Abstract
We examine the association between education and smoking by women in the population, including smoking during pregnancy, and identify risk factors for smoking and the consequences of smoking in pregnancy for children's smoking and behavioral problems. Secondary analyses of four national data sets were implemented: The National Survey of Drug Use and Health (2006), the National Longitudinal Survey of Youth (1979–2004); the National Longitudinal Survey of Adolescent Health (Wave III); The National Health and Nutrition Examination Survey (2005-2006). The lower the level of education, the greater the risk of being a current smoker, smoking daily, smoking heavily, being nicotine dependent, starting to smoke at an early age, having higher levels of circulating cotinine per cigarettes smoked, and continuing to smoke in pregnancy. The educational gradient is especially strong in pregnancy. Educational level and smoking in pregnancy independently increase the risk of offspring smoking and antisocial and anxious/depressed behavior problems. These effects persist with control for other covariates, except maternal age at child's birth, which accounts for the impact of education on offspring smoking and anxious/depressed behavior problems. Women with low education should be the target of public health efforts toward reducing tobacco use. These efforts need to focus as much on social conditions that affect women's lives as on individual level interventions. These interventions would have beneficial effects not only for the women themselves but also for their offspring.
Keywords: Education, Smoking by women, Smoking in pregnancy, Offspring smoking, Offspring behavior problems
1. Introduction
The association between socioeconomic disadvantage, smoking, and morbidity and mortality in the population has been well established in the U.S. (U.S. Department of Health and human Services, 2001; 2007; Greaves et al., 2006; House, 2002; McCaffery et al., 2007; Mirowsky et al., 2000; Robert and House, 2000; Schaap et al., 2008; Schnittker and McLeod, 2005) as well as in other Western countries (Giskes et al., 2005; Graham et al., 2008). While socioeconomic indicators other than education contribute to disparities in rates of smoking (Schaap et al., 2008), education, which is highly related to overall status (Laaksonen et al., 2005), is the most frequently used indicator of socioeconomic status (SES) in studies of smoking (Schaap et al., 2008). The disparity in smoking rates related to educational level persists even in societies with a strong welfare system (Eikemo et al., 2007; Olafsdottir, 2007).
The negative association between educational level and smoking among women is also observed in pregnancy (Matthews, 2001). Smoking during pregnancy has special public health relevance because of the impact of prenatal smoking on offspring. Children whose mothers have smoked during pregnancy are more likely to smoke in adolescence (Al Mamun et al., 2006; Cornelius et al., 2000; Kandel et al., 1994; unpublished data; O'Callagan et al., 2006) and to become dependent on nicotine (Buka et al., 2003). Furthermore, epidemiological, clinical and animal studies have also established that offspring of mothers who smoke during pregnancy are more likely to manifest behavior problems, both externalizing and internalizing (D'Onofrio et al., 2008; Griesler et al., 1998; Milberger et al., 1996; Orlebeke et al., 1997; Richardson and Tizabi, 1994; Shea and Steiner, 2008; Vaglenova et al., 2004; Wakschlag et al., 2002; 2006; Weissman et al., 1999; Winzer-Serhan, 2008). Behavioral disturbances, e.g., hyperactivity and conduct disorder, are risk factors for delinquency and substance use (Moffitt, 1993), in particular smoking (Brown et al., 1996; Kollins et al., 2005; Lynskey and Ferguson, 1995), and nicotine dependence (Breslau et al., 1993; Storr et al., 2004). Effects on child smoking may be direct due to an induced biological vulnerability to the addictive properties of nicotine and indirect through nicotine induced behavioral problems in childhood. It is not clear to what extent the impact of prenatal smoking varies according to SES.
Why is there such a strong negative relationship between educational attainment and smoking? How is educational level associated with differential exposure to risk factors that contribute to smoking? Education is related to most aspects of a person's lifestyle, social performance and psychosocial adjustment, including participation in the labor force, family roles, parenting, and psychological well being. The higher the education, the higher the labor force participation and marriage rates, and the lower the levels of psychological distress and depression (Lorant et al., 2003; Thornton et al., 1995; U.S. Census Bureau, 2007). Thus, at any particular historical point in time, the association between SES and a health-related behavior, such as smoking, could be accounted for by differential attitudes about heath related behaviors, differential psychosocial characteristics, and differential participation in the social roles of adulthood.
In this article, we address four issues:
What is the association between education and patterns of smoking among women?
Do these patterns persist with control for covariates?
What is the association between education and patterns of smoking in pregnancy?
Does education account for the impact of prenatal smoking on offspring smoking and psychosocial adjustment?
We provide a broad overview of these issues and new empirical findings rather than an in-depth exploration of each question. We explore these issues in multiple data sets that each provides unique information to illuminate a particular question. We use data from three surveys to explore the first two issues: the National Survey on Drug Use and Health (NSDUH 2006) (Substance Abuse and Mental Health Services Administration, 2007a), the National Longitudinal Survey of Adolescent Health (ADD HEALTH III) (Harris et al., 2003; Kandel et al., 2007a), and the National Health and Nutrition Examination Survey (2005-2006) NHANES (National Center for Health Statistics, cdc.gov/nchs/nhanes.htm accessed on 3/4/2008). We use data from The National Longitudinal Survey of Youth (NLSY) (l979-2004) (Center for Human Resource Research, 2006) to explore the last two issues.
We explicitly do not deal with questions related to race/ethnicity, although these are relevant to socioeconomic disadvantage, because race/ethnicity is the specific focus of the article by J. M. Wallace (in press). However, we control for race/ethnicity in our statistical models.
2. Methods
2.1. Data Sources
Greater detail about each of the four national surveys and the measurement of variables of interest is provided in the references cited for each study, although we briefly describe the design and selected variables for each study.
2.1.1. NSDUH 2006
The NSDUH 2006 is a national multistage area probability sample of the US population 12 years old and over. The target civilian non-institutionalized population represents over 98% of the total population, including persons living in non-institutionalized group quarters, such as homeless shelters, rooming houses and college dormitories. Individuals on active military duty, in jail or drug treatment programs, and the homeless not in shelters were excluded. Youths (12-25 years old) were over-sampled. The completion rate was 67.2%. Weights take into account the stratified multistage cluster sampling design and correct for over-sampling and non-response rates so that the resulting weighted sample is representative of the U.S. population.
Respondents were administered computer assisted structured personal household interviews and asked about the use of tobacco and 11 other drug classes, selected attitudes about drugs, major depressive disorder episode experienced in the last year, and sociodemographic characteristics (Substance Abuse and Mental Health Services Administration, 2007b). Nicotine dependence was assessed by the Nicotine Dependence Syndrome Scale (NDSS) (Shiffman et al., 2004). Although developed as continuous scale, a cut-off point was identified to define dependence as a categorical variable.
The analyses are based on females 18 years old and over (N=19,574).
2.1.2. ADD HEALTH Wave III
Data were derived from Wave III of ADD HEALTH, a subset of participants in a school survey conducted in 1994-1995 with a national representative sample of 90,118 adolescents in grades 7-12. In 1994-95 (Wave I), interviews were completed with 20,745 adolescents and their parents (78.9% participation rate) at mean age, 15.5 years, SD=1.7. In 1996 (Wave II), 14,738 of 16,706 Wave I adolescents in target grades 7-11 were reinterviewed, including dropouts (88.2% completion). In 2001-2002, (Wave III), interviews were completed with 15,197 youths whose mean age was 21.8 years (SD=1.9) (77.4% participation rate). A urine sample was collected from respondents at a random time.
At Wave III, 2,982 youths reported smoking on 30 of the last 30 days and were assumed to have smoked on the survey day. An analytical subsample of 1,016 cases was selected, which included all the minorities [African Americans (N=307), Hispanics (N=274), and Asians (N=125)] and a random subsample of Whites to equal the number of African Americans (N=310); 904 respondents provided urine samples. Since cotinine has a half-life of 16-20 hours, the current smokers in the analytical sample were expected to have detectable cotinine levels. Cotinine level per cigarette smoked was calculated by dividing total values by the number of cigarettes currently smoked per day. The Clinical Pharmacology Laboratory at the University of California, San Francisco, assayed the samples for cotinine. For further details see Kandel et al. (2007a).
2.1.3. NHANES, 2005-2006
NHANES is a nationally representative sample of the civilian non-institutionalized population two months old and over. Conducted as a continuous annual survey since 1999, data are released in two-year increments. Interviews are conducted in households and blood sera are collected in mobile examination centers via venipuncture.
Data from 2005-2006 are used in this report (77.4% completion rate). The analysis is based on current smokers among women aged 20 and over (N=350). Cotinine level per cigarette smoked was calculated by dividing total cotinine values by the number of cigarettes currently smoked per day. Serum cotinine was measured by an isotope dilution-high performance liquid chromatography/atmospheric pressure chemical ionization tandem mass spectrometry (NHANES, 2008).
2.1.4. NLSY 1979-2004
The NLSY is a multistage stratified national probability sample, representative of youths 14-22 years old in 1979 born between 1957 and 1963 in the coterminous United States. As of 1979, subjects have been re-interviewed annually through 1994, biennially thereafter. Biennial assessments of children were implemented as of 1986 from mothers about all children. As of 1988, children aged 10 years and older also completed a self-administered questionnaire. The 1979 interview completion rate was 90%; retention rates have consistently been over 90%. Informed consent was obtained from mothers for their own participation and that of their children.
The analyses are based on mothers and their first born child (N=4,911) with data on maternal smoking during and after pregnancy (mothers' mean age at child's birth=23.9 years, SD=5.6; children's age range in 2004=1 to 34 years). Prenatal exposure to maternal tobacco use was first ascertained in 1983 for the youngest child, in 1986 for all births not asked about previously (62.6% of children), and as of 1988 biennially for all new births. As of 1988, children 10 and older reported biennially on their cigarette smoking. Two children's behavior problems, antisocial and anxious-depressed, were measured by the Behavior Problems Index (BPI) (Peterson and Zill, 1986), administered biennially to mothers since 1986. Mothers reported on the frequency of behavior problems experienced in the last 3 months among children aged 4 and older from 1986 to1992, and 4-14 as of 1994. For analytical purposes, two scores were defined for each behavior: maximum score over the multiple waves; score prior to the child's first smoking report. High scores for each behavior problem were dichotomized at the top quartile.
2.2. Analysis
Regular and multinomial logistic regressions were implemented to assess the unique effects of education and other covariates on the outcomes of interest. For NSDUH, the analyses were implemented with SUDAAN V9.0.1 in order to account for design effects. This was not possible for NLSY, since variables necessary to correct for design effects are not available on the public use data file, or for ADD HEALTH and NHANES, since selected subsamples were used.
3. Results
3.1. Education and smoking behavior
The association between education and patterns of smoking differs for lifetime and current (last 30 days) smoking. An inverse relationship appears with respect to current but not lifetime smoking. As documented by NSDUH 2006, women with less than a high school education are less likely to have ever smoked (54.7%) than high school graduates (65.9%), those with some college (70.3%), or college graduates (66.6%). The opposite pattern characterizes current smoking, for which college graduates have the lowest rates of smoking of any group; the rate of current smoking is twice as high among women who have not graduated from high school (29.3%), among high school graduates (28.5%), and among those with some college (25.2%) than among college graduates (13.0%). Indeed, persistence of smoking decreases strikingly and linearly with level of education: more than half (53.7%) of women with the lowest education continue to smoke compared with less than a fifth (19.5%) of college graduates; the rates of persistence are 43.3% among high school graduates and 35.8% among women with some college (Table 1).
Table 1.
Smoking history by education among women smokers aged 18 and over (NSDUH 2006, N=13,043)
| Smoking History | Less than H.S. | H.S. Graduate | Some College | College Graduate |
|---|---|---|---|---|
| Among lifetime smokers | ||||
| Smoked last month (%) | 53.7 | 43.3 | 35.8 | 19.5 |
| Ever smoked daily (%) | 73.8 | 66.3 | 55.5 | 41.0 |
| Age of onset (years) (M (S.D.)) | 14.9 (3.8) | 15.6 (4.0) | 15.7 (3.6) | 16.2 (4.1) |
| Total N | (1,913) | (4,212) | (4,077) | (2,742) |
| Among last month smokers | ||||
| Cigarettes per day (M (S.D.)) | 14.1 (12.2) | 12.0 (9.7) | 11.6 (5.8) | 8.6 (8.4) |
| Nicotine dependent (%) | 51.3 | 42.3 | 43.3 | 24.1 |
| Total N | (1,200) | (2,227) | (1,813) | (708) |
Not only is education inversely related to persistent smoking, but women with lower education are more likely to exhibit behavioral patterns reflecting greater involvement in smoking (Table 1). Educational level is inversely related to having ever smoked daily, number of cigarettes smoked per day, and being dependent on nicotine. Women who have not graduated from high school smoke on average 14.1 cigarettes per day compared with 8.6 cigarettes for college graduates. Educational level is also related to older age at smoking onset. Women with less than a high school education started to smoke on average 15 months earlier than college graduates.
Furthermore, women with lower education have higher concentrations of cotinine per cigarette smoked than those with higher education. Cotinine levels were assessed from urine samples in ADD HEALTH and blood sera in NHANES. Cotinine levels assessed in urine can be 3-8 times higher than in serum (NHANES, 2008; Jarvis et al., 1984). In both samples, the mean cotinine levels are 37%-40% higher among women with less than a high school education than those with more education, although the difference is statistically significant only in ADD HEALTH (Table 2). In ADD HEALTH, the values for high school graduates are not statistically significantly different from the other two educational groups, while in NHANES, they are not different from women with more than a high school education.
Table 2.
Cotinine intake per cigarette smoked by education in two national samples (ADD HEALTH III, N=386; NHANES 2005-2006, N=349)
| Less than H.S. | H.S. Graduate | More than H.S. | ||||
|---|---|---|---|---|---|---|
| M | S.D. | M | S.D. | M | S.D. | |
| ADD HEALTH III (18-24 years) | ||||||
| Urine cotinine (ng/ml) | 162.4a | (174.4) | 138.0ab | (135.5) | 115.6b | (117.3) |
| Total N | (105) | (149) | (132) | |||
| NHANES 2005-2006 (20+ years) | ||||||
| Serum cotinine (ng/ml) | 32.3a | (61.0) | 19.1b | (16.6) | 23.6ab | (30.1) |
| Total N | (108) | (111) | (130) | |||
Cells with different letters are statistically significantly different from each other.
Thus, besides differences in smoking patterns associated with educational level, there are also differences with respect to levels of cotinine circulating in the body.
3.2. Do individual risk factors explain educational disparities in smoking among women?
We tested the hypothesis that individual characteristics might explain the disparities in smoking behaviors associated with educational level by controlling relevant variables available in the NSDUH. We categorized smoking behavior into four categories of increasing extensiveness of involvement: (1) never smoked; (2) former smoker, did not smoke in last month; (3) last month smoker, not nicotine dependent; (4) last month smoker, nicotine dependent. We implemented multinomial logistic regressions in which each smoking group was compared to each succeeding group. The covariates included sociodemographic variables (age, education, race/ethnicity, family income), family roles (marital status, number of own children in household), labor force participation, psychological characteristics (major depression episode last year, risk taking), religious commitment (religiosity, religious services attendance), and attitudes about harmfulness of drugs, smoking cigarettes, drinking heavily and using marijuana (Table 3).
Table 3.
Multinomial logistic regression predicting cigarette smoking and nicotine dependence among women aged 18 and over (NSDUH 2006, N≥18,973)
| Covariates | Former smoker (not last month) vs. Never | Last month smoker, not dependent vs. Former | Nicotine dependent vs. Last month smoker, not dependent |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| UOR | 95% CI | AOR | 95% CI | UOR | 95% CI | AOR | 95% CI | UOR | 95% CI | AOR | 95% CI | |
| Age (vs. 18-25 years) | ||||||||||||
| 26-34 | 1.41 *** | (1.23-1.61) | 1.31 *** | (1.12-1.54) | 0.57 *** | (0.50-0.66) | 0.86 | (0.71-1.05) | 1.32 * | (1.06-1.64) | 1.31 * | (1.03-1.67) |
| 35-49 | 1.73 *** | (1.52-1.96) | 1.57 *** | (1.33-1.87) | 0.43 *** | (0.38-0.48) | 0.72 *** | (0.61-0.86) | 1.74 *** | (1.46-2.09) | 1.80 *** | (1.44-2.24) |
| 50 and older | 1.66 *** | (1.47-1.88) | 1.96 *** | (1.67-2.31) | 0.22 *** | (0.19-0.26) | 0.42 *** | (0.34-0.52) | 1.44 ** | (1.12-1.84) | 1.31 | (0.94-1.84) |
| Education (vs. < H.S.) | ||||||||||||
| H.S. graduate | 1.70 *** | (1.43-2.01) | 1.42 *** | (1.17-1.71) | 0.79 ** | (0.66-0.95) | 0.81 * | (0.67-0.99) | 0.71 *** | (0.59-0.86) | 0.68 *** | (0.55-0.85) |
| Some college | 2.22 *** | (1.90-2.58) | 1.72 *** | (1.45-2.04) | 0.59 *** | (0.49-0.70) | 0.56 *** | (0.45-0.68) | 0.58 *** | (0.48-0.69) | 0.60 *** | (0.49-0.74) |
| College graduate | 2.65 *** | (2.24-3.14) | 1.60 *** | (1.29-1.98) | 0.34 *** | (0.28-0.41) | 0.40 *** | (0.32-0.51) | 0.25 *** | (0.19-0.33) | 0.24 *** | (0.18-0.33) |
| Race/ethnicity (vs. white) | ||||||||||||
| African American | 0.38 *** | (0.33-0.44) | 0.52 *** | (0.45-0.61) | 1.13 | (0.97-1.33) | 0.92 | (0.77-1.10) | 0.65 *** | (0.53-0.81) | 0.60 *** | (0.48-0.75) |
| Hispanic | 0.43 *** | (0.37-0.49) | 0.61 *** | (0.53-0.71) | 1.00 | (0.86-1.18) | 0.75 ** | (0.61-0.91) | 0.37 *** | (0.27-0.51) | 0.29 *** | (0.21-0.42) |
| Other | 0.29 *** | (0.23-0.36) | 0.35 *** | (0.28-0.44) | 1.34 | (0.95-1.90) | 1.21 | (0.82-1.81) | 0.58 ** | (0.39-0.87) | 0.60 * | (0.39-0.95) |
| Marital status (vs. married/widowed) | ||||||||||||
| Divorced/separated | 1.33 ** | (1.12-1.58) | 1.41 *** | (1.18-1.72) | 2.12 *** | (1.79-2.51) | 1.89 *** | (1.57-2.28) | 1.22 | (1.00-1.48) | 1.00 | (0.79-1.25) |
| Never married | 0.67 *** | (0.61-0.74) | 0.85 * | (0.74-0.98) | 2.99 *** | (2.66-3.35) | 1.55 *** | (1.32-1.83) | 0.66 *** | (0.57-0.76) | 0.79 * | (0.63-0.97) |
| Children in household (vs. none) | ||||||||||||
| 1 | 1.03 | (0.91-1.17) | 1.23 ** | (1.08-1.41) | 1.03 | (0.90-1.18) | 1.09 | (0.94-1.26) | 1.38 ** | (1.13-1.68) | 1.23 | (0.97-1.55) |
| 2 | 1.16 * | (1.02-1.31) | 1.37 *** | (1.17-1.80) | 0.80 ** | (0.69-0.92) | 1.02 | (0.86-1.21) | 1.42 *** | (1.16-1.73) | 1.16 | (0.91-1.47) |
| 3 or more | 1.17 | (0.96-1.43) | 1.52 *** | (1.19-1.94) | 0.70 *** | (0.57-0.86) | 0.88 | (0.66-1.16) | 1.80 *** | (1.42-2.28) | 1.39 * | (1.07-1.81) |
| Work status last week (vs. worked) | ||||||||||||
| Had job, did not work | 1.07 | (0.86-1.32) | 1.08 | (0.86-1.34) | 0.87 | (0.69-1.10) | 0.83 | (0.66-1.06) | 0.96 | (0.70-1.31) | 0.96 | (0.69-1.35) |
| Unemployed | 0.57 *** | (0.41-0.79) | 0.90 | (0.64-1.27) | 2.33 *** | (1.79-3.03) | 1.31 | (0.98-1.75) | 1.39 * | (1.04-1.85) | 1.24 | (0.95-1.63) |
| Kept house | 0.68 *** | (0.58-0.80) | 0.81 * | (0.88-0.97) | 0.88 | (0.73-1.06) | 0.98 | (0.80-1.20) | 1.59 *** | (1.27-2.00) | 1.25 | (0.96-1.63) |
| School/training | 0.55 *** | (0.45-0.66) | 0.74 ** | (0.80-0.90) | 1.63 *** | (1.26-2.13) | 0.96 | (0.72-1.28) | 0.42 *** | (0.27-0.65) | 0.48 ** | (0.30-0.78) |
| Disabled/retired/no job | 0.95 | (0.85-1.07) | 1.01 | (0.88-1.17) | 0.55 *** | (0.47-0.63) | 0.71 *** | (0.60-0.85) | 1.85 *** | (1.56-2.19) | 1.37 * | (1.08-1.75) |
| Family income | 1.00 *** | (1.00-1.00) | 1.00 | (1.00-1.00) | 1.00 *** | (1.00-1.00) | 1.00 ** | (1.00-1.00) | 1.00 *** | (1.00-1.00) | 1.00 *** | (1.00-1.00) |
| Major depressive episode last year | 1.46 *** | (1.24-1.72) | 1.29 ** | (1.06-1.56) | 1.56 *** | (1.31-1.87) | 1.24 * | (1.01-1.51) | 1.61 *** | (1.31-1.98) | 1.38 ** | (1.11-1.73) |
| Risk taking | 1.51 *** | (1.40-1.64) | 1.36 *** | (1.25-1.48) | 1.48 *** | (1.37-1.59) | 1.21 *** | (1.11-1.32) | 1.07 | (0.98-1.16) | 1.17 *** | (1.07-1.29) |
| Perceived risk of: Smoking 1+ pack cigarettes/day (vs. no/slight/moderate risk) | ||||||||||||
| Great | 1.12 | (0.99-1.27) | 1.31 *** | (1.13-1.52) | 0.35 *** | (0.31-0.40) | 0.42 *** | (0.36-0.48) | 0.80 *** | (0.70-0.91) | 0.96 | (0.83-1.12) |
| Having 5+ drinks 1-2 times/week (vs. no/slight risk) | ||||||||||||
| Moderate | 0.95 | (0.84-1.08) | 1.00 | (0.86-1.16) | 0.68 *** | (0.59-0.79) | 0.88 | (0.75-1.04) | 1.04 | (0.88-1.22) | 1.09 | (0.90-1.32) |
| Great | 0.62 *** | (0.55-0.69) | 0.83 ** | (0.73-0.96) | 0.59 *** | (0.52-0.68) | 0.97 | (0.83-1.14) | 0.97 | (0.82-1.15) | 1.02 | (0.83-1.27) |
| Smoking marijuana once/month (vs. no risk) | ||||||||||||
| Slight | 0.86 | (0.72-1.04) | 0.84 | (0.70-1.03) | 0.60 *** | (0.52-0.71) | 0.75 ** | (0.62-0.90) | 0.76 * | (0.62-0.94) | 0.80 * | (0.64-0.99) |
| Moderate | 0.59 *** | (0.49-0.71) | 0.61 *** | (0.50-0.75) | 0.43 *** | (0.37-0.50) | 0.63 *** | (0.52-0.76) | 0.80 * | (0.66-0.96) | 0.80 * | (0.65-0.98) |
| Great | 0.37 *** | (0.30-0.44) | 0.42 *** | (0.33-0.53) | 0.36 *** | (0.30-0.43) | 0.72 ** | (0.58-0.90) | 0.75 * | (0.60-0.93) | 0.72 * | (0.56-0.92) |
| Frequency attended religious services last year (vs. 0 times) | ||||||||||||
| 1-2 | 1.05 | (0.89-1.24) | 1.14 | (0.95-1.37) | 0.92 | (0.77-1.10) | 0.95 | (0.77-1.17) | 0.77 * | (0.62-0.94) | 0.88 | (0.70-1.12) |
| 3-5 | 1.17 * | (1.01-1.36) | 1.24 ** | (1.08-1.46) | 0.84 | (0.71-1.01) | 0.99 | (0.83-1.20) | 0.67 *** | (0.54-0.84) | 0.75 * | (0.60-0.95) |
| 6-24 | 1.11 | (0.98-1.26) | 1.14 | (0.98-1.32) | 0.72 *** | (0.61-0.85) | 0.94 | (0.78-1.15) | 0.71 ** | (0.57-0.88) | 0.77 * | (0.60-0.99) |
| 25-52 | 0.93 | (0.81-1.07) | 0.91 | (0.77-1.08) | 0.41 *** | (0.35-0.49) | 0.71 *** | (0.58-0.86) | 0.47 *** | (0.35-0.61) | 0.52 *** | (0.38-0.70) |
| 52 or more | 0.73 *** | (0.63-0.84) | 0.87 | (0.74-1.02) | 0.26 *** | (0.21-0.33) | 0.48 *** | (0.37-0.61) | 0.53 ** | (0.37-0.78) | 0.59 * | (0.39-0.89) |
| Importance of religion | 0.76 *** | (0.72-0.80) | 0.88 *** | (0.83-0.94) | 0.66 *** | (0.62-0.67) | 0.84 *** | (0.77-0.91) | 0.95 | (0.89-1.01) | 1.05 | (0.95-1.16) |
| Total N 's≥ | (13,196) | (10,452) | (5,777) | |||||||||
p<0.05;
p<0.01;
p<0.001
UOR= unadjusted odds ratio; AOR= adjusted odds ratio
With the exception of perceived risk of alcohol drinking, all the covariates were statistically significant and the majority, including education, remained highly statistically significant at each stage of progressive involvement in smoking with control for other covariates. The lower the level of education, the lesser the risk of quitting smoking and the greater the risk of smoking currently and being dependent on nicotine. The relationship is not linear. Compared with smokers with less than a high school education, the odds of being dependent are four times lower (.24) for college graduates, 1.5 lower (.68) for high school graduates, and 1.7 (.60) lower for those with some college. Attitudes are the least important factors.
3.3. Education and smoking in pregnancy
The association between educational level and smoking is exacerbated with respect to smoking in pregnancy. In the NLSY, the rates of smoking in pregnancy were 45.0% for those with less than high school, 34.1% for high school graduates, 17.4% for those with some college, and 5.1% for college graduates. The rate of smoking was nine times higher among those without a high school degree than among college graduates. In a sample of women 18-44 years old drawn from the NSDUH, the rate was 2.8 times higher. We compared the rates of smoking in the NSDUH among currently pregnant and non-pregnant women after standardizing the age distributions of the two groups. These ratios ranged from .85 among those without a high school degree to .68 among high school graduates, .45 among those with some college, and .20 among college graduates. While among college educated women the rate of smoking in pregnancy was one fifth of those not pregnant, the rate among those with less than a high school education was almost as high as among those not pregnant. Education is highly related to quitting smoking in pregnancy.
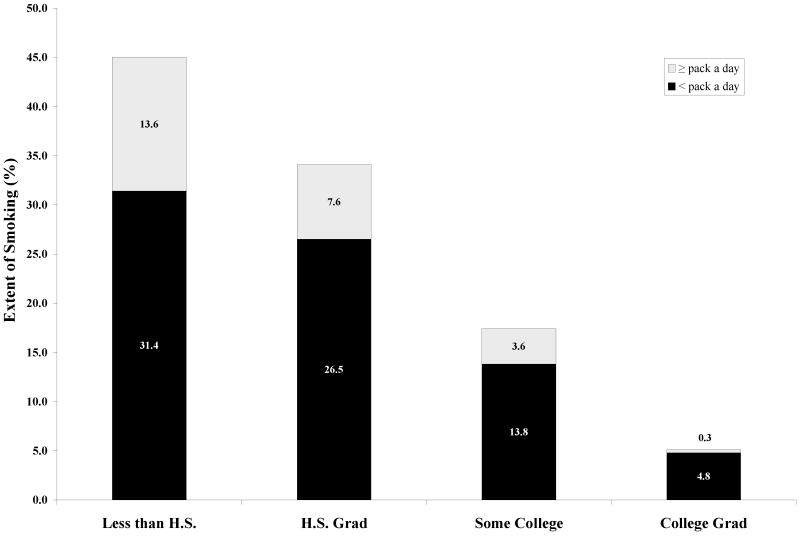
Not only is education inversely related to persistence of smoking, it is also highly related to extensiveness of smoking during pregnancy. When pregnant, 0.3% of college graduates in the NLSY smoked a pack or more of cigarettes a day on average compared with 13.6% of those who failed to graduate from high school (Figure 1).
Figure 1.
Extent of smoking in first pregnancy by maternal education at child's birth (NLSY 1979-2004, N=4,553
3.4. Maternal education, prenatal smoking, and child outcomes
Both mother's educational level at the time of the child's birth and smoking in pregnancy have independent deleterious effects on offspring. We examined three child outcomes in the NLSY: lifetime smoking and two behavior problems, antisocial and anxious/depressed. Maternal education was still defined as of the child's birth since it clearly preceded the children's outcomes and preserved parallelism with the analysis of smoking in pregnancy. Furthermore, education at child's birth is very highly related (r=0.86) to maternal highest educational attainment.
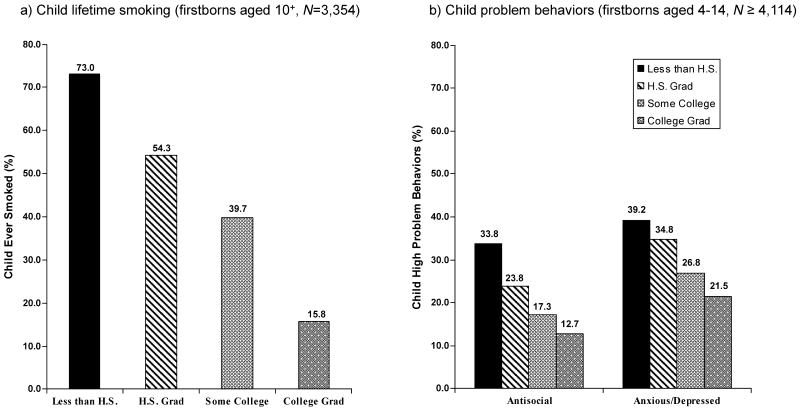
There is a very strong association between maternal education at the time of the child's birth and child outcomes. Almost five times as many children of mothers without a high school degree have smoked (73.0%) as among the children of college graduates (15.8%) (Figure 2-a). Similarly, the rates of antisocial behavior and anxiety/depression decline with increasing level of maternal education at the time of the child's birth (Figure 2-b).
Figure 2.
Maternal education at birth of firstborn child and child outcomes (NLSY 1979-2004)
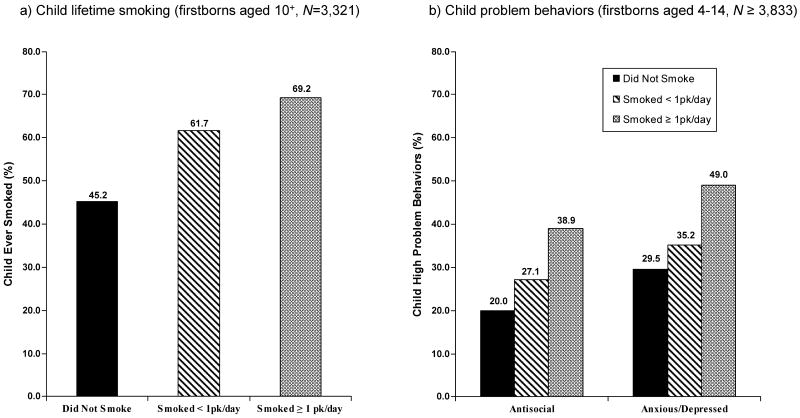
Parallel trends are observed in relation to maternal smoking in pregnancy. Fifty percent more children have smoked when their mothers smoked a pack or more of cigarettes a day compared with children whose mothers did not smoke (Figure 3-a). Behavior problems in offspring increase also with increasing levels of smoking in pregnancy (Figure 3-b).
Figure 3.
Maternal smoking in pregnancy and firstborn child outcomes (NLSY 1979-2004)
In order to specify the unique impact of maternal education on children's outcomes, over and beyond the impact of prenatal and postnatal smoking, we estimated logistic regressions to predict offspring's smoking (Table 4) and problem behaviors (Table 5). Maternal education was included in the models together with prenatal and postnatal smoking and other covariates. The predictors included sociodemographic variables, and measures of maternal depression and delinquency to control for maternal psychopathology. Child behavior problems (antisocial and anxious/depressed) prior to the onset of smoking were also included in the model for child smoking.
Table 4.
Maternal education at child's birth and prenatal smoking as predictors of child lifetime N=3,262)
| Covariates | Lifetime Smoking | |||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | |||||
| UOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Maternal education at child's birth (vs. less than high school) | ||||||
| High school | 0.44*** | 0.37-0.52 | 1.02 | 0.81-1.28 | 0.53*** | 0.43-0.65 |
| Some college | 0.24*** | 0.20-0.30 | 1.13 | 0.85-1.51 | 0.40*** | 0.31-0.51 |
| College or more | 0.07*** | 0.05-0.09 | 0.70 | 0.48-1.02 | 0.17*** | 0.12-0.24 |
| Maternal prenatal smoking (vs. no) | ||||||
| Smoked < pack/day | 1.95*** | 1.66-2.29 | 1.35** | 1.09-1.69 | 1.30* | 1.06-1.61 |
| Smoked ≥ pack/day | 2.72*** | 2.07-3.57 | 1.56** | 1.10-2.22 | 1.41* | 1.01-1.99 |
| Maternal postnatal smoking (vs. no) | ||||||
| Smoked < pack/day | 1.76*** | 1.49-2.07 | 0.95 | 0.77-1.19 | 0.93 | 0.76-1.15 |
| Smoked ≥ pack/day | 1.44** | 1.12-1.85 | 0.90 | 0.65-1.25 | 0.81 | 0.59-1.10 |
| Maternal age at first birth | 0.79*** | 0.07-0.80 | 0.78*** | 0.76-0.81 | - | - - |
| Income at first birth | 0.97*** | 0.96-0.97 | 0.99*** | 0.98-0.99 | 0.97*** | 0.97-0.98 |
| Marital status at first birth (vs. married) | ||||||
| Divorced, separated, widowed | 1.41 | 1.01-1.96 | 0.90 | 0.60-1.35 | 0.68* | 0.47-0.99 |
| Never married | 2.08*** | 1.75-2.45 | 0.86 | 0.68-1.08 | 1.10 | 0.89-1.37 |
| Number of children ever born | 1.14*** | 1.08-1.21 | 0.89** | 0.83-0.96 | 0.89** | 0.83-0.96 |
| Maternal depression | 1.05*** | 1.03-1.06 | 0.99 | 0.97-1.01 | 0.98 | 0.97-1.00 |
| Maternal delinquency | 1.69*** | 1.34-2.13 | 1.25 | 0.94-1.66 | 1.23 | 0.94-1.61 |
| Race/ethnicity (vs. white) | ||||||
| Hispanic | 1.54*** | 1.20-1.98 | 0.89 | 0.66-1.20 | 0.88 | 0.66-1.20 |
| African American | 1.00 | 0.85-1.19 | 0.38*** | 0.30-0.48 | 0.44*** | 0.36-0.56 |
| Child sex (vs. female) | 1.10 | 0.97-1.24 | 0.95 | 0.81-1.11 | 1.04 | 0.97-1.11 |
| Child antisocial (vs. no) | 3.74*** | 3.16-4.42 | 2.64*** | 2.14-3.24 | 2.59*** | 2.12-3.15 |
| Child anxious/depressed (vs. no) | 2.45*** | 2.11-2.84 | 1.65*** | 1.37-2.00 | 1.66*** | 1.38-1.98 |
| -2 log likelihood (df) | 4036.11 (27) | 4345.11 (26) | ||||
p<0.05;
p<0.01;
p<0.001
UOR= unadjusted odds ratio; AOR= adjusted odds ratio
Table 5.
Maternal education at child's birth and prenatal smoking as predictors of child behavior problems (NLSY first born mother-child dyads 1979-2004, child 4-14 years N≥3,971)
| Covariates | Antisocial (N=3,971) | Anxious/Depressed (N=3,977) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |||||||||
| UOR | 95% CI | AOR | 95% CI | AOR | 95% CI | UOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Maternal education at child's birth (vs. less than high school) | ||||||||||||
| High school | 0.61*** | 0.52-0.72 | 0.84 | 0.69-1.04 | 0.80* | 0.66-0.97 | 0.82 | 0.71-0.97 | 1.12 | 0.92-1.36 | 0.93 | 0.78-1.12 |
| Some college | 0.41*** | 0.33-0.51 | 0.68** | 0.51-0.90 | 0.62*** | 0.48-0.80 | 0.57*** | 0.47-0.69 | 1.34 | 0.81-1.34 | 0.77* | 0.61-0.98 |
| College or more | 0.28*** | 0.22-0.36 | 0.67* | 0.48-0.96 | 0.59*** | 0.43-0.80 | 0.43*** | 0.34-0.52 | 1.08 | 0.79-1.46 | 0.69** | 0.52-0.90 |
| Maternal prenatal smoking (vs. no) | ||||||||||||
| Smoked < pack/day | 1.48*** | 1.25-1.75 | 1.01 | 0.82-1.24 | 1.01 | 0.82-1.25 | 1.30*** | 1.11-1.52 | 0.98 | 0.81-1.18 | 0.99 | 0.82-1.19 |
| Smoked ≥ pack/day | 2.54*** | 1.99-3.25 | 1.45* | 1.07-1.96 | 1.44* | 1.06-1.95 | 2.30*** | 1.82-2.91 | 1.51** | 1.13-2.01 | 1.47** | 1.11-1.96 |
| Maternal postnatal smoking (vs. no) | ||||||||||||
| Smoked < pack/day | 1.63*** | 1.38-1.92 | 1.25* | 1.02-1.54 | 1.26* | 1.02-1.54 | 1.33*** | 1.14-1.56 | 1.00 | 0.83-1.21 | 1.01 | 0.84-1.22 |
| Smoked ≥ pack/day | 1.94*** | 1.51-2.47 | 1.51** | 1.11-2.05 | 1.50** | 1.11-2.03 | 2.04*** | 1.63-2.56 | 1.40* | 1.06-1.86 | 1.37* | 1.04-1.81 |
| Maternal age at first birth | 0.93*** | 0.92-0.94 | 0.98 | 0.96-1.00 | - | - | 0.94*** | 0.92-0.95 | 0.94*** | 0.92-0.96 | - | - |
| Income at first birth | 0.99*** | 0.99-0.99 | 0.99 | 0.99-1.00 | 0.99 | 0.99-1.00 | 0.99*** | 0.99-0.99 | 0.99* | 0.99-0.99 | 0.99** | 0.99-0.99 |
| Marital status at first birth (vs. married) | ||||||||||||
| Divorced, separated, widowed | 1.63** | 1.18-2.26 | 1.24 | 0.87-1.77 | 1.22 | 0.86-1.74 | 0.92 | 0.67-1.27 | 0.74 | 0.52-1.05 | 0.70* | 0.50-0.99 |
| Never married | 2.22*** | 1.86-2.64 | 1.35** | 1.09-1.67 | 1.39** | 1.13-1.72 | 1.61*** | 1.37-1.89 | 1.19 | 0.98-1.45 | 1.31 | 1.08-1.59 |
| Number of children ever born | 1.19*** | 1.12-1.27 | 1.11** | 1.04-1.19 | 1.11** | 1.04-1.19 | 1.16*** | 1.09-1.22 | 1.07*** | 1.00-1.14 | 1.13*** | 1.06-1.14 |
| Maternal depression | 1.10*** | 1.09-1.12 | 1.08*** | 1.06-1.10 | 1.08*** | 1.06-1.10 | 1.10*** | 1.09-1.12 | 1.09*** | 1.07-1.11 | 1.09*** | 1.07-1.10 |
| Maternal delinquency | 1.93*** | 1.56-2.40 | 1.46** | 1.15-1.84 | 1.45** | 1.15-1.84 | 1.56*** | 1.27-1.93 | 1.22 | 0.98-1.53 | 1.21 | 0.94-1.51 |
| Race/ethnicity (vs. white) | ||||||||||||
| Hispanic | 1.42** | 1.09-1.84 | 1.21 | 0.91-1.62 | 1.22 | 0.92-1.63 | 0.97 | 0.76-1.24 | 0.79 | 0.61-1.03 | 0.80 | 0.61-1.05 |
| African American | 2.03*** | 1.69-2.42 | 1.60*** | 1.30-1.98 | 1.62*** | 1.31-2.00 | 0.94 | 0.79-1.12 | 0.67*** | 0.54-0.82 | 0.70*** | 0.61-1.04 |
| Child sex (vs. female) | 1.97*** | 1.72-2.27 | 2.12*** | 1.83-2.46 | 2.13*** | 1.83-2.47 | 0.91 | 0.81-1.03 | 0.91 | 0.80-1.04 | 0.92 | 0.81-1.05 |
| -2 log likelihood (df) | 4448.01 (23) | 4450.52 (22) | 5344.28 (23) | 5381.57 (22) | ||||||||
p<0.05;
p<0.01;
p<0.001
UOR= unadjusted odds ratio; AOR= adjusted odds ratio
The patterns of significant zero-order predictors were very similar for all three outcomes, with two exceptions: race/ethnicity did not predict anxious/depressed behavior; child gender predicted neither anxious/depressed behavior nor lifetime smoking. All other covariates were highly significant. Maternal education at the time of the child's birth, maternal prenatal and postnatal smoking, maternal depression and delinquency were highly significant zero-order predictors of the three outcomes. In the multivariate models, with control for the other covariates, maternal education remained significant, albeit at a much lower level for antisocial behavior, and lost its significance for lifetime smoking and anxiety/depression (Table 5, Models 1). Further analysis, where each covariate was excluded from the models in turn, indicated that the disparity in children's outcomes observed with maternal education appeared to be explained by maternal age at time of child's birth for lifetime smoking and anxiety depression, and only partially explained for antisocial behavior (see Tables 4 and 5, Models 2). Maternal education regained its significance when maternal age at child's birth was omitted from the models. Maternal age at child's birth and educational level are very highly related (r=0.67). Maternal age at child's birth apparently explains the seemingly protective effect of maternal education on child lifetime smoking and anxiety depression but does not eliminate the benefit of having a mother with at least some college education for child antisocial behavior.
Prenatal smoking remained a highly significant predictor of offspring smoking irrespective of the extensiveness of maternal smoking, but was significant only when the mother smoked heavily (one or more packs of cigarettes per day) for both problem behaviors. Postnatal smoking was no longer significant for offspring smoking but remained significant for both problem behaviors, but only when smoking a pack or more a day for anxious/depressed. Maternal depression remained significant for the two problem behaviors, but not lifetime smoking, while maternal delinquency remained significant only for antisocial behavior.
4. Conclusion
Disparities in women's smoking by educational level are pervasive. This study provides further confirmation for the observation that lower education significantly increases the risk of smoking and smoking heavily (Yang et al., 2008; Marmot and Wilkinson, 1999).
The negative impact of educational disadvantage for smoking by women persists with controls for participation in adult social roles, attitudes toward drug use, religiosity, and other predictors of smoking behavior. Each of these factors, which reflect every aspect of women's lives, is related to their smoking. Women's educational disadvantage also has a pervasive negative impact on the second generation. Indeed, women of lower educational level are more likely than women of higher educational level to smoke during pregnancy and their offspring are more likely to smoke themselves and to manifest behavior problems. Thus, the increased risk of smoking associated with lower education appears not only for the women themselves but also for their offspring. Both maternal educational level and smoking in pregnancy have independent negative effects on offspring antisocial behavior, with control for each other and for other predictors of child behavior, except maternal age at time of the child's birth. Maternal education is highly positively related to maternal age at child's birth. Inclusion of this covariate eliminates the impact of maternal education on child smoking and anxiety/depression, but not an antisocial behavior. Maternal smoking in pregnancy is a more important predictor than postnatal smoking of child's smoking. An important finding is the observation that maternal pathology has general or specific effects, depending on the pathology. Maternal depression is associated with increased problem behaviors in offspring, whether antisocial or anxious/depressed, while maternal delinquency is associated only with antisocial behavior. Maternal depression has more widespread consequences than maternal delinquency for the child's adjustment.
A developmental perspective on educational disparities in smoking behavior needs also to consider that there is a cumulative impact of socioeconomic disadvantage from childhood to adulthood that we could not measure in this study. Thus, a British survey found that heavy smoking by young women was related to cumulative exposure to childhood disadvantage, educational disadvantage, early motherhood, and financial hardship (Graham et al., 2006). Similarly, Melchior et al. (2007) found in the Dunedin New Zealand cohort that nicotine dependence at age 32 was higher for those with low SES as children.
In accounting for the impact of socioeconomic disadvantage on women's smoking, one may need to consider other individual factors as well as contextual and biological ones. Contextual factors, in particular tobacco control interventions, may be especially important for low education women (Greaves et al., 2006; Thomas et al., 2008). The smoking behavior of women with lower socioeconomic status appears to be more influenced by tobacco control policies than women with higher status (Kim and Clark, 2006; Levy et al., 2006).
From a biological perspective, we observed that lower education was related to lower levels of circulating cotinine, controlling for number of cigarettes smoked. It should be noted that in prior waves of NHANES, O'Connor et al. (2006) found smaller differences than we did in cotinine levels across educational groups (NHANES III, 1988-1994) or no differences at all (NHANES, 1999-2002). Fidler et al. (2008) report for a national English sample that nicotine intake was significantly higher among individuals with lower social class and higher levels of economic deprivation. Whether higher levels of cotinine among smokers of lower education are due to differences in the topography of smoking cannot be determined from these data. We could not locate national data sets with the appropriate measures to investigate this hypothesis further. However, data on inhalation were available on the mothers of a school-based sample of adolescents in our study of the Transition to Nicotine Dependence in Adolescence (Kandel et al., 2007b). In that sample, while there were no differences in reported frequency of inhalation by educational levels, there were sharp differences in depth of inhalation. The proportions of mothers reporting inhaling deeply or very deeply in the lungs decreased with increasing education from 27.8% of smokers without a high school degree compared with 15.4% of high school graduates, 13.5% of those with some college, and 11.1% of college graduates. Women of lower education may smoke in such a way as to increase the yield of nicotine from cigarettes by inhaling more deeply, but not necessarily more often. This novel finding needs to be replicated. Education may be related to smoking behaviors that enhance the absorption of nicotine from cigarettes, with all the negative health consequences that this entails.
The educational disparity in rates of smoking in pregnancy documented in the NLSY replicates the findings reported in the literature (Clay et al., 1988; Ebrahim et al., 2000; Gilman et al., 2008; Mathews, 2001). Similarly, the impact of prenatal smoking on offspring smoking and negative child behaviors has been reported by others (Al Mamun et al., 2006; Cnattingius, 2004; Griesler et al., 1998; Kandel et al., 1994; Obel et al., 2009; Wakschlag et al., 2002; 2006; Weissman et al., 1999). However, Maughan et al. (2004) found that the association between prenatal smoking and conduct problems disappeared with control for maternal depression and antisocial behavior, whereas the association persisted in our analysis of the NLSY. Furthermore, a recent study stresses that, because of methodological flaws, epidemiological findings regarding the negative consequences of prenatal smoking on children's behavior problems, which did not consider familial factors, may have led to misleading conclusions (D'Onofrio et al., 2008). In multiple births with discrepant maternal smoking across pregnancies within the same family, rates of problem behaviors among offspring were the same irrespective of maternal smoking in pregnancy. The authors conclude that the observed effect of prenatal smoking is due to genetic or environmental factors and not to prenatal smoking. However, it is difficult to reconcile this conclusion with the well documented impact of prenatal smoking on offspring behavioral problems observed repeatedly in animal models (Baler et al., 2008; Slotkin, 2008). Animal studies suggest strongly that these effects are due to nicotine induced neurophysiological changes in the brain of the fetus. There may well be additional genetic or environmental determining factors acting by themselves or in interaction with prenatal smoking (Becker et al., 2008). Prenatal smoking itself appears to have a strong negative influence on offspring development.
Women of low education, especially those without a high school education, are particularly vulnerable to the consequences of smoking, not only for themselves but also for their offspring. These women are more likely to smoke than any other group, and more likely also to continue smoking while pregnant. Their children are more likely to smoke and to exhibit behavioral problems. Since tobacco control policies, such as price and media campaigns, are more effective among women with low education than those with high education (Kim and Clark, 2006; Levy et al., 2006), public health efforts specifically targeted toward low education women would have beneficial effects not only for the women themselves but also for their offspring. As emphasized by Graham et al. (2006), these efforts need to focus as much on social conditions and social policies that affect women's lives, including those in childhood, as on individual level interventions. These would include taxation, social transfer policies, and publicly funded services, such as education, health care, and housing (Graham et al., 2006: p.ii10). We believe that the data we presented make it clear that the optimum strategy for reducing smoking among low SES women, and the negative consequences of smoking for themselves and their children, is to enhance academic achievement and reduce educational disparities at their inception. Targeting the educational system and expanding efforts to enable adolescents to complete high school and strive for higher education will have greater benefits, both for reducing smoking and more broadly for enhancing the life opportunities of women, than remedial efforts targeted towards reducing smoking initiated later in the life cycle when these young women have become adults. Additional educational interventions during pregnancy and postnatally would also be beneficial.
Acknowledgments
One of the four data sets used in the research is from ADD HEALTH, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by a grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. No direct support was received from grant P01-HD31921 for the analysis.
Role of funding source: This research was partially supported by research grants DA12697 from NIDA/NCI and ALF CU51672301A1 from the National Institute on Drug Abuse to Denise Kandel. These agencies had no further role in the study design; in the collection, analysis and interpretation of the data; in the writing of the report; or in the decision to submit the manuscript for publication.
Footnotes
Contributors: Denise B. Kandel developed the study and data analysis plan, supervised the date analysis and implementation, and wrote the manuscript. Pamela Griesler and Christine Schaffran implemented the statistical analysis and assisted in the preparation of the manuscript. All authors read and approved the final manuscript for submission. They all had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest: The authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Al Mamun A, O'Callaghan FV, Alati R, O'Callaghan M, Najman JM, Williams GM, Bor W. Does maternal smoking during pregnancy predict the smoking patterns of young adult offspring? A birth cohort study. Tob Control. 2006;15:452–457. doi: 10.1136/tc.2006.016790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baler RD, Volkow ND, Fowler JS, Benveniste H. Is fetal brain monoamine oxidase inhibition the missing link between maternal smoking and conduct disorders? J Psychiatry Neurosci. 2008;33:187–95. [PMC free article] [PubMed] [Google Scholar]
- Becker K, El-Faddagh M, Schmidt MH, Esser G, Laucht M. Interaction of dopamine transporter genotype with prenatal smoke exposure on ADHD symptoms. J of Pediatr. 2008;152:263–9. doi: 10.1016/j.jpeds.2007.07.004. [DOI] [PubMed] [Google Scholar]
- Buka SL, Schenassa ED, Niaura R. Elevated risk of tobacco dependence among offspring of mothers who smoked during pregnancy: a 30-year prospective study. Am J Psychiatry. 2003;160:1978–1984. doi: 10.1176/appi.ajp.160.11.1978. [DOI] [PubMed] [Google Scholar]
- Breslau N, Fenn N, Peterson EL. Early smoking initiation and nicotine dependence in a cohort of young adults. Drug Alcohol Depend. 1993;33:129–137. doi: 10.1016/0376-8716(93)90054-t. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lewisohn PM, Seeley JR, Wagner EF. Cigarette smoking, major depression, and other psychiatric disorders among adolescents. J Am Acad Child Adolesc Psychiatry. 1996;35:1602–1610. doi: 10.1097/00004583-199612000-00011. [DOI] [PubMed] [Google Scholar]
- Center for Human Resource Research. NLSY 1979 user's guide: a guide to the 1979-2004 National Longitudinal Survey of Youth data. The Ohio State University; Columbus, OH: 2006. [Google Scholar]
- Clay CM, Dyer AR, Liu K, Stamler J, Shekelle RB, Berkson DM, Paul O, Schoenberger JA, Lepper M, Undberg HA, Marquardt J, Stamler R, Collette P, Garside D. Education, smoking and non-cardiovascular mortality: findings in three Chicago epidemiological studies. Int J Epidemiol. 1988;17:341–347. doi: 10.1093/ije/17.2.341. [DOI] [PubMed] [Google Scholar]
- Cnattingius S. The epidemiology of smoking during pregnancy: smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob Res. 2004;6:S125–S140. doi: 10.1080/14622200410001669187. [DOI] [PubMed] [Google Scholar]
- Cornelius MD, Goldschmidt L, Leech S, Day NL. Prenatal tobacco exposure: a risk factor for preadolescent smoking. Nicotine Tob Res. 2000;2:45–52. doi: 10.1080/14622200050011295. [DOI] [PubMed] [Google Scholar]
- D'Onofrio BM, Van Hulle CA, Waldman ID, Rodgers JL, Harden KP, Rathouz PJ, Lahey BB. Smoking during pregnancy and offspring externalizing problems: an exploration of genetic and environmental confounds. Development Psychopathology. 2008;20:139–164. doi: 10.1017/S0954579408000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahim SH, Floys RI, Merritt RK, II, Decoufle P, Holtzman D. Trends in pregnancy-related smoking rates in the United States, 1987-1996. JAMA. 2000;283:361–366. doi: 10.1001/jama.283.3.361. [DOI] [PubMed] [Google Scholar]
- Eikemo TA, Huisman M, Bambra C, Kunst AE. Health inequalities according to educational level in different welfare regimes: a comparison of 23 European countries. Sociology Health Illn. 2007;30:565–582. doi: 10.1111/j.1467-9566.2007.01073.x. [DOI] [PubMed] [Google Scholar]
- Fidler JA, Jarvis MJ, Mindell J, West R. Nicotine intake in cigarette smokers in England: distribution and demographic correlates. Cancer Epidemiol Biomarkers Prev. 2008;17:3331–3336. doi: 10.1158/1055-9965.EPI-08-0296. [DOI] [PubMed] [Google Scholar]
- Gilman SE, Breslau J, Subramanian SV, Hitsman B, Koenan KC. Social factors, psychopathology and maternal smoking during pregnancy. Am J Public Health. 2008;98:448–453. doi: 10.2105/AJPH.2006.102772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giskes K, Kunst AE, Benach J, Borrel C, Costa G, Dahl E, Dalstra JAA, Federico B, Helmert U, Judge K, Lahelma E, Moussa K, Ostergren PO, Platt S, Prattala R, Rasmussen NK, Mackenbach JP. Trends in smoking behaviour between 1985 and 2000 in nine European countries by education. J Epidemiol Community Health. 2005;59:395–401. doi: 10.1136/jech.2004.025684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham H, Inskip HM, Francis B, Harman J. Pathways of disadvantage and smoking careers: evidence and policy implications. J Epidemiol Comm Health. 2006;60:ii7–ii12. doi: 10.1136/jech.2005.045583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greaves L, Vallone D, Velicer W. Tobacco control policy and low socioeconomic status women and girls. J Epidemiol Comm Health. 2006;60:ii1–ii12. doi: 10.1136/jech.2006.052480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griesler PC, Kandel DB, Davies M. Maternal smoking in pregnancy, child behavior problems, and adolescent smoking. J Res Adol. 1998;8:159–185. [Google Scholar]
- Harris KM, Florey F, Tabor J, Bearman PS, Jones J, Udry JR. Chapel Hill, NC: Carolina Population Center, University of North Carolina; 2003. [7/11/2008]. The national longitudinal study of adolescent health: research design. http://www.cpc.unc.edu/projects/addhealth/design. [Google Scholar]
- House JS. Understanding social factors and inequalities in health: 20th century progress and 21st century prospects. J Health Social Behav. 2002;43:125–142. [PubMed] [Google Scholar]
- Jarvis MJ, Tunstall-Pedoe H, Feyerabend C, Vesey C, Saloojee Y. Biochemical markers of smoke absorption and self-reported exposure to passive smoking. J Epidemiol Comm Health. 1984;38:335–339. doi: 10.1136/jech.38.4.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel DB, Hu M, Schaffran C, Udry JR, Benowitz NL. Urine nicotine metabolites and smoking behavior in a multiracial/multiethnic national sample of young adults. Am J Epidemiol. 2007a;165:901–910. doi: 10.1093/aje/kwm010. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Hu M, Griesler PC, Schaffran C. On the development of nicotine dependence in adolescence. Drug Alc Depend. 2007b;91:26–39. doi: 10.1016/j.drugalcdep.2007.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel DB, Wu P, Davies M. Maternal smoking during pregnancy and smoking by adolescent daughters. Am J Public Health. 1994;84:1407–1413. doi: 10.2105/ajph.84.9.1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, Clark PI. Cigarette smoking transition in females of low socioeconomic status: impact of state, school, and individual factors. J Epidemiol Comm Health. 2006;60:13–19. doi: 10.1136/jech.2005.045658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kollins SH, McClernon J, Fuemmeler BF. Association between smoking and attention-deficit/hyperactivity disorder symptoms in a population-based sample of young adults. Arch Gen Psychiatry. 2005;62:1142–1147. doi: 10.1001/archpsyc.62.10.1142. [DOI] [PubMed] [Google Scholar]
- Laaksonen M, Rahkonen O, Karvonen S, Lahelma E. Socioeconomic status and smoking: analyzing inequalities with multiple indicators. Eur J Public Health. 2005;15:262–269. doi: 10.1093/eurpub/cki115. [DOI] [PubMed] [Google Scholar]
- Levy DT, Mumford EA, Compton C. Tobacco control policies and smoking in a population of low education women, 1992-2002. J Epidemiol Comm Health. 2006;60:ii20–ii26. doi: 10.1136/jech.2005.045542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Fergusson DM. Childhood conduct problems, attention deficit behaviors, and adolescent alcohol, tobacco, and illicit drug use. J Abnorm Child Psychol. 1995;23:281–302. doi: 10.1007/BF01447558. [DOI] [PubMed] [Google Scholar]
- Marmot M, Wilkinson RG. Social determinants of health. Oxford University Press; New York, NY: 1999. [Google Scholar]
- Maughan B, Taylor A, Caspi A, Moffit TE. Prenatal smoking and early childhood conduct problems. Arch Gen Psychiatry. 2004;61:836–843. doi: 10.1001/archpsyc.61.8.836. [DOI] [PubMed] [Google Scholar]
- Matthews TJ. Smoking during pregnancy in the 1990s. Nat Vital Stat Rep. 2001;49:1–14. [PubMed] [Google Scholar]
- McCaffery JM, Papandonatos GD, Lyons MJ, Koenen KC, Tsuang MT, Niaura R. Educational attainment, smoking initiation and lifetime nicotine dependence among male Vietnam-era twins. Psychological Med. 2007;37:1–11. doi: 10.1017/S0033291707001882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchior M, Moffitt TE, Milne BJ, Poulton R, Caspi A. Who do children from socioeconomically disadvantaged families suffer from poor health when they reach adulthood? A life-course study. Am J Epidemiol. 2007;166:966–74. doi: 10.1093/aje/kwm155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milberger S, Biederman J, Faraone SV, Chen L, Jones J. Is maternal smoking during pregnancy a risk factor for attention deficit hyperactivity disorder in children? Am J Psychiatry. 1996;153:1138–1142. doi: 10.1176/ajp.153.9.1138. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Ross CE, Reynolds J. Links between social status and health. In: Bird CE, Conrad P, Fremont AM, editors. Handbook of Medical Sociology. Prentice Hall; New Jersey: 2000. pp. 47–67. [Google Scholar]
- Moffitt TE. Adolescent-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychol Rev. 1993;100:647–701. [PubMed] [Google Scholar]
- National Health and Nutrition Examination Survey Codebook for Data Production (2005-2006) [3/4/2008];2008 Serum cotinine (COT-D), http://www.cdc.gov/nchs/nhanes.
- Obel C, Linnet KM, Hanriksen TB, Rodriguez A, Jarvelin MR, Kotimaa A, Moilanen I, Ebeling H, Bilenberg N, Taanila A, Ye G, Olsen J. Smoking during pregnancy and hyperactivity-inattention in the offspring: comparing results from three Nordic cohorts. Int J Epidemiol. 2009;38:1–8. doi: 10.1093/ije/dym290. [DOI] [PubMed] [Google Scholar]
- O'Callaghan FV, O'Callaghan M, Najman JM, Williams GM, Bor W, Alati R. Prediction of adolescent smoking from family and social risk factors at 5 years, and maternal smoking in pregnancy and at 5 and 14 years. Addiction. 2006;101:282–290. doi: 10.1111/j.1360-0443.2006.01323.x. [DOI] [PubMed] [Google Scholar]
- O'Connor RJ, Giovino GA, Kozlowski LT, Shiffman S, Hyland A, Bernert JT, Caraballo RS, Cummings KM. Changes in nicotine intake and cigarette use over time in two nationally representative cross-sectional samples of smokers. Am J Epidemiol. 2006;164:750–759. doi: 10.1093/aje/kwj263. [DOI] [PubMed] [Google Scholar]
- Olafsdottir S. Fundamental causes of health disparities, the welfare state, and health in the United States and Iceland. J Health Social Behav. 2007;48:239–253. doi: 10.1177/002214650704800303. [DOI] [PubMed] [Google Scholar]
- Orlebeke JF, Knol DL, Verhulst FC. Increase in child behavior problems resulting from maternal smoking in pregnancy. Arch Environ Health. 1997;52:317–321. doi: 10.1080/00039899709602205. [DOI] [PubMed] [Google Scholar]
- Peterson JL, Zill N. Marital disruption, parent-child relationships, and behavioral problems in children. J Marriage Family. 1986;48:367–374. [Google Scholar]
- Richardson SA, Tizabi Y. Hyperactivity in the offspring of nicotine-treated rats: role of the mesolimbic and nigrostriatal dopaminergic pathways. Pharmacol Biochem Behav. 1994;47:331–337. doi: 10.1016/0091-3057(94)90018-3. [DOI] [PubMed] [Google Scholar]
- Robert SA, House JS. Socioeconomic inequalities in health: an enduring sociological problem. In: Bird A, Conrad P, Fremont A, editors. Handbook of Medicinal Sociology. London: Sage Publishing Company; 2000. [Google Scholar]
- Schaap MM, Van Agt HME, Kunst AE. Identification of socioeconomic groups at increased risk for smoking in European countries: looking beyond educational level. Nicotine Tob Res. 2008;10:359–369. doi: 10.1080/14622200701825098. [DOI] [PubMed] [Google Scholar]
- Schnittker J, McLeod JD. The social psychology of health disparities. Annual Rev Sociology. 2005;31:75–103. [Google Scholar]
- Shea AK, Steiner M. Cigarette smoking during pregnancy. Nicotine Tob Res. 2008;10:267–278. doi: 10.1080/14622200701825908. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Waters AJ, Hickcox M. The nicotine dependence syndrome scale: a multi-dimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6:327–348. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- Slotkin TA. If nicotine is a developmental neurotoxicant in animal studies, dare we recommend nicotine replacement therapy in pregnant women and adolescents? Neur Teratology. 2008;30:1–19. doi: 10.1016/j.ntt.2007.09.002. [DOI] [PubMed] [Google Scholar]
- Storr CL, Reboussin BA, Anthony JC. Early childhood misbehavior and the estimated risk of becoming tobacco-dependent. Am J Epidemiol. 2004;160:126–130. doi: 10.1093/aje/kwh184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health, 2006. Research Triangle Park, NC: Research Triangle Institute; Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2007a. Office of Applied Studies. [Computer file]. ICPSR21240-v2. [producer], 2007. [distributor], 2007-12-10. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. 2006 National Survey on Drug Use and Health, Public Use File Codebook. Office of Applied Studies; Rockville, MD: 2007b. [Google Scholar]
- Thomas S, Fayter D, Misso K, Ogilvie D, Petticrew M, Sowden A, Whitehead M, Worthy G. Population tobacco control interventions and their effects on social inequalities in smoking: systematic review. Tob Control. 2008 doi: 10.1136/tc.2007.023911. Ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton A, Axinn WG, Teachman JD. The influence of school enrollment and accumulation on cohabitation and marriage in early adulthood. Am Soc Rev. 1995;60:762–774. [Google Scholar]
- U.S. Census Bureau. Statistical Abstract of the United States: 2008. 127th. Washington, D.C.: 2007. [Google Scholar]
- U.S. Department of Health and Human Services. Women and Smoking: a report of the surgeon general. U.S. Department of Health and Human Services, Public Health Office of the Surgeon General; Washington, D.C.: 2001. [Google Scholar]
- U.S. Department of Health and Human Services. Preventing smoking and exposure to secondhand smoke before, during, and after pregnancy. U.S. Department of Health and Human Services, Centers for Disease Prevention and Health Promotion; Atlanta, GA: 2007. [Google Scholar]
- Vaglenova J, Birru S, Pandiella NM, Breese CR. An assessment of the long-term developmental and behavioral teratogenicity of prenatal nicotine exposure. Behav Brain Res. 2004;150:159–170. doi: 10.1016/j.bbr.2003.07.005. [DOI] [PubMed] [Google Scholar]
- Wakschlag LS, Leventhal BL, Pine DS, Pickett KE, Carter AS. Elucidating early mechanisms of developmental psychopathology: the case of prenatal smoking and disruptive behavior. Child Development. 2006;77:893–906. doi: 10.1111/j.1467-8624.2006.00909.x. [DOI] [PubMed] [Google Scholar]
- Wakschlag LS, Pickett KE, Cook E, Benowitz NL, Leventhal BL. Maternal smoking during pregnancy and severe antisocial behavior in offspring: a review. Am J of Public Health. 2002;92:966–974. doi: 10.2105/ajph.92.6.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace J. Understanding racial and ethnic influences on smoking among women. Drug Alcohol Depend in press. [Google Scholar]
- Weissman MM, Warner V, Wickramaratne P, Kandel DB. Maternal smoking during pregnancy and psychopathology in offspring followed to adulthood. J Am Acad Chold Adolesc Psychiatry. 1999;38:892–899. doi: 10.1097/00004583-199907000-00020. [DOI] [PubMed] [Google Scholar]
- Winzer-Serhan UH. Long-term consequences of maternal smoking and developmental chronic nicotine exposure. Front Bioscience. 2008;13:636–649. doi: 10.2741/2708. [DOI] [PubMed] [Google Scholar]
- Yang S, Lynch J, Schulenberg J, Diez Roux AV, Raghunathan T. Emergence of socioeconomic inequalities in smoking and overweight and obesity in early adulthood: the National Longitudinal Adolescent Health. Am J Pub Health. 2008;98:468–477. doi: 10.2105/AJPH.2007.111609. [DOI] [PMC free article] [PubMed] [Google Scholar]