Abstract
In a study of spousal support for smoking cessation, 34 couples in which one partner continued to smoke despite having a heart or lung problem used an adaptation of Cohen & Lichtenstein’s (1990) Partner Interaction Questionnaire to describe the spouse’s attempts to help the primary (ill) smoker quit. Female smokers received less support for quitting from their spouse or partner than male smokers did, regardless of whether the support was positive or negative, whether the partner also smoked, or whether the smoker or partner rated the partner’s support behavior Female patients in a treatment sub-sample were also less likely than men to achieve stable 1-year cessation if the couple had rated partner support at baseline as coercive or unhelpful. Given known gender differences in relapse risk, cessation interventions for health-compromised female smokers might profitably include partners in addition to the smokers themselves.
Introduction
On average, adult women who smoke appear to have more difficulty quitting and staying abstinent than men. Broad-based evidence for this generalization comes from epidemiological surveys (e.g., Escobedo & Peddicord, 1996), large-scale community intervention trials (e.g., Bjornson et al., 1995), and clinical studies of smokers seeking treatment (e.g., Wetter, Fiore et al., 1999). At the same time, efforts to identify mediating mechanisms that explain this gender difference, or moderator variables that consistently define differential relapse risk for men and women, have not been particularly successful. In fact, nearly a decade ago, Wetter, Kenford et al., (1999) cited “a compelling need for additional research specifically aimed at elucidating the relation between gender and abstinence” (p. 555), and perusal of more recent literature gives little reason to conclude that this need has been fulfilled.
Curiously, attempts to explain the gender difference in quit rates have focused almost exclusively on processes occurring within the individual smoker. For example, one line of research emphasizes gender differences in the biochemical mechanisms underlying nicotine dependence and withdrawal (Perkins, 1996; Perkins, Jacobs, Sanders, & Caggiula, 2002), and another builds on evidence that gender and (un)successful quitting both correlate with depression and other forms of negative emotional experience (Borrelli, Bock, King, Pinto, & Marcus, 1996). While such intrapersonal avenues of inquiry may ultimately prove illuminating, an alternative view, grounded jointly in family-systems theory, research on partner support for quitting, and gender differences in the health consequences of marital quality, would shift inquiry outward, toward the interpersonal context in which smoking occurs (Rohrbaugh et al., 2001; Shoham, Rohrbaugh, Trost, & Muramoto, 2006). Guiding assumptions of this view are (a) that the smoker’s marital and family relationships play a key role in whether he or she continues to smoke, and (b) that the quality of those relationships is likely to have greater consequence for women who smoke than for men.
Research on the intimate social context of smoking actually provides some of the most consistent findings in the cessation literature. For example, having a spouse or partner who smokes is a major risk factor for continued smoking and failure in future quit attempts (Ferguson, Bauld, Chesterman, & Judge, 2005; Homish & Leonard, 2005; Murray, Johnston, Dolce, Lee, & O’Hara, 1995). In addition, at least a dozen studies suggest that positive partner support behaviors such as expressing confidence in a smoker’s ability to quit or offering compliments for not smoking facilitate successful cessation, while negative support such as nagging or criticism impedes it (e.g., Cohen et al., 1988; Coppoteli & Orleans, 1985; Roski, Schmid, & Lando, 1996). Although attempts to base interventions on the findings from naturalistic social support studies have had consistently disappointing results (Park, Schultz, Tudiver, Campbell, 2004; McBride et al., 2004), it may be too soon to foreclose on the possibility of effective couple- or family-focused interventions for health-compromised smokers—perhaps especially for the women who need them most (Rohrbaugh et al., 2001; Shoham et al., 2006).
Research is less clear on the role gender plays in associations between partner support and successful quitting. On one hand, several community trials suggest that men benefit more than women do from simply having a partner participate in an intervention program (Murray et al., 1995; Pirie, Rooney, Pechacek, Lando, & Schmid, 1997). This parallels “social integration” research indicating that being married tends to benefit the health and survival of men more than women (House, Landis, & Umberson, 1988). At the same time, there is growing evidence that the quality of close relations, given that a close relationship exists, is generally more crucial to the health of women than men (Kiecolt-Glaser & Newton, 2001; Rohrbaugh, Shoham, & Coyne, 2006; Saxbe, Repetti, & Nishina, 2008). The alcoholism literature, for example, suggests that marital distress is a stronger predictor of relapse for female drinkers than for male drinkers (Connors, Maisto, & Zywiak, 1998; Walitzer & Dearing, 2006). In the smoking literature, women attempting to quit appear more handicapped than men by having a spouse or partner who smokes (Homish & Leonard, 2005). There is also intriguing evidence that female smokers benefit less from a partner’s attempts to influence their smoking (social control) than male smokers do (Westmaas, Wild, & Ferrence, 2002), though it is unclear if this reflects inherent differences in the smokers themselves (Perkins, Gerlach, Vender, Meeker, Hutchinson, 2001), gender differences in influence strategies (Brown & Smith, 1992), or both.
Several conceptual and methodological issues in research on partner “support” are especially relevant to the preliminary work we report here. First, as the quotes around “support” imply, it is evident that some of the partner behaviors under investigation do not always have supportive consequences in the sense of helping the smoker quit. In fact, one of the main implications of this literature is that negative support (e.g., nagging and criticism) tends not only to be ineffective but could also serve to perpetuate the very behavior a partner wants to eliminate. This kind of ironic process, in which a partner’s well-intended but persistent “solutions” to the problem of smoking feed back to keep it going or make it worse, is central to the interpersonal-systems model of smoking maintenance that guides the “family consultation” intervention used in the present study (Rohrbaugh et al., 2001; Shoham et al., 2006). In this framework, the phrase “partner influence attempt” seems descriptively preferable to “partner support,” because the former more readily directs attention to how the smoker responds to what the partner does (and vice versa), leaving open the possibility that the net effect of the interaction could be ironic rather than supportive.
A methodological limitation is that most studies of partners’ attempts to support or influence quitting have assessed this construct only from the perspective of the smoker. Given that inter-spouse agreement in perceptions of marital interaction is typically modest (Christensen, Sullaway, & King, 1983), it is not very clear to what extent the active ingredients of effective support reside in actual partner behavior (about which the partners would presumably agree) or more simply in the smoker’s perception of what the partner does. In a recent study of 394 pregnant smokers where the researchers did obtain ratings of partner support from both the smoker and her husband, a couple-level (summed) partner-support score predicted late-pregnancy cessation, at least for positive support, while individual scores did not (Pollak et al., 2006). Although the two partners’ support ratings in this study correlated significantly with each other, the strength of their association was modest (r = .19 and r =.39 for positive and negative support, respectively). In any case, the Pollak et al. (2006) results highlight the importance of including both providers’ and recipients’ perspectives in studies of how partners attempt to support (or influence) smoking cessation.
A final limitation is that the partner support literature, with a few exceptions (e.g., Westmaas et al., 2002), has barely begun to grapple with questions of gender. For example, the Pollak et al. (2006) project, despite its methodological virtues, provides no information about possible gender differences because all of the smokers were pregnant women. Nor do most other studies that have measured partner support (or influence attempts) naturalistically, even from just the smoker’s perspective. In other words, we know surprisingly little about possible gender differences in either (a) the level(s) or types of support or influence male and female smokers receive from their partners, (b) the perceived or observed effectiveness of that support/influence, or (c) the extent to which a partner’s stance toward smoking predicts successful (stable) quitting outcomes. These questions take on added interest in view of evidence from the broader literature that men and women provide support, and attempt to influence a partner’s health behavior, in fundamentally different ways (Brown & Smith, 1992; Derlega, Barbee, & Winstead, 1994).
The present study examines gender differences in partner support for quitting in a small sample of couples where one partner (the patient) had a health problem compromised by smoking. Some of these patients later chose to participate in a couple-focused intervention program (Shoham et al., 2006), while others did not, and some had a spouse or partner who also smoked, while others did not. Following other investigators, we operationalized partner support and influence attempts with a shortened version of the Partner Interaction Questionnaire (PIQ) (Cohen & Lichtenstein, 1990; cf. Roski et al., 1996), which yields separate scores for positive and negative support, but administered this to both participants rather than just the smoker alone. In addition, to accommodate the possibility of ironic social influence processes, we included a bi-polar item capturing each person’s perception of whether the partner’s net influence attempts made it easier or more difficult for the primary smoker to approach abstinence.
We hypothesized that the patient’s gender would make a difference in the quantity and/or quality of smoking-specific influence attempts she or he received from a spouse or partner, with female partners of male primary smokers offering more total support (more influence attempts) than male partners of female patients. In addition, given tentative evidence that female smokers respond less favorably than male smokers to a partner’s social control attempts (Westmaas et al., 2002), and that male spouses employ more negative or coercive support strategies than female spouses when trying to influence a heart patient’s health behavior (Brown & Smith, 1992), we also expected that participants would perceive partner support for female smokers to be relatively more negative and relatively less effective than would be the case for male patients. A final hypothesis, based on apparent gender differences in links between marital quality and individual health (Kiecolt-Glaser & Newton, 2001), was that predictive associations between partner support and later outcomes of the cessation intervention would be stronger for female primary smokers than for males. Secondary aims were (a) to examine agreement between patients and spouses in rating the partner’s support behavior, and (b) to investigate the partner’s smoking status (in single- vs. dual-smoker couples) as a possible moderator of the hypothesized associations described above.
Methods
Participants
Participants were 34 couples in which one partner (the patient) continued to smoke cigarettes despite having a diagnosed heart or lung problem or at least two documented risk factors (in addition to smoking) for coronary artery disease (e.g., hypertension, diabetes, obesity, high blood cholesterol). Most of the patients were referred by Tucson-area physicians or medical clinics to participate in a preliminary “couples and smoking” assessment project that did not involve intervention, and later for the “family consultation” project that did. All of the patients had smoked at least 10 cigarettes per day on average for the previous 6 months.
The patients included 14 women and 20 men, and in 15 (dual-smoker) couples the patient’s spouse or partner also smoked. There were thus 19 couples where only the patient smoked. All couples were either married (n = 30) or had lived together in an unmarried but committed relationship for at least 2 years (n = 4). All but two – a gay couple with two smokers and a lesbian couple with one – were heterosexual. Demographically, patients and their partners averaged 54.4 (SD = 9.3) and 55.1 (SD = 10.5) years of age, respectively, with a range from 35 to 72. Five of the 68 participants were Mexican American, one was Native American, and the rest were Caucasian. A minority (18% of patients and 24% of spouses) had graduated from college, and 54% were at least partially retired. Couples had been together an average of 21 years (range 2 – 47), and 62% of the participants had been previously married. Although no couple had children living in their household, most (65%) had an adult child in the local area.
In the clinical domain, 20 (59%) of the 34 primary smokers (but none of their partners) had a diagnosed heart or lung problem aggravated by smoking, and all reported multiple unsuccessful prior quit attempts. At the time of initial screening, patients and their smoking partners reported averaging 25.3 (SD = 9.2) and 23.4 (SD = 11.3) cigarettes a day, respectively. On the Fagerstrom Test of Nicotine Dependence, where scores in the 6–7 range indicate “high dependence” (Heatherton, Kozlowski, Frecher, & Fagerstrom, 1991), patients and smoking partners had respective scores of 6.5 (SD = 2.1) and 5.6 (SD = 2.2).
Procedure
As noted above, we recruited health-compromised smokers in two waves. The first 8 couples completed a modified Partner Interaction Questionnaire (PIQ) and provided other health and relationship information as part of a preliminary “Couples and Smoking Assessment Study” (Rohrbaugh et al., 2001) that involved no intervention. The remaining 26 couples came to a similar assessment session signing on for couple-focused “family consultation” aimed at helping at least the patient quit smoking (Shoham et al., 2006). Six couples provided data but did not participate in the smoking-cessation intervention, usually because a partner was reluctant to attend the required sessions, and in one case because the couple separated before treatment began. All 34 couples received monetary compensation for participating in assessments.
For the sub-sample of 20 couples who received the family consultation (FAMCON) intervention, a research assistant assessed the patient’s subsequent smoking status 6 months following the first FAMCON session, and again 12 months following the patient’s initial quit attempt, in separate telephone interviews with the patient and spouse/partner. On average, quit attempts (at least 2 consecutive days of intentional abstinence) occurred about 45 days after the first FAMCON session. For three patients who never met this quit-attempt criterion, the follow-up period began one month after 1 session.
Measures
Partner Support (Influence Attempts)
Using a modified version of the PIQ (Cohen & Lichtenstein, 1990), both the patient and spouse provided independent ratings of behaviors by the partner directed at helping the patient give up cigarettes. In addition, for the 15 dual-smoker couples where the partner also smoked, the patient and partner similarly rated the patient’s efforts to influence the partner’s smoking using the same items. Following previous research with the PIQ (e.g., Roski et al., 1996; Pollak et al., 2006), we analyzed separate scores for positive and negative partner support, each based on a 7-item scale (see Appendix 1), with questions answered in a “How often?” format ranging from 1 = “never” to 7 = “Very often.” Internal consistency was good for both the positive and negative support scales when patients and partners rated both the other person’s support behavior and their own (all alphas > .75).
Two additional single-item scales, also used by both participants and reproduced in Appendix 1, concerned the partner refusing to allow smoking and the overall effectiveness of the partner’s attempts to influence smoking. Although other researchers have sometimes scored the first (refusal) item as negative support, we treated it here as a stand-alone measure because (a) it did not correlate as highly as other negative support items did with the sum of those items, and (b) it seemed to represent a relatively forceful attempt to control smoking that could conceivably play a role in ironic interpersonal-influence processes. Mean scores on this item were 2.6 (SD = 2.2) and 2.5 (SD = 2.3) for patients and their partners, respectively. The second (effectiveness) item, available only for the 26 couples assessed for the FAMCON project, had a bi-polar response scale that permitted defining a partner’s influence attempts as effective at one pole (+5 = “helps me smoke less”) or ironically counterproductive at the other (−5 = “makes me want to smoke more”). Mean scores for patients and partners were −0.3 (SD = 2.4) and −0.8 (SD = 2.2), with 42% and 45%, respectively, rating effectiveness in the negative range (below 0).
Marital Quality and Psychological Distress
Participants also completed questionnaire measures of relationship quality and psychological distress, and we examined these too as potential correlates of partner support for quitting. Couples in this sample were fairly satisfied with their relationships, as reflected in average scores toward the high end of Hendrick’s (1988) Relationship Assessment Scale (Mdn partner score = 4.6 out of 5). Similar positive scores were recorded for Heavey, Larson, Christensen, and Zumtobe’s (1996) Constructive Communication Scale, which correlated highly with the Hendrick measure for both patients (r = .82) and their partners (r = .60). To create a couple-level index of marital quality we averaged the z-scores for both of these measures across both partners.
The last variable examined as a possible covariate of partner support was psychological distress, operationalized via a 25-item version of the Hopkins Symptom Checklist (HSCL-25) (Heshbacher, Downing, & Stephansky, 1978). On this measure, 37% of the patients and 21% of their partners scored in a range associated with a diagnosis of anxiety or depression.
Smoking Cessation Outcome
Assessment of smoking outcomes was based on modified Timeline Follow-back interviews (Sobell & Sobell, 1992), conducted with both the patient and partner, through which it was possible to generate both a dichotomous 30-day point-prevalence abstinence index for the patient’s smoking status at 12 months (40% were abstinent) and a continuous % abstinent days measure for the full 1-year follow-up interval (M = 48%). There was no biochemical verification of smoking outcomes, though collateral reports from the patient’s spouse or partner may lend more credence to the abstinence results than would the patient’s report alone.
Results
Preliminary Analyses
Consistent with Pollak et al. (2006), agreement between patients’ and spouses’ ratings of the partner’s support behavior tended to be better for negative support (r = .69, p < .001) than for positive support (r = .27, p > .1). Inter-rater reliability for the two single-item measures paralleled this pattern, with somewhat better agreement for “refuses to allow smoking in the house” (r = .49, p < .01) than for perceived effectiveness of the partner’s influence attempts (r = .29, p < .10).
In further preliminary analyses, we averaged patient and partner support scores and used these couple-level variables to examine relationships among the support dimensions and to identify demographic and clinical characteristics of the primary smoker (patient) or couple other than gender or partner smoking status that might co-vary with partner support. Interestingly, the joint perceptions of positive and negative support tended to correlate positively with each other (r = .34, p < .10), suggesting that the amount of support a partner provides, regardless of its valence, could be a meaningful dimension of a smoker’s or a couple’s experience. Perceived effectiveness of the partner’s influence attempts, on the other hand, correlated negatively with both negative support (r = −.43, p < .05) and refusal to allow household smoking (r = −.55, p< .05), but only modestly with positive partner support (r = .22).
Neither (individual) patient nor couple characteristics showed much association with reports of partner support for smoking cessation. For example, the patient’s age, education, and level of nicotine addiction, and the duration of the couple’s relationship, correlated negligibly with all four of the support variables. The only statistically significant associations in these exploratory analyses (which themselves could have occurred by chance, given the large number of comparisons we performed) suggest (a) that patients received more positive support when they had a diagnosed heart or lung problem than when they did not (r = .50, p < .01), and (b) that influence and support attempts were less effective for patients who reported relatively more psychological distress (r = −.40, p < .05). Interestingly, the marital-quality composite score did not correlate significantly with any of the partner support variables (maximum r = .27 for effectiveness), which may have implications for the construct validity of cessation-specific support.
Mean-Level Gender Differences
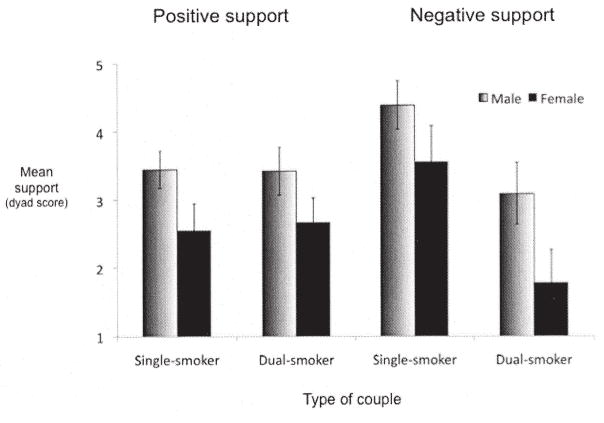
To test the main hypothesis, we performed a mixed-model analysis of variance (ANOVA) on ratings of positive and negative partner support for the patient, using the couple as the unit of analysis. This ANOVA included patient gender (male vs. female) and couple type (single vs. dual-smoker couple) as between-case factors, with valence (positive vs. negative support) and reporter (patient vs. spouse) as within-case variables. A significant main effect of patient gender (F[1, 30] = 8.64, p = .006) indicated that female primary smokers received significantly less total support (both positive and negative) from their partners than males did, regardless of the partner’s smoking status and which spouse was the reporter. The means and standard deviations from this ANOVA, collapsed over reporter (for which there were no significant main or interaction effects), appear in Figure 1. The analysis also revealed a significant main effect for couple-type (F= 5.30, p = .028), with patients in single-smoker couples receiving more total support than those in double-smoker couples, and a significant valence by couple-type interaction (F= 9.98, p = .004), with simple-effect tests indicating a difference between single- and dual-smoker couples in negative support (p < .05) but not positive support. Gender played no role in interaction with either valence or couple type.
Figure 1.
Partner support by patient gender in single and dual-smoker couples.
Supplementary ANOVAs performed on household smoking refusal and influence effectiveness revealed no main effects or interactions involving gender. The only notable finding, consistent with the main ANOVA results, was a significant main effect of couple-type reflecting a greater tendency for partners to disallow smoking in the house when only the patient smoked (F[1,26] = 5.93, p = .02). We also repeated the main ANOVAs without the two homosexual couples and found this had little effect on the results obtained.
Because the analyses reported so far focused only on partner support for the patient’s efforts to quit smoking, we performed a separate ANOVA for the 15 dual-smoker couples, including averaged positive and negative support scores for both the patient and his or her smoking partner. Here patient gender was the sole between-case factor and role (patient vs. partner) was an additional within-case factor. The results revealed a significant main effect of valence (F[1,13] = 6.90, p = .021), with positive support in dual-smoker couples exceeding negative support, and a significant role by patient-gender interaction (F[1,13] = 6.65, p < 023). The latter reflected a significant difference in total support received by male and female patients, with females again on the short end (p < .05), but no gender difference in the amount of support patients provided to their smoking partners. Thus, in this small sample of dual-smoker couples, the female smokers most disadvantaged by lacking partner support for quitting appear to have been those with documented health problems, who arguably needed it most.
Predictors of Cessation Outcome
The last set of analyses, summarized in Table 1, examined the partner influence and support variables as predictors of quit outcomes for male and female patients who participated in the couple-focused FAMCON intervention. Consistent with our third hypothesis, correlations between couple-level measures of baseline partner support and 12-month cessation outcomes suggest larger effect sizes for female primary smokers than for males. Particularly striking is the differential prognostic importance of how helpful and/or coercive a partner’s influence attempts appear to be, though the small sample size limits possibilities for statistically significant gender moderation. Finally, controlling couple-level marital quality did not substantially change the associations between cessation-specific partner-support and quit outcomes.
Table 1.
Predictive Associations Between Pre-Treatment Partner Support and 12-Month Cessation Outocomes
| Male Patients (n = 12) | Female Patients (n = 8) | |||
|---|---|---|---|---|
| Partner support variables | Abstinent at 12 months (past 30 days) | % abstinent days over 12 months | Abstinent at 12 months (past 30 days) | % abstinent days over 12 month |
| Positive support | .30 | .24 | .61† | .66† |
| Negative support | .42 | .43 | −.12 | −.16 |
| Refusal to allow smoking in the house | .39 | .38 | −.67† | −.66† |
| Effectiveness of support and influence attempts | .10 | .16 | .77* | .77* |
Note. Table entries are point-biserial and product-moment correlations between couple-level measures of partner support before treatment and smoking cessation outcomes 12 months after the patient’s initial quit attempt.
p < .10,
p < .05 (two-tail tests).
Discussion
The results of this small study highlight the likely importance of gender differences in partner support for smoking cessation. Women who continued to smoke despite having health problems received less support for quitting from their spouse or partner than male smokers did, regardless of whether the support was positive or negative, whether the partner also smoked, or whether it was the smoker or partner who rated the partner’s support behavior. At the same time, the quality of partner support smokers did receive appeared to predict later quit success more for women than for men, particularly if the support was negative or seen by the patient and partner as unhelpful. These findings are consistent with a broader literature linking gender, relationships, and health—specifically, with evidence that women are generally more oriented to relationships than men (Taylor, 2006), that male and female partners give each other support in fundamentally different ways (Brown & Smith, 1992), and that associations between marital quality and health tend to be stronger for women than for men (Kiecolt-Glaser & Newton, 2001; Rohrbaugh et al., 2006; Saxbe et al., 2008). Still, it is important to acknowledge that many of the key sex differences in the study (e.g., moderating effects of gender on association between partner support and later cessation) were not significant statistically, so drawing conclusions from these data about gender differences in partner quit support would be premature at best.
Methodologically, the results support Pollak et al.’s (2006) recommendation that attempts to measure partner support behavior take into account the perceptions of both the smoker and partner, as this appears to improve prediction of quit outcomes. Like Pollak et al., we found better inter-spouse agreement in reports of positive rather than negative partner influence attempts, highlighting the advisability of having both participants’ perspectives on the latter. There was also rather modest inter-partner agreement about how helpful or effective the partner’s influence attempts were, even though the partners’ combined effectiveness rating was a good predictor of cessation success. Because the unspecified temporal frame of our modified PIQ questions (i.e., asking what one’s partner usually does) probably limits precision of measurement, further work in this area might benefit from repeated (e.g., daily) assessments of various support and influence behaviors overtime. This would permit a more dynamic examination of within-case co-variation between the two partners’ influence/support ratings and their reports of smoking behavior (Affleck, Zautra, Tennen, & Armeli, 1999).
Several broader implications of this study concern the specific nature of partner support for smoking cessation and the (in)adequacy of the term “support” for capturing smoking-relevant interaction between smokers and their partners. For one, the relatively low correlations between general relationship quality and measures of partner support specific to smoking (both negative and positive) may indicate that these constructs are conceptually and empirically distinct. In other words, how a couple interacts around smoking may say little about the quality of their marriage (though one might also argue that the low correlations reflect the rather restricted range of marital quality in our sample of self-selected couples, most of whom clustered toward the high end of the two relationship measures). Second, it is clear from this and other studies that partner behaviors intended to be supportive do not always have supportive consequences. We would thus argue that any useful formulation of smoker-partner interaction must ultimately take into account not only what the partner does, but also what the smoker does in response to that, how the partner responds in turn, and so on. The present study only begins to approach such a cyclical, dyad-level analysis by asking participants about the effectiveness of partner influence attempts. Still, the fact that almost half of the participants rated the helpfulness of these attempts in the negative range of our response scale (i.e., more toward “makes me want to smoke more” than toward “helps me smoke less”) points to the likely relevance of ironic interpersonal processes (Rohrbaugh et al., 2001; Shoham et al., 2006).
This study has important limitations – most notably its small sample size. In particular, having only 15 female patients in the main gender-difference analyses and 8 for predicting cessation outcomes makes it difficult to generalize about the understudied and possibly heterogeneous sub-group of health-compromised female smokers. The fact that we studied only smokers with health problems similarly constrains the generalizability of results. Nor do we know if the possibly predictive role of negative partner support or ironic processes would hold for female smokers not participating in a couple-focused intervention like FAMCON. Interestingly, this intervention attempted to change the very ironic support patterns that predicted poor outcome for women, and if this in fact happened, the impact was apparently not sufficient to neutralize the negative prognostic significance of pre-treatment couple relationship patterns.
On the positive side, our FAMCON intervention appears well-suited to female smokers. Although gender differences in outcome fell short of statistical significance, virtually all cessation, health, and client satisfaction indices were in the direction of better outcomes for women than men (Shoham et al., 2006). This could reflect the fact that FAMCON, more than most other cessation interventions, explicitly takes relationship dynamics into account.
In summary, women who smoke in the face of health problems appear to receive less support for cessation from their partners than male smokers do, but appear to need it more. Given known gender differences in relapse risk, cessation interventions for health-compromised female smokers might profitably include partners in addition to the smokers themselves.
Acknowledgments
This research was supported by awards R21-DA13121, R01 DA017539, and U10-DA15815 from the National Institute on Drug Abuse. The authors presented some of the results at meetings of the College of Problems of Drug Dependence (Quebec City, June 2007) and the American Psychological Association (San Francisco, August 2007).
We thank Sarah Trost, Myra Muramoto, Rodney Cate, Scott Leischow, Lisa Hoffman-Konn, Mary-Frances O’Connor, Mari Sol D’Urso, and Donald Miretsky for their contributions to the project.
Biographies
Michael J. Rohrbaugh, Ph.D., is Professor of Psychology and Family Studies/Human Development and Director of the Psychology Department Clinic at the University of Arizona. His research focuses on social factors in the maintenance and treatment of health problems and addictions.
Varda Shoham, Ph.D., is Professor of Psychology and Director of Clinical Training at the University of Arizona. She studies individual, couple, and family treatments for change-resistant clients who engage in health-compromising behavior such as smoking and substance abuse. Her research has been continuously funded by NIDA, NIMH, and NIAAA since 1991.
Catherine L. Dempsey, Ph.D., is a Research associate in the Family Research Laboratory at the University of Arizona and a postdoctoral (respecialization) fellow in the clinical psychology program. Her research concerns addictions, PTSD, and social relationships among diverse populations.
Appendix 1. Modified Partner Influence Questionnaire (PIQ) Scales: Smoker Form*
How often does your partner…
Positive support:
1. Compliment you on not smoking.
2. Help you think of substitutes for smoking.
3. Help to calm you down when you are feeling stressed or irritable.
4. Express confidence in your ability to quit.
-
5. Participate in an activity with you that keeps you from smoking (e.g., going for a walk instead of smoking).
Negative support:
6. Ask you to quit smoking
7. Comment that smoking is a dirty habit.
8. Comment that the house smells of smoke.
9. Mention being bothered by smoke.
-
10. Refuse to clean up your cigarette butts.
Refusal:
-
11. Refuse to let you smoke in the house).
Support effectiveness:
-
12. To what extent are your partner’s attempts to influence your smoking successful?
−5 −4 −3 −2 −1 0 +1 +2 +3 +4 +5 not at all; makes me want to smoke more makes no difference very successful; helps me to smoke less * Items 1–11 answered on 7-point scales ranging from 1 = “never” 7 = “very often.” Partner form uses alternative wordings (e.g., “How often do you…compliment your partner on not smoking?”).
Source: Cohen and Lichtenstein (1990)
References
- Affleck G, Zautra A, Tennen H, Armeli S. Multilevel daily process designs for consulting and clinical psychology: A preface for the perplexed. Journal of Consulting and Clinical Psychology. 1999;67:746–754. doi: 10.1037//0022-006x.67.5.746. [DOI] [PubMed] [Google Scholar]
- Bjornson W, Rand C, Connett JE, Lindgren P, Nides M, Pope F. Gender differences in smoking cessation after 3 years in the lung health study. American Journal of Public Health. 1995;85:223–230. doi: 10.2105/ajph.85.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrelli B, Bock B, King T, Pinto B, Marcus BH. The impact of depression on smoking cessation in women. American Journal of Preventive Medicine. 1996;12:378–387. [PubMed] [Google Scholar]
- Brown PC, Smith TW. Social influence, marriage, and the heart: Cardiovascular consequences of interpersonal control in husbands and wives. Health Psychology. 1992;11:88–96. doi: 10.1037//0278-6133.11.2.88. [DOI] [PubMed] [Google Scholar]
- Christensen A, Sullaway M, King C. Systematic error in behavioral reports of dyadic interaction: Egocentric bias and content effects. Behavioral Assessment. 1983;5:129–140. [Google Scholar]
- Cohen S, Lichtenstein E. Partner behaviors that support quitting smoking. Journal of Consulting and Clinical Psychology. 1990;58:304–309. doi: 10.1037//0022-006x.58.3.304. [DOI] [PubMed] [Google Scholar]
- Cohen S, Lichtenstein E, Mermelstein R, Kingsolver K, Baer JS, Kamarck TW. Social support interventions for smoking cessation. In: Gottleib BH, editor. Marshalling social support: Formats, processes, and effects. New York: Sage; 1988. [Google Scholar]
- Connors GJ, Maisto SA, Zywiak WH. Male and female alcoholics’ attributions regarding the onset and termination of relapses and the maintenance of abstinence. Journal of Substance Abuse. 1998;10:27–42. doi: 10.1016/s0899-3289(99)80138-2. [DOI] [PubMed] [Google Scholar]
- Coppotelli HC, Orleans CT. Partner support and other determinants of smoking cessation maintenance among women. Journal of Consulting and Clinical Psychology. 1985;53:455–460. doi: 10.1037//0022-006x.53.4.455. [DOI] [PubMed] [Google Scholar]
- Derlega VJ, Barbee AP, Winstead BA. Friendship, gender, and social support: Laboratory studies of social interaction. In: Burleson BR, Albrecht TL, Sarason IG, editors. The communication of social support: Message, interactions, relationships, and community. Newbury Park, CA: Sage; 1994. pp. 136–151. [Google Scholar]
- Escobedo LG, Peddicord JP. Smoking prevalence in U.S. birth cohorts: The influence of gender and education. American Journal of Public Health. 1996;86:231–236. doi: 10.2105/ajph.86.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson J, Bauld L, Chesterman J, Judge K. The English smoking treatment services: One year outcomes. Addiction. 2005;100:59–69. doi: 10.1111/j.1360-0443.2005.01028.x. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecher RC, Fagerstrom K. The Fagerstrom Test for Nicotine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Heavey CL, Larson B, Christensen A, Zumtobel DC. The Communication Patterns Questionnaire: The reliability and validity of a constructive communication subscale. Journal of Marriage and the Family. 1996;58:796–800. [Google Scholar]
- Hendrick SS. A generic measure of relationship satisfaction. Journal of Marriage and the Family. 1988;15:93–98. [Google Scholar]
- Heshbacher PK, Downing RW, Stephansky P. Assessment of psychiatric illness severity by family physicians. Social Science and Medicine. 1978;12:45–52. [Google Scholar]
- Homish GG, Leonard KE. Spousal influence on smoking behaviors in a US community sample of newly married couples. Social Science and Medicine. 2005;61:2557–2567. doi: 10.1016/j.socscimed.2005.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- McBride CM, Baucom DH, Peterson BL, Pollak KI, Palmer C, Westman E, Lyna P. Prenatal and postpartum smoking abstinence: A partner-assisted approach. American Journal of Preventive Medicine. 2004;27:232–238. doi: 10.1016/j.amepre.2004.06.005. [DOI] [PubMed] [Google Scholar]
- Murray RP, Johnston JJ, Dolce JJ, Lee WW, O’Hara P. Social support for smoking cessation and abstinence: The Lung Health Study. Addictive Behaviors. 1995;20:159–170. doi: 10.1016/s0306-4603(99)80001-x. [DOI] [PubMed] [Google Scholar]
- Park E, Tudiver F, Schultz JK, Campbell T. Does enhancing partner support and interaction improve smoking cessation? A meta-analysis. Annals of Family Medicine. 2004;2:170–174. doi: 10.1370/afm.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins KA. Sex differences in nicotine versus non-nicotine reinforcement as determinants of tobacco smoking. Experimental and Clinical Psychopharmacology. 1996;4:1–12. [Google Scholar]
- Perkins KA, Gerlach D, Vender J, Meeker J, Hutchinson S. Sex differences in the subjective and reinforcing effects of visual and olfactory cigarette smoke stimuli. Nicotine and Tobacco Research. 2001;3:141–150. doi: 10.1080/14622200110043059. [DOI] [PubMed] [Google Scholar]
- Perkins KA, Jacobs L, Sanders M, Caggiula AR. Sex differences in the subjective and reinforcing effects of cigarette nicotine dose. Psychopharmacology. 2002;163(2):94–201. doi: 10.1007/s00213-002-1168-1. [DOI] [PubMed] [Google Scholar]
- Pirie PL, Rooney BL, Pechacek TF, Lando HA, Schmid LA. Incorporating social support into a community-wide smoking cessation contest. Addictive Behaviors. 1997;22:131–137. doi: 10.1016/0306-4603(95)00106-9. [DOI] [PubMed] [Google Scholar]
- Pollak KL, Baucom DH, Palmer CA, Peterson BL, Ostbye T, Stanton S. Couples reports of support for smoking cessation predicting women’s late pregnancy cessation. American Journal of Health Promotion. 2006;21(2):90–96. doi: 10.4278/0890-1171-21.2.90. [DOI] [PubMed] [Google Scholar]
- Rohrbaugh MJ, Shoham V, Coyne JC. Effects of marital quality on 8-year survival of patients with heart failure. American Journal of Cardiology. 2006;98:1069–1072. doi: 10.1016/j.amjcard.2006.05.034. [DOI] [PubMed] [Google Scholar]
- Rohrbaugh MJ, Shoham V, Trost S, Muramoto M, Cate R, Leischow S. Couple-dynamics of change resistant smoking: Toward a family-consultation model. Family Process. 2001;40:15–31. doi: 10.1111/j.1545-5300.2001.4010100015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roski J, Schmid LA, Lando HA. Long-term associations of helpful and harmful spousal behaviors with smoking cessation. Addictive Behaviors. 1996;21:173–185. doi: 10.1016/0306-4603(95)00047-x. [DOI] [PubMed] [Google Scholar]
- Saxbe DE, Repetti RL, Nishina A. Marital satisfaction, recovery from work, and diurnal cortisol among men and women. Health Psychology. 2008;27:15–25. doi: 10.1037/0278-6133.27.1.15. [DOI] [PubMed] [Google Scholar]
- Shoham V, Rohrbaugh MJ, Trost SE, Muramoto M. A family consultation intervention for health-compromised smokers. Journal of Substance Abuse Treatment. 2006;31:395–402. doi: 10.1016/j.jsat.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Taylor SE. Tend and befriend: Biobehavioral bases of affiliation under stress. Current Directions in Psychological Science. 2006;15:273–277. [Google Scholar]
- Walitzer KS, Dearing RL. Gender differences in alcohol and substance abuse relapse. Clinical Psychology Review. 2006;26:128–148. doi: 10.1016/j.cpr.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Westmaas JL, Wild TC, Ferrence R. Effects of gender in social control of smoking cessation. Health Psychology. 2002;21:368–376. doi: 10.1037//0278-6133.21.4.368. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Fiore MC, Young TB, McClure JB, de Moor CA, Baker TB. Gender differences in response to nicotine replacement therapy: Objective and subjective indexes of tobacco withdrawal. Experimental and Clinical Psychopharmacology. 1999;7:135–144. doi: 10.1037//1064-1297.7.2.135. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Kenford SL, Smith SS, Fiore MC, Jorenby DE, Baker TB. Gender differences in smoking cessation. Journal of Consulting and Clinical Psychology. 1999;67:555–562. doi: 10.1037//0022-006x.67.4.555. [DOI] [PubMed] [Google Scholar]