Abstract
Context:
To our knowledge, no one has compared the prepractice hydration status of male and female National Collegiate Athletic Association (NCAA) Division I athletes or has studied the effects of the menstrual cycle phase on women's prepractice hydration status.
Objective:
To report prepractice hydration status of collegiate athletes and determine the factors that might influence that status.
Design:
Cross-sectional, descriptive study.
Setting:
University sports team practices.
Patients or Other Participants:
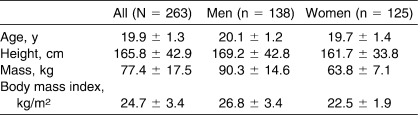
Participants included 138 male and 125 female athletes (age = 19.9 ± 1.3 years, height = 165.8 ± 42.9 cm, mass = 77.4 ± 17.5 kg) from an NCAA Division I New England university.
Intervention(s):
One spontaneously voided (spot) urine sample was collected from each participant before his or her team practice and was measured 2 times.
Main Outcome Measure(s):
A refractometer was used to analyze the amount of light that passed through a small drop of urine and assess urine specific gravity. Fluid intake and menstrual history for women were also collected. Three hydration-status groups were defined based on the American College of Sports Medicine and National Athletic Trainers' Association criteria: (1) euhydrated, which was urine specific gravity less than 1.020; (2) hypohydrated, from 1.020 to 1.029; and (3) significantly hypohydrated, equal to or more than 1.030.
Results:
Thirteen percent of student-athletes appeared significantly hypohydrated, with a mean urine specific gravity of 1.031 ± 0.002 (χ2 = 12.12, P < .05); 53% appeared hypohydrated, with a mean urine specific gravity of 1.024 ± 0.003 (χ2 = 12.12, P < .05); and 34% appeared euhydrated, with a mean urine specific gravity of 1.012 ± 0.005 (χ2 = 0.03, P > .05). A greater percentage of men (47%) than women (28%) were hypohydrated (χ2 = 8.33, P < .05). In women, no difference was evident between the luteal and follicular phases of their menstrual cycles (χ2 = 0.02, P > .05).
Conclusions:
Before activity, athletes were hypohydrated at different levels. A greater percentage of men than women were hypohydrated. Menstrual cycle phase did not appear to affect hydration in women.
Keywords: dehydration, sex, hypohydration, refractometer, sports, urine specific gravity
Key Points
National Collegiate Athletic Association Division I athletes need to be educated about proper hydration techniques to prevent hypohydration and protect athletic performance or need to be encouraged to properly hydrate before practices.
More men than women appeared to be hypohydrated before practice.
Hydration status did not differ with different phases of the menstrual cycle, but confirmation of this finding is needed through comparison of urine specific gravity or plasma osmolarity within the same athletes at different times in their menstrual cycles.
Dehydration is defined as a dynamic loss of body water or the transition from euhydration to hypohydration. Euhydration is defined as normal body-water content, and hypohydration is a body-water deficit.1 During exercise, hypohydration is associated with an increase in core body temperature and cardiovascular strain and a decrease in stroke volume and serum sodium levels.2,3 These imbalances can increase the risk of heat syncope, heat exhaustion, and, most seriously, heat stroke.1 Proper hydration and fluid replacement are essential for enabling competitive athletes to perform optimally, have uncompromised future exercise sessions, and maintain overall health.
For athletes competing in team sports, appropriate hydration is an important but often overlooked aspect of proper training and competition.4 Burke and Hawley4 stated that hydration guidelines applied to team sports are often prepared based on sports such as distance running. Team sports require athletes to switch intermittently between maximal-effort and low-intensity exercise, potentially causing large losses of body water; therefore, hydration in team sports needs to be studied.4 Nichols et al5 examined the knowledge and behaviors of hydration and fluid replacement in collegiate athletes and determined that they were not properly educated about appropriate hydration for practice and competition.
Despite ongoing efforts to educate athletes about the harmful effects of dehydration, some athletes still commonly begin practice or competition (or both) in a hypohydrated condition, increasing the risk of developing severe dehydration.6 Hypohydration of 2% to 3% of body mass can compromise exercise performance, heat dissipation, and cardiovascular function.7 Collegiate athletes are a population at increased risk for hypohydration because of the frequency and intensity of their exercise bouts.8 In addition, sex-related differences in hydration status might exist.9 In women, threshold temperature for the onset of thermoregulatory responses, such as sweating, is increased during the luteal phase9,10; thus, hydration status should be observed in the same phase of the menstrual cycle.
To date, little research has been reported on the hydration status of National Collegiate Athletic Association (NCAA) Division I athletes. Investigators have induced dehydration in athletes or observed hydration status during specific sport practices, but they have not performed a cross-sectional assessment of prepractice hydration status of collegiate athletes in general.11 To our knowledge, a cross-sectional, descriptive study in which prepractice hydration status is compared between male and female NCAA Division I collegiate athletes does not exist. Furthermore, a cross-sectional study of the effects of the menstrual cycle phase on women's prepractice hydration status has not been conducted. Therefore, the purpose of our study was to determine the prepractice hydration status of NCAA Division I athletes from a variety of sport teams. In addition, we wanted (1) to compare the prepractice hydration status of male and female collegiate athletes and (2) to examine differences in the prepractice hydration status of female collegiate athletes in the follicular and luteal phases of menstruation.5
METHODS
Participants
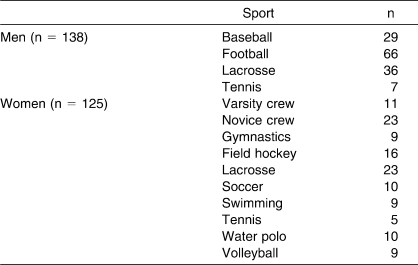
The athletes who participated in our study were from an NCAA Division I university in New England. First, we requested permission from the coaches of all the collegiate sport teams to recruit student-athletes. Second, we invited varsity student-athletes from teams either in-season or in the conditioning period to participate. A total of 263 student-athletes (138 men, 125 women; age range, 18–23 years) were recruited from 14 different sports (4 men's sports, 10 women's sports), representing approximately 65% of student-athletes from 23 sport teams (Tables 1 and 2). Of the participants, 29.2% were freshmen (n = 77), 24.7% were sophomores (n = 65), 24.0% were juniors (n = 63); 13.7% were seniors (n = 36); and 8.4% (n = 22) did not state their academic years. All student-athletes provided written informed consent, and the study was approved by the university's institutional review board.
Table 1.
Participant Demographics
Table 2.
Collegiate Team Sports Represented in the Sample
Procedures
Urine Specific Gravity
For each participant, 1 spontaneously voided (spot) urine sample was collected in a urine specimen cup before team practice and was analyzed for specific gravity using a handheld refractometer (model A300CL; Spartan, Tokyo, Japan) within 1 hour of specimen collection. The refractometer was calibrated before each analysis using distilled water. Most of these prepractice urine collections were conducted approximately 1 hour before practice; most practices began about 4:00 pm, but some practices began about 5:30 am. A drop of urine was placed onto the refractometer using a disposable, mineral-free pipette, and 1 researcher (K.A.P.) read and recorded the corresponding specific gravity. All measurements were conducted in duplicate, and the average urine specific gravity was used for the final assessment for each athlete.
Urine collection was conducted over 9 months because of the timing of appointments with coaches and teams and because we wanted to ensure that we were not disrupting practice time. Although the participants knew the purpose of the study, they were not told the details of the study before data collection, so it is unlikely they changed their hydration practices before data collection. We were able to recruit 14 sport teams because we explained that the data would be used to inform the coaches and student-athletes of the student-athletes' hydration status and to teach them how to properly hydrate for improved sport performance.
Three hydration-status groups were defined based on urine specific gravity, which has been found to be valid and reliable.12,13 Euhydrated was defined as urine specific gravity less than 1.020; hypohydrated, from 1.020 to 1.029; and significantly hypohydrated, equal to or more than 1.030. These hydration-status groups were based on those most recently established by the American College of Sports Medicine12 and the National Athletic Trainers' Association.13
Urine specific gravity was used as the mode of evaluation because it is a simple, validated measure to use in the field. Drawing blood from all participants would not have been feasible because of the number of athletes and expense of analyzing for plasma osmolarity.7
Although Popowski et al14 stated, “urinary measurements (urine specific gravity and urine osmolarity) are sensitive to changes in hydration status during acute dehydration …,” our study was cross-sectional, and urine was not collected as the first morning void. Many investigators believe that the first morning void is more representative of hydration status; however, the validity of the first morning void has been debated.15 Our study was conducted to provide a general indication of hydration status of collegiate athletes before practice and to lead to future research in this population. Nonetheless, the advantages of urine specific gravity are that it is easy to use in the field, rapid, and inexpensive. In addition, Stuempfle and Drury16 stated, “Only the refractometer should be used to determine urine specific gravity in collegiate wrestlers during the weight-certification process.” Furthermore, with respect to a sport such as wrestling, urine specific gravity is not always assessed using the morning void.
However, a disadvantage of our mode of collection is that urine specific gravity does not assess acute dehydration as well as plasma osmolarity does. A disadvantage of not collecting the first morning void is that a first morning urine sample is considered a more accurate indicator of hydration status because food and beverage consumption and sweat and urinary losses throughout the day and during exercise can affect true hydration status.17
Fluid Intake
We developed a fluid consumption questionnaire and administered it to the student-athletes (Table 3). Questions included items relating to the intake of caffeine and alcohol.8 The student-athletes were given specific instructions about how to properly complete the questionnaire. In addition, we provided an example of 8 fl oz (240 mL) because we instructed them to provide the amount of fluids consumed in fluid ounces. They also were instructed to answer as honestly as possible and to ask for clarification of any question, if needed. The same researcher (K.A.P.) administered the questionnaire and was present while the student-athletes completed it; however, interactions between the researcher and student-athletes were limited. Thus, it should be assumed that the student-athletes answered all questions honestly because the researcher did not influence them. The researcher also checked for completeness of the questionnaire after each student-athlete completed it.
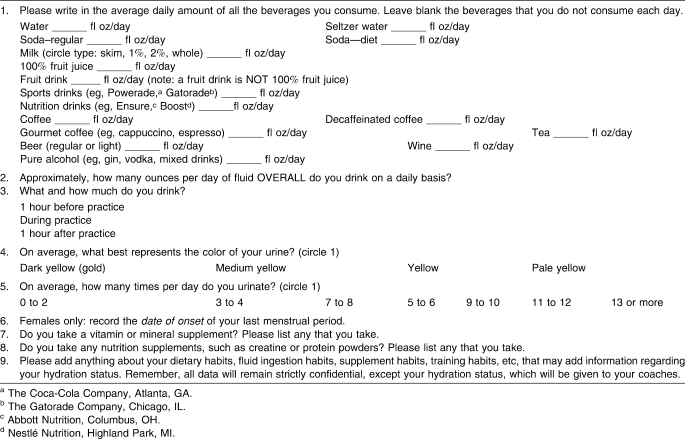
Table 3.
Fluid Intake Questionnaire
Menstrual History
On the questionnaire, each female student-athlete was instructed to report the date of onset of her last menstrual period, so we could determine whether she was in the follicular or luteal phase of her menstrual cycle (Table 3).
Body Mass and Height
All participants self-reported body mass and height. We calculated body mass index (kg/m2) from these measures. Although we are aware of the potential inaccuracies of self-reported body mass and height, our goal was to assess hydration status. Furthermore, the time allotted for data collection (ie, prepractice) was limited to completion of the questionnaire and urine collection.
Statistical Analyses
Statistical analyses were conducted using SPSS (version 9.0 for Windows; SPSS Inc, Chicago, IL) and Minitab (Release 13; Minitab Inc, State College, PA). A χ2 analysis was used (1) to determine the prevalence of hypohydration in collegiate athletes, (2) to compare the prepractice hydration status of male and female collegiate athletes, and (3) to examine differences in the prepractice hydration status of female collegiate athletes in the follicular and luteal phases of menstruation. We used 2-tailed, independent-samples t tests to compare differences between time of day that urine samples were collected and class level of the student-athletes (ie, freshman, sophomore, junior, senior). Descriptive statistics were calculated for demographic purposes. The α level was set a priori at .05.
RESULTS
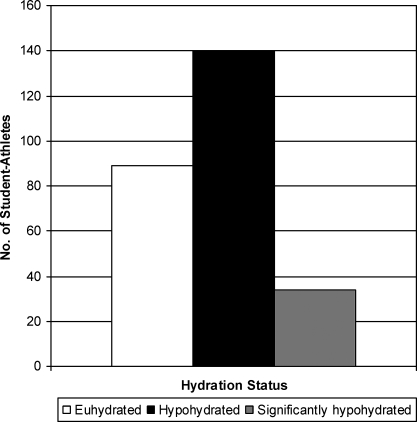
Overall, 66% (n = 174) of the collegiate athletes tested manifested a urine specific gravity that was equal to or more than 1.020, indicating the probability of prepractice hypohydration (Figure). Chi-square analysis indicated that 13% (n = 34) of student-athletes appeared significantly hypohydrated (mean urine specific gravity = 1.031 ± 0.002; χ2 = 12.12, P < .05), 53% (n = 140) appeared hypohydrated (mean urine specific gravity = 1.024 ± 0.003; χ2 = 12.12, P < .05), and 34% (n = 89) appeared euhydrated (mean urine specific gravity = 1.012 ± 0.005; χ2 = 0.03, P > .05). A greater percentage of men (47%) were hypohydrated than women (28%) (χ2 = 8.33, P < .05). In women, no difference was evident between the luteal and follicular phases of their menstrual cycles (χ2 = 0.02, P > .05).
Figure.
Prepractice hydration status of collegiate athletes. Euhydrated indicates a urine specific gravity of less than 1.020; hypohydrated, from 1.020 to 1.029; and significantly hypohydrated, more than or equal to 1.030.
We found no difference between the hydration status of athletes whose urine samples were collected in the morning (at approximately 5:30 am) and that of athletes whose urine samples were collected in the afternoon (at about 4:00 pm) (P > .05). We also found no difference in hydration status between juniors and seniors versus freshmen and sophomores (1.02 ± 0.01 for each class level; P > .05). However, comparisons can be drawn between male-reported and female-reported fluid intake. Female athletes reported drinking an average of 53 fl oz (1590 mL) of water, whereas male athletes reported drinking 51 fl oz (1530 mL) of water. However, for overall fluid consumption, male athletes reported on average drinking more fluids than female athletes (men = 127 fl oz [3810 mL], women = 102 fl oz [3060 mL]). Fourteen student-athletes (5.3%; 10 men, 4 women) either did not complete the fluid consumption questionnaire or reported not drinking anything on an average day (ie, did not properly complete the questionnaire). Despite this, their urine specific gravity data were used.
DISCUSSION
The primary purpose of our cross-sectional, descriptive study was to estimate the prepractice hydration status of male and female NCAA Division I athletes by using urine specific gravity. Our secondary aims were (1) to compare the prepractice hydration status of male and female collegiate athletes and (2) to examine differences in the prepractice hydration status of female collegiate athletes in the follicular and luteal phases of menstruation.
Prepractice Hydration Status
Collegiate Athletes
We found that 66% of collegiate athletes appeared hypohydrated, suggesting that they either need to be educated about proper hydration techniques to prevent hypohydration and protect athletic performance or need to be encouraged to execute a proper hydration schedule before practices. Athletes may have been hypohydrated before practices because of their individual hydration habits and not necessarily because of their lack of knowledge or education. For instance, athletes with early morning practices may not wake up early enough to properly hydrate themselves.
Although we were unable to determine if consumption of caffeinated beverages was associated with prepractice hydration status, Grandjean et al18 reported no differences in hydration status in healthy men who consumed a combination of beverages (eg, noncaffeinated, caffeinated) on 4 separate occasions. Thus, hydration strategies should focus more on the sport than on the sex or menstrual stage of the participant.
Male and Female Collegiate Athletes
Education about proper hydration cannot be identified as a definitive reason for a smaller percentage of women than men being hypohydrated; however, a relationship may exist. Although we did not examine hydration education in this study, we have identified a potential relationship between hydration status and hydration education based on the results of this study and previous studies.
A greater percentage of women than men could have been better hydrated for several reasons. Lopez et al19 explained that women have a higher thermoregulatory threshold than men and, therefore, do not begin sweating until their core temperatures are higher. Thus, hypohydration may not be as prevalent in women as in men. Using a handheld refractometer, Stover et al15 assessed the urine specific gravity of recreational exercisers before exercise. They examined 329 women and men from 2 fitness centers: 1 in Los Angeles, California, and 1 in Chicago, Illinois. Similar to our results, they reported that 46% of the recreational athletes were hypohydrated and that men had a greater mean urine specific gravity (1.020 ± 0.007) compared with women (1.017 ± 0.008) (P = .001). Other researchers have reported similar results for males and females combined, as well as between males and females.19,20 Francesconi et al20 studied US Army trainees and found that 18.7% had a urine specific gravity equal to or more than 1.030, which was used as an initial criterion of hypohydration. Armstrong et al2 found sex differences in the hydration status of tennis players who competed on 3 consecutive days; female athletes had lower urine specific gravity than male athletes on the first and third days of competition. This difference could have been a result of sex, individual knowledge about hydration, or the current phase of menstruation.2,5,21
Follicular and Luteal Phases of Menstruation
The threshold temperature for sweating has been shown to increase in the luteal phase of the menstrual cycle9,18; however, Haddad et al22 did not report differences in total body water between the midfollicular and midluteal phases of the menstrual cycle. We did not find differences in hydration status with different phases of the menstrual cycle; however, to confirm these findings, urine specific gravity or plasma osmolarity needs to be compared within the same athletes at different times in their menstrual cycles. Having each participant record the date of onset of her last menstrual cycle could have been a reason for not finding differences in hydration status with different phases of the menstrual cycle. The request was not valid for participants who were amenorrheic and ovulating or those who took oral contraceptives and were not ovulating. This limitation affected the conclusions we drew from the data.
Application of Results
Although humans drink to quench physiologic thirst based on plasma osmolality, a water debt typically remains (“voluntary dehydration”), especially in those who are physically active on a regular basis. Hypohydration has been shown to impair endurance performance; increase core body temperature; and increase cardiovascular strain associated with body-water loss, such as hypovolemia, tachycardia, decreased venous return, and decreased stroke volume.6
All athletes could benefit from learning to recognize the signs of hypohydration. Several methods for testing hydration status include urine specific gravity, urine conductivity, serum osmolarity specific gravity, urine color, and assessment of pre-exercise and postexercise body mass.2,23 However, urine color is perhaps the easiest method for athletes to assess their hydration status, and the simplest, most reliable method of self-evaluation of urine color is a urine color chart,2,13,24 which can be easily placed in locker rooms used by recreational and competitive athletes. This chart is a subjective measurement of hydration status that is quick and easy to teach and use. The first morning void provides the most accurate urine color assessment of true hydration status.
When examining the hydration status of collegiate athletes, education regarding proper hydration must take into consideration the variety of sports that are played. We did not compare the percentages of student-athletes who were hypohydrated across various sports; however, different sports require various levels of exertion and different types of uniforms and equipment. In addition, sports are played in different seasons, at different locations, and at different times of day. All of these factors can cause athletes playing certain sports to be more prone to hypohydration. Burke and Hawley4 examined proper hydration for team sports, noting the differences between team sports and individual sports. Most often in team sports, athletes perform at or near maximal effort for periods, which are interspersed with lower-intensity work or rest. This pattern has been associated with large losses of body water4 and large interindividual variation among athletes.25 Especially high levels of probable dehydration occur in team sports, such as football and men's lacrosse, that are typically played in warmer weather, with much padding, and requiring intermittent exertion levels. The rest periods in team sports are perfect opportunities for rehydration.
Combining basic education about proper hydration and the risks of dehydration, instruction about how to perform self-assessment of hydration status, and targeted training in sport-specific hydration needs and practices could increase collegiate athletes' knowledge about proper fluid needs and potentially generate better hydration practices and lower levels of dehydration. Proper hydration could improve athletic performance.
Limitations
We realize the limitation of assessing urine specific gravity via a spot urine sample. The first morning void or the void after a 12-hour fast has been well established as the recommended time to assess urine specific gravity.21,26 We chose to assess spot urine samples before practice for several reasons: (1) It was more convenient for the coaches and athletes, (2) It provided the coaches and athletes with a general idea of prepractice hydration status, and (3) It offered some basis for comparisons for practitioners who may only have the opportunity to assess spot urine samples before team practices. The ultimate goal of our study was to provide descriptive data for collegiate athletes to be used as a catalyst for further research. In addition, our study resulted in these athletes and their coaches being more aware of their hydration status and viewing their urine color daily. We recommend that researchers study collegiate athletes using the first morning urine sample to more accurately evaluate hydration status.
CONCLUSIONS
Most NCAA Division I athletes whom we assessed via spot urine samples appeared hypohydrated. Such athletes would benefit from either more education about proper hydration practices or encouragement to create and use hydration schedules. This will help protect both their health and their athletic performance.
ACKNOWLEDGMENTS
We thank the student-athletes who participated in this study. We also thank their coaches for allowing us to collect these data before their practices. Finally, we thank Elizabeth Staebler for her assistance in preparing the article.
Footnotes
Stella L. Volpe, PhD, RD, LDN, FACSM, and Kristen A. Poule, BS, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. Erica G. Bland, BSN, contributed to analysis and interpretation of the data and drafting, critical revision, and final approval of the article.
REFERENCES
- 1.Sawka M. N. Physiological consequences of hypohydration: exercise performance and thermoregulation. Med Sci Sports Exerc. 1992;24(6):657–670. [PubMed] [Google Scholar]
- 2.Armstrong L. E., Maresh C. M., Castellani J. W., et al. Urinary indices of hydration status. Int J Sport Nutr. 1994;4(3):265–279. doi: 10.1123/ijsn.4.3.265. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong L. E., Soto J. A., Hacker F. T., Jr, Casa D. J., Kavouras S. A., Maresh C. M. Urinary indices during dehydration, exercise, and rehydration. Int J Sport Nutr. 1998;8(4):345–355. doi: 10.1123/ijsn.8.4.345. [DOI] [PubMed] [Google Scholar]
- 4.Burke L. M., Hawley J. A. Fluid balance in team sports: guidelines for optimal practices. Sports Med. 1997;24(1):38–54. doi: 10.2165/00007256-199724010-00004. [DOI] [PubMed] [Google Scholar]
- 5.Nichols P. E., Jonnalagadda S. S., Rosenbloom C. A., Trinkaus M. Knowledge, attitudes, and behaviors regarding hydration and fluid replacement of collegiate athletes. Int J Sport Nutr Exerc Metab. 2005;15(5):515–527. doi: 10.1123/ijsnem.15.5.515. [DOI] [PubMed] [Google Scholar]
- 6.Armstrong L. E., Maresh C. M., Gabaree C. V., et al. Thermal and circulatory responses during exercise: effects of hypohydration, dehydration, and water intake. J Appl Physiol. 1997;82(6):2028–2035. doi: 10.1152/jappl.1997.82.6.2028. [DOI] [PubMed] [Google Scholar]
- 7.Maughan R. J. Impact of mild dehydration on wellness and on exercise performance. Eur J Clin Nutr. 2003;57(suppl 2):S19–S23. doi: 10.1038/sj.ejcn.1601897. [DOI] [PubMed] [Google Scholar]
- 8.Rehrer N. J. Fluid and electrolyte balance in ultra-endurance sport. Sports Med. 2001;31(10):701–715. doi: 10.2165/00007256-200131100-00001. [DOI] [PubMed] [Google Scholar]
- 9.Bunt J. C., Lohman T. G., Boileau R. A. Impact of total body water fluctuations on estimation of body fat from body density. Med Sci Sports Exerc. 1989;21(1):96–100. doi: 10.1249/00005768-198902000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Cheung S. S., McLellan T. M., Tenaglia S. The thermophysiology of uncompensable heat stress: physiological manipulations and individual characteristics. Sports Med. 2000;29(5):329–359. doi: 10.2165/00007256-200029050-00004. [DOI] [PubMed] [Google Scholar]
- 11.Godek S. F., Godek J. J., Bartolozzi A. R. Hydration status in college football players during consecutive days of twice-a-day preseason practices. Am J Sports Med. 2005;33(6):843–851. doi: 10.1177/0363546504270999. [DOI] [PubMed] [Google Scholar]
- 12.Sawka M. N., Burke L. M., et al. American College of Sports Medicine. American College of Sports Medicine position stand: exercise and fluid replacement. Med Sci Sports Exerc. 2007;39(2):377–390. doi: 10.1249/mss.0b013e31802ca597. [DOI] [PubMed] [Google Scholar]
- 13.Casa D. J., Armstrong L. E., Hillman S. K., et al. National Athletic Trainers' Association position statement: fluid replacement for athletes. J Athl Train. 2000;35(2):212–224. [PMC free article] [PubMed] [Google Scholar]
- 14.Popowski L. A., Oppliger R. A., Lambert G. P., Johnson R. F., Johnson A. K., Gisolfi C. V. Blood and urinary measures of hydration status during progressive acute dehydration. Med Sci Sports Exerc. 2001;33(5):747–753. doi: 10.1097/00005768-200105000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Stover E. A., Petrie H. J., Passe D., Horswill C. A., Murray B., Wildman R. Urine specific gravity in exercisers prior to physical training. Appl Physiol Nutr Metab. 2006;31(3):320–327. doi: 10.1139/h06-004. [DOI] [PubMed] [Google Scholar]
- 16.Stuempfle K. J., Drury D. G. Comparsion of 3 methods to assess urine specific gravity in collegiate wrestlers. J Athl Train. 2003;38(4):315–319. [PMC free article] [PubMed] [Google Scholar]
- 17.Shirreffs S. M., Maughan R. J. Urine osmolality and conductivity as indices of hydration status in athletes in the heat. Med Sci Sports Exerc. 1998;30(11):1598–1602. doi: 10.1097/00005768-199811000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Grandjean A. C., Reimers K. J., Bannick K. E., Haven M. C. The effect of caffeinated, non-caffeinated, caloric and non-caloric beverages on hydration. J Am Coll Nutr. 2000;19(5):591–600. doi: 10.1080/07315724.2000.10718956. [DOI] [PubMed] [Google Scholar]
- 19.Lopez M., Sessler D. I., Walter K., Emerick T., Ozaki M. Rate and gender dependence of the sweating, vasoconstriction, and shivering thresholds in humans. Anesthesiology. 1994;80(4):780–788. doi: 10.1097/00000542-199404000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Francesconi R. P., Hubbard R. W., Szlyk P. C., et al. Urinary and hematologic indexes of hypohydration. J Appl Physiol. 1987;62(3):1271–1276. doi: 10.1152/jappl.1987.62.3.1271. [DOI] [PubMed] [Google Scholar]
- 21.Aoyagi Y., McLellan T. M., Shephard R. J. Interactions of physical training and heat acclimation: the thermophysiology of exercising in a hot climate. Sports Med. 1997;23(3):173–210. doi: 10.2165/00007256-199723030-00004. [DOI] [PubMed] [Google Scholar]
- 22.Haddad L., Milke P., Zapata L., et al. Effect of the menstrual cycle in ethanol pharmacokinetics. J Appl Toxicol. 1998;18(1):15–18. doi: 10.1002/(sici)1099-1263(199801/02)18:1<15::aid-jat463>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 23.Food and Nutrition Board: National Academy of Sciences of the Institute of Medicine. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: National Academy Press; 2005. [Google Scholar]
- 24.Armstrong L. E. Performing in Extreme Environments. Champaign, IL: Human Kinetics; 2000. [Google Scholar]
- 25.Shirreffs S. M., Aragon-Vargas L. F., Chamorro M., Maughan R. J., Serratosa L., Zachwieja J. J. The sweating response of elite professional soccer players to training in the heat. Int J Sports Med. 2005;26(2):90–95. doi: 10.1055/s-2004-821112. [DOI] [PubMed] [Google Scholar]
- 26.Armstrong L. E. Hydration assessment techniques. Nutr Rev. 2005;63(6 pt 2):S40–S54. doi: 10.1111/j.1753-4887.2005.tb00153.x. [DOI] [PubMed] [Google Scholar]