Abstract
Objectives
Although mental health treatment dropout is common, patterns and predictors of dropout are poorly understood. This study explores patterns and predictors of mental health treatment dropout in a nationally representative sample.
Methods
Data come from the National Comorbidity Survey Replication (NCS-R), a nationally representative household survey. Respondents in mental health treatment in the 12 months (n=1,664) before interview were asked about dropout defined as quitting treatment before the provider wanted. Cross-tabulation and discrete-time survival analyses were used to identify predictors.
Results
Approximately one-fifth (22.4%) of patients quit treatment prematurely. The highest dropout rate was from the general medical sector (31.6%) and the lowest was from psychiatrists (15.1%). Dropout rates were intermediate in the human service sector (19.7%) and among patients seen by non-psychiatrist mental health professionals (18.9%). Over 70% of all dropout occurred after the first or second visits. Mental health insurance was associated with low odds of dropout (0.6, 0.4–0.9). Psychiatric comorbidity was associated with a trend towards dropout. Several patient characteristics differentially predicted dropout across treatment sectors and in early and later phases of treatment.
Conclusions
Roughly one-fifth of adults in mental health treatment each year drop out before completing the recommended course of treatment. Dropout is most common in the general medical sector and varies by patient characteristics across treatment sectors. Interventions focused on high-risk patients and sectors will likely be required to reduce the high proportion of patients who prematurely terminate treatment.
Keywords: Mental health treatment adherence, treatment dropout, termination of treatment
Many outpatients fail to complete the recommended course of treatment (1,2). Patient-initiated treatment dropout is widespread (3–5,10,11) and limits treatment effectiveness (6,7). Because patients commonly receive mental health treatment from several different professionals (12, 13), focusing on a single treatment sector may overstate dropout from all sources of care.
Few studies compare treatment dropout across multiple treatment sectors. One recent Canadian study reported that dropping out of treatment -- defined as stopping before completing recommended treatment or before improvement -- was lowest for patients treated by primary care physicians (11.8%) followed by psychologists (21.9%), psychiatrists (22.7%), and nurses (29.1%) (1). A combined analysis of National Comorbidity Survey (1990–1992) and Ontario Health Survey (1990) data found that dropout was lower among patients treated within settings that could provide psychotherapy and pharmacotherapy than among other settings (14). Neither study assessed treatment continuity for individuals across sectors, a key domain of care continuity.
Gender has not been found to predict dropout (14), though younger adults may be more likely than older clients to drop out (1,14,15). Socio-economic disadvantage, including ethnic minority status (1), low income (14), lack of health insurance (2, 14), lower educational attainment (15), and unemployment (15) has been linked to dropout. Findings have been inconsistent across studies, however, perhaps due to methodological differences.
In the current report, a uniform definition of treatment dropout is applied to a nationally representative sample of adults with a range of disorders who received care from several treatment sectors. We explore patient socio-demographic and clinical factors related to early and late dropout. We seek to inform efforts to understand the clinical significance of dropout and to inform efforts to improve treatment engagement and outcomes.
METHODS
Sample
The NCS-R is a nationally representative household survey of adults (ages 18+) in the coterminous United States (16). Face-to-face interviews were conducted with 9,282 respondents (2001–2003) by professional interviews. The response rate was 70.9%. Part I included a core diagnostic assessment of DSM-IV mental disorders along with questions on service use and pharmacology administered to all 9,282 respondents. Part II included questions about correlates and additional disorders. Part II was administered to a probability sub-sample of 5,692 Part I respondents that included 100% of those who met lifetime criteria for any Part I disorder and a probability sub-sample of other respondents. The current analysis was limited to Part II respondents who reported treatment in the past 12 months for problems with “emotions or nerves” or drug or alcohol use. NCS-R procedures were approved by the Human Subjects Committees of Harvard Medical School and University of Michigan.
Measures
Mental health service sectors
Sources of care were classified into four sectors: psychiatrist; other mental health specialty sector treatment (psychologist or other non-psychiatrist mental health professional in any setting or social worker/counselor in a mental health specialty setting, or use of a mental health hotline); general medical treatment (primary care doctor, other general medical doctor, nurse, any other health professional not previously mentioned); and human service treatment (religious or spiritual advisor or social worker/counselor in any setting other than a specialty mental health setting). In the NCS-R the complementary-alternative medicine (CAM) sector is defined as treatment from healers and self-help groups.
Socio-demographic predictor variables
These included age (18–29, 30–44, 45–59, 60+), gender, race-ethnicity (Non-Hispanic white, Non-Hispanic black, Hispanic, Other), marital status (married/cohabitating, previously married, never married), completed years of education (0–15, 16+), urbanicity, and family income. Family income was defined by multiples of the poverty line as either low (≤1.5 times), low-average (1.5+ to 3 times), high-average (3+ to 6 times), and high (6+ times). Health insurance for treatment of mental disorders (yes-no) was also examined as a predictor of dropout.
Health service predictor variables
Respondents were classified by any prior lifetime history of mental health utilization, including inpatient care, outpatient counseling/psychotherapy, or prescription of psychotropic medications. Number of different provider groups seen in the past 12 months for mental health treatment and treatment stage (measured by number of visits at time of dropout) were also examined as predictors.
Diagnostic predictor variables
DSM-IV diagnoses were made using the WHO Composite International Diagnostic Interview (CIDI) Version 3.0 (17), a fully-structured lay-administered diagnostic interview of any DSM-IV (19) mood, anxiety, substance, and intermittent explosive disorder (IED). A blind clinical reappraisal study using the Structured Clinical Interview for DSM-IV (SCID) (20) as the validation standard showed generally good concordance between DSM-IV CIDI and SCID diagnoses for anxiety, mood, and substance disorders. The CIDI diagnosis of IED was not validated.
Treatment dropout
For each treatment sector, respondents were asked whether they received treatment in the past 12 months and, if so, whether treatment had stopped or was ongoing. Respondents who stopped treatment in that sector were asked whether they “quit before the [provider(s) in that sector] wanted [them] to stop.” Respondents who reported quitting before the provider(s) wanted them to stop are classified as having dropped out from that treatment sector. Respondents who reported 20 or more visits in the past 12-months in any single sector were classified as being stably in treatment whether or not they subsequently dropped out. A separate variable (“overall drop out”) denotes dropping out from all sectors. Because self-help groups have no providers, it was not possible to determine whether drop out occurred before the provider wanted. In addition, the number of respondents seeking treatment from healers in the past 12 months was too small to analyze independently (62). Therefore, analyses of dropout predictors from CAM are not conducted, although adjunctive CAM treatment in the past 12 months is used as a predictor of dropout from other sectors.
Analysis Procedures
NCS-R data were weighted to adjust for differences in selection probabilities, differential non-response, and residual differences between the sample and US population on socio-demographic variables. An additional weight was used in the Part II sample to adjust for over-sampling of Part I cases (16). Twelve-month treatment episodes were aggregated into the four treatment sectors. Basic patterns were examined within sector of the median number and interquartile range of visits and the proportion of patients that had dropped out, completed, and were still in treatment. Kaplan-Meier curves were used to examine dropout by number of visits. Predictors of dropout were examined with discrete-time survival analysis. Separate models examined dropout after the first two visits versus later visits. Differences in predictors across sectors were examined with interaction terms between predictors and dummy variables for sector. Standard errors were estimated using the SUDAAN (21) software system to adjust for clustering and weighting data. Multivariate significance tests were conducted using Wald χ2 tests based on coefficient variance–covariance matrices adjusted for design effects using the Taylor series method. Statistical significance was evaluated using two-sided design-based tests (α=.05).
RESULTS
Treatment within sectors
General medical sector is the most common treatment sector, accounting for approximately half of treatment episodes (Table 1). The longest treatment episodes measured by average number of visits, though, are to other mental health professionals followed by psychiatrists. A majority of 12-month patients were in treatment at the time of interview. The proportion of patients who dropped out differ significantly across sectors from general medical sector (32%) followed by human services (20%), other mental health (19%), and psychiatrists (15%) (Table 1).
Table 1.
Distribution of treatment across treatment sectors1
| Proportion of patients in the sector who …2 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Distribution of patients across sectors |
Average number of visits within sector |
… dropped out of treatment3 |
… completed treatment3 |
… were still In treatment3 |
||||||||||
| N1 | % | SE | Median | IQR | N1 | % | SE | N1 | % | SE | N1 | % | SE | |
| Psychiatrist | 400 | 24 | 1 | 3 | 1–7 | 50 | 15 | 2 | 95 | 23 | 2 | 255 | 62 | 4 |
| Other Mental Health professional | 591 | 35 | 2 | 7 | 2–20 | 108 | 19 | 2 | 157 | 27 | 2 | 326 | 54 | 2 |
| General Medical | 853 | 52 | 1 | 1 | 1–2 | 270 | 32 | 2 | 203 | 22 | 2 | 380 | 46 | 2 |
| Human Services | 303 | 18 | 2 | 2 | 1–5 | 65 | 20 | 3 | 93 | 31 | 4 | 145 | 49 | 4 |
| Any4 | 1572 | 100 | 0 | 3 | 1–10 | 357 | 22 | 1 | 381 | 24 | 1 | 834 | 54 | 1 |
Unweighted number of respondents who received treatment in the sector. IQR denotes inter-quartile range.
Proportion (standard error) of patients in the sector either dropped out of treatment, completed treatment, or were still in treatment at the time of interview. These three proportions sum to 100% in each row.
The proportion of patients who dropped out of treatment varies significantly across sectors (χ23 = 49.3. p < .001). The proportion of patients who completed treatment, in comparison, does not varies significantly across sectors (χ23 = 5.5. p = .14). The proportion of patients still in treatment varies significantly when we compare across the four sectors (χ23 = 11.5, p = ..009).
Average number of visits in this row represents the median across all sectors, not within any one sector, among patients treated in one or more sectors. The 23% reported in this row to have dropped out of treatment represents those who dropped out in treatment in all sectors. Patient treated in multiple sectors over the 12-month period who were still in treatment in any of those sectors at the time of interview were classified still in treatment, while those no longer in any treatment who reported completing treatment in ay least one sector were classified as having completed treatment.
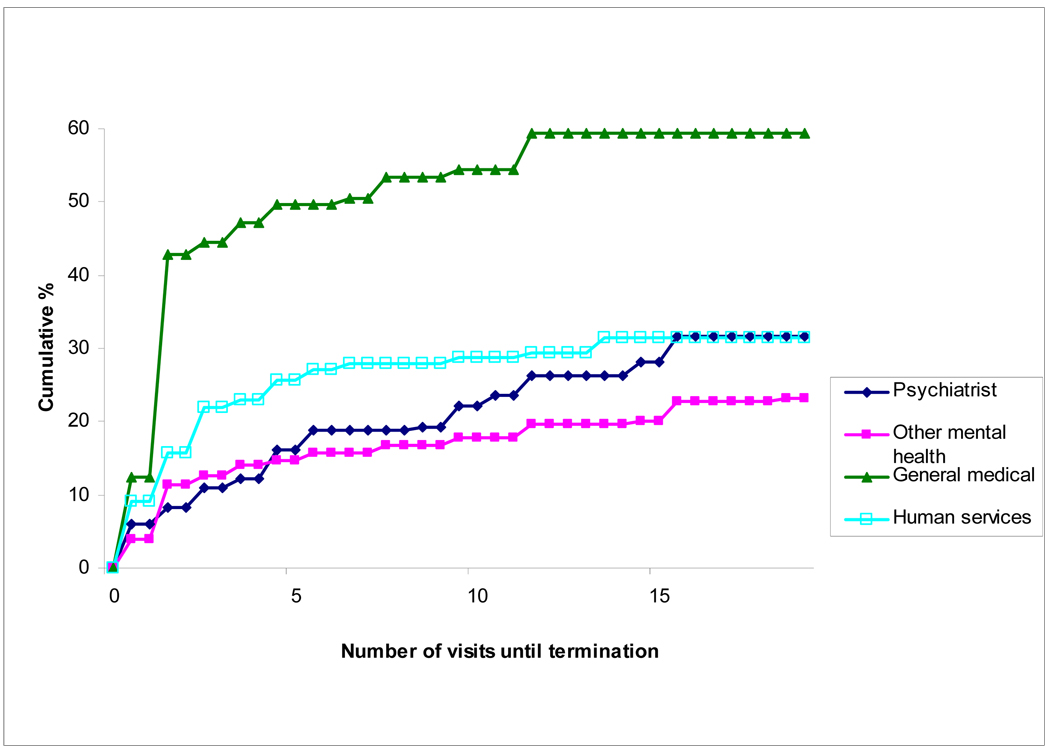
The cumulative probability of dropout varied significantly across the four sectors (Figure 1). Survival curves indicate that nearly 60% of patients eventually drop out of treatment from the general medical sector. Among patients who dropout, the median number of visits until dropout is 4–6 in the specialty mental health sector and 3 in the general medical and human services sectors.
Figure 1.
Cumulative probability of treatment dropout over the course of treatment by sector
Dropout across sectors
In multivariable models pooled across sectors, initial phase of treatment, absence of health insurance, provision of care in one or two sectors (versus 3–4), not receiving complementary-alternative medicine, and treatment in general medical sector significantly predicts elevated odds of dropout (Table 2). Treatment in the mental health specialty sector is associated with significantly reduced odds of dropout.
Table 2.
Predictors of treatment dropout overall and by sector1
| Treatment sector | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Psychiatrist | Other Mental Health Professions2 |
General Medical |
Human Services |
Significance of between- sector differences |
|||||||||||
| OR | CI | χ2 | OR | CI | χ2 | OR | CI | χ2 | OR | CI | χ2 | OR | CI | χ2 | χ2 | |
| Number of visits | ||||||||||||||||
| Initial (1–2) | 5.8* | 3.9–8.6 | 1.6 | .8–2.9 | 3.6* | 2.6–5.0 | 5.1* | 3.1–8.4 | 1.8 | .9–3.8 | ||||||
| Later (3+ visit) | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ21 | 83.0* | 2.0 | 59.4* | 43.6* | 2.8 | 17.4* | ||||||||||
| Age | ||||||||||||||||
| 18–29 | 1.0 | .6–1.7 | 2.2 | .3–14.0 | 2.0 | .3–11.3 | 1.2 | .6–2.6 | .4 | .1–1.4 | ||||||
| 30–44 | .9 | .6–1.4 | .7 | .1–3.2 | 1.0 | .6–1.7 | .7 | .2–2.6 | ||||||||
| 45–59 | .7 | .5–1.1 | .4 | .1–2.3 | .7 | .4–1.1 | .3 | .1–1.1 | ||||||||
| 60+ | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ23 | 3.6 | 8.8* | .6 | 4.9 | 6.7 | 473.7* | ||||||||||
| Gender | ||||||||||||||||
| Male | 1.0 | .7–1.3 | 2.2 | .8–5.6 | .8 | .5–1.5 | 1.3 | 1.0–1.8 | .3* | .1–.6 | ||||||
| Female | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ21 | .1 | 2.7 | .5 | 3.0 | 10.9* | 10.1* | ||||||||||
| Ethnicity | ||||||||||||||||
| Black | 1.0 | .6–1.7 | 2.4* | 1.0–5.6 | * | .6 | .2–1.6 | 1.3 | .8–2.0 | 1.0 | .2–4.0 | |||||
| Hispanic | 1.2 | .8–1.9 | 2.3 | .7–8.0 | 1.3 | .7–2.5 | 1.1 | .7–1.8 | 1.3 | .4–3.9 | ||||||
| Other | .9 | .4–2.0 | .0 | .0–.0 | .3 | .0–2.5 | 1.7 | .8–3.5 | 1.2 | .2–8.4 | ||||||
| Whites | 1.0 | -- | 1.0 | 1.0 | -- | 1.0 | -- | 1.0 | -- | |||||||
| χ23 | .8 | 484.1 | 4.0 | 3.0 | .2 | 3.9 | ||||||||||
| Marital statuss | ||||||||||||||||
| Married/Cohabitated | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| Sep/Div/Wid | .8 | .6–1.1 | .3* | .1–.7 | .5* | .3–.8 | .9 | .6–1.4 | 1.5 | .7–3.3 | ||||||
| Never Married | .9 | .6–1.3 | 1.1 | .4–2.7 | .9 | .5–1.5 | .8 | .6–1.2 | .8 | .4–1.8 | ||||||
| χ22 | 1.5 | 7.3* | 7.2* | 1.2 | 1.1 | 6.8 | ||||||||||
| Education | ||||||||||||||||
| 0–15 | 1.1 | .7–1.7 | 1.6 | .5–5.0 | 1.9* | 1.1–3.4 | .9 | .7–1.4 | 1.4 | .4–4.8 | ||||||
| 16+ | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ21 | .3 | .6 | 5.2* | .1 | .4 | 2.2 | ||||||||||
| Income | ||||||||||||||||
| Low | 1.0 | .6–1.6 | 4.1 | .8–21.8 | .9 | .4–2.0 | .9 | .6–1.4 | .4 | .1–1.4 | ||||||
| Average-low | 1.2 | .8–1.9 | 6.0* | 1.2–28.9 | 1.7 | .8–3.6 | .9 | .6–1.5 | 1.1 | .3–3.5 | ||||||
| Average-high | 1.1 | .7–1.7 | 1.8 | .5–6.8 | .8 | .4–2.0 | 1.1 | .6–2.1 | 2.2 | .8–6.5 | ||||||
| High | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ23 | 1.1 | 6.9 | 6.0 | 1.1 | 10.9* | 34.3* | ||||||||||
| Insurance (Yes/No) | .6* | .4–.9 | .3* | .1–.9 | .5* | .2–1.0 | .8 | .5–1.2 | 1.0 | .4–2.3 | ||||||
| χ21 | 6.2* | 4.9* | 4.0* | 1.4 | .0 | 1.2 | ||||||||||
| LT mental health treatment | .8 | .6–1.0 | .3* | .1–.8 | .7 | .4–1.3 | .8 | .6–1.1 | 1.0 | .5–2.0 | ||||||
| χ21 | 3.3 | 6.1* | 1.4 | 1.3 | .0 | 5.4 | ||||||||||
| Mental Disorders | ||||||||||||||||
| Any Mood | .7 | .5–1.0 | .8 | .3–1.9 | .9 | .5–1.7 | .6* | .4–.9 | 1.1 | .4–3.3 | 2.3 | |||||
| Any Anxiety | 1.1 | .7–1.5 | 1.5 | .5–4.1 | 1.3 | .7–2.7 | 1.0 | .7–1.4 | .8 | .3–2.1 | .4 | |||||
| Any Substance | .9 | .6–1.5 | .7 | .3–2.0 | 1.9* | 1.1–3.5 | 1.1 | .8–1.7 | 1.0 | .3–2.9 | 3.3 | |||||
| Any Impulse | .9 | .5–1.5 | 1.1 | .3–4.4 | .5 | .2–1.1 | .9 | .5–1.5 | 2.8* | 1.1–7.2 | 12.0* | |||||
| χ24 | 5.3 | 3.0 | 11.1* | 8.0 | 6.4 | 20.5 | ||||||||||
| # of disorders | ||||||||||||||||
| Only 1 | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| 2 or more | 1.3 | .8–2.1 | .4 | .1–2.5 | .5 | .2–1.3 | 1.5* | 1.0–2.3 | .7 | .2–2.9 | ||||||
| χ21 | 1.0 | .9 | 2.3 | 4.8* | .3 | 10.7* | ||||||||||
| Number of Providers | ||||||||||||||||
| 1 or 2 | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| 3 or 4 | .3* | .1–.6 | 1.0 | .4–2.3 | .9 | .5–1.6 | 1.0 | .7–1.4 | .5 | .2–1.0 | ||||||
| χ21 | 11.8* | .0 | .1 | .0 | 4.0* | 203.8* | ||||||||||
| Types of provider | ||||||||||||||||
| Complementary-alternative medicine (Y/N) | .3* | .2–.6 | .4 | .1–1.3 | .4* | .2–.9 | .2* | .1–.4 | .7 | .2–2.3 | ||||||
| χ21 | 14.2* | 2.6 | 5.5* | 27.1* | .3 | |||||||||||
| Psychiatrist | .3* | .1–.6 | ||||||||||||||
| Other Mental Health Profession | .6* | .3–1.0 | ||||||||||||||
| General Medical | 2.2* | 1.4–3.5 | ||||||||||||||
| Human Services | 1.0 | -- | ||||||||||||||
| χ23 | 81.3* | 2.4 | ||||||||||||||
| (n)3 | (1572) | (400) | (591) | (853) | (303) | |||||||||||
Significant at the .05 level of significance, two-sided test
Models are multivariate (all predictors in each column entered at once) and based on a survival framework (with person-visit file); each column represents a separate multivariate model of dropout from care in that sector.
For other mental health professions, the age categories are 18–59 vs 60 due to scarce data
Patients treated only in the complementary-alternative medicine sector were excluded from the analysis based on the low rate of dropout from complementary-alternative medicine treatment
Dropout after first or second visit is significantly associated with psychiatric comorbidity, care in only one sector, treatment in general medical sector, and complementary-alternative medicine (Table 3). Dropout after third or later visit is significantly associated with Hispanic ethnicity; average-low income; substance use disorder; treatment in general medical/human services sectors, absence of health insurance, previous mental health treatment, and psychiatric comorbidity (Table 4).
Table 3.
Predictors of treatment dropout overall and by sector after the first or second visits
| Treatment sector | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Psychiatrist | Other Mental Health Professions2 |
General Medical |
Human Services |
Significance of between-sector differences |
|||||||||||
| OR | CI | χ2 | OR | CI | χ2 | OR | CI | χ2 | OR | CI | χ2 | OR | CI | χ2 | χ2 | |
| Age | ||||||||||||||||
| 18–29 | .9 | .5–1.8 | 7.9* | 1.1–58.2 | .2–6.1 | 1.5 | .6–3.4 | .5 | .1–2.2 | |||||||
| 30–44 | .9 | .6–1.5 | 2.0 | .4–9.4 | 1.1 | 1.1 | .7–1.9 | .6 | .2–2.5 | |||||||
| 45–59 | .8 | .5–1.2 | .8 | .1–6.2 | .7 | .4–1.2 | .5 | .1–1.8 | ||||||||
| 60+ | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ23 | 1.0 | 12.5* | .0 | 4.7 | 1.8 | 439.3* | ||||||||||
| Gender | ||||||||||||||||
| Male | 1.1 | .7–1.6 | 4.5 | .9–22.2 | .8 | .4–1.8 | 1.4 | .9–2.1 | .2* | .1–.6 | ||||||
| Female | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ21 | .2 | 3.6 | .3 | 2.9 | 9.0* | 8.0* | ||||||||||
| Ethnicity | ||||||||||||||||
| Black | 1.2 | .7–2.0 | 2.5 | .9–7.1 | .5 | .2–1.5 | 1.5 | 1.0–2.3 | 1.6 | .4–6.7 | ||||||
| Hispanic | .9 | .5–1.5 | 2.6 | .6–10.6 | 1.0 | .4–2.5 | 1.0 | .6–1.6 | 1.4 | .3–6.6 | ||||||
| Other | .7 | .2–2.7 | .0* | .0–.0 | .4 | .1–3.6 | 1.5 | .5–4.3 | .4 | .0–6.1 | ||||||
| Whites | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ23 | .9 | 357.2* | 3.0 | 4.0 | 1.3 | 3.4 | ||||||||||
| Marital status | ||||||||||||||||
| Married/Cohabitated | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| Sep/Div/Wid | 1.0 | .6–1.4 | .5 | .2–1.5 | .9 | .4–2.1 | .9 | .6–1.3 | 1.7 | .7–4.3 | ||||||
| Never Married | 1.0 | .7–1.4 | .6 | .2–2.0 | 1.0 | .4–2.2 | .9 | .6–1.3 | .8 | .3–2.2 | ||||||
| χ22 | .1 | 1.7 | .1 | 1.1 | 1.7 | 6.8 | ||||||||||
| Education | ||||||||||||||||
| 0–15 | 1.1 | .7–1.6 | .9 | .2–4.4 | 1.6 | .9–3.0 | .9 | .6–1.3 | 2.2 | .5–10.2 | ||||||
| 16+ | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ21 | .2 | .0 | 2.4 | .2 | 1.1 | 2.2 | ||||||||||
| Income | ||||||||||||||||
| low | 1.0 | .6–1.8 | 10.5 | .9–122.5 | .5 | .1–1.9 | .9 | .5–1.5 | .8 | .1–4.6 | ||||||
| average-low | 1.1 | .6–1.8 | 2.0 | .2–19.3 | 1.7 | .7–4.5 | .8 | .5–1.5 | 3.1 | .5–18.9 | ||||||
| average-high | 1.1 | .7–1.8 | .6 | .0–7.4 | .6 | .2–1.9 | 1.3 | .6–2.5 | 6.2* | 1.1–33.2 | ||||||
| high | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ23 | .2 | 12.2* | 5.0 | 2.5 | 11.4* | 36.4* | ||||||||||
| Insurance (Yes/No) | .7 | .4–1.2 | .4 | .1–1.3 | .5 | .2–1.5 | .7 | .4–1.3 | 2.1 | .7–6.0 | ||||||
| χ21 | 2.1 | 2.6 | 1.7 | 1.2 | 1.9 | 2.3 | ||||||||||
| LT mental health treatment | .9 | .6–1.4 | .2* | .1–.6 | 1.2 | .5–2.7 | .8 | .6–1.2 | 1.4 | .6–3.3 | ||||||
| χ21 | .3 | 7.9* | .2 | 1.0 | .5 | 5.6 | ||||||||||
| Mental Disorders | ||||||||||||||||
| Any Mood | .6 | .4–1.0 | .3 | .1–1.6 | 1.3 | .6–2.7 | .7 | .5–1.1 | 1.2 | .3–4.0 | .7 | |||||
| Any Anxiety | 1.0 | .6–1.6 | 5.5 | .9–32.2 | 2.3 | .8–6.4 | .9 | .6–1.2 | .6 | .2–1.6 | 4.4 | |||||
| Any Substance | .6 | .3–1.0 | .5 | .1–2.7 | 1.8 | .8–4.0 | 1.0 | .6–1.7 | 1.0 | .3–3.7 | 4.9 | |||||
| Any Impulse | .7 | .3–1.5 | .4 | .1–1.5 | .2* | .0–.9 | .9 | .4–1.7 | 2.0 | .7–5.3 | 10.4* | |||||
| χ24 | 11.3* | 9.7* | 9.7* | 6.6 | 4.2 | 31.4* | ||||||||||
| # of disorders | ||||||||||||||||
| Only 1 | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| 2 or more | 2.5* | 1.4–4.6 | .4 | .1–2.4 | .5 | .1–1.6 | 1.7* | 1.1–2.7 | 1.1 | .3–4.4 | ||||||
| χ21 | 9.1* | 1.2 | 1.5 | 6.4* | .0 | 6.1 | ||||||||||
| Number of Providers | ||||||||||||||||
| 1 | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| 2 | .1* | .0–.3 | .7 | .3–1.9 | .3 | .1–.6 | .5* | .3–.9 | .5 | .2–1.1 | ||||||
| χ21 | 15.5* | .5 | 13.6* | 5.9* | 3.2 | 91.7* | ||||||||||
| Types of provider | ||||||||||||||||
| Complementary Med(Y/N) | .2* | .1–.5 | .2 | .0–2.7 | .2 | .0–1.7 | .2* | .1–.4 | .6 | .2–2.1 | ||||||
| χ21 | 10.7* | 1.5 | 2.4 | 18.6* | .6 | |||||||||||
| Psychiatrist | .4 | 1–1.3 | ||||||||||||||
| Other Mental Health Profession | 1.0 | .5–2.1 | ||||||||||||||
| General Medical | 2.9 | 1.6–5.5 | ||||||||||||||
| Human Services | 1.0 | -- | ||||||||||||||
| χ23 | 46.3* | 4.8 | ||||||||||||||
| (n)3 | (730) | (141) | (156) | (645) | (152) | |||||||||||
Models are multivariate (all predictors in each column entered at once) and based on a survival framework (with person-visit file); each column represents a separate multivariate model of dropout from care in that sector. Because the sample is restricted to those with 1–2 visits- it is not possible to have more than 2 providers.
For other mental health professions, the age categories are 18–59 vs 60 due to scarce data
Number of cases that received treatment from the provider
Table 4.
Predictors of treatment dropout overall and by sector after three or more visits
| Treatment sector | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Psychiatrist | Other Mental Health Professions2 |
General Medical |
Human Services |
Significance of between-sector differences |
|||||||||||
| OR | CI | χ2 | OR | CI | χ2 | OR | CI | χ2 | OR | CI | χ2 | OR | CI | χ2 | χ2 | |
| Age | ||||||||||||||||
| 18–29 | .6 | .2–2.2 | .2 | .0–4.8 | 1204.9–8930.0 | 1.2 | .2–8.4 | .7 | .0–25.0 | |||||||
| 30–44 | .5 | .2–1.3 | .1 | .0–1.8 | 3280.2* | 2.1 | .4–10.8 | 3.0 | .1–100.6 | |||||||
| 45–59 | .2 | .1–1.0 | .1 | .0–4.6 | 1.7 | .4–7.3 | .0* | .0–.0 | ||||||||
| 60+ | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ23 | 4.2 | 3.9 | 266.1* | 1.0 | 157.6* | 284.8* | ||||||||||
| Gender | ||||||||||||||||
| Male | .5 | .2–1.6 | 2.0 | .5–8.1 | .9 | .3–2.6 | 1.1 | .2–5.0 | .6 | .2–1.8 | ||||||
| Female | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ21 | 1.3 | 1.1 | .0 | .0 | .8 | 2.7 | ||||||||||
| Ethnicity | ||||||||||||||||
| Black | .4 | .1–1.6 | 4.0* | 1.0–15.0 | .5 | .1–2.0 | .0* | .0–.0 | .0* | .0-.0 | ||||||
| Hispanic | 3.3* | 1.3–8.5 | 2.7 | .2–29.7 | 1.3 | .5–3.5 | 1.6 | .2–11.4 | 8.9* | 1.1–73.5 | ||||||
| Other | 1.6 | .4–6.5 | .0* | .0–.0 | .0* | .0–.0 | 5.6 | .2–140.8 | 7.3 | .8–62.9 | ||||||
| Whites | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ23 | 8.8* | 75.5* | 499.6* | 98.2* | 450.6* | 1.9 | ||||||||||
| Marital status | ||||||||||||||||
| Married/Cohibitated | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| Sep/Div/Wid | .6 | .2–1.6 | .0* | .0–.7 | 1* | .0–.5 | 2.0 | .5–8.4 | .6 | .1–4.3 | ||||||
| Never Married | .8 | .3–2.0 | 2.8 | .6–14.4 | .7 | .3–1.5 | .8 | .2–4.3 | .6 | .1–4.0 | ||||||
| χ22 | 1.2 | 5.3 | 9.5* | 1.8 | .7 | 7.4 | ||||||||||
| Education | ||||||||||||||||
| 0–15 | 1.0 | .3–3.1 | 3.5 | .5–23.4 | 2.5 | .9–6.9 | .3 | .0–2.9 | 1.1 | .2–6.8 | ||||||
| 16+ | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ21 | .0 | 1.8 | 3.1 | 1.1 | .0 | 4.8 | ||||||||||
| Income | ||||||||||||||||
| Low | 1.9 | .7–5.4 | 1.0 | .2–5.8 | 2.8 | .8–9.6 | .7 | .0–14.5 | .5 | .1–2.9 | ||||||
| average-low | 4.6* | 1.4–14.9 | 54.4* | 8.1–366.1 | 2.9 | .9–8.6 | 3.6 | .4–29.8 | .7 | .2–3.1 | ||||||
| average-high | 1.8 | .5–6.1 | 5.0* | 1.0–23.7 | 2.0 | .6–6.3 | .1 | .0–3.2 | .8 | .1–5.3 | ||||||
| High | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| χ23 | 9.8* | 20.0* | 4.1 | 11.0* | .9 | 5.8 | ||||||||||
| Insurance (Yes/No) | .3* | .1–.7 | .1* | .0–.7 | .5* | .2–1.0 | 2.7 | .2–47.1 | .8 | .2–3.5 | ||||||
| χ21 | 8.0* | 6.2* | 4.6* | .5 | .1 | 4.0 | ||||||||||
| LT mental health treatment | .4* | .2–.8 | .3 | .1–1.7 | .5 | .2–1.1 | 2.2 | .6–8.6 | 1.2 | .3–4.7 | ||||||
| χ21 | 6.4* | 2.0 | 3.2 | 1.5 | .1 | 1.2 | ||||||||||
| Mental Disorders | ||||||||||||||||
| Any Mood | 1.0 | .4–2.4 | 2.0 | .3–11.3 | 1.0 | .3–3.1 | .4 | .0–5.9 | .7 | .1–5.3 | 1.3 | |||||
| Any Anxiety | 1.4 | .7–2.7 | .9 | .3–3.4 | 1.0 | .4–2.7 | 4.3 | .4–47.7 | 1.0 | .2–4.8 | 2.2 | |||||
| Any Substance | 4.5* | 1.9–10.7 | 3.0 | .8–11.8 | 2.3* | 1.0–5.2 | 4.5 | .7–27.5 | .7 | .2–2.9 | 8.9* | |||||
| Any Impulse | 1.4 | .4–5.1 | 10.8* | 1.7–67.9 | 1.1 | .4–2.9 | .9 | .1–13.5 | 3.6 | .6–20.7 | 1.5 | |||||
| χ24 | 14.1* | 9.0 | 7.8 | 9.2 | 2.7 | 15.0 | ||||||||||
| # of disorders | ||||||||||||||||
| Only 1 | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| 2 or more | .1* | .0–.6 | .1* | .0–.8 | .4 | .1–2.0 | .5 | .0–12.2 | .3 | .0–3.5 | ||||||
| χ21 | 8.4* | 5.0* | 1.5 | .2 | .9 | 5.0 | ||||||||||
| Number of Providers | ||||||||||||||||
| 1 or 2 | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | ||||||
| 3 or 4 | 4* | .2–1.0 | 2.1 | .8–6.0 | 1.4 | .6–3.0 | 6.5* | 1.2–36.8 | 1.1 | .2–6.7 | ||||||
| χ21 | 3.8* | 2.2 | .7 | 4.8* | .0 | 129.9* | ||||||||||
| Types of provider | ||||||||||||||||
| Complementary-alternative medicine (Y/N) | .4* | .1–1.0 | .8 | .2–3.7 | .7 | .3–1.7 | .0* | .0–.4 | 2.1 | .3–16.4 | ||||||
| χ21 | 4.0* | .1 | .6 | 7.5* | .6 | |||||||||||
| Psychiatrist | .4 | .1–1.4 | ||||||||||||||
| Other Mental Health Profession | .3* | .2–.6 | ||||||||||||||
| General Medical | 1.8 | .8–4.5 | ||||||||||||||
| Human Services | 1.0 | -- | ||||||||||||||
| χ23 | 16.6* | .9 | ||||||||||||||
| (n)5 | (842) | (259) | (435) | (208) | (151) | |||||||||||
Models are multivariate (all predictors in each column entered at once) and based on a survival framework (with person-visit file); each column represents a separate multivariate model. No extra controls (aside from the predictors specified in the table) were used for the models.
For other mental health professions, the age categories are 18–59 vs 60 and # of providers with 1 vs 2–4 instead due to scarce data
For interactions across providers, the categories used for age is 18–59 vs 60, for # of providers is 1 vs 2–4. Other categories are as specified in the rows. Interactions are done separately for each predictor instead of all interaction terms in the same model. Each interaction model controls for all predictors
Three df interaction tests done for types of disorders and # of disorders
Number of cases that received treatment from the provider
Several predictors differ significantly across sector or by timing of dropout, requiring a disaggregated analysis of predictors separately in each sector for early and later phases of treatment (Table 2–Table 4). Probability of treatment dropout in general medical/mental health specialty sectors (non-psychiatrists) is much higher after the first two visits than subsequent visits.
Age
Younger age significantly predicts dropout among patients treated by psychiatrists, an association limited to dropout after the first two visits. There is also a suggestion of a nonlinear association of age with dropout after ≥3 visits to human services, with highest odds of dropout among middle-aged patients.
Gender
Men were significantly less likely than women to leave treatment in the human services sector (OR:.3, 95% CI:.1–.6) (Table 2). This association was confined to the first two visits.
Race-ethnicity
As compared with Non-Hispanic whites, patients in the “Other” ethnic group are less likely to drop out, while Non-Hispanic black patients are more likely to drop out of psychiatric care, an association limited to dropout after the third visit. Although patient race-ethnicity does not significantly predict dropout from other provider groups in the overall model, several associations between patient race-ethnicity and dropout are evident among patients making at least 3 visits (Table 4).
Marital status
Married-cohabiting as compared with previously married patients have a higher odds of dropout from the mental health specialty sector.
Income
Income has a nonlinear association with dropout from human service treatment, with highest odds of dropout among average-high income patients. Average-high (versus high) income predicts human services dropout only after the first two visits. Average-low income is associated with increased odds of dropout from psychiatric care, but only after ≥3 visits.
Education
Low education (0–15 years) is associated with elevated odds of dropout from treatment with mental health professionals other than psychiatrists (OR: 1.9, 1,1–3.4), but not from other sectors (Table 2).
Mental health insurance
Mental health insurance is significantly associated with low odds of dropout from psychiatrist (OR:.3, 95% CI:.1–.9) and other mental health professionals (OR:.5, 95% CI:.2–1.0), but not other sectors (Table 2). Significant effects in the specialty sector, though, are confined to dropout after the third or later visit.
Past mental health treatment
A lifetime history of mental health treatment is significantly associated with low odds of dropout from psychiatric care (OR: .3, 95% CI: .1–.8) (Table 2), but not other sectors, and is limited to dropout after ≥2 visits (OR: .2, 95% CI: .1–.6) (Table 3).
Mental disorders
Patients with substance use disorder (versus no mental disorder) are at significantly elevated risk of drop out from mental health professionals other than psychiatrists. This association is significant for patients with ≥3 but not fewer visits. Impulse control disorder predicts dropout only from human service professionals. An analysis of serious compared with non-serious cases (22) revealed no significant associations with dropout overall or to any of the individual sectors. (Results available upon request.) Given the large number of associations examined, this small number of individually significant associations could occur by chance.
Psychiatric comorbidity
Patients who met criteria for ≥2 classes of psychiatric disorders were at significantly elevated risk of dropout from general medical treatment overall (OR: 1.5, 95% CI: 1.0–2.3) and before the third visit (OR: 1.7, 95% CI:1.1–2.7) (Table 2). Psychiatric comorbidity was associated with reduced dropout, however, from psychiatric treatment after ≥3 visits (OR:.5, 95% CI:.0–.8) (Table 4).
Number of sectors in which treatment is obtained
A total of 26.6% of patients received care in ≥1 sector (Data Not Shown). Among patients with ≥3 visits, receiving care from three or four sectors was associated with elevated odds of dropout from general medical sector (OR: 6.5, 95% CI:1.2–36.8) (Table 4).
Complementary Alternative Medicine
Use of complementary-alternative medicine was associated with significantly reduced odds of treatment dropout from general medical sector and mental health professionals other than psychiatrists. These associations are limited to dropout after ≥3 visits, though the association for other mental health professionals in this subanalysis did not reach statistical significance. Complementary-alternative medicine is also associated with reduced odds of dropout from general medical treatment after ≥3 visits.
DISCUSSION
The overall services dropout rate (21%) resembles earlier national estimates for the United States (19%) (14) and Canada (17% – 22%) (1). While in Canada, there was a lower dropout in care from primary care physicians than psychiatrists or psychologists (1), in this US study, we found the highest dropout for the general medical sector. As compared with Americans, Canadians may have closer and more established relationships with their primary care providers.
In the United States, the brevity of general medical visits (23) offers little opportunity to develop patient rapport, trust, and participation (24) and may contribute to risk of dropout. Although general medical care has been traditionally delivered by individual practitioners (25), newer models involve collaborations between general medical and mental health professionals (26, 27). Lower rates of dropout among patients receiving care from multiple sectors support the potential of this approach.
We found that the first two visits are a period of high risk for dropout, especially in the general medical and non-psychiatrist mental health sectors. The initial two visits are likely key for patient engagement, diagnostic evaluation, and initiation counseling. A high risk of early dropout highlights the importance of understanding consequences of dropout and of effective engagement in care (5).
The behavioral model of health care access (28) offers one framework for organizing findings about client predictors of dropout. Under this framework, dropout risk can be viewed as a joint function of 1) predisposing demographic (e.g., gender, age) and social (e.g., ethnicity, marital status, education) factors, 2) enabling (e.g., health insurance, income, number of providers) factors, and 3) need (e.g., psychiatric disorder, comorbidity, past treatment). We review these factors, considering stage and sector of treatment.
In keeping with NCS data (14) and clinical research (11) patient gender was not significantly related to overall risk of treatment dropout. However, women were significantly more likely than men to drop out early from human services sector. The reasons for this are unclear, although it might relate to lower levels of illness severity in women than men treated in this sector that persisted despite adjustment for number and type of mental disorder. Patient age also did not significantly predispose to overall dropout, though young age did increase risk of early dropout from psychiatric care (14).
Aspects of social structure including marital status, education, and ethnicity had complex relationships with dropout risk. As compared with separated, divorced, or widowed patients, married patients were significantly more likely to dropout from specialty mental health care later in treatment. This is in accord with evidence that spouses of individual psychotherapy patients sometimes respond negatively to their partner’s treatment (29–31). Alternatively, patients without partners may tend to become more dependent on their psychotherapists and more likely to comply with treatment recommendations (32).
Although patient education was not related to overall treatment dropout, ≥16 years of education was associated with a lower risk of dropout from mental health professionals other than psychiatrists. Acceptance (33), utilization (34), and completion (35, 36) of psychotherapy have been directly linked to level of patient education. Patients who have more education may also be more responsive to certain forms of psychotherapy (37, 38).
Patient ethnicity had no overall effect on the odds of dropout. African Americans, however, were significantly more likely than whites to dropout of psychiatric care. Racial differences in quality of mental health care (39, 40) may contribute to racial differences dropout.
Health insurance, higher income, and care coordination may enable service use and reduce dropout. The effect of insurance was evident after the first two visits, when greater out-of-pocket costs would be incurred. The recent increase in uninsured Americans (41) may increase risk for dropping out of specialty mental health treatment. Similarly, high income patients were less likely than low average income patients to drop out (42), especially from psychiatric services later in the course of care. Receiving mental health care from a larger number of provider sectors also reduced the probability of treatment dropout, but this could reflect a selection effect, such as more adherent or more assertive patients being more apt to visit multiple sectors.
Use of complementary-alternative medicine strongly reduced odds of dropout from traditional mental health care services. These protective effects were greatest early in treatment. Self-help group attendance enhances adherence (42) with conventional mental health services. Participation in self-help groups and other forms of complementary alternative medicine also increase appreciation or satisfaction with mental health services (44) which in turn may enhance retention in treatment (45) and tend to be used as supplements rather than alternatives to traditional care (46). Our results raise the possibility that greater coordination of professional services with self-help and other complementary-alternative medicine services might help reduce dropout from professional care, a hypothesis requiring experimental evaluation.
Need as measured by individual mental disorders, comorbid disorders, and past treatment demonstrated complex relationships with risk of dropout. In the aggregate, substance use disorders were related to dropout after the first two visits, a finding consistent with reports of high dropout rates from specific substance use treatment programs (47–49) and low perceived need for such treatment (50). This is a particularly concerning finding, given that longer-term treatments tend to be more successful than brief treatments for substance abuse (51).
Overall, mood and anxiety disorders appeared to exert little influence on the propensity to dropout, although dropout were from general medical sector was significantly lower among respondents with than without mood disorders. In evaluating dropout risk, consideration should be given to factors beyond measured clinical symptoms. Concepts such as predisposition to use services and enabling resources that have been primarily studied as predictors of service use (28) may also guide assessment of treatment dropout risk.
Early in treatment, patients with comorbid psychiatric disorders were more likely than patients with one disorder to leave treatment delivered in general medical sector while later in treatment the reverse was true. General medical professionals likely have less experience managing patients with psychiatric comorbidities (12, 52). Mismatches of clinical complexity and provider skill and resources may contribute to risk of treatment dropout.
Previous mental health treatment was linked to lower risk of dropout from psychiatric care. This was observed early in psychiatric treatment and overall after ≥2 visits and is consistent with evidence that prior mental health service use tends to predict future use (53). Stigma or embarrassment, which can contribute to treatment refusal or dropout (54), may be more pronounced among new patients.
CONCLUSIONS
The current study has several limitations. First, because psychiatric disorder, service use, and treatment dropout were retrospectively assessed by self-report, the results are subject to recall bias. Distressed community respondents may tend to overstate the number of visits they received (55). Second, the duration of recommended treatment may vary between provider groups and among providers within these groups and patient perceptions of provider intentions provide another level uncertainty. Third, treatment episodes were measured by number of visits. Provider groups may vary in period of time between scheduled visits (56) and treatment duration may be more important than visit number (57). Fourth, many potentially relevant patient (e.g., stigma, functional impairment, and satisfaction with treatment), professional (e.g., communication skills and clinical expertise), and service (e.g., co-payment and environmental obstacles) characteristics were not examined. Fifth, selection of high users into more treatment sectors may explain their lower rate of dropout. Sixth, because a large number of comparisons are examined, some significant associations may have occurred by chance. Seventh, the survey captured only visits from the most recent 12 months of long treatment episodes. However, because only 21% of all treatment episodes included more than 12 visits, it is unlikely that this truncation substantially influences reported treatment dropout patterns. Finally, we are unable to account for aspects of care for the same episode occurring in the period before or after the 12-month reporting interval.
It may be fruitful to study dropout in national surveys, an aspect of quality of care usually reserved for studies of clinical populations. The findings highlight the importance of research to understand the clinical significance of dropout, especially for populations at high risk. Achieving this work will require a broadening of the concepts of treatment and dropout, to consider the value of services provided or discontinued across multiple, often uncoordinated sectors.
Several clinical strategies may reduce dropout (5) including appointment reminders (58), treatment contracts (59), case management (60), and patient education and activation (61). As one example, primary care physician communications about medication treatment plans and education about side-effects may reduce early treatment termination (62). Our findings help clarify which patients, at which stage of treatment and in what sector, may most benefit from such strategies to optimize treatment goals.
Acknowledgements
The National Comorbidity Survey Replication (NCS-R) is supported by NIMH (U01-MH60220) with supplemental support from the National Institute on Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; Grant 044780), and the John W. Alden Trust. Collaborating NCS-R investigators include Ronald C. Kessler (Principal Investigator, Harvard Medical School), Kathleen Merikangas (Co-Principal Investigator, NIMH), James Anthony (Michigan State University), William Eaton (The Johns Hopkins University), Meyer Glantz (NIDA), Doreen Koretz (Harvard University), Jane McLeod (Indiana University), Mark Olfson (New York State Psychiatric Institute, College of Physicians and Surgeons of Columbia University), Harold Pincus (University of Pittsburgh), Greg Simon (Group Health Cooperative), Michael Von Korff (Group Health Cooperative), Philip S. Wang (NIMH), Kenneth Wells (UCLA), Elaine Wethington (Cornell University), and Hans-Ulrich Wittchen (Max Planck Institute of Psychiatry; Technical University of Dresden). The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or U.S. Government. A complete list of NCS publications and the full text of all NCS-R instruments can be found at http://www.hcp.med.harvard.edu/ncs. Send correspondence to ncs@hcp.med.harvard.edu.
The NCS-R is carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the staff of the WMH Data Collection and Data Analysis Coordination Centres for assistance with instrumentation, fieldwork, and consultation on data analysis. These activities were supported by the National Institute of Mental Health (R01 MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, and Bristol-Myers Squibb. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/.
Footnotes
Disclosure: Dr. Kessler has been a consultant for GlaxoSmithKline Inc., Kaiser Permanente, Pfizer Inc., Sanofi-Aventis, Shire Pharmaceuticals, and Wyeth-Ayerst; has served on advisory boards for Eli Lilly & Company and Wyeth-Ayerst; and has had research support for his epidemiological studies from Bristol-Myers Squibb, Eli Lilly & Company, GlaxoSmithKline, Johnson & Johnson Pharmaceuticals, Ortho-McNeil Pharmaceuticals Inc., Pfizer Inc., and Sanofi-Aventis. Dr. YY has received research support Bristol Myers-Squibb, Eli Lilly & Company, and AstraZeneca, served as a consultant to Ortho-McNeil Janssen Scientific Affairs, Pfizer, Lilly, AstraZeneca, and Bristol-Myers Squibb, and as a speaker for Janssen. The remaining authors have no interests to disclose.
REFERENCES
- 1.Wang J. Mental health treatment dropout and its correlates in a general population sample. Medical Care. 2007;45:224–229. doi: 10.1097/01.mlr.0000244506.86885.a5. [DOI] [PubMed] [Google Scholar]
- 2.Wang PS, Gilman SE, Guardino M, et al. Initiation of and adherence to treatment for mental disorders: examination of patient advocate group members in 11 countries. Medical Care. 2000;38:926–936. doi: 10.1097/00005650-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Goldenberg V. Ranking the correlates of psychotherapy duration. Administration and Policy in Mental Health. 2002;29:201–214. doi: 10.1023/a:1015187324925. [DOI] [PubMed] [Google Scholar]
- 4.Hatchett GT, Han K, Cooker PG. Predicting premature termination from counseling using the Butcher Treatment Planning Inventory. Assessment. 2002;9:156–163. doi: 10.1177/10791102009002006. [DOI] [PubMed] [Google Scholar]
- 5.Ogrodniczuk JS, Joyce AS, Piper WE. Strategies for reducing patient-initiated premature termination of psychotherapy. Harvard Review of Psychiatry. 2005;13:57–70. doi: 10.1080/10673220590956429. [DOI] [PubMed] [Google Scholar]
- 6.Killaspy H, Banerjee S, King M, et al. Prospective controlled study of psychiatric out-patient non-attendance. Characteristics and outcome. British Journal of Psychiatry. 2000;176:160–165. doi: 10.1192/bjp.176.2.160. [DOI] [PubMed] [Google Scholar]
- 7.Melartin TK, Rytsala HJ, Leskela US, et al. Continuity is the main challenge in treating major depressive disorder in psychiatric care. Journal of Clinical Psychiatry. 2005;66:220–227. doi: 10.4088/jcp.v66n0210. [DOI] [PubMed] [Google Scholar]
- 8.Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. New England Journal of Medicine. 2005;353:1209–1223. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]
- 9.McEvoy JP, Lieberman JA, Perkins DO, et al. Efficacy and tolerability of olanzapine, quetiapine, and risperidone in the treatment of early psychosis: a randomized, double-blind 52-week comparison. American Journal of Psychiatry. 2007;164:1050–1060. doi: 10.1176/ajp.2007.164.7.1050. [DOI] [PubMed] [Google Scholar]
- 10.Hunt C, Andrews G. Drop-out rate as a performance indicator in psychotherapy. Acta Psychiatrica Scandinavica. 1992;85:275–278. doi: 10.1111/j.1600-0447.1992.tb01469.x. [DOI] [PubMed] [Google Scholar]
- 11.Green CA, Polen MR, Dickinson DM, et al. Gender differences in predictors of initiation, retention, and completion in an HMO-based substance abuse treatment program. Journal of Substance Abuse Treatment. 2002;23:285–295. doi: 10.1016/s0740-5472(02)00278-7. [DOI] [PubMed] [Google Scholar]
- 12.Uebelacker LA, Wang PS, Berglund PA, et al. Clinical differences among patients treated for mental health problems in general medical and specialty mental health settings in the National Comorbidity Survey Replication. General Hospital Psychiatry. 2006;28:387–395. doi: 10.1016/j.genhosppsych.2006.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sturm R, Meredith LS, Wells KB. Provider choice and continuity for the treatment of depression. Medical Care. 1996;34:723–734. doi: 10.1097/00005650-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Edlund MJ, Wang PS, Berglund PA, et al. Dropping out of mental health treatment: patterns and predictors among epidemiological survey respondents in the United States and Ontario. American Journal of Psychiatry. 2002;159:845–851. doi: 10.1176/appi.ajp.159.5.845. [DOI] [PubMed] [Google Scholar]
- 15.de Mello MF, Myczcowisk LM, Menezes PR. A randomized controlled trial comparing moclobemide and moclobemide plus interpersonal psychotherapy in the treatment of dysthymic disorder. Journal of Psychotherapy Practice and Research. 2001;10:117–123. [PMC free article] [PubMed] [Google Scholar]
- 16.Kessler RC, Berglund P, Chiu WT, et al. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. International Journal of Methods in Psychiatric Research. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Geneva, Switzerland: World Health Organization; International Classification of Diseases (ICD-10) 1991
- 19.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 20.First MB, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-IV (SCID-I) New York, NY: 1995. [Google Scholar]
- 21.Research Triangle Institute. SUDAAN, Version 8.0.1. Research Triangle Park, NC: Research Triangle Institute; 2002. [Google Scholar]
- 22.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hing E, Cherry DK, Woodwell BA. National ambulatory care survey: 2004 summary. Advance Data. 2006;372:1–34. [PubMed] [Google Scholar]
- 24.Gross DA, Zyzanski SJ, Borawski EA, Cebul RD, Stange KC. Patient satisfaction with time spent with their physician. Journal of Family Practice. 1998;47:133–137. [PubMed] [Google Scholar]
- 25.Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–1221. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bartels SJ, Coakley EH, Zubritsky C, et al. Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. American Journal of Psychiatry. 2004;161:1455–1462. doi: 10.1176/appi.ajp.161.8.1455. [DOI] [PubMed] [Google Scholar]
- 27.Katon W, Unutzer J. Collaborative care models for depression: time to move from evidence to practice. Archives of Internal Medicine. 2006;166:2304–2306. doi: 10.1001/archinte.166.21.2304. [DOI] [PubMed] [Google Scholar]
- 28.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of Health & Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- 29.Roberts J. Perceptions of the significant other of the effects of psychodynamic psychotherapy. Implications for thinking about psychodynamic and systemic approaches. British Journal of Psychiatry. 1996;168:87–93. doi: 10.1192/bjp.168.1.87. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz RS. Psychotherapy and social support: unsettling questions. Harvard Review of Psychiatry. 2005;13:272–279. doi: 10.1080/10673220500326458. [DOI] [PubMed] [Google Scholar]
- 31.Sandell R, Blomberg J, Lazar A, et al. Varieties of long-term outcome among patients in psychoanalysis and long-term psychotherapy. A review of findings in the Stockholm Outcome of Psychoanalysis and Psychotherapy Project (STOPP) International Journal of Psychoanalysis. 2000;81:921–942. doi: 10.1516/0020757001600291. [DOI] [PubMed] [Google Scholar]
- 32.Bornstein RF. Dependency and patienthood. Journal of Clinical Psychology. 1993;49:397–406. doi: 10.1002/1097-4679(199305)49:3<397::aid-jclp2270490314>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 33.Furnham A, Wardley Z. Lay theories of psychotherapy. I: Attitudes toward, and beliefs about, psychotherapy and therapists. Journal of Clinical Psychology. 1990;46:878–890. doi: 10.1002/1097-4679(199011)46:6<878::aid-jclp2270460630>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 34.Wei W, Sambamoorthi U, Olfson M, et al. Use of psychotherapy for depression in older adults. American Journal of Psychiatry. 2005;162:711–717. doi: 10.1176/appi.ajp.162.4.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Howard KI, Cornille TA, Lyons JS, et al. Patterns of mental health service utilization. Archives of General Psychiatry. 1996;53:696–703. doi: 10.1001/archpsyc.1996.01830080048009. [DOI] [PubMed] [Google Scholar]
- 36.Nakao M, Fricchione G, Myers P, et al. Depression and education as predicting factors for completion of a behavioral medicine intervention in a mind/body medicine clinic. Behavioral Medicine. 2001;26:177–184. doi: 10.1080/08964280109595765. [DOI] [PubMed] [Google Scholar]
- 37.Schaefer BA, Koeter MW, Wouters L, et al. What patient characteristics make clinicians recommend brief treatment? Acta Psychiatrica Scandinavica. 2003;107:188–196. doi: 10.1034/j.1600-0447.2003.01453.x. [DOI] [PubMed] [Google Scholar]
- 38.Valbak K. Suitability for psychoanalytic psychotherapy: a review. Acta Psychiatrica Scandinavica. 2004;109:164–178. doi: 10.1046/j.1600-0447.2003.00248.x. [DOI] [PubMed] [Google Scholar]
- 39.Wells K, Klap R, Koike A, Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. American Journal of Psychiatry. 2001;158:2027–2032. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- 40.Wang PS, Berglund P, Kessler RC. Recent care of common mental disorders in the United States. Journal of General Internal Medicine. 2000;15:284–292. doi: 10.1046/j.1525-1497.2000.9908044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Garson A., Jr The uninsured: problems, solutions, and the role of academic medicine. Academic Medicine. 2006;81:798–801. doi: 10.1097/00001888-200609000-00006. [DOI] [PubMed] [Google Scholar]
- 42.Weinick RM, Byron SC, Bierman AS. Who can't pay for health care? Journal of General Internal Medicine. 2005;20:504–509. doi: 10.1111/j.1525-1497.2005.0087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Magura S, Laudet AB, Mahmood D, et al. Adherence to medication regimens and participation in dual-focus self-help groups. Psychiatric Services. 2002;53:310–316. doi: 10.1176/appi.ps.53.3.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hodges JQ, Markward M, Keele C, et al. Use of self-help services and consumer satisfaction with professional mental health services. Psychiatric Services. 2003;54:1161–1163. doi: 10.1176/appi.ps.54.8.1161. [DOI] [PubMed] [Google Scholar]
- 45.Rossi A, Amaddeo F, Sandri M, et al. What happens to patients seen only once by psychiatric services? Psychiatry Research. 2008;157:53–65. doi: 10.1016/j.psychres.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 46.Druss BG, Rosenheck RA. Association between use of unconventional therapies and conventional medical services. JAMA. 1999;282:651–651. doi: 10.1001/jama.282.7.651. [DOI] [PubMed] [Google Scholar]
- 47.Deren S, Goldstein MF, Des Jarlais DC, et al. Drug use, HIV-related risk behaviors and dropout status of new admissions and re-admissions to methadone treatment. Journal of Substance Abuse Treatment. 2001;20:185–189. doi: 10.1016/s0740-5472(00)00153-7. [DOI] [PubMed] [Google Scholar]
- 48.Gossop M, Marsden J, Stewart D, et al. Methadone treatment practices and outcome for opiate addicts treated in drug clinics and in general practice: results from the National Treatment Outcome Research Study. British Journal of General Practice. 1999;49:31–34. [PMC free article] [PubMed] [Google Scholar]
- 49.McFarland BH, Deck DD, McCamant LE, et al. Outcomes for medicaid clients with substance abuse problems before and after managed care. Journal of Behavioral Health Services Research. 2005;32:351–367. doi: 10.1007/BF02384196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fiorentine R, Anglin MD. Perceiving need for drug treatment: a look at eight hypotheses. International Journal of Addiction. 1994;29:1835–1854. doi: 10.3109/10826089409128260. [DOI] [PubMed] [Google Scholar]
- 51.Moos RH. Addictive disorders in context: principles and puzzles of effective treatment and recovery. Psychology of Addictive Behaviors. 2003;17:3–12. doi: 10.1037/0893-164x.17.1.3. [DOI] [PubMed] [Google Scholar]
- 52.Kessler RC, Zhao S, Katz SJ, et al. Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. American Journal of Psychiatry. 1999;156:115–123. doi: 10.1176/ajp.156.1.115. [DOI] [PubMed] [Google Scholar]
- 53.Yokopenic PA, Clark VA, Aneshensel CS. Depression, problem recognition, and professional consultation. Journal of Nervous and Mental Disease. 1983;171:15–23. doi: 10.1097/00005053-198301000-00004. [DOI] [PubMed] [Google Scholar]
- 54.Ben-Noun L. Characterization of patients refusing professional psychiatric treatment in a primary care clinic. Israeli Journal of Psychiatry & Related Sciences. 1996;33:167–174. [PubMed] [Google Scholar]
- 55.Rhodes AE, Fung K. Self-reported use of mental health services versus administrative records: care to recall? International Journal of Methods in Psychiatric Research. 2004;13:165–175. doi: 10.1002/mpr.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fortney J, Rost K, Zhang M, et al. The impact of geographic accessibility on the intensity and quality of depression treatment. Medical Care. 1999;37:884–893. doi: 10.1097/00005650-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 57.Ritsher JB, Moos RH, Finney JW. Relationship of treatment orientation and continuing care to remission among substance abuse patients. Psychiatric Services. 2002;53:595–601. doi: 10.1176/appi.ps.53.5.595. [DOI] [PubMed] [Google Scholar]
- 58.Kitcheman J, Adams CE, Pervaiz A, Kader I, Mohandas D, Brookes G. Does an encouraging letter encourage attendance at psychiatric out-patient clinics? The Leeds PROMPTS randomized study. Psychological Medicine. 2008;38:717–723. doi: 10.1017/S0033291707001766. [DOI] [PubMed] [Google Scholar]
- 59.Sledge WH, Moras K, Hartley D, et al. Effect of time-limited psychotherapy on patient dropout rates. American Journal of Psychiatry. 1990;147:1341–1347. doi: 10.1176/ajp.147.10.1341. [DOI] [PubMed] [Google Scholar]
- 60.Miranda J, Azocar F, Organista KC, et al. Treatment of depression among impoverished primary care patients from ethnic minority groups. Psychiatric Services. 2003;54:219–225. doi: 10.1176/appi.ps.54.2.219. [DOI] [PubMed] [Google Scholar]
- 61.Brown JM, Miller WR. Impact of motivational interviewing on participation and outcome in residential alcoholism treatment. Psychology of Addictive Behavior. 1993;7:211–218. [Google Scholar]
- 62.Bull SA, Hu XH, Lee JY, Ming EE, Markson LE, Fireman B. Discontinuation of use and switching of antidepressants: influence of patient-physician communication. JAMA. 2002;288:1403–1409. doi: 10.1001/jama.288.11.1403. [DOI] [PubMed] [Google Scholar]