SYNOPSIS
Objective
We assessed the relationship between Chlamydia trachomatis (CT) infections identified during pregnancy and adverse perinatal birth outcomes (including premature rupture of membranes, preterm delivery, and low birthweight) by matching CT reports and birth records.
Methods
We merged California birth records from 1997, 1998, and 1999 with California CT reports from the same years to determine the proportion of birth records matched to a female CT report, using maternal last name, first name, date of birth, and county of residence. We used logistic regression to assess the crude and adjusted association between a CT report less than 10 months before the birth record date and premature rupture of membranes, preterm delivery, and low birthweight. These results were adjusted for age, race/ethnicity, level of education, and prenatal care.
Results
Of 675,786 birth records and 101,296 female CT reports, 14,039 women had a CT case report and a birth record; 10,917 birth records (1.6%) were matched to a CT report during pregnancy, and 10,940 (10.8%) of CT reports were matched to a birth record date 10 months after date of diagnosis/report. For premature rupture of membranes, the adjusted odds ratio (AOR) was 1.2, 95% confidence interval (CI) 1.0, 1.3; for low birthweight, the AOR was 1.2, 95% CI 1.1, 1.3. The reduction in birthweight associated with prenatal CT infection was 31.7 grams.
Conclusions
The increased risk of adverse perinatal outcomes associated with prenatal CT infection supports current prenatal CT screening guidelines. Matching of surveillance and vital statistics data sources was an efficient method to assess this association.
Chlamydia trachomatis (CT) is the most commonly reported infectious disease in the United States, with 780,715 cases reported among women in 2006, accounting for three-fourths of communicable diseases in the United States.1 Because most CT infections are asymptomatic, the majority of these cases have been identified through the implementation of screening programs beginning in the late 1980s, using national guidelines that target young women.2
The primary goal of screening programs is to identify and treat asymptomatic CT infections in women to prevent adverse reproductive outcomes such as pelvic inflammatory disease and infertility.3 Beyond this, prenatal CT screening has been implemented to reduce adverse neonatal outcomes such as ophthalmia neonatorum, inclusion conjunctivitis,4 and pneumonia5 acquired by vertical transmission. However, studies attempting to evaluate the role of prenatally acquired CT infections in adverse perinatal outcomes, such as premature rupture of membranes, preterm delivery, and low birthweight, have yielded inconsistent findings. Most of these studies have been limited to retrospective or cross-sectional analyses of hospital-based populations; were not designed to evaluate the role of other coexisting lower-genital-tract bacterial infections; lacked sufficient information to adjust for potential confounding by factors related to either CT infection or the outcome; and were conducted prior to the development of highly sensitive nucleic acid amplified tests, which are more effective in identifying asymptomatic infections than are tissue culture techniques used in older studies.
Given the increases seen in CT screening coverage6 nationally, the population burden of adverse perinatal outcomes due to prenatal CT infection may have decreased. However, current studies of prenatal CT infection and adverse outcomes that are generalizable to the U.S. population are limited to one analysis in which CT infections noted on birth records in Washington State were associated with a higher risk of premature rupture of membranes and preterm birth identified through infant hospital discharge data.7
We examined the association of CT infection with adverse perinatal outcomes in California by linking statewide CT case registry data to birth records.
METHODS
Study population
The analysis included calendar years 1997, 1998, and 1999 CT and birth record data for 48 local health jurisdictions (LHJs) out of the 61 total health jurisdictions (58 county and three city health departments) in California that reported line-listed CT case reports. The 11 small LHJs that did not provide line-listed CT case reports for January 1997 through December 1999 were excluded from merging of CT case reports and birth records. Additionally, San Francisco County and Los Angeles County were not included, due to the lack of last name and first name data on CT case reports transmitted to the state. Birth records indicating multiple births, mothers with preeclampsia or eclampsia, or mothers with chronic hypertension were excluded from analysis because of the known strong association between these conditions and the outcomes assessed in this analysis.
Variables and case definitions
Data elements available in both CT case report and birth record files included mother's first and last name, county of residence, race/ethnicity, date of birth, and residential zip code. Additional data elements on the birth record included level of education, parity, trimester in which prenatal care was initiated, number of visits during the pregnancy, previous history of preterm birth or low birthweight deliveries, payment sources for prenatal and delivery care, tobacco use during pregnancy, herpes noted as a complication during pregnancy or labor/delivery, fever noted during labor, premature rupture of membranes, preterm birth, and infant birthweight.
Adequacy of prenatal care utilization was assessed with the use of the Kotelchuck Index, an aggregate measure in which timing of prenatal care initiation and the percentage of recommended prenatal care visits that a woman attended are categorized in an ordinal scale as inadequate, intermediate, adequate, or adequate plus.8 Infants were considered to have low birthweight if they were less than 2,500 grams at delivery. Deliveries were considered preterm if they occurred before 37 completed weeks of gestation.
Matching procedures
First, we assessed the number and proportion of birth records and CT case reports with missing data for potential data elements for matching records. Second, we assessed the efficiency of matching CT and birth records, and compared them across different algorithms, using mother's first and last name, county of residence, and date of birth; additionally, mother's first and last names were also transformed into Soundex numeric codes, which were constructed by assigning numbers to different groups of consonants.9,10 Matching yield across each of the algorithms was assessed by comparing the proportion of CT records matched within 10 months prior to the birth record date. Individual matched records were further examined to validate the accuracy of the matching procedure; selection of matching algorithm for the final analytic sample was based on minimizing false-positive matches that would result in a conservative estimate of the association between prenatal CT infection and adverse perinatal outcomes.
Analysis
We calculated the proportion of overall birth records that had adverse perinatal outcomes matched to a CT case report during at least one trimester of the woman's pregnancy. Mothers who had a CT case report matched to a birth record were compared with mothers who did not have matched records, on the basis of demographic and prenatal care characteristics. We assessed comparisons of proportions using the Chi-square test. We estimated adjusted odds ratios (AORs) and 95% confidence intervals (CIs) to assess the association of prenatal CT infection with premature rupture of membranes, preterm birth, and low birthweight, using separate multivariate logistic regression analyses. We conducted our analyses using SAS® version 6.2.11 Covariates included in the logistic regression models were age, race/ethnicity, level of education, and utilization of prenatal care, which were found to be significantly associated with a CT case report in univariate analysis. We used linear regression to assess the relationship of birthweight (in grams) to a matched CT case report.
RESULTS
A total of 675,786 birth records and 101,296 CT case reports were available for 1997 through 1999 among the residents of the 48 LHJs included in the analysis. The proportion of records with missing data varied by data element. For example, the percent missing for mother's last name, first name, and county of residence was <1.0% for both files; the percent missing for mother's date of birth was 3.2% in CT case reports, compared with <0.1% in the birth records.
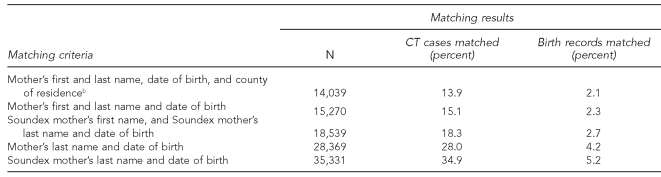
The comparison of algorithms to match CT case reports to birth records demonstrated a wide range of proportion matched (Table 1). The highest number of matched birth records and CT case reports (i.e., most liberal criterion with higher sensitivity, lower specificity) was found based on the Soundex code of mother's last name and date of birth (35,331 matches), representing 34.9% of CT case reports and 5.2% of birth records. The lowest number of matches (i.e., most conservative criterion with lower sensitivity, higher specificity) was found based on mother's first and last name, date of birth, and county of residence (14,039 matches), representing 13.9% of CT case reports and 2.1% of birth records. With the use of the most conservative match criterion, 10,917 records were found to match a CT case report during pregnancy. The total number of matched birth and CT case reports within the prenatal period represented 1.6% of births and 10.8% of CT cases.
Table 1.
Comparison of algorithms to match chlamydia case reports (n=101,296) to birth records (n=675,786), 1997–1999, Californiaa
aPrepared by the California Department of Public Health
bMost conservative matching algorithm chosen for further analyses
CT = Chlamydia trachomatis
Using the most conservative algorithm, among the 10,917 CT case reports matched to birth records, the distribution of CT case reports according to trimester of pregnancy was relatively even: 30% occurred during the first trimester, 28% occurred during the second trimester, 36% occurred during the third trimester, and 6% occurred in multiple trimesters.
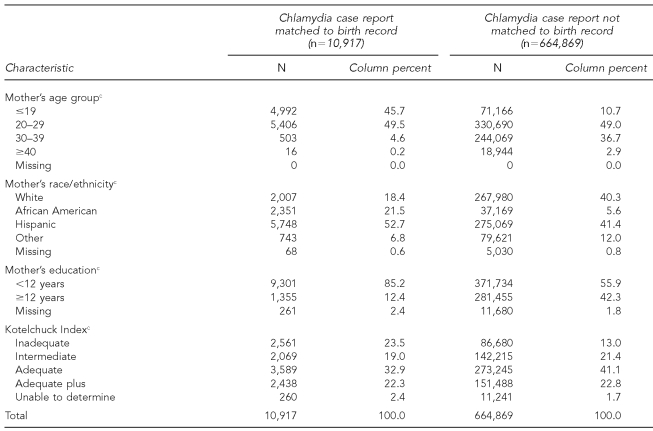
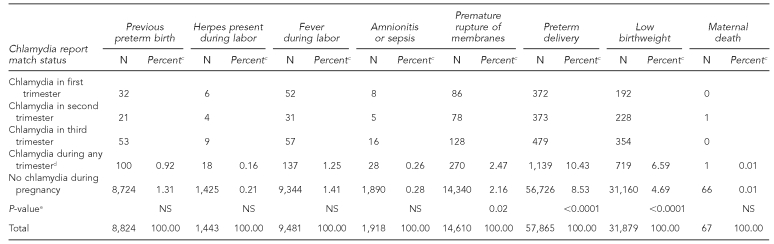
Mothers who had a perinatal CT case report matched to a birth record were more likely to be younger than age 20, to be African American, and to have a high school or lower level of education (Table 2). The proportion of women with CT case reports matched to birth records indicating -premature rupture of membranes, preterm delivery, and low birthweight was significantly greater than for women with unmatched records, whereas the proportion of women with CT case reports matched to birth records indicating previous premature birth, herpes present during labor, fever during labor, amnionitis/sepsis, and maternal death was not significantly greater than for women with unmatched records (Table 3). For these three conditions, the highest proportion (40% to 42%) of matched CT case reports was associated with the third trimester. After adjustment for maternal age, race/ethnicity, level of education, and Kotelchuck Index score, the AOR was 1.2 (95% CI 1.0, 1.3) for the association between premature rupture of membranes and prenatal CT infection; for the association between low birthweight and prenatal CT infection, the AOR was 1.2 (95% CI 1.1, 1.3). Preterm birth was not associated with prenatal CT infection. The reduction in birthweight associated with prenatal CT infection as assessed by linear regression analysis was 31.7 grams (95% CI 31.6, 31.7).
Table 2.
Comparison of demographic characteristics among mothers matcheda vs. not matched to chlamydia case report within one year prior to birth record date, 1997–1999, Californiab
aMatching of records based on last name, first name, date of birth, and county of residence
bPrepared by the California Department of Public Health
cP-value <0.0001
Table 3.
Proportion of birth records with selected adverse perinatal outcomes that were matcheda to at least one chlamydia case report within 10 months prior to birth record date, by prenatal trimester, 1997–1999, Californiab
aMatching of records based on last name, first name, date of birth, and county of residence
bPrepared by the California Department of Public Health
cPercentages were not calculated for the trimester-specific chlamydia cases because these were not mutually exclusive subcategories.
dTotals include birth records matched to chlamydia reports in multiple trimesters and reflect unique female chlamydia cases (i.e., trimester categories are not mutually exclusive).
eP-value for Chi-square comparison of proportions between mothers with matched vs. unmatched records
NS = not significant
DISCUSSION
This analysis of population-based birth records matched to CT case reports during a three-year period in California demonstrated that prenatal CT infection is weakly associated with a higher risk of premature rupture of membranes and low birthweight, after adjustment for demographic and prenatal care factors. However, these findings related to higher risk of premature rupture of membranes and low birthweight were consistent with findings of other, smaller, older cross-sectional and historical prospective studies conducted in hospital-based obstetric populations that were less generalizable and that identified CT infection using less sensitive tissue culture techniques.12–16
Only one other large population-based analysis, by Blas et al., of the association between prenatal CT infection and adverse perinatal outcomes has been conducted; this analysis demonstrated that perinatal CT infection noted on the birth record itself was significantly associated with adverse outcomes, including preterm delivery and premature rupture of membranes, but not low birthweight.7 Inconsistencies in findings from historical cohort and prospective studies regarding the association of CT infection across these adverse perinatal outcomes may be related to differences in the obstetric populations studied and potentially different etiologies for these conditions.13,14,17
Much of the challenge in interpreting the inconsistent results from previous studies may be related to the plausibility of mechanisms and causal pathways through which CT infection may be influencing the risk of adverse perinatal outcomes. In the case of mechanisms for causing increased risk of premature rupture of membranes, Alger et al. have demonstrated that lower-genital-tract CT infection may cause chorioamnionitis and, consequently, premature rupture of membranes. The impact of more recent CT infection as determined by CT immunoglobulin M (IgM) seropositivity on premature rupture of membranes was supported by the finding of a higher proportion of women who were CT IgM-positive among those with this premature rupture outcome compared with those without premature rupture.18 Our analysis found that while the occurrence of matched CT reports was relatively evenly distributed by pregnancy trimester, in the case of premature rupture of membranes, preterm delivery outcomes, and low birthweight outcomes, the highest frequency of matched CT reports was in the third trimester, suggesting a more direct role for CT infection in the pathogenesis of adverse outcomes associated with labor and delivery.
Our analysis found that the profile of mothers with CT case reports matched to birth records was consistent with that of populations with the higher risk of CT rates in these groups—e.g., adolescents, African American women, and women with poor and/or late utilization of prenatal care. Concurrently, we found consistent racial/ethnic disparities in low birthweight, with significantly higher rates among African American mothers (12.8%) than other racial/ethnic groups in 2005, which are likely related to the profile of the matched cases.19 As with other conditions, such as asthma and diabetes, for which access to preventive and clinical services is crucial to management and control, integration of services related to sexually transmitted disease prevention and control with maternal and child health services to improve access to CT screening and treatment early in the prenatal period could potentially minimize racial/ethnic disparities and have broader impact on reproductive health.
Limitations
Our analysis had a number of limitations to its reliability and validity. First, this analysis was limited to the data elements available from CT case reports and birth records submitted from clinicians, laboratories, and hospital personnel, which may differ widely in the quality of their reporting. To the extent that CT case reporting is not complete in California, the ability to match birth records may have resulted in an underestimate of CT during pregnancy and minimized the strength of associations seen. However, because laboratories in California also complete CT reporting, this may have exerted less of an influence on the estimate of effect. Lack of completeness for key demographic factors such as race/ethnicity as a result of the majority of the case reports coming from laboratory providers does suggest other limitations for assessing the extent of racial disparities for CT infection and adverse birth outcomes.
A second issue was the sensitivity and specificity of the matching algorithm used to link birth records to CT case reports. While achieving a high matching proportion is desirable, low sensitivity and/or specificity of matching may have caused an underestimate of the association between prenatal CT infection and adverse perinatal outcomes, due to misclassification of cases. To the extent that changes in the name for a given individual in the two data sources occur, the sensitivity of the matching algorithm will decrease, and the resulting misclassification will bias associations toward the null. However, validation studies, conducted with vital statistics and hospital discharge data, of the most conservative matching algorithm used in this study have indicated that there is a high degree of accuracy compared with other algorithms with higher matching rates and lower specificity.10,20
A concerning issue noted in our analysis may be the extent to which CT-infected women may not be accessing prenatal care and, therefore, are not being screened for CT, resulting in misclassification of exposure. However, it is encouraging that, despite these limitations, we were able to observe an effect of prenatal CT on increased risk of premature rupture of membranes and low birthweight. Little information about prenatal screening coverage for CT in California or elsewhere is available, but efforts to assess adherence to prenatal CT screening guidelines would be informative for evaluating this potential source of bias on our estimate of risk.
As noted previously, the data available for this -analysis were limited to the elements routinely collected on CT case reports and birth records. While demographic and prenatal data were available to control for confounding associated with both CT and adverse perinatal outcomes, there were no data related to other perinatal risk behaviors, such as smoking, drug and alcohol use, sexual risk behaviors, or patient compliance with CT treatment regimens. Further, there were no data on concurrent lower-genital-tract infections, such as Group B streptococcus, Mycoplasma hominis/gentalium, and bacterial vaginosis, all of which have also been associated with adverse perinatal outcomes. However burdensome it may be to add additional clinical and behavioral information to birth records, this information would be needed to adequately assess the relationship between perinatal exposures and adverse outcomes. Finally, because only 48 LHJs were included in this analysis, it is possible that the results may not be generalizable outside of those jurisdictions.
CONCLUSIONS
This analysis points to the utility of using existing population-based datasets to examine the association between prenatal CT infection and adverse birth outcomes. To the degree that the existing surveillance systems have been able to confirm findings from older and smaller studies of the impact of prenatal CT infections, the results from this type of analysis should be used to encourage timely identification and treatment of those at risk for prenatal CT infection and to minimize risk of adverse perinatal outcomes.
Acknowledgments
The authors gratefully acknowledge the support of the Centers for Disease Control and Prevention's Outcome Assessment through Systems of Integrated Surveillance workgroup, which was established to encourage collaborations among public health surveillance partners to identify conditions comorbid with sexually transmitted diseases and human immunodeficiency virus.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) Sexually transmitted disease surveillance, 2006. Atlanta: CDC; 2007. [Google Scholar]
- 2.Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep. 2006;55(RR-11):38–40. [PubMed] [Google Scholar]
- 3.Westrom L, Joesoef R, Reynolds G, Hagdu A, Thompson SE. Pelvic inflammatory disease and fertility. A cohort study of 1,844 women with laparoscopically verified disease and 657 control women with normal laparoscopic results. Sex Transm Dis. 1992;19:185–92. [PubMed] [Google Scholar]
- 4.Schachter J, Rose L, Meyer KF. The venereal nature of inclusion conjunctivitis. Am J Epidemiol. 1967;85:445–52. doi: 10.1093/oxfordjournals.aje.a120706. [DOI] [PubMed] [Google Scholar]
- 5.Beem MO, Saxon EM. Respiratory-tract colonization and a distinctive pneumonia syndrome in infants infected with Chlamydia trachomatis. N Engl J Med. 1977;296:306–10. doi: 10.1056/NEJM197702102960604. [DOI] [PubMed] [Google Scholar]
- 6.National Committee for Quality Assurance. The state of health care quality 2007. Washington: National Committee for Quality Assurance; 2007. [Google Scholar]
- 7.Blas MM, Canchihuaman FA, Alva IE, Hawes SE. Pregnancy outcomes in women infected with Chlamydia trachomatis: a population-based cohort study in Washington State. Sex Transm Infect. 2007;83:314–8. doi: 10.1136/sti.2006.022665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. Am J Public Health. 1994;84:1414–20. doi: 10.2105/ajph.84.9.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fan Z. Matching character variables by sound: a closer look at Soundex function and sounds-like operator. SAS® Users Group Institute, Paper 072-29. [cited 2008 Jun 5]. Available from: URL: http://www2.sas.com/proceedings/sugi29/072-29.pdf.
- 10.Li B, Quan H, Fong A, Lu M. Assessing record linkage between health care and Vital Statistics databases using deterministic methods. BMC Health Serv Res. 2006;6:48. doi: 10.1186/1472-6963-6-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.SAS Institute, Inc. SAS®: Version 6.2. Cary (NC): SAS Institute, Inc.; 2000. [Google Scholar]
- 12.Harrison HR, Alexander ER, Weinstein L, Lewis M, Nash M, Sim DA. Cervical Chlamydia trachomatisand mycoplasmal infections in pregnancy. Epidemiology and outcomes. JAMA. 1983;250:1721–7. [PubMed] [Google Scholar]
- 13.Martin DH, Koutsky L, Eschenbach DA, Daling JR, Alexander ER, Benedetti JK, et al. Prematurity and perinatal mortality in pregnancies complicated by maternal Chlamydia trachomatis infections. JAMA. 1982;247:1585–8. [PubMed] [Google Scholar]
- 14.Sweet RL, Landers DV, Walker C, Schachter J. Chlamydia trachomatis infection and pregnancy outcome. Am J Obstet Gynecol. 1987;156:824–33. doi: 10.1016/0002-9378(87)90338-3. [DOI] [PubMed] [Google Scholar]
- 15.Gravett MG, Nelson HP, DeRouen T, Critchlow C, Eschenbach DA, Holmes KK. Independent associations of bacterial vaginosis and Chlamydia trachomatis infection with adverse pregnancy outcome. JAMA. 1986;256:1899–903. [PubMed] [Google Scholar]
- 16.Ryan GM, Jr, Abdella TN, McNeeley SG, Baselski VS, Drummond DE. Chlamydia trachomatis infection in pregnancy and effect of treatment on outcome. Am J Obstet Gynecol. 1990;162:34–9. doi: 10.1016/0002-9378(90)90815-o. [DOI] [PubMed] [Google Scholar]
- 17.Andrews WW, Goldenberg RL, Mercer B, Iams J, Meis P, Moawad A, et al. The Preterm Prediction Study: association of second-trimester genitourinary chlamydia infection with subsequent spontaneous preterm birth. Am J Obstet Gynecol. 2000;183:662–8. doi: 10.1067/mob.2000.106556. [DOI] [PubMed] [Google Scholar]
- 18.Alger LS, Lovchik JC, Hebel JR, Blackmon LR, Crenshaw MC. The association of Chlamydia trachomatis, Neisseria gonorrhoeae, and group B streptococci with preterm rupture of the membranes and pregnancy outcome. Am J Obstet Gynecol. 1988;159:397–404. doi: 10.1016/s0002-9378(88)80093-0. [DOI] [PubMed] [Google Scholar]
- 19.California Department of Public Health. Birth statistics 2005. [cited 2008 Aug 6]. Available from: URL: http://www.cdph.ca.gov/data/statistics/Pages/StatewideBirthStatisticalDataTables.aspx.
- 20.Leiss JK. A new method for measuring misclassification of maternal sets in maternally linked birth records: true and false linkage proportions. Matern Child Health J. 2007;11:293–300. doi: 10.1007/s10995-006-0162-3. [DOI] [PubMed] [Google Scholar]