing no information with clinical staff, and ensuring a zero breath alcohol level at the time of the interview. Urine drug screens were conducted at the 3 and 6-month follow-up using ON TRAK® (Roche; Indianapolis, IN) test cups with positive tests confirmed with EMIT, gas chromatography and mass spectrometry for benzoylecgonine (cocaine metabolite), opiates, cannabis, benzodiazepines, and barbiturates. Reports of abstinence were coded as relapse if urine results were positive or invalid. The Addition Severity Index – 5th edition (ASI; McLellan, Luborsky, O’Brien, & Woody, 1980) drug and alcohol sections were administered at treatment entry and the subsections on the last 30 days were re-administered at each follow up. The ASI was scored by making a composite index for each section according to McGahan, Griffith, and McLellan (1986).
2.4. Analysis Approach
IPDA Scoring: parallel to the procedures used in Project MATCH (see Zywiak et al., 2002), 23 indices were calculated. The first three indices of fundamental network characteristics evaluate the client’s investment in his/her social network. Index 1 (network size) is the number of people in the client’s social network (with a maximum of 12 elicited), using the square root transformation to provide a more normal distribution. Index 2 (size of daily network) is the number of network members with whom the client is in daily contact. Index 3 is the average importance rating of the most important people (people rated as very or extremely important). The next four indices assess network drinking. Index 4 is the drinking status of each network member (with abstainers and recovering people combined) multiplied by frequency of contact, averaged across all members listed. Index 5 is the drinking frequency of members multiplied by frequency of contact averaged across all members listed. Index 6 is percentage of heavy drinkers in the network. Index 7 is percentage of abstainers and recovering alcoholics in the network. Another four indices assess network drug use: Index 8 is the drug use status of each network member multiplied by frequency of contract. Index 9 is the drug use frequency of members multiplied by frequency of contact averaged across all members listed. Index 10 is the percentage of heavy drug users in the network. Index 11 is the percentage of abstainers and drug users in recovery in the network. Another six indices (Indices 12 – 17) address support for drinking or drug use of the most important network members: the highest support rating for drinking, the lowest support rating for drinking, and the average support rating for drinking (multiplied by the person’s importance rating), and three parallel indices for drug use. Support was recoded into encouraged = 2, accepted = 1, and neutral to left or made you leave as 0. Indices 12 – 17 were calculated based on support ratings from only the people rated as very or extremely important. A final six indices address support in general (Indices 18-20) or for treatment (Indices 21-23) in terms of the highest support rating, the lowest support rating, and the average support rating. (Specific scoring algorithms are available from the first or fifth author.)
The statistical analyses were conducted in five phases: 1) descriptive statistics and examination of distributional characteristics, 2) component analysis of IPDA indices, 3) internal consistency reliabilities with item elimination if needed to obtain acceptable reliability, 4) concurrent validity, and 5) predictive validity. Given the large number of indices with conceptual overlap, principal components analysis (PCA) with a varimax rotation was conducted to determine the number of separate components. The number of components was determined using parallel analysis (PA; Horn, 1965) and the minimum average partial methods (MAP; Velicer, 1976) reported by Zwick and Velicer (1986) to be the most accurate methods for determining number of components to retain. Internal consistency reliabilities were calculated using Cronbach’s alpha. Concurrent validity analyses used correlations of IPDA baseline scores with pretreatment substance use variables (frequency of drug days, drinking days, ASI Drug and Alcohol composite indices, and abstinence goals for cocaine and alcohol). Predictive validity analyses used correlations of baseline IPDA scores with number of drug use days and number of drinking days during each follow-up window (months 1-3 and 4-6) separately and with ASI Drug and Alcohol composite scores at each follow-up. ANOVAs compared baseline IPDA scores by 3 or 6 month abstinence versus relapse to any drugs or alcohol. The relationship of change from pre-to posttreatment in five of the IPDA scores to relapse was analyzed using repeated measures ANOVAs in which each final IPDA variable at pretreatment and at 3-month follow-up was the repeated measure and relapse to any drugs or alcohol at 3-month follow-up was the between-groups factor. (A relapse by time repeated measures ANOVA was not run on the composite scale of support for substance use because this was inherently missing for all abstainers at follow up.) The analyses were then also conducted using pre to 6-month IPDA and 6 month relapse. (Including 3 and 6 month data in the same analyses would have resulted in excluding too many valid observations due to listwise case deletion.) The interaction of relapse group by time was inspected to determine the relationship of change in scores to relapse status, and the main effect for relapse was inspected to determine stable differences in IPDA variables that differed between relapsers and abstainers. Main effects for time were not inspected since only relationship to relapse status was of interest.
3. Results
3.1. Participant Characteristics
The 141 participants who completed the baseline assessment all met criteria for current cocaine dependence. See Table 1 for participant characteristics. Follow-up data plus baseline IPDA data were available for 77% of the 141 participants (n = 109) at the 3-month follow-up and for 74% of the sample (n = 104) at the 6-month follow-up. (IPDA data at 3 months were not available for 21 of these people because participants not interviewed at 3 months were asked at 6 months about the first 3 months’ drug and alcohol use but were not given the 3-month IPDA.) By 3-months, 44% of the sample with data had relapsed to drugs and/or alcohol and by 6 months 63% had relapsed to drugs and/or alcohol. Of patients who said they were abstinent from cocaine at follow-up, 6 (7%) were disconfirmed by urine at 3 months and 7 (9%) at 6 months; they were coded as relapsed and their number of drug used days replaced using regression estimation procedures (based on their pretreatment number of drug days, and the slope and intercept of the regression line for baseline drug days and follow-up drug days for those cases with valid data).
Table 1.
Participant characteristics and substance use
| Percent (n) | M (SD) | |
|---|---|---|
| Age | 33.7 (7.4) | |
| Education | 12.1 (2.0) | |
| Male | 53% (75) | |
| White | 70% (100) | |
| Black | 21% (30) | |
| Hispanic | 6% (9) | |
| Native American | 4% (6) | |
| Married or cohabiting | 10% (14) | |
| Employed | 11% (15) | |
| Most common cocaine administration used: | ||
| Smoked freebase | 51% (72) | |
| Smoked crack | 32% (45) | |
| Intravenous | 9% (13) | |
| Intranasal | 6% (9) | |
| Alcohol abuse or dependence diagnosis | 69% (93) | |
| Length of stay in treatment (days) | 39 (21) | |
| Network size (square root) | 2.43 (0.54) | |
| Size of daily network | 2.30 (2.33) | |
| Importance of most important people | 5.66 (0.52) | |
| Addiction Severity Index – Drug composite | 0.16 (0.14) | |
| Addiction Severity Index – Alcohol composite | 0.21 (0.28) | |
| % days used drugs pretreatment (out of 180 days) | 48.1 (27.6) | |
| % days used drugs 1-3 months follow up | 12.2 (23.4) | |
| % days used drugs 4-6 months follow up | 14.3 (26.9) | |
| % days used alcohol pretreatment | 24.1 (26.8) | |
| % days used alcohol 1-3 months follow up | 4.85 (13.3) | |
| % days used alcohol 4-6 months follow up | 6.4 (15.2) |
3.2. Preliminary analyses
The following IPDA indices were skewed and therefore were log-transformed (base 10) prior to further analysis: Index 3 (average importance rating), Index 14 (average support rating for drinking), Index 17 (average support rating for drug use), Index 18 (maximum general support), Index 21 (maximum treatment support), Index 22 (minimum treatment support). The variables of frequency of cocaine use during months 1-3 and 4-6 during the follow-up were log transformed to correct skewness.
3.3. Component Analysis
Entering all 23 indices into PCA failed to generate a solution. Therefore, PCA was conducted again entering only those indices that were correlated with another index with at least a correlation of .70. (This strategy is analogous to pruning items from a scale in order to boost the Cronbach alpha.) Again, the PCA failed to generate a solution. In the third step, when the PCA was conducted with only those 14 indices correlated at least .75 with another index a solution was obtained (Indices 4, 5, 8, 9, 12, 14, 15, and Indices 17 through 23). The PA and MAP methods revealed three interpretable components accounting for 69% of the variance with good internal consistency as indicated by good Cronbach alphas. (1) Substance involvement of support system members (α = .92) consisted of the drinking status, drug use status, drinking frequency, and drug use frequency indices (Indices 4, 5, 8, 9). (2) General/treatment support (α = .84) consisted of most, average, and least general support, and most, average, and least support for treatment (Indices 18-23). (3) Support for substance use (α = .85) consisted of most and average support for drinking, and most and average support for drug use (Indices 12, 14, 15, 17). Component scores were calculated for each subject by averaging the z-scores of the relevant indices. Intercorrelations of the three components and the three indices are displayed in Table 2. The three generic indices (network size, daily network size, average importance of the most important people) were retained because they reflect social investment and because they have been important predictors of alcohol treatment outcomes (Zywiak et al., 2002). Untransformed means and SDs for these three generic network characteristics are reported in Table 1. (Component means are not displayed because z-scores have a mean of 0 and a SD of 1.)
Table 2.
Index and Component Intercorrelations
| Index 2 | Index 3 | Comp. 1 | Comp. 2 | Comp. 3 | |
|---|---|---|---|---|---|
| Index 1. network size | .43*** | .06 | .39*** | .05 | .16* |
| Index 2. daily network size | .22** | .22** | .17* | .15* | |
| Index 3. importance | -.02 | .37*** | .01 | ||
| Component 1. substance involvement | -.22** | .41*** | |||
| Component 2. general/treatment support | -.36*** | ||||
| Component 3. support for substance use |
p < .05;
p < .01;
p < .001
3.4. Concurrent Validity Analyses
These three components and the three fundamental network indices were selected for validation and predictive analyses. The correlations between pretreatment IPDA variables and pretreatment alcohol and drug use and severity are displayed in Table 3. These showed that the general/treatment support component and network size were both inversely related to days using drugs, and that general /treatment support was inversely related to ASI drug composite score, but both were unrelated to alcohol use. Support for substance use was positively related to ASI drug severity composite scores but not to alcohol use or composite scores. The network substance involvement component was positively related to drinking and ASI alcohol composite scores, but not to drug use variables. Pretreatment network size and daily network size were positively related to the ASI alcohol composite, but inversely related to the pretreatment number of drug use days. Importance of the most important people was not significantly related to pretreatment drinking or drug use variables.
Table 3.
IPDA Pretreatment Index and Component Correlations with Number of Drug and Alcohol Use Days During 6 Months Pretreatment, and with Addiction Severity Index Drug and Alcohol Composite Scores at Treatment Entry
| Drug days | Drinking days | ASI Drug | ASI Alcohol | |
|---|---|---|---|---|
| Index 1. network size | -.17* | .00 | -.01 | .18* |
| Index 2. daily network size | -.03 | -.04 | -.01 | .17* |
| Index 3. importance | .08 | .00 | -.02 | .10 |
| Comp. 1. substance involvement | .14 | .19** | .12 | .19* |
| Comp. 2. general/treatment support | -.23** | .05 | -.28*** | .07 |
| Comp. 3. support for substance use | .14 | .02 | .27*** | -.01 |
p < .05;
p < .01;
p < .001
3.5. Predictive Validity Analyses
As can be seen in Table 4, the size of the pretreatment daily network was negatively correlated with drug use frequency, drinking frequency, and ASI drug and alcohol composite scores during the first 3 months, and to three of these four variables during the second 3 months. The size of the overall network at treatment entry was inversely related to ASI drug composite scores during both the first 3 and second 3 months after treatment. Pretreatment importance of the most important people was negatively correlated with the number of drug use days during months 4-6 after treatment. The pretreatment IPDA composite scores from the principal components analysis were not predictive of treatment outcome and no other correlations were significant.
Table 4.
IPDA Pretreatment Index and Component Correlations with Substance Use Outcomes at 3 and 6 Months: 90-day Number of Drug Use Days, 90-Day Number of Alcohol Use Days, 30-Day ASI Drug Composite Index, and 30-Day ASI Alcohol Composite Index
| 1-3 months: |
4-6 months: |
|||||||
|---|---|---|---|---|---|---|---|---|
| Drug days | Drinking days | ASI Drug | ASI Alc. | Drug days | Drinking days | ASI Drug | ASI Alc. | |
| Index 1. network size | -.13 | -. 04 | -.22* | -.05 | -.06 | -.05 | -.19* | .02 |
| Index 2. daily network size | -.23** | -.22** | -.24* | -.28** | -.10 | -.19* | -.17* | -.20* |
| Index 3. importance | -.03 | -.12 | .04 | .00 | -.18* | -.11 | -.14 | -.04 |
| Comp. 1. substance involvement | -.15 | -.02 | -.10 | .02 | -.03 | .01 | -.03 | .02 |
| Comp. 2. general/treatment support | -.14 | -.06 | -.09 | .05 | -.06 | .00 | -.16 | -.01 |
| Comp. 3. support for substance use | .03 | -.06 | -.08 | -.15 | -.01 | .01 | .05 | -.14 |
p < .05;
p < .01;
p < .001
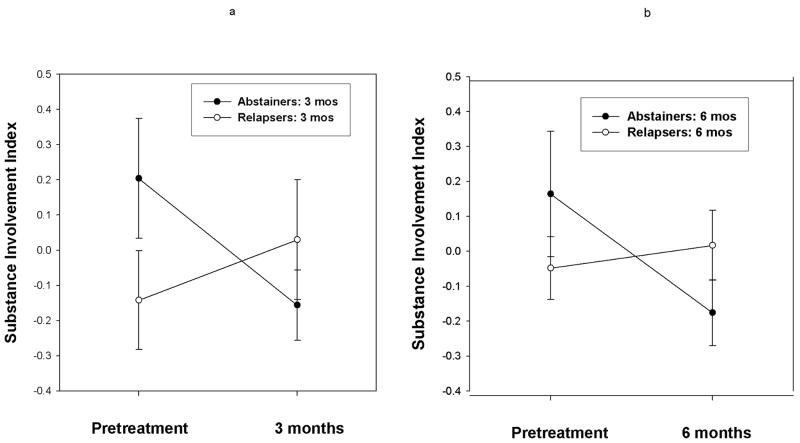
The repeated measures ANOVA revealed an interaction between network substance involvement assessed at pretreatment and 3-months by 3-month relapse status [F(1,69) = 4.14; p < .05]. Post-hoc tests indicate that substance involvement decreased in the networks of patients who stayed abstinent [F(1,69) = 4.32, p < .05] and showed no significant change in the networks of patients who relapsed [F(1,69) < 1]. (See Figure 1.) A similar interaction was observed when pretreatment and 6-month time-points were compared in the ANOVA [F(1,98) = 4.47; p < .05]. The post hoc tests again indicated that substance involvement decreased in the networks of patients who stayed abstinent [F(1,98) = 5.00, p < .03] and non-significantly increased in the networks of patients that relapsed [F(1,98) < 1] . No other relapse by time interaction effects were significant.
Figure 1.
Change in network substance involvement from 0-3 months (Fig. 1a) and from 0-6 months (Fig. 1b) by relapse to substances or abstinence during the same period.
The repeated measures ANOVAs also revealed several main effects of relapse status. People who were abstinent at 3 months had more people in their networks before and after treatment [transformed M = 2.64 ± 0.52 (SD)] than did relapsers [transformed M = 2.42 ± 0.59; F(1,71) = 4.18, p < .05]. The same was true for 6 month relapse status [transformed M = 2.58 ± 0.56 for abstainers, M = 2.34 ± 0.58 for relapsers, F(1,101) = 5.89, p < .02]. People who were abstinent at 3 months had more daily contact with people in their networks before and after treatment (M = 3.29 ± 2.62) than did relapsers [M = 2.23 ± 2.17; F(1,71) = 4.19, p < .05]. The same was true for 6 month relapse status [M = 2.96 ± 2.15 for abstainers, M = 1.92 ± 1.92 for relapsers, F(1,101) = 8.84, p < .005].
Additional analyses were conducted to explicate how substance involvement changed in the networks of abstainers even though the total number of people in these networks did not change. With abstainers and relapsers examined separately, repeated measures ANOVAs were conducted on percentage of network members who were abstainers (or recovering) from alcohol or drugs at 0 versus 3 months and at 0 versus 6 months. Abstainers had a significant increase in the percentage of abstainers in their networks from pretreatment (M = 49% ± 31% alcohol abstainers, M = 67% ± 30% drug abstainers) to 3 months [M = 65% ± 23% alcohol abstainers; M = 87% ± 19% drug abstainers; n = 43; F(1, 42) = 10.52, p < .002, for alcohol abstainers; F(1,42) = 15.26, p < .001, for drug abstainers]. Abstainers also had a significant increase in the percentage of drug or alcohol abstainers in their networks from pretreatment (M = 50% ± 31% alcohol abstainers, M = 66% ± 30% drug abstainers) to 6 months [M = 65% ± 28% alcohol abstainers; M = 89% ± 17% drug abstainers; n = 53; F(1, 52) = 10.33, p < .002, for alcohol abstainers; F(1,52) = 27.54, p < .001, for drug abstainers]. Relapsers showed no significant change in percentage of their network who were abstinent from alcohol or drugs (pretreatment M = 55% ± 31% alcohol abstainers, M = 73% ± 26% drug abstainers; 3 months M = 59% ± 32% alcohol abstainers; M = 80% ± 28% drug abstainers, n = 30; 6 months (M = 55% ± 30% alcohol abstainers; M = 73% ± 29% drug abstainers, n = 50) with all F statistics < 1.17 and all effect sizes small (Cohen’s f ≤ .20).
3.6. Attrition Analysis
Follow-up rates for the 3 and 6-month follow-ups were 77 and 74%, respectively. While comparable to other drug treatment outcome studies such as the Drug Abuse Treatment Outcome Study which had a 70% follow-up rate with a longer follow-up interval of 1 year (Hubbard, Craddock, Flynn, Anderson, & Etheridge, 1997), these rates are still lower than the rule-of-thumb level of an acceptable follow-up rate of 80% (Stout, Brown, Longabaugh, & Noel, 1996). We therefore conducted an attrition analysis to assess whether there was a systematic bias in the portion of the sample retained. There was more statistical power to examine an attrition bias at the 6-month follow-up than the 3-month follow-up. We therefore compared the 104 participants that completed the 6-month follow-up to the 37 participants that did not on the variables assessed at baseline reported in Tables 1 and 2. Ethnicity and most common route of administration were dichotomized based on the most prevalent category to optimize the statistical power. T-tests were used for continuous variables, and chi-square analyses were used for dichotomous variables. Across 22 comparisons, an attrition bias was found for two variables. White clients were less likely to complete the follow-up (69%) than clients of other ethnicities (86%) [X2(1, N = 141) = 4.42, p = .036]. Clients that commonly freebased were more likely to complete follow-ups (82%) than clients that were more likely to use another route of administration (65%) [X2(1, N = 141) = 5.36, p = .021].
4. Discussion
Concurrent and predictive validity of the indices and components of the IPDA are supported. For the components, internal consistency is also evidenced. This may be the first time that adequate internal consistency has been demonstrated for a multi-factorial scoring algorithm of an IP interview. The IPDA, with internal consistency and validity, can be a useful tool for future research in the substance abuse treatment outcome research field. All of the final scores developed appear to have value in terms of concurrent or predictive validity except the importance rating of the most important people in their network which showed no concurrent correlations and a correlation with only one of the eight outcome variables. This index may have been hampered by a restriction of range. In other studies using the Important People instrument, participants have instead been asked to rate the importance of their four most important people.
The size of the daily network was the most robust predictor of drug use frequency, drinking frequency, and relapse status at 3 and 6 months, with a larger daily social network predicting better treatment outcome. This finding replicates the positive relationship found between the size of the daily network and drinking outcomes (percent days abstinent and monthly volume) in Project MATCH (Zywiak et al., 2002). This finding is also consistent with results indicating that network size was a significant mediator of the relationship between AA attendance and lower alcohol consumption (Kaskutas, Bond, & Humphreys, 2002). The size of the daily network is considered to be a measure of social investment, and there are a number of ways social investment could influence outcome according to social learning theory (Monti et al., 2002) particularly by providing alternative sources of reinforcement and assistance with coping with stressors that might otherwise lead to relapse.
Network substance involvement decreased from baseline to 3- and 6-months for those patients who remained abstinent and increased nonsignificantly among those who relapsed, despite no significant change in number of people in the network. Analyses to help investigate explanations of these apparently contradictory findings showed that patients who relapsed had no apparent change in percentage of network members involved with drugs or alcohol versus abstinent between these time points (55% of network members were alcohol abstainers at both pretreatment and 6 months, 73% were drug abstainers at both pretreatment and 6 months). However, patients who were successful abstainers apparently replaced some people in their networks in such a way that the percentage of network members who were abstinent from alcohol or drugs increased significantly from 50% alcohol abstainers pretreatment to 65% at 6 months, and from 66% drug abstainers at pretreatment to 89% at 6 months. These results are consistent with results found for clients in alcohol treatment in Project MATCH (PMRG, 1998). Such changes are also consistent with recommendations commonly made in skills training programs for substance abusers (e.g., Rohsenow, Monti, Martin, Michalec, & Abrams, 2000; Rohsenow et al., 2004) and provide evidence that such changes are associated with successful outcomes. The results of Rohsenow et al. (2005) suggest some specific ways that having abstinent people in one’s support network may help with abstinence; this study found that cocaine abstinence was correlated with lifestyle changes focused on clean ways to have fun, living with clean and sober people, and relying on people other than counselors and sponsors for social support.
It was unexpected that the general/treatment support component and support for substance use component were not related to substance use outcomes, in contrast to findings with alcohol dependent patients (Beattie & Longabaugh, 1999). It appears that network substance use is a more powerful predictor of substance use outcomes than is perceived general/treatment support or perceived support for substance use as opposed to abstinence. It may be that participants are able to more accurately report on drinking/drug use and status for their network members than they are able to report on general/treatment support and support for substance use. Alternatively, mere use of drugs by a network member, regardless of their encouraging drug use or treatment, may be a strong risk factor due to increased availability and effects of conditioned responses (Rohsenow, Niaura, Childress, Abrams, & Monti, 1990). In the present study, the general/treatment support variable was related to lower drug use frequency prior to treatment entry, suggesting that possibly such support was instrumental in encouraging treatment entry at an earlier stage of substance severity.
Limitations of this study included using only patients drawn from one inner-city residential treatment program, all of whom had cocaine dependence as at least one substance diagnosis. Future research should be conducted with other broader groups of substance dependent patients from a variety of treatment programs. Another limitation is that the follow-up rate was below 80%. Our attrition analysis results indicating that White participants were more likely to be lost to follow-up than participants of other ethnicities parallels the findings of Lapham, Baum, Skipper, and Chang (2000) with a DWI sample. Attrition results indicate that our findings may not generalize to White clients, nor clients using various routes of cocaine administration. A number of strategies to optimize follow-up rates are described by Zweben, Barrett, Berger, and Murray (2005).
There are a number of treatment implications of this study. The easiest changes to implement into a treatment program would be the recommendations that clients increase the number of people they see daily and replace substance-involved with abstinent support people in their networks. More ambitious treatment programs may want to administer the IPDA to see which clients may be in particular need of changing their social networks. Conceivably this could be done in a group format. Finally, it may be useful to administer the IPDA pre and post-treatment to assess the degree to which these social network changes have been achieved, and to assess the extent to which these changes still need to be made. Since social network characteristics have been found to be related to treatment outcome three years later (Zywiak et al., 2002), these social network changes are one way of achieving sustained treatment gains. Future research could examine moderators of network changes both in and outside of mutual help programs.
Acknowledgments
Special thanks to two anonymous reviewers and to Suzanne Sales for conducting the attrition analysis for the revised manuscript. This research was supported in part by a grant from the National Institute on Drug Abuse 1 RO1 DA11071 to the last author and by T32 AA07459 from the National Institute on Alcoholism and Alcohol Abuse. Participation of Dr. Rohsenow was supported by a Veterans Affairs Merit Review grant from the Office of Research and Development, Medical Research Service, Department of Veterans Affairs, and by a Career Scientist award from the Department of Veterans Affairs.
Footnotes
A preliminary version of these results was presented at the annual meeting of the College on Problems in Drug Dependence, San Juan, Puerto Rico, USA, June 2004.
References
- Allen JP, Wilson VB. Assessing Alcohol Problems: A Guide for Clinicians and Researchers. 2. DHHS; Bethesda, MD: 2003. [Google Scholar]
- Beattie MC, Longabaugh R. General and alcohol-specific support following treatment. Addictive Behaviors. 1999;24:593–606. doi: 10.1016/s0306-4603(98)00120-8. [DOI] [PubMed] [Google Scholar]
- Bond J, Kaskutas LA, Weisner C. The persistent influence of social networks and alcoholics anonymous on abstinence. Journal of Studies on Alcohol. 2003;64:579–588. doi: 10.15288/jsa.2003.64.579. [DOI] [PubMed] [Google Scholar]
- Borsari BE, Carey KB. Understanding fraternity drinking: Five recurring themes in the literature, 1980 – 1998. Journal of American College Health. 1999;48:30–37. doi: 10.1080/07448489909595669. [DOI] [PubMed] [Google Scholar]
- Brown SA, Vik PW, Craemer VA. Characteristics of relapse following adolescents substance abuse treatment. Addictive Behaviors. 1989;14:291–300. doi: 10.1016/0306-4603(89)90060-9. [DOI] [PubMed] [Google Scholar]
- COMBINE Research Group. Testing combined pharmacotherapies and behavioral interventions in alcohol dependence: Rationale and methods. Alcoholism: Clinical and Experimental Research. 2003;27:1107–1122. doi: 10.1097/00000374-200307000-00011. [DOI] [PubMed] [Google Scholar]
- Connors GJ, Tarbox AR. Macroenvironmental factors as determinants of substance use and abuse. In: Galizio M, Maisto SA, editors. Determinants of Substance Abuse: Biological, Psychological, and Environmental Factors. New York: Plenum Press; 1985. pp. 283–314. [Google Scholar]
- Dobkin PL, Civita MD, Paraherakis A, Gill K. The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction. 2002;97:347–356. doi: 10.1046/j.1360-0443.2002.00083.x. [DOI] [PubMed] [Google Scholar]
- Donovan DM. Assessment of addictive behaviors for relapse prevention. In: Donovan DM, Marlatt GA, editors. Assessment of Addictive Behaviors. 2. New York: Guilford; 2005. pp. 1–48. [Google Scholar]
- Ehrman RN, Robbins SJ. Reliability and validity of six-month timeline reports of cocaine and heroin use in a methadone population. Journal of Consulting and Clinical Psychology. 1994;62:843–850. doi: 10.1037//0022-006x.62.4.843. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis-I Disorders – Patient Edition. Biometrics Research Department, Psychiatric Institute; New York: 1995. [Google Scholar]
- Galanter M. Network Therapy for Alcohol and Drug Abuse. New York: Guilford; 1993. [Google Scholar]
- Havassy BE, Hall SM, Wasserman DA. Social support and relapse: Commonalities among alcoholics, opiate users, and cigarette smokers. Addictive Behaviors. 1991;16:235–246. doi: 10.1016/0306-4603(91)90016-b. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Unipolar depression, life context vulnerabilities, and drinking to cope. Journal of Consulting and Clinical Psychology. 2004;72:269–275. doi: 10.1037/0022-006X.72.2.269. [DOI] [PubMed] [Google Scholar]
- Horn IL. A rationale and test for the number of factors in factor analysis. Psychometrika. 1965;30:179–185. doi: 10.1007/BF02289447. [DOI] [PubMed] [Google Scholar]
- Hser YI, Grella CE, Hsieh SC, Anglin MD, Brown BS. Prior treatment experience related to process and outcomes in DATOS. Drug and Alcohol Dependence. 1999;57:137–150. doi: 10.1016/s0376-8716(99)00081-2. [DOI] [PubMed] [Google Scholar]
- Hubbard RL, Craddock G, Flynn PM, Anderson J, Etheridge RM. Overview of 1-year follow-up outcomes in the drug abuse treatment outcome study (DATOS) Psychology of Addictive Disorders. 1997;11:261–278. [Google Scholar]
- Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97:891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- Lapham S, Baum G, Skipper B, Chang I. Attrition in a follow-up study of driving while impaired offenders: Who is lost? Alcohol and Alcoholism. 2000;35:464–470. doi: 10.1093/alcalc/35.5.464. [DOI] [PubMed] [Google Scholar]
- Makela K. Alcoholics Anonymous as a Mutual-Help Movement: A Study in Eight Societies. Madison, Wisconsin: University of Wisconsin Press; 1996. [Google Scholar]
- McGahan PL, Griffith JA, McLellan AT. Composite Scores from the Addiction Severity Index: manual and computer software. Veterans Administration Press; Philadelphia VA Medical Center, University Avenue, Philadelphia, PA 19104: 1986. [Google Scholar]
- McLellan AT, Luborsky L, O’Brien CP, Woody GE. An improved diagnostic instrument for substance abuse patients: The Addiction Severity Index. Journal of Nervous and Mental Disease. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- McMahon RC. Personality, stress, and social support in cocaine relapse prediction. Journal of Substance Abuse Treatment. 2001;9:225–235. doi: 10.1016/s0740-5472(01)00187-8. [DOI] [PubMed] [Google Scholar]
- Mohr CD, Averna S, Kenny DA, Del Boca FK. “Getting by (or getting high) with a little help from my friends”: An examination of adult alcoholics’ friendships. Journal of Studies on Alcohol. 2001;62:637–645. doi: 10.15288/jsa.2001.62.637. [DOI] [PubMed] [Google Scholar]
- Monti PM, Kadden RM, Rohsenow DJ, Cooney NL, Abrams DB. Treating Alcohol Dependence: A Coping Skills Training Guide. 2. New York: Guilford; 2002. [Google Scholar]
- O’Farrell TJ, Fals-Stewart W. Behavioral Couples Therapy for Alcoholism and Drug Abuse. New York: Guilford; 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to patient heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to patient heterogeneity: Project MATCH three-year drinking outcomes. Alcoholism: Clinical and Experimental Research. 1998;22:1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Martin RA, Eaton CA, Monti PM. Cocaine craving as a predictor of treatment attrition and outcomes after residential treatment for cocaine dependence. Journal of Studies on Alcohol and Drugs. 2007;68:641–648. doi: 10.15288/jsad.2007.68.641. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Martin RA, Monti PM. Urge-specific and lifestyle coping strategies of cocaine abusers: Relationships to treatment outcomes. Drug and Alcohol Dependence. 2005;78:211–219. doi: 10.1016/j.drugalcdep.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Martin RA, Colby SM, Myers MG, Gulliver SB, Brown RA, Mueller TI, Gordon A, Abrams DB. Motivational enhancement and coping skills training for cocaine abusers: Effects on substance use outcomes. Addiction. 2004;99:862–874. doi: 10.1111/j.1360-0443.2004.00743.x. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Martin RA, Michalec E, Abrams DB. Brief coping skills treatment for cocaine abuse: 12-month substance use outcomes. Journal of Consulting and Clinical Psychology. 2000;68:515–520. doi: 10.1037//0022-006x.68.3.515. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Niaura RS, Childress AR, Abrams DB, Monti PM. Cue reactivity in addictive behaviors: Theoretical and treatment implications. International Journal of the Addictions. 1990;25:957–993. doi: 10.3109/10826089109071030. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Convergent validity: An approach to increasing confidence in treatment outcome conclusions with alcohol and drug abusers. In: Sobell LC, Sobell MB, Ward E, editors. Evaluating alcohol and drug abuse treatment effectiveness: Recent advances. New York: Pergamon; 1980. pp. 177–183. [Google Scholar]
- Sobell LC, Sobell MB. Can we do without alcohol abusers’ self-reports? Behavioral Therapist. 1986;7:141–146. [Google Scholar]
- Stout RL, Brown PJ, Longabaugh R, Noel N. Determinants of research follow-up participation in an alcohol treatment outcome trial. Journal of Consulting and Clinical Psychology. 1996;64:614–618. doi: 10.1037//0022-006x.64.3.614. [DOI] [PubMed] [Google Scholar]
- The UKATT Research Team. United Kingdom Alcohol Treatment Trial (UKATT): Hypotheses, Design, and Methods. Alcohol and Alcoholism. 2001;36:11–21. doi: 10.1093/alcalc/36.1.11. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Najavits LM, Hufford C, Kogan J, Thompson HJ, Albeck JH, Bishop S, Daley DC, Mercer D, Siqueland L. Self-help activities in cocaine dependent patients entering treatment: Results from the NIDA collaborative cocaine treatment study. Drug and Alcohol Dependence. 1996;43:79–86. doi: 10.1016/s0376-8716(96)01292-6. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. American Psychologist. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Velicer WF. Determining the number of components from the matrix of partial correlations. Psychometrika. 1976;41:321–327. [Google Scholar]
- Zweben A, Barrett D, Berger L, Murray KT. Recruiting and retaining participants in a combined behavioral and pharmacological clinical trial. Journal of Studies on Alcohol. 2005;(Supplement No 15):72–81. doi: 10.15288/jsas.2005.s15.72. [DOI] [PubMed] [Google Scholar]
- Zwick WR, Velicer WF. Comparison of five rules for determining the number of components to retain. Psychological Bulletin. 1986;99:432–442. [Google Scholar]
- Zywiak WH, Longabaugh R, Wirtz P. Decomposing the effects of social networks upon alcohol treatment outcome. Journal of Studies on Alcohol. 2002;63:114–121. [PubMed] [Google Scholar]