Abstract
The Dietary Approaches to Stop Hypertension (DASH) diet reduces blood pressure, and consistency with the DASH diet has been associated with lower rates of heart failure (HF) in women. The authors examined the association between consistency with DASH and rates of HF hospitalization or mortality in 38,987 participants in the Cohort of Swedish Men aged 45 to 79 years. Diet was measured using food-frequency questionnaires, and scores were created to assess consistency with DASH by ranking intake of DASH diet components. Cox models were used to calculate rate ratios of HF (807 incident cases) determined through the Swedish inpatient and cause-of-death registers between January 1, 1998 and December 31, 2006. In multivariable-adjusted analyses, men in the highest quartile of the DASH component score had a 22% lower rate of HF events then those in the lowest quartile (95% confidence interval: 5%, 35%, p for trend = 0.006). In conclusion, greater consistency with the DASH diet was associated with lower rates HF events in men aged 45 to 79 years.
Keywords: diet, heart failure, epidemiology
Elevated blood pressure is a key risk factor for heart failure (HF), a prevalent condition among older adults that causes high mortality and morbidity.1, 2 The Dietary Approaches to Stop Hypertension (DASH) diet represents a potential non-pharmacologic strategy for the prevention of HF.1 Although trials of the DASH diet were not long enough to determine the effect on HF incidence, we previously reported that consistency with the DASH diet was associated with lower rates of HF events in women.3 In other populations, DASH diet scores have been associated with rates of coronary heart disease, stroke, and mortality.4–6 We therefore examined the association between consistency with the DASH diet and rates of HF hospitalization and mortality in men aged 45 to 79 years.
METHODS
This study included 38,987 participants in the Cohort of Swedish Men. The cohort recruitment process, characteristics, and study methods have been previously described.7 Men aged 45 to 79 years in Västmanland and Örebro counties in central Sweden were sent self-administered questionnaires on demographics, weight, height, and intake of foods and beverages in late 1997 and early 1998 and 48,850 responded. Participants were excluded (n = 2,201) because of missing or incorrect national identification numbers, blank questionnaires, or previous diagnosis of cancer (except non-melanoma skin cancer). For this analysis, men with implausible energy intake (>3 standard deviations from the natural logarithm transformed mean) or missing data for more than half of the food and beverage items (n = 1,667) and men with a history of HF, myocardial infarction, or diabetes mellitus at baseline were also excluded (n = 5,995). Participants with baseline myocardial infarction or diabetes mellitus were excluded because men with these conditions receive dietary counseling and may change both their diet and their reporting of diet. History of HF and myocardial infarction were determined through linkage to the inpatient register; history of diabetes was assessed using self-report and linkage to the inpatient register. The study was approved by the Regional Ethical Review Board at Karolinska Institute, Stockholm, Sweden. Completion and return by mail of the self-administered questionnaire was assumed to imply consent.
Self-administered food-frequency items in the questionnaires asked participants to report usual frequency of consumption of 96 foods and beverages over the previous year. For foods such as milk, coffee, cheese, and bread that are commonly eaten in Sweden, participants reported their consumption in servings per day or per week. For other foods there were 8 predefined responses ranging from never to ≥ 3 times/day. Portion sizes for most foods were not specified. In validation studies using weighed diet records, habitual portion sizes were found to vary by age. The total consumption of foods and beverages was calculated by multiplying the frequency of consumption by age-specific portion sizes. To make the food intake data comparable to US dietary recommendations, we standardized portion sizes to those used in the United States.8 Nutrient values were calculated using food composition data from the Swedish National Food Administration.9
The DASH diet component score was based on the score proposed by Fung and colleagues which ranked participants on intake of 1) fruits, 2) vegetables, 3) nuts and legumes, 4) low-fat dairy, 5) whole grains, 6) sodium, 7) sweetened beverages, and 8) red and processed meats.5 Participants in the highest quintile of fruits, vegetables, nuts and legumes, low-fat dairy, and whole grains received a score of 5 and those in the lowest quintile received a score of 1; participants in intermediate quintiles received intermediate scores. Participants in the highest quintile of sodium, sweetened beverages, and red and processed meats received a score of 1 and those in the lowest quintile received a score of 5; participants in intermediate quintiles received intermediate scores. The score for each component was summed to get the overall DASH score.
Participants were followed from January 1, 1998 until December 31, 2006 through record linkage to the Swedish inpatient and cause-of-death registers. The inpatient register captures more than 99% of inpatient care.10 Hospitalization for or death from HF was identified by codes 428 (International Classification of Disease-9), I50, or I11.0 (International Classification of Disease-10). Ingelsson and colleagues found that 95% of people with these codes as primary diagnosis in the inpatient register had confirmed HF on medical record review using European Society of Cardiology criteria.11 We included only hospitalizations or deaths with HF listed as the primary diagnosis and only the first HF event recorded in the registers for each individual. Incident myocardial infarction during follow-up was also assessed through the inpatient register.
Because some of the participants were missing data on body mass index (4.6%) and physical activity (21.6%), we used Markov chain Monte Carlo multiple imputation to simulate 5 complete datasets.12 All statistical analyses described were performed in each dataset separately. The results were averaged, and confidence intervals and p values were calculated accounting for uncertainty in the imputed estimates.12 Results from complete case analyses were similar in the primary and stratified analyses, though with wider confidence intervals; only the multiple imputation analyses are presented.
We calculated the mean food and nutrient intake by approximate quartiles of the DASH component score. We computed means and percentages of demographic, behavioral, and health covariates and tested for differences across quartiles using analysis of variance for continuous variables and χ2 tests for categorical variables. We used Cox proportional hazards models that accounted for the effect of age by allowing the baseline rate to vary to calculate incidence rate ratios and associated 95% confidence intervals.13 This allows for a flexible and unspecified relationship between age and HF. We examined the incidence rate ratios of HF associated with quartiles of the DASH score. We tested for linear trend by entering the median value in each quartile as a continuous predictor. We adjusted for physical activity (linear), energy intake (linear), education (< high school, high school, university), family history of myocardial infarction at < 60 years (yes, no), cigarette smoking (current, past, never), marital status (single, married, divorced, widowed), self-reported history of hypertension and high cholesterol, body mass index (linear), and incident myocardial infarction as a time varying covariate (none, within 1 year, and more distant history).
We examined whether the associations between the DASH component score and HF varied by self-reported history of hypertension, self-reported history of high cholesterol, current smoking, and overweight (body mass index ≥ 25 kg/m2) and performed tests of interaction. Because unrecognized illness at baseline may have influenced diet, we conducted a sensitivity analysis excluding the first 2 years of follow-up. We tested for violations of the proportional hazards assumption by entering the product of the DASH diet score and the natural logarithm of time in the model. The proportional hazards assumption did not appear to be violated in any of the models. Statistical analyses were performed using SAS version 9.1 (Cary, NC). A 2-sided p value < 0.05 was considered statistically significant.
RESULTS
Over 9 years of follow-up of 38,987 men aged 45 to 79 years, 710 were hospitalized for HF and 97 died of HF, a rate of 24 cases per 10,000 person-years. Men in the top quartile of the DASH diet component score consumed, on average, more fruit, vegetables, whole grains, and low-fat dairy and less sweetened beverages and red or processed meat than men in the bottom quartile of the DASH diet component score (Table 1). Compared to men in the lowest quartile of the DASH component score, men with diets more consistent with DASH were more likely to have a history of high cholesterol and to have completed high school or university, less likely to smoke cigarettes, and more likely to be married (Table 2).
Table 1.
Dietary Approaches to Stop Hypertension component score and nutrient and food intake
| Dietary Approaches to Stop Hypertension component score |
||||
|---|---|---|---|---|
| Variable | Quartile 1 | Quartile 2 | Quartile 3 | Quartile 4 |
| Mean nutrient intake* | ||||
| Total energy (kcal/d) | 2,753 | 2677 | 2,687 | 2,675 |
| Total fat (g/d) | 79.2 | 76.4 | 74.1 | 69.2 |
| Saturated fat (g/d) | 36.5 | 34.8 | 33.4 | 30.7 |
| Protein (g/d) | 83.9 | 86.0 | 87.3 | 89.0 |
| Carbohydrate (g/d) | 268 | 272 | 276 | 286 |
| Cholesterol (mg/d) | 314 | 302 | 293 | 271 |
| Sodium (mg/d) | 3,210 | 3,220 | 3,224 | 3,211 |
| Potassium (mg/d) | 3,111 | 3,346 | 3,541 | 3,854 |
| Calcium (mg/d) | 1,133 | 1,193 | 1,229 | 1,289 |
| Magnesium (mg/d) | 355 | 384 | 403 | 435 |
| Fiber (g/d) | 21.0 | 24.4 | 26.7 | 30.6 |
| Alcohol (g/d) | 10.5 | 10.9 | 10.8 | 10.4 |
| Mean food intake | ||||
| Fruit (servings/d) | 1.1 | 1.5 | 1.9 | 2.6 |
| Vegetables (servings/d) | 1.2 | 1.6 | 2.0 | 2.6 |
| Whole grain (servings/d) | 6.2 | 7.7 | 8.5 | 9.9 |
| Low-fat dairy (servings/d) | 0.7 | 1.2 | 1.5 | 2.0 |
| Sweetened beverages (servings/d) | 1.0 | 0.6 | 0.4 | 0.2 |
| Red or processed meat (servings/d) | 1.6 | 1.3 | 1.2 | 1.0 |
Nutrients (except total energy and alcohol) were adjusted for energy intake using the residuals method
Table 2.
Characteristics of study participants by quartiles of Dietary Approaches to Stop Hypertension component score*
| Dietary Approaches to Stop Hypertension component score |
||||
|---|---|---|---|---|
| Variable | Quartile 1 | Quartile 2 | Quartile 3 | Quartile 4 |
| Number of subjects | 10,978 | 6,878 | 10,773 | 10,358 |
| Age (years) | 58.4 (9.7) | 59.0 (9.6) | 59.5 (9.4) | 59.9 (9.1) |
| Body mass index (kg/m2) | 25.8 (3.4) | 25.8 (3.3) | 25.7 (3.2) | 25.5 (3.1) |
| History of hypertension | 19.0% | 19.1% | 20.5% | 20.3% |
| History of high cholesterol | 10.5% | 11.2% | 12.4% | 13.2% |
| Family history of myocardial infarction at < 60 years | 16.0% | 16.3% | 15.8% | 15.7% |
| Physical activity (Metabolic equivalent task-hours/d) | 41.8 (5.2) | 41.6 (5.0) | 41.5 (4.8) | 41.6 (4.7) |
| Education | ||||
| < high school | 74.0% | 69.8% | 67.0% | 60.6% |
| High school | 13.4% | 14.3% | 14.4% | 16.4% |
| University | 12.6% | 15.9% | 18.6% | 23.0% |
| Cigarette smoker | ||||
| Current | 31.4% | 26.0% | 22.7% | 18.3% |
| Past | 36.5% | 37.8% | 39.4% | 39.1% |
| Never | 32.1% | 36.17% | 37.8% | 42.6% |
| Marital Status | ||||
| Single | 8.5% | 6.4% | 5.9% | 5.2% |
| Married | 79.0% | 83.7% | 85.2% | 86.0% |
| Divorced | 8.4% | 6.8% | 5.8% | 6.2% |
| Widowed | 4.2% | 3.1% | 3.1% | 2.5% |
Values are mean (standard deviation) or %. All variables except family history of myocardial infarction at < 60 years are significantly different across quartiles of Dietary Approaches to Stop Hypertension component score.
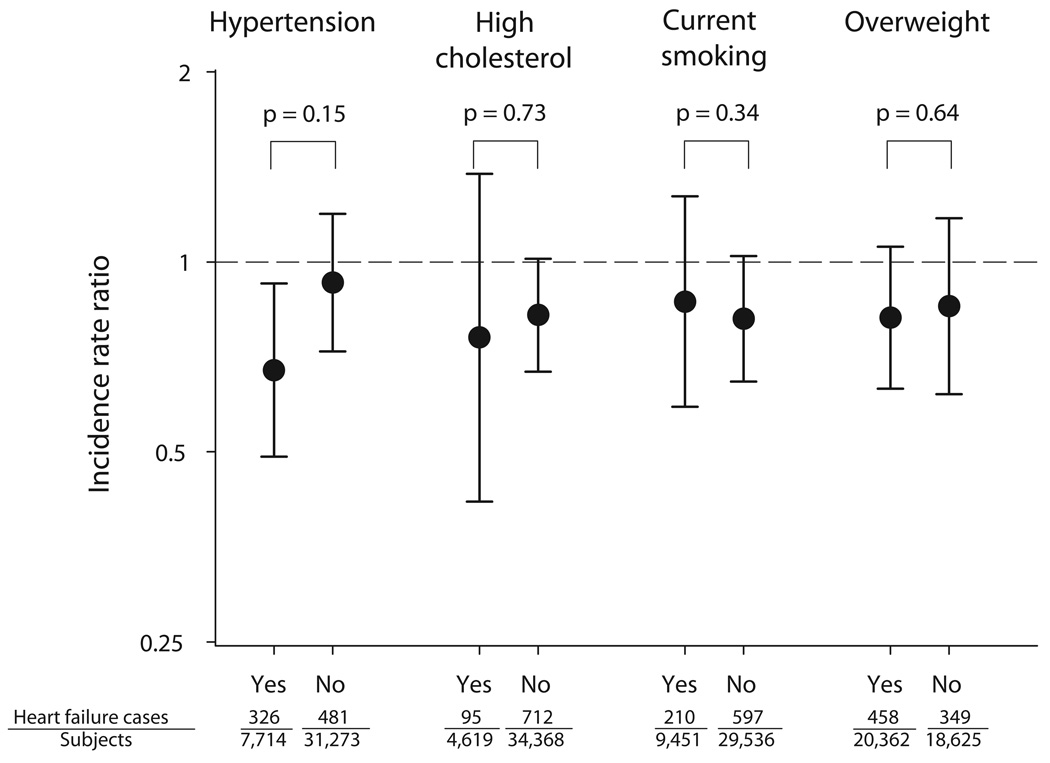
In multivariable-adjusted analysis, men in the highest quartile of the DASH diet component score had a lower rate of HF events then those in the lowest quartile (Table 3). Results were not materially different when the first 2 years of follow-up were excluded. The association between the DASH diet component score and HF events appeared to be stronger in men who reported a history of hypertension than in men who did not, but the difference did not reach statistical significance (Figure). The association did not appear to vary by high cholesterol, cigarette smoking, or overweight.
Table 3.
Association of Dietary Approaches to Stop Hypertension component score with incident heart failure
| Dietary Approaches to Stop Hypertension component score |
|||||
|---|---|---|---|---|---|
| Quartile 1 | Quartile 2 | Quartile 3 | Quartile 4 | p Value | |
| DASH component score | |||||
| Range | 8–21 | 22–23 | 24–26 | 27–38 | |
| Cases | 257 | 146 | 212 | 192 | |
| Person-years | 93,667 | 58,916 | 92,445 | 89,207 | |
| Incidence rate ratio | |||||
| (95% confidence interval)* | 1.00 (Reference) | 0.86 (0.70–1.06) | 0.77 (0.64–0.93) | 0.71 (0.59–0.86) | <0.001 |
| Incidence rate ratio | |||||
| (95% confidence interval)† | 1.00 (Reference) | 0.88 (0.72–1.08) | 0.80 (0.67–0.96) | 0.78 (0.65–0.95) | 0.006 |
Cox proportional hazards models accounting for age.
Cox proportional hazards models accounting for age and additionally adjusted for physical activity (linear), energy intake (linear), education (less than high school, high school, university), family history of myocardial infarction at less than 60 years (yes, no), cigarette smoking (current, past, never), marital status (single, married, divorced, widowed), self-reported history of hypertension and high cholesterol (yes, no), body mass index (linear), and incident myocardial infarction (none, within 1 year, and more distant history).
Figure 1.
The circles represent the incidence rate ratios of heart failure comparing the top to bottom quartiles of the DASH component score, and lines represent 95% confidence intervals. P values are for tests of the difference in estimates between those with and without history of hypertension, history of high cholesterol, current cigarette smoking, and body mass index ≥ 25 kg/m2. Estimates come from Cox proportional hazards models accounting for age and adjusted for physical activity (linear), energy intake (linear), education (< high school, high school, university), family history of myocardial infarction at < 60 years (yes, no), cigarette smoking (current, past, never), marital status (single, married, divorced, widowed), history of hypertension and high cholesterol (yes, no), body mass index (linear), and incident myocardial infarction (none, within 1 year, and more distant history). All variables except incident myocardial infarction and incident heart failure are based on self-report.
DISCUSSION
In this population, consistency with the DASH diet was associated with lower rates of HF events; men in the top quartile of a score which ranked DASH diet components had 22% lower rates of HF events than those in the lowest quartile. We previously reported that women in the top quartile of the DASH diet component score had a 37% lower rate of HF events compared to those in the lowest quartile; scores using other strategies to measure consistency with DASH had similar patterns of association.3 The weaker association in this population of men may be due to chance variation. However, the men with diets most similar to the DASH diet consumed fewer fruits and vegetables in the setting of greater total energy intake compared to the women in the previous report. In addition, the men in the top quartiles of the DASH diet scores ate more red or processed meat and drank more sweetened beverages than the women.
These results are consistent with observational studies of other cardiovascular diseases. Fung and colleagues found statistically significant associations between a diet score based on ranking DASH diet components and incidence of coronary heart disease and stroke.5 Although the associations did not reach statistical significance, there was a trend towards lower rates of incident hypertension, coronary heart disease mortality, stroke mortality, and cardiovascular mortality associated with a DASH diet score based on food and nutrient recommendations in a study by Folsom and colleagues.4 Parikh and colleagues observed that a DASH score based on nutrient recommendations was associated with lower rates of all-cause, ischemic heart disease, and stroke mortality in hypertensive men and women.6 In a cross-sectional analysis, people in the top quartile of a DASH diet score had 1.5 mmHg lower systolic blood pressure and 1.4 mmHg lower diastolic blood pressure.14 During 5.4 years of follow-up, the blood pressure of those in the top quartile of the DASH score increased less than those with lower DASH scores. The PREMIER trial of multiple lifestyle interventions showed that a DASH adherence index was associated with lower systolic blood pressure, but the association was not statistically significant after control for weight change.15 In a nationally representative study of US adults, consistency with DASH was associated with older age, a diagnosis of diabetes, and higher education.16
In a 2-month randomized trial of 459 adults with normal or modestly elevated blood pressure, the DASH diet lowered mean systolic blood pressure by 5.5 mmHg and diastolic blood pressure by 3.0 mm Hg.17 Sodium restriction lead to a further reduction in blood pressure in a second trial.18 The DASH diet lowered low density lipoprotein cholesterol, decreasing risk of cardiovascular disease, but it also lowered high density lipoprotein cholesterol and may have increased triglycerides.19 The 5.5 mm Hg decrease in systolic blood pressure seen in the DASH trial would be expected to reduce the rate of HF by approximately 12% based data from the Framingham Heart Study.20 Several other potentially beneficial effects of the DASH diet have been reported including estrogenic activity from phytochemicals 21, 22 and lower oxidative stress.23 Excess fatty acids and glucose in circulation can be caused by poor diet and may be the link between diet and HF through changes in the heart’s mechanical efficiency, triglyceride content, hypertrophy, fibrosis, and mitochondrial function.24
There are several important limitations of this study. HF is a heterogeneous syndrome rather than a single disease, and risk factors may not be the same for all HF subtypes.1 We did not have information on HF etiology or subtype in this population. Although Swedish inpatient and cause-of-death registers are nearly complete and the accuracy of HF diagnosis is high,11, 25 we could only assess cases of HF that resulted in hospitalization or death. Therefore, our results may not apply to less severe cases of HF treated on an outpatient basis. Because there was no in-person examination, hypertension and other exposures were measured by self-report, which is inherently less reliable than clinical measurement. This could have resulted in residual confounding of the association between the DASH diet component score and HF. The DASH diet component score has not been validated against an external standard; however, the food-frequency questionnaire used in this population has been validated against diet records. Correlations with diet records were 0.5–0.7 for fruits,26 0.4–0.6 for vegetables,26 0.5–0.7 for whole grains,27 0.4–0.6 for dairy,28 and 0.6 for sweetened beverages.29 Using food-frequency questionnaires resulted in some exposure misclassification. If the misclassification of diet was unrelated to HF incidence, the results would likely be biased towards the null. However, this assumption was not verifiable with the data available.
Acknowledgments
This study was supported by grants from the Swedish Research Council/Committee for infrastructure and the Committee for Medicine, Stockholm, Sweden, the Swedish Foundation for International Cooperation in Research and Higher Education (STINT), Stockholm, Sweden, and National Institutes of Health, Bethesda, Maryland grant F32 HL091683 (to Dr. Levitan).
References
- 1.Schocken DD, Benjamin EJ, Fonarow GC, Krumholz HM, Levy D, Mensah GA, Narula J, Shor ES, Young JB, Hong Y. Prevention of heart failure: A scientific statement from the American Heart Association Councils on Epidemiology and Prevention, Clinical Cardiology, Cardiovascular Nursing, and High Blood Pressure Research; Quality of Care and Outcomes Research Interdisciplinary Working Group; and Functional Genomics and Translational Biology Interdisciplinary Working Group. Circulation. 2008;117:2544–2565. doi: 10.1161/CIRCULATIONAHA.107.188965. [DOI] [PubMed] [Google Scholar]
- 2.Kozak LJ, DeFrances CJ, Hall MJ. Nation hospital discharge survey: 2004 annual summary with detailed diagnosis and procedure data. National Center for Health Statistics. Vital Health Stat. 2006;13(162) [PubMed] [Google Scholar]
- 3.Levitan EB, Wolk A, Mittleman MA. Consistency with the DASH diet and incidence of heart failure. Arch Intern Med. 2009;169:851–857. doi: 10.1001/archinternmed.2009.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Folsom AR, Parker ED, Harnack LJ. Degree of concordance with DASH diet guidelines and incidence of hypertension and fatal cardiovascular disease. Am J Hypertens. 2007;20:225–232. doi: 10.1016/j.amjhyper.2006.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–720. doi: 10.1001/archinte.168.7.713. [DOI] [PubMed] [Google Scholar]
- 6.Parikh A, Lipsitz SR, Natarajan S. Association between a DASH-like diet and mortality in adults with hypertension: Findings from a population-based follow-up study. Am J Hypertens. 2009 doi: 10.1038/ajh.2009.10. [DOI] [PubMed] [Google Scholar]
- 7.Larsson SC, Rutegard J, Bergkvist L, Wolk A. Physical activity, obesity, and risk of colon and rectal cancer in a cohort of Swedish men. Eur J Cancer. 2006;42:2590–2597. doi: 10.1016/j.ejca.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Pennington JAT. Bowes and Church’s food values of portions commonly used. 15 ed. New York: Harper & Row; 1989. [Google Scholar]
- 9.Bergström L, Kylberg E, Hagman U, Erikson H, Bruce Å. The food composition database KOST: the National Administration’s information system for nutritive values of food. Vår Föda. 1991;43:439–447. [Google Scholar]
- 10.The Nation Board of Health and Welfare. The Swedish Hospital Discharge Registry 1964’2003. Stockholm: 2005. [Google Scholar]
- 11.Ingelsson E, Arnlov J, Sundstrom J, Lind L. The validity of a diagnosis of heart failure in a hospital discharge register. Eur J Heart Fail. 2005;7:787–791. doi: 10.1016/j.ejheart.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Schafer JL. Analysis of incomplete multivariate data. Boca Raton: CRC Press; 1997. [Google Scholar]
- 13.Collett D. Modelling survival data in medical research. 2 ed. Boca Raton: Chapman & Hall/CRC; 2003. [Google Scholar]
- 14.Dauchet L, Kesse-Guyot E, Czernichow S, Bertrais S, Estaquio C, Peneau S, Vergnaud AC, Chat-Yung S, Castetbon K, Deschamps V, Brindel P, Hercberg S. Dietary patterns and blood pressure change over 5-y follow-up in the Su.Vi.Max cohort. Am J Clin Nutr. 2007;85:1650–1656. doi: 10.1093/ajcn/85.6.1650. [DOI] [PubMed] [Google Scholar]
- 15.Obarzanek E, Vollmer WM, Lin PH, Cooper LS, Young DR, Ard JD, Stevens VJ, Simons-Morton DG, Svetkey LP, Harsha DW, Elmer PJ, Appel LJ. Effects of individual components of multiple behavior changes: The PREMIER trial. Am J Health Behav. 2007;31:545–560. doi: 10.5555/ajhb.2007.31.5.545. [DOI] [PubMed] [Google Scholar]
- 16.Mellen PB, Gao SK, Vitolins MZ, Goff DC., Jr Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988–1994 and 1999–2004. Arch Intern Med. 2008;168:308–314. doi: 10.1001/archinternmed.2007.119. [DOI] [PubMed] [Google Scholar]
- 17.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH collaborative research group. New Engl J Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 18.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, 3rd, Simons-Morton DG, Karanja N, Lin PH. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-sodium collaborative research group. New Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 19.Obarzanek E, Sacks FM, Vollmer WM, Bray GA, Miller ER, 3rd, Lin PH, Karanja NM, Most-Windhauser MM, Moore TJ, Swain JF, Bales CW, Proschan MA. Effects on blood lipids of a blood pressure-lowering diet: The Dietary Approaches to Stop Hypertension (DASH) trial. Am J Clin Nutr. 2001;74:80–89. doi: 10.1093/ajcn/74.1.80. [DOI] [PubMed] [Google Scholar]
- 20.Haider AW, Larson MG, Franklin SS, Levy D. Systolic blood pressure, diastolic blood pressure, and pulse pressure as predictors of risk for congestive heart failure in the Framingham Heart Study. Ann Intern Med. 2003;138:10–16. doi: 10.7326/0003-4819-138-1-200301070-00006. [DOI] [PubMed] [Google Scholar]
- 21s.Konhilas JP, Leinwand LA. The effects of biological sex and diet on the development of heart failure. Circulation. 2007;116:2747–2759. doi: 10.1161/CIRCULATIONAHA.106.672006. [DOI] [PubMed] [Google Scholar]
- 22.Most MM. Estimated phytochemical content of the Dietary Approaches to Stop Hypertension (DASH) diet is higher than in the control study diet. J Am Diet Assoc. 2004;104:1725–1727. doi: 10.1016/j.jada.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Lopes HF, Martin KL, Nashar K, Morrow JD, Goodfriend TL, Egan BM. DASH diet lowers blood pressure and lipid-induced oxidative stress in obesity. Hypertension. 2003;41:422–430. doi: 10.1161/01.HYP.0000053450.19998.11. [DOI] [PubMed] [Google Scholar]
- 24.Chess DJ, Stanley WC. Role of diet and fuel overabundance in the development and progression of heart failure. Cardiovasc Res. 2008;79:269–278. doi: 10.1093/cvr/cvn074. [DOI] [PubMed] [Google Scholar]
- 25.McCullough PA, Philbin EF, Spertus JA, Kaatz S, Sandberg KR, Weaver WD. Confirmation of a heart failure epidemic: Findings from the resource utilization among congestive heart failure (REACH) study. J Am Coll Cardiol. 2002;39:60–69. doi: 10.1016/s0735-1097(01)01700-4. [DOI] [PubMed] [Google Scholar]
- 26.Larsson SC, Hakansson N, Naslund I, Bergkvist L, Wolk A. Fruit and vegetable consumption in relation to pancreatic cancer risk: A prospective study. Cancer Epidemiol Biomarkers Prev. 2006;15:301–305. doi: 10.1158/1055-9965.EPI-05-0696. [DOI] [PubMed] [Google Scholar]
- 27.Larsson SC, Giovannucci E, Bergkvist L, Wolk A. Whole grain consumption and risk of colorectal cancer: A population-based cohort of 60,000 women. Br J Cancer. 2005;92:1803–1807. doi: 10.1038/sj.bjc.6602543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Larsson SC, Bergkvist L, Wolk A. Milk and lactose intakes and ovarian cancer risk in the Swedish Mammography Cohort. Am J Clin Nutr. 2004;80:1353–1357. doi: 10.1093/ajcn/80.5.1353. [DOI] [PubMed] [Google Scholar]
- 29.Larsson SC, Bergkvist L, Wolk A. Consumption of sugar and sugar-sweetened foods and the risk of pancreatic cancer in a prospective study. Am J Clin Nutr. 2006;84:1171–1176. doi: 10.1093/ajcn/84.5.1171. [DOI] [PubMed] [Google Scholar]