Abstract
Background
Little is known about the distribution of diagnoses that account for fatigue in patients in primary care. We evaluated the diagnoses established within 1 year after presentation with fatigue in primary care that were possibly associated with the fatigue.
Methods
We conducted a prospective observational cohort study with 1-year follow-up. We included adult patients who presented with a new episode of fatigue between June 2004 and January 2006. We extracted data on diagnoses during the follow-up period from the patients’ medical records as well as data on pre-existing chronic diseases.
Results
Of the 571 patients for whom diagnostic data were available, 268 (46.9%) had received one or more diagnoses that could be associated with fatigue. The diagnoses were diverse and mostly included symptom diagnoses, with main categories being musculoskeletal (19.4%) and psychological problems (16.5%). Clear somatic pathology was diagnosed in 47 (8.2%) of the patients. Most diagnoses were not made during the consultation when fatigue was presented.
Interpretation
Only a minority of patients were diagnosed with serious pathology. Half of the patients did not receive any diagnosis that could explain their fatigue. Nevertheless, because of the wide range of conditions and symptoms that may explain or co-occur with the fatigue, fatigue is a complex problem that deserves attention not only as a symptom of underlying specific disease.
Fatigue is a common problem seen in primary care. It is reported as the main presenting symptom in 5% to 10% of patients.1–3 Both its nonspecific nature and its high prevalence make fatigue a challenging problem for general practitioners to manage. The symptom may indicate a wide range of conditions, including respiratory, cardiovascular, endocrine, gastrointestinal, hematologic, infectious, neurologic and musculoskeletal diseases, mood disorders, sleep disorders and cancer.4–13 Patients with a chronic disease often report symptoms of fatigue,14,15 and the prevalence of chronic disease is higher among patients presenting with fatigue than among other patients.16 Regardless of the underlying pathology, fatigue is a phenomenon with social, physiologic and psychological dimensions.17–20
Little is known about the distribution of diagnoses in populations of patients presenting with fatigue as a main symptom in primary care. A Dutch morbidity registration of episodes of care showed that fatigue was a symptom diagnosis in about 40% of patients.21 Previous studies involving patients presenting with fatigue as a main symptom either had small samples22,23 or reported diagnoses that were based on standardized laboratory testing at baseline.24,25 Because of the wide range of possible diagnoses, large observational studies are needed to determine the distribution of diagnoses in primary care.
We carried out a prospective study involving patients in primary care practices in whom fatigue was the main presenting symptom. The aim of our study was to describe the distribution of diagnoses established within 1 year after presentation that were possibly associated with the fatigue.
Methods
Study population
We conducted an observational cohort study in 147 general practices across the Netherlands involving adult patients who presented with a new episode of fatigue between June 2004 and January 2006. We defined a presenting symptom of fatigue as a report of tiredness or synonyms indicating fatigue such as exhaustion; we excluded more general reports of “malaise.” We also excluded patients who were receiving or had received chemotherapy or radiation therapy within 3 months before presentation, as well as women who were pregnant or had had a baby within 3 months before presentation.
Eligible patients were informed about the study by their general practitioner and invited to participate. If interested, they were sent an information letter and baseline questionnaire. Patients were enrolled in the study when they returned a signed consent form and the baseline questionnaire. Participating patients completed several questionnaires during the follow-up year (at 1, 4, 8 and 12 months after baseline).
The study design was approved by the Medical Ethics Committee of the VU University Medical Center, the Netherlands.
Data collection and analysis
We extracted data from the participants’ patient files concerning diagnoses made during the follow-up period and selected diagnoses that could provide an explanation for the presented fatigue. We also extracted data on pre-existing chronic diseases at the time of presentation. We limited these chronic diseases to conditions that could be related to fatigue and that could be assumed to be current at the moment of presentation of fatigue, regardless of treatment. We used descriptive statistics to describe frequencies of diagnoses, comorbidities and patient characteristics.
Results
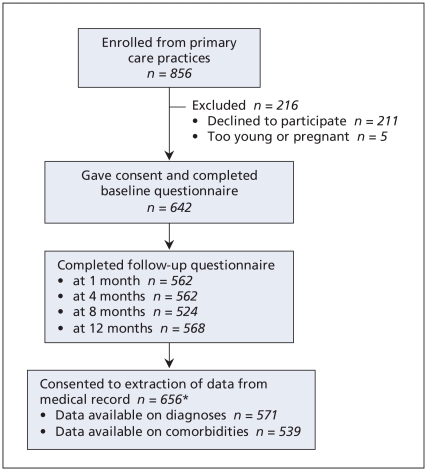
General practitioners enrolled 856 patients, of whom 642 consented to participate and returned the baseline questionnaire (Figure 1). All but 1 of these patients also consented to have data extracted from their general practitioner’s medical records. In addition, 15 patients who did not complete the baseline questionnaire consented to have data extracted from their medical records. We were able to obtain data on diagnoses for 571 (87.0%) of these 656 patients. Characteristics of the 571 participants are shown in Table 1.
Figure 1.
Selection of participants and collection of data. *Includes 15 patients who did not complete any of the questionnaires but who consented to extraction of data.
Table 1.
Characteristics of 571 patients in primary care practices who presented with fatigue as a main symptom
| Characteristic | No. (%) of patients* |
|---|---|
| Age, yr, mean (SD) | 43 (16) |
| Female sex (n = 571) | 422 (73.9) |
| Duration of fatigue (n = 546) | |
| < 1 mo | 44 (8.1) |
| 1–3 mo | 87 (15.9) |
| 3–6 mo | 98 (17.9) |
| 6–12 mo | 103 (18.9) |
| > 1 yr | 214 (39.2) |
| Localization of fatigue (n = 556) | |
| Primarily head (mental fatigue) | 91 (16.4) |
| Primarily extremities | 46 (8.3) |
| Whole body, or head and extremities | 362 (65.1) |
| Not clear | 57 (10.3) |
| Psychological symptom† (n = 556) | |
| Distress | 338 (60.8) |
| Depression | 131 (23.6) |
| Anxiety | 52 (9.4) |
| Sleep problem‡ (n = 556) | 365 (65.6) |
| Other physical symptoms,§ mean no. (SD) | 4.3 (2.7) |
| Fatigue attributed to stress or worry (n = 551) | 307 (55.7) |
| Prolonged difficulties** (n = 556) | 458 (82.4) |
| Score combining number and severity of difficulties (range 0–25), mean (SD) | 4.3 (4.3) |
| Severe difficulties in at least 1 area (n = 556) | 105 (18.9) |
| Expectation that general practitioner is able to find the cause of the fatigue (n = 548) | 287 (52.4) |
| Satisfied with general practitioner’s management of the fatigue during consultation (n = 552) | 504 (91.3) |
Note: SD = standard deviation.
Unless stated otherwise.
As indicated by elevated score on the Four-dimensional Symptom Questionnaire (4DSQ).26
As indicated by elevated score on the Symptom Checklist-90 (SCL-90).27
From 13 physical symptoms listed on the Illness Perception Questionnaire–Revised.28
Long-term difficulties, including work-related, family, neighbourhood, housing and financial problems, experienced in the year before presentation.28
Diagnoses made in the year following consultation represented all categories of the International Classification of Primary Care (ICPC).29,30 In total, 268 (46.9%) of the 571 patients received one or more diagnoses (378 in total) that could be associated with fatigue (Table 2).
Table 2.
Diagnoses during 1-year follow-up period among 571 patients in primary care practices who presented with fatigue as a main symptom
| Diagnosis (code*) | No. (%)of patients | Diagnosis recorded during initial visit |
|---|---|---|
| Musculoskeletal (L) | 111 (19.4) | |
| Rheumatoid arthritis or polymyalgia rheumatica | 2 | 0 |
| Back problem | 35 | 2 |
| Neck problem | 20 | 1 |
| Joint problem in extremities | 42 | 0 |
| Myalgia | 21 | 2 |
| Noncardiac chest symptoms | 8 | 0 |
| Osteoarthritis | 7 | 0 |
| Psychological or social (P or Z) | 94 (16.5) | |
| Depressive symptoms or depression | 28 | 4 |
| Strain, neurasthenia, burnout | 31 | 15 |
| Anxiety, tension, hyperventilation (R), distress or worry | 25 | 4 |
| Sleeplessness or sleeping problem | 11 | 1 |
| Family or relationship problem | 9 | 1 |
| Psychological problem | 5 | 2 |
| Loss or mourning | 4 | 1 |
| Affective psychosis | 1 | 0 |
| Digestive (D) | 46 (8.1) | |
| Abdominal pain or symptoms | 23 | 0 |
| Diarrhea | 8 | 1 |
| Constipation | 5 | 0 |
| Abnormal liver function | 1 | 0 |
| Irritable bowel syndrome | 12 | 2 |
| Neurologic (N) | 38 (6.7) | |
| Headache | 13 | 2 |
| Dizziness | 11 | 1 |
| Chronic tension-type headache | 8 | 2 |
| Migraine | 3 | 0 |
| Polyneuropathy | 2 | 0 |
| Concussion | 2 | 1 |
| General (A) | 28 (4.9) | |
| Anemia | 9 | 3 |
| Adverse drug effect | 6 | 1 |
| Chronic fatigue syndrome | 4 | 0 |
| Chronic pain syndrome or widespread pain | 3 | 1 |
| Hay fever, rhinitis, allergy | 6 | 2 |
| Infection (various) | 104† | 2 |
| Respiratory (R) | 28 (4.9) | |
| Asthma, chronic obstructive pulmonary disease, decreased pulmonary function or chronic bronchitis, including exacerbations | 12 | 1 |
| Chronic sinusitus | 3 | 0 |
| Cough | 9 | 1 |
| Upper airway or throat symptoms | 3 | 0 |
| Dyspnea | 2 | 0 |
| Endocrine (T) | 16 (2.8) | |
| Hypothyroidism | 7 | 1 |
| Diabetes mellitus | 4 | 0 |
| Hyperthyroidism | 3 | 0 |
| Celiac disease | 1 | 0 |
| Vitamin B12 deficiency | 1 | 0 |
| Obesity | 1 | 0 |
| Cardiovascular (K) | 11 (1.9) | |
| Heart failure | 3 | 0 |
| Angina pectoris | 3 | 0 |
| Arrhythmia | 3 | 0 |
| Cardiac symptoms | 2 | 1 |
| Intermittent claudication | 1 | 0 |
| Female genital organs (X) | 6 (1.1) | |
| Climacteric symptoms | 6 | 0 |
| Malignant disease | 4 (0.7) | |
| Bladder (U) | 1 | 0 |
| Leukemia (B) | 1 | 0 |
| Melanoma (S) | 1 | 0 |
| Colon (D) | 1 | 0 |
| Skin (S) | 3 (0.5) | |
| Itch | 3 | 0 |
The most frequently recorded somatic diagnoses were musculoskeletal problems (n = 111 [19.4%]) and diseases or symptoms of the digestive system (n = 46 [8.1%]), nervous system (n = 38, [6.7%]) and respiratory tract (n = 28 [4.9%]). The majority of diagnoses reflected symptoms or signs only. A total of 47 patients (8.2%) received one or more diagnoses of clear somatic pathology (anemia, pulmonary pathology, thyroid dysfunction, diabetes mellitus, celiac disease, vitamin B12 deficiency, heart failure, angina pectoris, malignant disease, rheumatoid arthritis, adverse drug effect). Infections were diagnosed in 104 (18.2%) of the patients. When we considered the time frame from the onset of fatigue to the diagnosis of infection, infection was a likely explanation for the fatigue in 2 cases.
A total of 94 patients (16.5%) received a diagnosis indicating psychological problems or social difficulties. Stress or neurasthenia was the diagnosis most frequently recorded during the initial consultation (Table 2).
The frequency of psychological symptoms reported in the patient questionnaires differed from the frequency in the medical records. Overall, 155 (24.1%) of the 642 patients who completed a baseline questionnaire reported having depressive symptoms; this diagnosis was recorded in 28 (4.9%) of the 571 medical records that had diagnostic data. Distress or worry was reported by 392 (61.1%) of the patients but was recorded in 25 (4.4%) of the medical records. Sleep problems were reported by 417 (65.0%) of the patients but recorded in 11 (1.9%) of the patients’ charts (see also reference 29).
Data on comorbidities were available for 539 of the patients. A total of 58 patients had a concurrent disease that could explain the fatigue. The most frequently recorded comorbid diseases were respiratory diseases (n = 37) and diabetes (n = 17). Fourteen patients were known to have a malignant disease in their medical history. For 20 patients, a functional syndrome, most often irritable bowel syndrome, had been recorded in their chart.
Interpretation
The participants in our study received a wide range of diagnoses in the year following consultation that could have been associated with the fatigue. Psychological and physical problems were diagnosed more frequently than somatic diseases. The variety of diagnoses reflects evidence from the literature and practical experience regarding the differential diagnosis of fatigue.
The small proportion of patients who received a diagnosis of somatic pathology corresponds with findings of previously published smaller studies in primary care.24,25,32 Those studies, however, used stricter inclusion criteria, excluded patients with existing chronic disease or reported on diagnoses based only on laboratory test results. Two studies, one of which included only 52 patients, reported higher prevalence rates of somatic disease (45% and 51%) than in our study.22,33 Of chronic diseases that were likely to be present at the time of consultation, respiratory conditions were more frequent in our cohort than in the general patient population in primary care in the Netherlands.15 Our study population had fewer older patients compared with those in a Dutch national morbidity registry,34 which may explain the difference in prevalence of chronic respiratory conditions.
Of the patients in our study who received a symptom diagnosis during the follow-up year, one-fifth received a diagnosis of a musculoskeletal problem, mostly nonspecific. Virtually none of the symptom diagnoses were established during the consultation, which raises questions about the temporal association between fatigue and other symptoms. Because most symptoms may show a recurrent pattern over time, further research is needed to help clarify the association between fatigue and other nonspecific symptoms.
Although psychological or social problems were the second largest diagnostic category, the number may be an underestimation. Depressive symptoms and elevated distress scores were reported more frequently in the patient questionnaires than in the medical records. Furthermore, other studies have reported psychological symptoms in the majority of patients with fatigue.35–37 Because of the variation in how the general practitioners recorded or coded the diagnoses, psychological problems may have been identified but not explicitly recorded as diagnoses in the patients’ charts.
Sleep problems were recorded in only 1.9% of the patients’ charts. This number is in stark contrast to the number of sleep problems reported by the majority of patients in the questionnaires. As with psychological symptoms, problems with sleep might either not be recognized or not recorded.38–40 Because general practitioners may perceive a sleep problem as a lifestyle issue or evidently related to fatigue, they may not record it as a diagnosis.
At least half of the patients did not receive a diagnosis that could possibly explain their fatigue. This suggests that fatigue remains “medically unexplained” in many cases, which is consistent with previous findings.21 However, the lack of a medical explanation does not always mean that there is no explanation. Given the data in the questionnaires, other psychosocial factors, although not registered in the patients’ medical records, may have played a role in the fatigue of many patients.
Almost 50% of the patients did receive a diagnosis in the year following consultation that could explain their fatigue. However, for most of the diagnoses, we were unable to assess the potential association with fatigue more closely, even when considering the time frame from onset of the fatigue to the diagnosis. This would require more information both on the severity of the symptom or disorder diagnosed and on the severity of the fatigue at the time of diagnosis.
Limitations
One limitation of our study was that we did not use a standardized protocol for physical examination or diagnostic testing. The diagnoses represent those made and recorded in daily practice by individual general practitioners. Because general practitioners differ in their decision-making regarding diagnostic procedures and referrals, this will have resulted in variation in recorded diagnoses.
Data on existing comorbidities are important to provide when presenting an overview of diagnoses. We were able to show that respiratory conditions and diabetes were more often pre-existing than newly diagnosed conditions. Our data were not comprehensive, however, and we may have missed other conditions that could have been associated with the fatigue. Furthermore, patients presenting with fatigue may have several concurrent conditions.
Conclusion
The patients who presented with fatigue in primary care had a wide range of diagnoses. However, the prevalence of severe pathology was low. The number of psychosocial problems was relatively high and may explain in part the fatigue in this primary care population. In addition, the number of psychosocial symptoms, including sleep problems, differed between the patients’ medical records and the self-reported data from the questionnaires. Practitioners need to address these problems in patients presenting with fatigue.
Footnotes
This article has been peer reviewed.
Funding: No funding was received for this study.
Previously published at www.cmaj.ca
Competing interests: None declared.
Contributors: Iris Nijrolder contributed substantially to the acquisition, analysis and interpretation of the data and drafted the article. All of the other authors contributed to the revising of the manuscript. Henriëtte van der Horst contributed significantly to the concept and design of the study and the analysis and interpretation of the data. Daniëlle van der Windt and Henk de Vries contributed substantially to the analysis and interpretation of the data. All of the authors gave final approval of the version to be published.
REFERENCES
- 1.Cullen W, Kearney Y, Bury G. Prevalence of fatigue in general practice. Ir J Med Sci. 2002;171:10–2. doi: 10.1007/BF03168931. [DOI] [PubMed] [Google Scholar]
- 2.Nelson E, Kirk J, McHugo G, et al. Chief complaint fatigue: a longitudinal study from the patient’s perspective. Fam Pract Res J. 1987;6:175–88. [PubMed] [Google Scholar]
- 3.Sharpe M, Wilks D. ABC of psychological medicine: fatigue. BMJ. 2002;325:480–3. doi: 10.1136/bmj.325.7362.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaudhuri A, Behan PO. Fatigue in neurological disorders. Lancet. 2004;363:978–88. doi: 10.1016/S0140-6736(04)15794-2. [DOI] [PubMed] [Google Scholar]
- 5.Chen MK. The epidemiology of self-perceived fatigue among adults. Prev Med. 1986;15:74–81. doi: 10.1016/0091-7435(86)90037-x. [DOI] [PubMed] [Google Scholar]
- 6.Cornuz J, Guessous I, Favrat B. Fatigue: a practical approach to diagnosis in primary care. CMAJ. 2006;174:765–7. doi: 10.1503/cmaj.1031153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dick ML, Sundin J. Psychological and psychiatric causes of fatigue. Assessment and management. Aust Fam Physician. 2003;32:877–81. [PubMed] [Google Scholar]
- 8.Falk K, Swedberg K, Gaston-Johansson F, et al. Fatigue is a prevalent and severe symptom associated with uncertainty and sense of coherence in patients with chronic heart failure. Eur J Cardiovasc Nurs. 2007;6:99–104. doi: 10.1016/j.ejcnurse.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Greenfield JR, Samaras K. Evaluation of pituitary function in the fatigued patient: a review of 59 cases. Eur J Endocrinol. 2006;154:147–57. doi: 10.1530/eje.1.02010. [DOI] [PubMed] [Google Scholar]
- 10.Hamilton W, Peters TJ, Round A, et al. What are the clinical features of lung cancer before the diagnosis is made? A population based case-control study. Thorax. 2005;60:1059–65. doi: 10.1136/thx.2005.045880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kapella MC, Larson JL, Patel MK, et al. Subjective fatigue, influencing variables, and consequences in chronic obstructive pulmonary disease. Nurs Res. 2006;55:10–7. doi: 10.1097/00006199-200601000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Sanders DS, Patel D, Stephenson TJ, et al. A primary care cross-sectional study of undiagnosed adult coeliac disease. Eur J Gastroenterol Hepatol. 2003;15:407–13. doi: 10.1097/00042737-200304000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Schuitemaker GE, Dinant GJ, van der Pol GA, et al. Assessment of vital exhaustion and identification of subjects at increased risk of myocardial infarction in general practice. Psychosomatics. 2004;45:414–8. doi: 10.1176/appi.psy.45.5.414. [DOI] [PubMed] [Google Scholar]
- 14.Lewis G, Wessely S. The epidemiology of fatigue: more questions than answers. J Epidemiol Community Health. 1992;46:92–7. doi: 10.1136/jech.46.2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van der Linden M, Westert G, De Bakker D, et al. Second national study into diseases and actions in general practice [reports] Utrecht (Bilthoven): NIVEL (Dutch Institute for Health Services Research) and RIVM (National Institute of Public Health and Environment); 2005. Tweede Nationale Studie: naar ziekten en verrichtingen in de huisartspraktijk. [Google Scholar]
- 16.Kenter EG, Okkes IM. Patients with fatigue in family practice: prevalence and treatment [article in Dutch] Ned Tijdschr Geneeskd. 1999;143:796–801. [PubMed] [Google Scholar]
- 17.Ream E, Richardson A. Fatigue in patients with cancer and chronic obstructive airways disease: a phenomenological enquiry. Int J Nurs Stud. 1997;34:44–53. doi: 10.1016/s0020-7489(96)00032-6. [DOI] [PubMed] [Google Scholar]
- 18.Zautra AJ, Fasman R, Parish BP, et al. Daily fatigue in women with osteoarthritis, rheumatoid arthritis, and fibromyalgia. Pain. 2007;128:128–35. doi: 10.1016/j.pain.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Hwang SS, Chang VT, Rue M, et al. Multidimensional independent predictors of cancer-related fatigue. J Pain Symptom Manage. 2003;26:604–14. doi: 10.1016/s0885-3924(03)00218-5. [DOI] [PubMed] [Google Scholar]
- 20.Hilsabeck RC, Hassanein TI, Perry W. Biopsychosocial predictors of fatigue in chronic hepatitis C. J Psychosom Res. 2005;58:173–8. doi: 10.1016/j.jpsychores.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Okkes IM, Oskam SK, Lamberts H. The probability of specific diagnoses for patients presenting with common symptoms to Dutch family physicians. J Fam Pract. 2002;51:31–6. [PubMed] [Google Scholar]
- 22.Elnicki DM, Shockcor WT, Brick JE, et al. Evaluating the complaint of fatigue in primary care: diagnoses and outcomes. Am J Med. 1992;93:303–6. doi: 10.1016/0002-9343(92)90237-6. [DOI] [PubMed] [Google Scholar]
- 23.Kirk J, Douglass R, Nelson E, et al. Chief complaint of fatigue: a prospective study. J Fam Pract. 1990;30:33–41. [PubMed] [Google Scholar]
- 24.Kroenke K, Wood DR, Mangelsdorff AD, et al. Chronic fatigue in primary care. Prevalence, patient characteristics, and outcome. JAMA. 1988;260:929–34. [PubMed] [Google Scholar]
- 25.Ridsdale L, Evans A, Jerrett W, et al. Patients with fatigue in general practice: a prospective study. BMJ. 1993;307:103–6. doi: 10.1136/bmj.307.6896.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Terluin B, van Marwijk HW, Ader HJ, et al. The Four-Dimensional Symptom Questionnaire (4DSQ): a validation study of a multidimensional self-report questionnaire to assess distress, depression, anxiety and somatization. BMC Psychiatry. 2006;6:34. doi: 10.1186/1471-244X-6-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arrindell WA, Ettema JHM. SCL-90: handleiding bij een multidimensionele psy-chopathologie-indicator. Lisse (the Netherlands): Swets & Zeitlinger; 1986. [SCL-90: manual for a multidimensional psychopathology indicator] [Google Scholar]
- 28.Hendriks A, Ormel J, Willige G. Long-term difficulties measured with self-report questionnaire and semi-structured interview [Dutch] Gedrag Gezond. 1990;18:273–83. [Google Scholar]
- 29.International classification of primary care. 2nd ed. Oxford (UK): Oxford University Press; 1998. [Google Scholar]
- 30.Okkes IM, Becker HW, Bernstein RM, et al. The March 2002 update of the electronic version of ICPC-2. A step forward to the use of ICD-10 as a nomenclature and a terminology for ICPC-2. Fam Pract. 2002;19:543–6. doi: 10.1093/fampra/19.5.543. [DOI] [PubMed] [Google Scholar]
- 31.Nijrolder I, van der Windt DA, van der Horst HE. Prognosis of fatigue and functioning in primary care: a 1-year follow-up study. Ann Fam Med. 2008;6:519–27. doi: 10.1370/afm.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Knottnerus JA, Starmans R, Vissers A. Diagnostische conclusies van de huisarts naar aanleiding van onverklaarde moeheid. Huisarts Wet. 1987;30:9–12. [Google Scholar]
- 33.Morrison JD. Fatigue as a presenting complaint in family practice. J Fam Pract. 1980;10:795–801. [PubMed] [Google Scholar]
- 34.Kenter EG, Okkes IM, Oskam SK, et al. Tiredness in Dutch family practice. Data on patients complaining of and/or diagnosed with “tiredness. Fam Pract. 2003;20:434–40. doi: 10.1093/fampra/cmg418. [DOI] [PubMed] [Google Scholar]
- 35.Hickie IB, Hooker AW, Hadzi-Pavlovic D, et al. Fatigue in selected primary care settings: sociodemographic and psychiatric correlates. Med J Aust. 1996;164:585–8. doi: 10.5694/j.1326-5377.1996.tb122199.x. [DOI] [PubMed] [Google Scholar]
- 36.Manu P, Lane TJ, Matthews DA. Chronic fatigue and chronic fatigue syndrome: clinical epidemiology and aetiological classification. Ciba Found Symp. 1993;173:23–31. doi: 10.1002/9780470514382.ch3. [DOI] [PubMed] [Google Scholar]
- 37.Ridsdale L, Evans A, Jerrett W, et al. Patients who consult with tiredness: frequency of consultation, perceived causes of tiredness and its association with psychological distress. Br J Gen Pract. 1994;44:413–6. [PMC free article] [PubMed] [Google Scholar]
- 38.Culpepper L. Insomnia: a primary care perspective. J Clin Psychiatry. 2005;66 (Suppl 9):14–7. [PubMed] [Google Scholar]
- 39.Doghramji PP. Recognizing sleep disorders in a primary care setting. J Clin Psychiatry. 2004;65(Suppl 16):23–6. [PubMed] [Google Scholar]
- 40.Pagel JF. The burden of obstructive sleep apnea and associated excessive sleepiness. J Fam Pract. 2008;57(Suppl):S3–8. [PubMed] [Google Scholar]