Abstract
Introduction
A large variety of therapeutic modalities for calcaneal fractures have been described in the literature. No single treatment modality for displaced intra-articular calcaneal fractures has proven superior over the other. This review describes and compares the different percutaneous distractional approaches for intra-articular calcaneal fractures. The history, technique, anatomical and fracture considerations, limitations and the results of different distractional approaches reported in the literature are reviewed.
Method
Literature review on different percutaneous distractional approaches for displaced intra-articular calcaneal fractures.
Results
Eight studies in which application of a distraction technique was used for the treatment of calcaneal fractures were identified. Because of the use of different classification, techniques, and outcome scoring systems, a meta-analysis was not possible. A literature review reveals overall fair to poor result in 10–29% of patients. Ten up to 26% of patients are unable to return to work after percutaneous treatment of their fracture. A secondary arthrodesis has to be performed in 2–15% of the cases. Infectious complications occur in 2–15%. Some loss of reduction is reported in 4–67%.
Conclusion
Percutaneous distractional reduction and fixation appears to be a safe technique with overall good results and an acceptable complication rate, compared with other treatment modalities for displaced intra-articular calcaneal fractures. A meta-analysis, based on Cochrane Library criteria is not possible, because of a lack of level 1 and 2 trials on this subject.
Keywords: Calcaneus, Fracture, Minimal invasive, Percutaneous
Introduction
For many centuries the treatment of calcaneal fractures has been non-operative and included bandaging and elevation of the foot. The earliest published surgical attempts to reduce displaced fragments of a fractured calcaneus were by means of a pulley device, described by Clark in 1855 [8, 11, 31]. The first open reduction took place in a open fracture by Bell in 1882 [23] and the first open reduction and internal fixation (ORIF) by a lateral approach was performed by Morestin in 1902 [13].
In 1895, the radiographic visualization of fractures was introduced and many different treatment modalities, approaches and salvage procedures have been published since that time [23]. The minimal invasive techniques for the treatment of intra-articular calcaneal fractures have evolved from 1855 to present, but gained less popularity compared with ORIF. Minimal invasive surgery of calcaneal fractures can be divided into percutaneous reduction of fragments by Kirschner-wire leveraging [13, 28, 39, 53], application of external fixators [34, 48, 52], and percutaneous distraction of displaced fragments, thus applying the principle of ligamentotaxis with subsequent percutaneous screw fixation [30, 44].
This literature review deals with the treatment of displaced intra-articular calcaneal fractures (DIACF) by percutaneous distraction and screw fixation. The history of different distractional approaches reported in the literature is described, including a technical description, the anatomical and fracture considerations, their limitations, and the clinical outcome obtained.
History
The first skeletal traction applied for the reduction of a displaced calcaneal fracture was reported by Clark [8]. He described a pulley system, but did not elaborate on this method further. Since then, several techniques and traction devices were developed and applied in the treatment of DIACFs. In the early decades of the twentieth century the distraction methods were applied and were the most widely accepted treatment modality for displaced intra-articular calcaneal fractures [33].
The different distraction techniques can be divided into single-, two- and three-point distraction, using the number of inserted pins as points of skeletal distraction as common denominator.
Single-point distraction
Various authors described different single-point distraction techniques (Fig. 1). Some used the distraction as the only treatment [23, 51], while others used it to assist the reduction by additional interventions [6, 7, 22, 23, 38, 43, 51, 55].
Fig. 1.
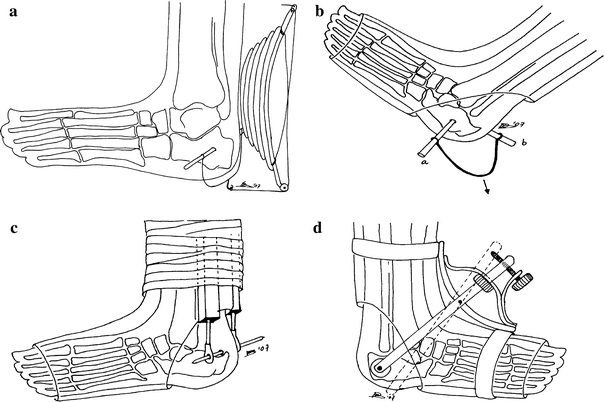
Single-point distraction techniques by Foldes [23] (1920; a), Kaess [23] (1922; b), Gillette [22] (c), and Carabba [7] (d)
Two-point (linear) distraction
In 1929, Böhler described the technique of closed reduction with a wooden wedge in the footsole, lateral clamp compression and traction on the calcaneus with countertraction on the tibia [4, 5]. Böhler changed this treatment strategy for calcaneal fractures repeatedly, and stopped using the transfixational pin through the tibia because of infectious complications [4, 5, 23, 35, 44]. Several authors applied the method used by Böhler completely or with (minor) modifications using specially designed traction devices [1, 9, 16, 17, 23, 33, 41, 47] (Fig. 2).
Fig. 2.
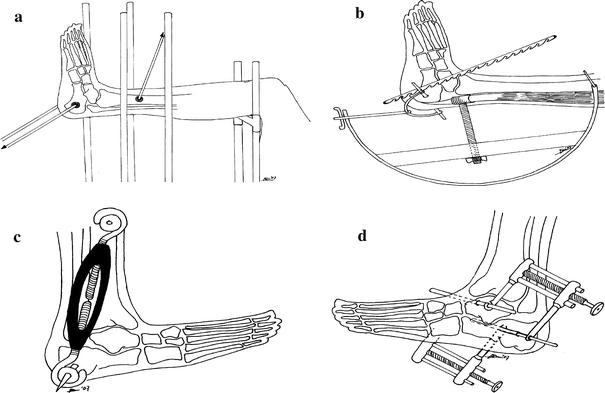
Two-point distraction techniques by Böhler [4] (1929; a), Conn [9] (b), Olson [41] (c) and Frohlich [17] (d)
Three-point (triangular) distraction
Three-point distraction was first introduced by McBride [37], followed by others [21, 26]. These triangular distraction methods were combined and formed the technique described by Forgon and Zadravecz in 1983 [15, 56]. This is currently one of the most frequently applied distraction techniques [29, 46, 54]. The three-point distraction approaches used nowadays differ in the direction of applied traction [14, 21, 26, 29, 37, 46, 54] (Fig. 3).
Fig. 3.
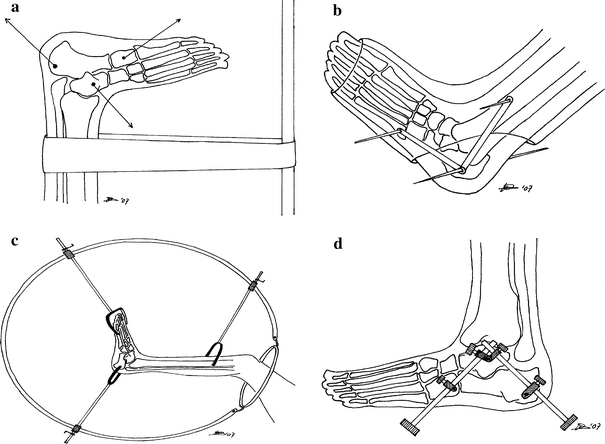
Three-point distraction techniques by Gill [21] (a), McBride [37] (b), Harris [26] (c) and Forgon-Zadravecz [15] (1983; d)
Biomechanical considerations
The subtalar joint is surrounded by a strong joint capsule and numerous ligaments, which stabilize the subtalar and ankle joints. The ligaments used in ligamentotaxis between the ankle joint, talus, and calcaneus are the calcaneofibular, the tibiocalcaneal ligament of the deltoid ligament, the talocalcaneal interosseous ligament, cervical and the anterior, lateral, posterior, and medial talocalcaneal ligaments. The plantar and dorsal calcaneonavicular ligaments and the calcaneonavicular portion of the bifurcate ligament are situated between the calcaneus and the navicular bone. The cuboid and calcaneus are connected by the dorsal calcaneocuboid ligament, the short and long plantar ligaments and the calcaneocuboid portion of the bifurcate ligament.
Ligamentotaxis, the indirect reposition of displaced osseous fragments through distraction on the ligaments attached to these fragments, restores the height of the posterior talocalcaneal joint and reduces the varus/valgus malalignment as well as the width of the calcaneal tuberosity. The lateral joint-fragment usually remains depressed, because the fracture lines run laterally to the interosseous ligament [20, 27]. This fragment needs to be lifted upwards using Kirschner-wire leveraging or a bone-punch inserted plantarly via the primary fracture line to restore the joint congruence [51].
It has been suggested that only Sanders type II DIACFs would benefit from distractional surgery, but the same has been said for severely comminuted calcaneal fractures, as anatomical reposition would be impossible even when using ORIF [21, 44]. The main benefit of percutaneous reduction and fixation is the protective nature of the technique towards the soft tissues. Only small stab incisions are made in the skin and the fracture haematoma is left in place, thus enhancing fracture healing [50].
Technique
Depending upon the distraction technique used, one to three Kirschner wires or Steinmann pins are inserted. The universal location, which is always used, is through the calcaneal tuberosity. Additional insertion sites are, depending on the applied technique, the tibia, the talar trochlea, the cuboid or the metatarsal bones. A distracting force is exerted from one distraction point or between two and three distraction points to reproduce the opposite force produced by the impact that caused the fracture. This procedure restores the arch of the foot and realigns the hindfoot, thereby restoring height and width, and reducing varus of the calcaneus.
Additional operative procedures to achieve reduction of fragments and to restore calcaneal anatomy include the Böhler press or clamp to reduce calcaneal widening and subsequent occurrence of impingement beneath the lateral malleolus [1, 4, 9, 16, 47]. Kirschner wires are used for additional leveraging of depressed fragments, especially the lateral joint fragment [6, 15, 18, 43, 51, 55]. A bone punch to unlock and lift up these fragments is preferred by others [46, 51, 54]. Percutaneous insertion of bone graft has been used, but no additional benefit was reported [51].
In order to improve the rate of anatomical fracture reduction, and therefore the overall outcome, several improvements have recently been implemented. The mobile C-arm system SIREMOBIL Iso-C3D enables intraoperative three-dimensional reconstructions of fracture reduction of the joint-surfaces. This was shown to be of value in ORIF of calcaneal fractures [45]. The same holds true for the intra-operative mobile CT-scanning [36]. The use of peroperative subtalar arthroscopy has been applied to obtain anatomic restoration of the posterior talocalcaneal joint, with a positive effect on outcome in retrospective series. [12, 19, 32, 40, 42].
Limitations and complications
Several concerns regarding the effectiveness of distraction techniques have been reported [1, 3, 24]. These include poor results in general, non-anatomical reduction, infectious complications and loss of reduction.
Poor results in general
Bankart reported clinically poor results using Böhler’s technique, probably because of the 3 months immobilization in plaster, which resulted in a stiff ankle joint [3]. His opinion was shared by others [24]. Currently, functional aftertreatment is applied shortly after surgery and outcome appears to be more favourable [15, 17, 46, 51].
Non-anatomical reduction
No universal treatment or surgical approach exists that can be applied to treat all fractures of the calcaneus [35]. The question remains whether adequate reduction of displaced intra-articular calcaneal fractures is even possible by closed methods [1]. Assessing the reduction on plain radiographs, by measuring the tuber-joint angle by Böhler, does not ensure a proper restoration of the posterior talocalcaneal facet [9, 10, 24]. As the percutaneous reduction of fractures is indirect, perfect anatomical restoration of the posterior facet anatomy and longitudinal arch of the foot should not be expected [9, 25, 30]. These effects might be amplified by the decrease in viability of the cartilage [2].
Infectious complications
The minimally invasive techniques were developed to protect the soft-tissues [30, 44, 50], but infectious complications do occur in patients treated percutaneously [46]. The later distraction techniques use screws situated subcutaneously rather than transosseous pins, which has resulted in a lower complication rate [15].
Loss of reduction
Percutaneously placed screws might provide a less rigid fixation of fracture fragments compared with plating, as collapse or loss of the obtained reduction has been reported after percutaneous reduction and subsequent fixation [46, 51, 54]. One study showed a similar strength of plating versus percutaneous screw fixation in Sanders type 2B fractures [49].
Literature review
A literature search was conducted in the electronic databases of Embase, Cochrane Library and PubMed using the following search-terms and Boolean operators: (‘calcaneus’ OR ‘os calcis’ OR ‘calcaneum’ OR ‘calcaneal’) AND ‘fracture’ AND (‘percutaneous’ OR ‘minimally invasive’) up to November 2008. Manuscripts were reviewed by both authors. Manuscripts were considered eligible if treatment of displaced intra-articular calcaneal fractures by traction was used. In addition, the reference lists of these manuscripts were checked to find additional studies. Studies from 1990 and forward were selected, as these made better use of outcome scoring systems and computed tomography (CT) classifications.
In total, two review articles were identified [30, 44], and eight retrospective case series were included [14, 17, 29, 38, 46, 51, 54, 55]. The level of evidence, as suggested by the Cochrane Collaboration, was level IV (non-randomized series of patients compared with previous or historical controls) for cohort studies.
Considerable differences were found in these eight studies (Table 1) [14, 17, 29, 38, 46, 51, 54, 55]. There is a large variety in the number of treated fractures (15–265 fractures), amount of open fractures, the type of classification used, the severity of the fractures, the average duration of follow-up (12–68 months), and the outcome scoring applied. This makes the comparison of this data in a systematic review impossible.
Table 1.
Demographics for eight available studies concerning percutaneous distraction techniques
| Study (evidence level) | Trauma | Classification | Surgical treatment | np/nf | Age (years) | Male (%) | FU (months) | Outcome |
|---|---|---|---|---|---|---|---|---|
|
Walde [55] Level IV |
85% Fall 15% MVA |
Sanders 16% Type II 57% Type III 27% Type IV |
1-Point distraction (tuberosity + K-wire leveraging) | 63/67 | 46 (18–82) | 72 | 68 (24–120) |
Zwipp 61% (Very) good 39% Fair–poor |
|
Schepers [46] Level IV |
84% Fall 16% MVA |
Sanders 38% Type II 28% Type III 28% Type IV |
3-Point distraction (tuberosity-cuboid, tuberosity-talus + bone-punch) | 50/61 | 46 (16–65) | 72 | 35 (13–75) |
AOFAS 36% Excellent 36% Good 28% Fair–poor |
|
Stulik [51] Level IV |
96% Fall 4% Other |
Sanders 61% Type II 30% Type III 9% Type IV |
1-Point distraction (tuberosity + K-wire leveraging or bone-punch) | 176/205 | 44 (13–67) | 85 | 43 (25–87) |
CN 16% Excellent 56% Good 28% Fair–poor |
|
McGarvey [38] Level IV |
32% Fall 48% MVA 20% other |
Sanders 32% Type II 26% Type III 29% Type IV |
1-Point distraction (tuberosity + bone-punch) External fixation |
31/33 | 42 (19–64) | 77 | 25 (6–55) |
AOFAS 66 points (42–92) |
|
Frohlich (1999) [17] Level III |
NS | NS | 2-Point distraction (talus-tuberosity) | NS/94 | NS | NS | NS | Mod Merle d’Aubigne |
| 79% Good to excellent | ||||||||
|
Van Loon [54] Level IV |
73% Fall 7% MVA 20% Other |
Crosby-Fitzgibbons 93% Type II 7% Type III |
Forgon-Zadravecz 3-Point distraction (talus-cuboid, tuberosity- talus) |
15/15 | 44 (21–67) | 73 | 14 (6–26) |
CN 27% Excellent 47% Good 26% Fair–poor |
|
Kuner [29] Level IV |
NS | NS | 3-Point distraction (MT1-tuberosity, tibia-tuberosity) | −/45 | NS | NS | NS | Merle d’Aubigne |
| 71% Good to excellent | ||||||||
|
Forgon [14] Level IV |
NS |
Own classification 30% Type I 40% Type II 30% Type III |
3-Point distraction (talus-cuboid, tuberosity-talus) | −/265 | 41 | NS | 12 |
Own score 43% Excellent 47% Good 10% Fair–poor |
MVA motor vehicle accident, np number of patients, nf number of fractures, FU follow-up, CN Creighton-Nebraska outcome score, AOFAS American Orthopaedic Foot Ankle Society hindfoot score, NS not specified
Table 2 shows an overview of data on outcome and complications as mentioned in the eight studies included. A fair to poor result was seen in 10–39% of patients; 26% on average. Ten up to 26% of patients with a calcaneal fracture were unable to return to work. Considering complications encountered; a secondary arthrodesis was performed in 2–15%, infections occurred in 2–30%, and a loss of reduction was reported in 4–67% [14, 17, 29, 46, 51, 54, 55].
Table 2.
Outcome and complication rates after treatment of displaced intra-articular calcaneal fractures with percutaneous distraction techniques
| Study | Fair/poor result (%) | Unable to work (%) | Loss of reduction (%) | Infection (%) | Arthrodesis (%) |
|---|---|---|---|---|---|
| Walde [55] | 39 | NS | 1 | 13 | NS |
| Schepers [46] | 28 | 10 | 30 | 15 | 15 |
| Stulik [51] | 28 | 26 | 4.5 | 8.7 | NS |
| McGarvey [38] | NS | NS | NS | 30 | NS |
| Frohlich [17] | 21 | NS | NS | 2.1 | 2.1 |
| Van Loon [54] | 26 | NS | 67 | 13 | NS |
| Kuner [29] | 29 | NS | NS | NS | NS |
| Forgon [14] | 10 | NS | 4.1 | 3.7 | NS |
NS not specified
To date, no randomized trial comparing the percutaneous distractional technique with ORIF or conservative treatment of intra-articular calcaneal fractures has been reported. In one study, two retrospective series of open and percutaneously treated patients were compared. This study revealed a favourable outcome and low complication rate for the percutaneously treated group [17].
Conclusion
The percutaneous approach with the use of distractional force is the oldest operative treatment for intra-articular calcaneal fractures. A total of eight studies were identified in the literature. Because of large differences in these studies, and the lack of randomized trials in which the percutaneous techniques are evaluated, a meta-analysis was impossible. However, overall treatment outcome was good in most studies. One study showed improved outcome in percutaneously treated patients compared to patients treated with ORIF.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Arnesen A. Fracture of the os calcis and its treatment. II. A contribution to the discussion on the treatment of calcaneus fracture based on an analysis of a ten-year material treated by closed reduction and traction, from Sentralsykehuset i Trondheim. Acta Chir Scand. 1958;15(Suppl 234):1–51. [PubMed] [Google Scholar]
- 2.Ball ST, Jadin K, Allen RT, Schwartz AK, Sah RL, Brage ME. Chondrocyte viability after intra-articular calcaneal fractures in humans. Foot Ankle Int. 2007;28(6):665–668. doi: 10.3113/FAI.2007.0665. [DOI] [PubMed] [Google Scholar]
- 3.Bankart ASB. Fractures of the os calcis. Lancet. 1942;240(6207):175. doi: 10.1016/S0140-6736(00)41474-1. [DOI] [Google Scholar]
- 4.Böhler L. Diagnosis, pathology and treatment of fractures of the os calcis. J Bone Joint Surg. 1931;13:75–89. [Google Scholar]
- 5.Böhler L. Die Technik der Knochenbruchbehandlung. Wien Band II: Verlag Wilhelm Maudrich; 1957. pp. 2148–2217. [Google Scholar]
- 6.Buch J, Blauensteiner W, Scherafati T, Vischer HM, Fischer W. [Conservative treatment of calcaneus fracture versus repositioning and percutaneous bore wire fixation. A comparison of 2 methods] Unfallchirurg. 1989;92(12):595–603. [PubMed] [Google Scholar]
- 7.Carabba V. Apparatus for treatment of fractured os calcis. Am J Surg. 1936;33(1):53–59. doi: 10.1016/S0002-9610(36)90629-3. [DOI] [Google Scholar]
- 8.Clark LG. Fracture of the os calcis. Lancet. 1855;65(1651):403–404. doi: 10.1016/S0140-6736(02)61561-2. [DOI] [Google Scholar]
- 9.Conn HR. The treatment of fractures of the os calcis. J Bone Joint Surg Am. 1935;17(2):392–405. [Google Scholar]
- 10.Dunlop J. The traction treatment of fractures of the os calcis. Surg Gynec Obst. 1940;70:408–412. [Google Scholar]
- 11.Eastwood DM, Phipp L. Intra-articular fractures of the calcaneum: why such controversy? Injury. 1997;28(4):247–259. doi: 10.1016/S0020-1383(97)00012-0. [DOI] [PubMed] [Google Scholar]
- 12.Elgafy H, Ebraheim NA. Subtalar arthroscopy for persistent subfibular pain after calcaneal fractures. Foot Ankle Int. 1999;20(7):422–427. doi: 10.1177/107110079902000705. [DOI] [PubMed] [Google Scholar]
- 13.Essex-Lopresti P. Mechanism, reduction technique and results in fractures of os calcis. Br J Surg. 1952;39:395–419. doi: 10.1002/bjs.18003915704. [DOI] [PubMed] [Google Scholar]
- 14.Forgon M. Closed reduction and percutaneous osteosynthesis: Technique and results in 265 calcaneal fractures. In: Tscherne H, Schatzker J, editors. Major fractures of the pilon, the talus, and the calcaneus. New York: Springer-Verlag; 1993. pp. 207–213. [Google Scholar]
- 15.Forgon M, Zadravecz G. Die Kalkaneusfraktur. Berlin: Springer; 1999. pp. 1–104. [Google Scholar]
- 16.Forrester CRG. Acute fractures of the os calcis. Am J Surg. 1934;25:404–413. doi: 10.1016/S0002-9610(34)90206-3. [DOI] [Google Scholar]
- 17.Frohlich P, Zakupszky Z, Csomor L. [Experiences with closed screw placement in intra-articular fractures of the calcaneus. Surgical technique and outcome] Unfallchirurg. 1999;102(5):359–364. doi: 10.1007/s001130050418. [DOI] [PubMed] [Google Scholar]
- 18.Fujii T, Takakura Y, Tanaka Y, Kitada C. Surgical tip: manipulation of closed pinning for intraarticular calcaneal fracture. Foot Ankle Int. 2004;25(9):685–686. doi: 10.1177/107110070402500915. [DOI] [PubMed] [Google Scholar]
- 19.Gavlik JM, Rammelt S, Zwipp H. Percutaneous, arthroscopically-assisted osteosynthesis of calcaneus fractures. Arch Orthop Trauma Surg. 2002;122(8):424–428. doi: 10.1007/s00402-002-0397-4. [DOI] [PubMed] [Google Scholar]
- 20.Giachino AA, Uhthoff HK. Intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 1989;71(5):784–787. [PubMed] [Google Scholar]
- 21.Gill GG. A three pin method for treatment of severely comminuted fractures of the os calcis. Surg, Gynec and Obstet. 1944;78:653–656. [Google Scholar]
- 22.Gillette E. An apparatus for treatment of fractures of the os calcis. J Bone Joint Surg Am. 1930;12:670–671. [Google Scholar]
- 23.Goff C. Fresh fractures of the os calcis. Arch Surg. 1938;36:744–765. [Google Scholar]
- 24.Gray CH. Crush fractures of the os calcis. Lancet. 1942;239(6178):106–108. doi: 10.1016/S0140-6736(00)79348-2. [DOI] [Google Scholar]
- 25.Harding M. Os calcis fracture, a new method of reduction. J Bone Joint Surg Am. 1926;8:720–722. [Google Scholar]
- 26.Harris RI. Fractures of the os calcis; their treatment by tri-radiate traction and subastragalar fusion. Ann Surg. 1946;124:1082–1100. doi: 10.1097/00000658-194612000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Herzenberg JE. CT of calcaneal fractures. AJR Am J Roentgenol. 1986;146(3):644–645. doi: 10.2214/ajr.146.3.644. [DOI] [PubMed] [Google Scholar]
- 28.King RE. Axial pin fixation of fractures of the Os calcis (method of Essex-Lopresti) Orthop Clin North Am. 1973;4(1):185–188. [PubMed] [Google Scholar]
- 29.Kuner EH, Bonnaire F, Hierholzer B. [Classification and osteosynthesis technique of calcaneus fractures. External fixator as temporary distractor] Unfallchirurg. 1995;98(6):320–327. [PubMed] [Google Scholar]
- 30.Levine DS, Helfet DL. An introduction to the minimally invasive osteosynthesis of intra-articular calcaneal fractures. Injury. 2001;32(Suppl 1):SA51–SA54. doi: 10.1016/s0020-1383(01)00061-4. [DOI] [PubMed] [Google Scholar]
- 31.Lindsay WR, Dewar FP. Fractures of the os calcis. Am J Surg. 1958;95(4):555–576. doi: 10.1016/0002-9610(58)90438-0. [DOI] [PubMed] [Google Scholar]
- 32.Lui TH. Arthroscopic subtalar release of post-traumatic subtalar stiffness. Arthroscopy. 2006;22(12):1364 e1–1364 e4. doi: 10.1016/j.arthro.2006.05.028. [DOI] [PubMed] [Google Scholar]
- 33.MacAusland W. The treatment of comminuted fractures of the os calcis. Surg Gynec Obst. 1941;73:671–675. [Google Scholar]
- 34.Magnan B, Bortolazzi R, Marangon A, Marino M, Dall’Oca C, Bartolozzi P. External fixation for displaced intra-articular fractures of the calcaneum. J Bone Joint Surg Br. 2006;88(11):1474–1479. doi: 10.1302/0301-620X.88B11.17759. [DOI] [PubMed] [Google Scholar]
- 35.Magnuson PB, Stinchfield F. Fracture of the os calcis. Am J Surg. 1938;42:685–692. doi: 10.1016/S0002-9610(38)91114-6. [DOI] [Google Scholar]
- 36.Mayr E, Hauser H, Ruter A, Bohndorf K. [Minimally invasive intraoperative CT-guided correction of calcaneal osteosynthesis] Unfallchirurg. 1999;102(3):239–244. doi: 10.1007/s001130050398. [DOI] [PubMed] [Google Scholar]
- 37.McBride E. Fractures of the os calcis; tripod-pin-traction apparatus. J Bone Joint Surg. 1944;26(3):578–579. [Google Scholar]
- 38.McGarvey WC, Burris MW, Clanton TO, Melissinos EG. Calcaneal fractures: indirect reduction and external fixation. Foot Ankle Int. 2006;27(7):494–499. doi: 10.1177/107110070602700703. [DOI] [PubMed] [Google Scholar]
- 39.Nakaima N, Yamashita H, Tonogai R, Ikata T. A technique of dynamic reduction for displaced fractures of the thalamus of the calcaneum. Int Orthop. 1983;7(3):185–190. doi: 10.1007/BF00269504. [DOI] [PubMed] [Google Scholar]
- 40.Nehme A, Chaminade B, Chiron P, Fabie F, Tricoire JL, Puget J. [Percutaneous fluoroscopic and arthroscopic controlled screw fixation of posterior facet fractures of the calcaneus] Rev Chir Orthop Reparatrice Appar Mot. 2004;90(3):256–264. doi: 10.1016/s0035-1040(04)70102-6. [DOI] [PubMed] [Google Scholar]
- 41.Olson P. The treatment of fractures of the os calcis. J Bone Joint Surg Am. 1939;21:747–751. [Google Scholar]
- 42.Parisien JS, Vangsness T. Arthroscopy of the subtalar joint: an experimental approach. Arthroscopy. 1985;1(1):53–57. doi: 10.1016/s0749-8063(85)80079-7. [DOI] [PubMed] [Google Scholar]
- 43.Poigenfurst J, Buch J. [Treatment of severe fractures of the calcaneus by reposition and percutaneous bore wire fixation] Unfallchirurg. 1988;91(11):493–501. [PubMed] [Google Scholar]
- 44.Rammelt S, Amlang M, Barthel S, Zwipp H. Minimally-invasive treatment of calcaneal fractures. Injury. 2004;35(Suppl 2):SB55–SB63. doi: 10.1016/j.injury.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 45.Rubberdt A, Feil R, Stengel D, Spranger N, Mutze S, Wich M, Ekkernkamp A. [The clinical use of the ISO-C(3D) imaging system in calcaneus fracture surgery] Unfallchirurg. 2006;109(2):112–118. doi: 10.1007/s00113-005-1015-z. [DOI] [PubMed] [Google Scholar]
- 46.Schepers T, Schipper IB, Vogels LM, Ginai AZ, Mulder PG, Heetveld MJ, Patka P. Percutaneous treatment of displaced intra-articular calcaneal fractures. J Orthop Sci. 2007;12(1):22–27. doi: 10.1007/s00776-006-1076-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schofield R. Fractures of the os calcis. J Bone Joint Surg Am. 1936;18:566–580. [Google Scholar]
- 48.Schwall R, Junge RH, Zenker W, Besch L. [Treatment of intra-articular calcaneus fractures with a para-articular external fixator] Unfallchirurg. 2000;103(12):1065–1072. doi: 10.1007/s001130050670. [DOI] [PubMed] [Google Scholar]
- 49.Smerek JP, Kadakia A, Belkoff SM, Knight TA, Myerson MS, Jeng CL. Percutaneous screw configuration versus perimeter plating of calcaneus fractures: a cadaver study. Foot Ankle Int. 2008;29(9):931–935. doi: 10.3113/FAI.2008.0931. [DOI] [PubMed] [Google Scholar]
- 50.Stein H, Rosen N, Lerner A, Kaufman H. Minimally invasive surgical techniques for the reconstruction of calcaneal fractures. Orthopedics. 2003;26(10):1053–1056. doi: 10.3928/0147-7447-20031001-15. [DOI] [PubMed] [Google Scholar]
- 51.Stulik J, Stehlik J, Rysavy M, Wozniak A. Minimally-invasive treatment of intra-articular fractures of the calcaneum. J Bone Joint Surg Br. 2006;88(12):1634–1641. doi: 10.1302/0301-620X.88B12.17379. [DOI] [PubMed] [Google Scholar]
- 52.Talarico LM, Vito GR, Zyryanov SY. Management of displaced intraarticular calcaneal fractures by using external ring fixation, minimally invasive open reduction, and early weightbearing. J Foot Ankle Surg. 2004;43(1):43–50. doi: 10.1053/j.jfas.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 53.Tornetta P., 3rd The Essex-Lopresti reduction for calcaneal fractures revisited. J Orthop Trauma. 1998;12(7):469–473. doi: 10.1097/00005131-199809000-00007. [DOI] [PubMed] [Google Scholar]
- 54.Van Loon C, Roumen R. Percutane repositie en fixatie van gedisloceerde intra-articulaire calcaneusfracturen: ervaringen bij de eerste vijftien patiënten. Ned Tijdschr Trauma. 1997;2:31–37. [Google Scholar]
- 55.Walde TA, Sauer B, Degreif J, Walde HJ. Closed reduction and percutaneus Kirschner wire fixation for the treatment of dislocated calcaneal fractures: surgical technique, complications, clinical and radiological results after 2–10 years. Arch Orthop Trauma Surg. 2008;128(6):585–591. doi: 10.1007/s00402-008-0590-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zadravecz G, Szekeres P. [Late results of our treatment method in calcaneus fractures] Aktuelle Traumatol. 1984;14(5):218–226. [PubMed] [Google Scholar]


